Summary
Multifocal cerebral venous sinus thrombosis (CVST) has a high mortality rate especially when patients present with stupor or coma. Medical treatment including anticoagulation raises concerns about the associated high risk of intracerebral hemorrhage. Treatment of multifocal CVST with mechanical thrombectomy devices and local tPA infusion have previously been reported. However, these devices may have technical limitations. Success of the new-generation aspiration thrombectomy device like the Penumbra system has been reported in few cases of isolated CVST without the use of chemical thrombolysis.
We describe two cases in which mechanical thrombectomy were used in conjunction with intra-sinus tPA infusion. Both cases were complicated and failed initial anticoagulation. Penumbra 054 was used in both cases. The Penumbra 054 is a novel device that has a bigger lumen which provides compatibility with other microcatheters, if additional therapies are required. The larger internal diameter of this catheter also allows for stronger thrombo-aspiration, potentially effecting more rapid sinus recanalization. Both cases showed remarkable clinical recovery without any major complications.
This is the first reported simultaneous use of the Penumbra system 054 along with tPA infusion. New devices such as the Penumbra system may offer additional therapeutic options in the treatment of multifocal CVST.
Key words: venous sinus thrombosis, angiography, mechanical thrombectomy
Introduction
Cerebral venous sinus thrombosis (CVST) can be a devastating disease. It is a rare form of stroke (0.5% to 1% of all strokes) that preferentially affects the younger population 1. Increased awareness of this potentially life-threatening disease has been raised in the recent past.
There is limited evidence regarding best treatment practices for CVST. Data from three randomized controlled clinical trials in combination with observational data on outcomes and bleeding complications of anticoagulation that supports a role for anticoagulation in treatment of CVST regardless of the presence of intracerebral hemorrhage before the initiation of the treatment 2. Anticoagulation alone may not be sufficient to dissolve a large and extensive thrombus or multifocal thrombosis leading to clinical deterioration and increased mortality and morbidity 2. Small retrospective studies and case series have shown some benefit of direct catheter fibrinolytic treatment which is usually reserved for refractory CVST 2,3. Data on using mechanical thrombectomy devices is anecdotal and only mentioned in case reports and small case series. Most of the mechanical thrombectomy devices have technical limitations 2.
We describe two cases of CVST in which the new-generation Penumbra 054 was used along with local tPA infusion. In our institute use of mechanical thrombectomy is reserved for patients who show clinical deterioration despite being on therapeutic anticoagulation for at least 24 hours.
Case 1
A 54-year-old woman with diabetes and hypertension presented with a three-day history of headache followed by unconsciousness. On examination, the patient was comatose with extensor posturing to painful stimuli. Her admission NIHSS was 31. Non-contrast head CT revealed extensive CVST involving the superior sagittal sinus (SSS), straight sinus (StrS), right transverse sinus (TvS) and left frontal lobe ischemic infarction. (Figure 1). An MRI brain revealed bilateral thalamic and basal ganglia hyperintensities on fluid attenuated inversion recovery (FLAIR) images and left frontal lobe hyperintensity on FLAIR and diffusion-weighted image (DWI), supporting diagnoses of multifocal CVST involving both superficial and deep venous sinuses. There was no evidence of hemorrhagic infarction on gradient echo images (Figure 1). Hypercoagulable profile was unremarkable except for Factor VIII activity of 262% (50-150%) and ESR of 56. The patient received heparin infusion for two days with no clinical improvement. It was decided to pursue endovascular treatment.
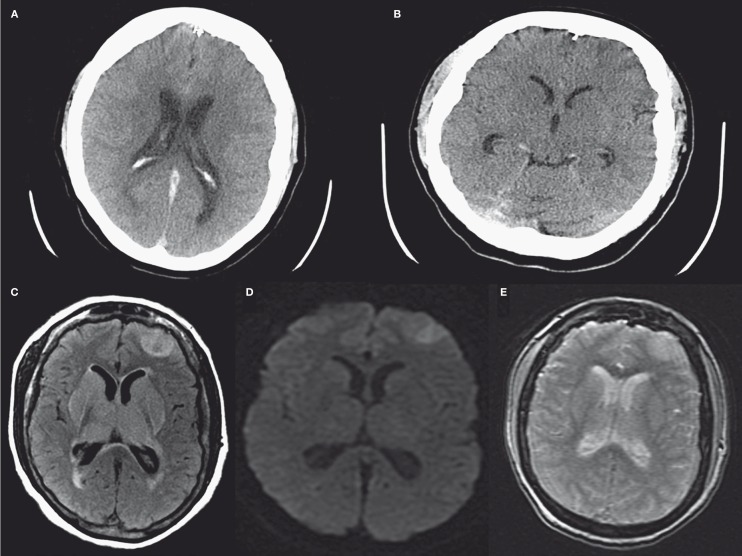
Figure 1.
A,B) Non-contrast head CT of case 1 shows extensive CVST involving the SSS, StrS, right TvS and left frontal lobe venous infarction. C) MRI FLAIR of case 1 shows left frontal, bilateral thalamic and basal ganglia hyperintensities. D) MRI DWI of case 1 shows left frontal diffusion restriction. E) GRE of case 1 shows no hemorrhagic conversion of left frontal lobe venous infarction.
The patient underwent cerebral angiography, showing extensive filling defects involving the SSS, TvS s, right sigmoid sinus (SigS) and StrS. Venous sinuses were catheterized using the Penumbra 054 device and microwire Synchro 14 in conjunction with local catheter delivered tPA administration. A 6 French Shuttle sheath was used as a guiding catheter. The microcatheter and the Penumbra system were positioned within the right tvS, sigS, mid SSS and StrS and multiple mechanical clot aspirations were performed with the Penumbra microcatheter and separator system under direct fluoroscopic observation, in conjunction with local tPA administration (2 mg in right tvS and sigS, 2 mg in mid SSS and 4mg in StrS). A microcatheter was left in the StrS for overnight infusion of tPA (10 mg at 1 mg/h) (Figure 2). Repeat angiogram the next day showed partial recanalization of the right SigS, right TvS, StrS and vein of Galen. Occlusive thrombus remained in the SSS. Multiple mechanical clot aspirations were performed in the right SigS, TvS and SSS. Microcatheter was again left in the anterior aspect of the SSS for overnight tPA infusion (10 mg at 1 mg/h). Repeat angiogram showed marked improvement of the overall patency of the superficial and deep sinuses (Figure 3).
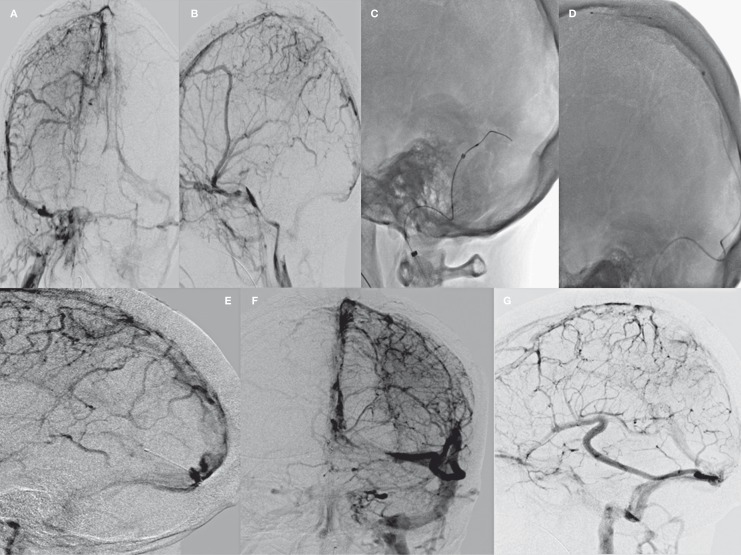
Figure 2.
A,B) Diagnostic angiography of case 1 showing extensive cerebral venous sinus thrombosis. C-E) Day 1 of treatment: Clot aspiration and microcatheter tPA infusion. F,G) Day 2, diagnostic angiography of case 1 showing partial recanalization of the right SigS, right TvS, StrS and vein of Galen. Occlusive thrombus remained in the SSS.
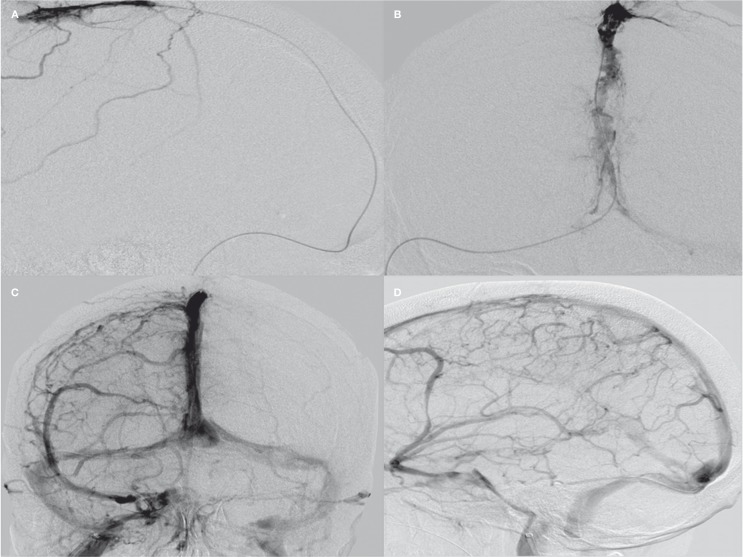
Figure 3.
A,B) Day 2 of treatment: Clot aspiration and microcatheter tPA infusion. C,D) Day 3, diagnostic angiography showed improved flow in the right TvS, SigS, right IJV as well as deep venous system.
The patient gradually regained consciousness on hospital day 5. She was discharged on anticoagulation with warfarin. At discharge, she was oriented to name, had normal language, followed commands and had residual right hemiparesis. She scored 3 on modified Rankin Scale (mRS) at discharge. Her total hospital stay was ten days.
Case 2
A 54-year-old woman with a history of myeloproliferative disorder, multiple deep venous thromboses (DVTs), left internal jugular vein (IJV) and brachiocephalic vein thromboses and hypertension presented with a three-week history of headache. The patient had been on warfarin for DVTs but had stopped taking it one week earlier for a dental procedure. MR venogram of the brain showed partially occlusive filling defect within the torcula, StrS, and right TvS and left IJV. The bilateral internal cerebral veins and proximal vein of Galen were patent. The patient was heparinized and discharged on warfarin once her INR was therapeutic at 2.3. She returned one week later with worsening headache and right eye pain despite being therapeutic on warfarin. The patient also developed facial swelling secondary to bilateral IJV occlusion. A repeat MRV showed progression of thrombosis with involvement of posterior SSS and right IJV. However, MRI brain did not show any evidence of venous infarction. The patient underwent cerebral angiography which showed complete occlusion of the posterior one fifth of the SSS extending into the torcula. There was no filling of the left TvS, StrS or bilateral IJV. There was only partial filling of the right TrS with extensive clot burden noted. The patient was considered a candidate for endovascular intervention because of worsening headaches, facial swelling and eye pain and evidence of clot progression on MRV despite being on therapeutic warfarin with an INR of 3.2. A 6 French Shuttle sheath was used as a guiding catheter. Under fluoroscopic guidance, a synchro 14 microwire was used to macerate the clot and microcatheter was advanced over wire across the distal right IJV, right TrS and into the posterior SSS beyond the thrombus. The Penumbra 054 catheter was then advanced and mechanical thrombectomy and clot aspiration was performed in the distal right IJV and right TrS. The microcatheter was then advanced over wire through the Penumbra catheter back into the posterior SSS with tip in the center of the clot. 4 mg of intra-sinus tPA was then administered. The microcatheter was then attached to tPA infusion (10 mg at 1 mg/h) and left in place overnight.
The next day diagnostic angiography showed some improvement in the distal SSS flow and right TrS flow, but there was still significant flow limitation in the right SigS and IJVs. Further, there was still a significant amount of venous drainage going retrograde into the petrosal veins. The microcatheter was then withdrawn and the Penumbra 054 catheter was then advanced over the wire which was then used to perform mechanical thrombectomy and clot aspiration of the right SigS and IJV. Subsequent venograms through the Penumbra catheter demonstrated progressive opening of the SigS and IJV. The microcatheter was then advanced over the wire through the Penumbra catheter back into the sigmoid-transverse sinus junction and was attached to tPA infusion and left in place overnight. The following day, a repeat angiogram showed improved flow in the right transverse, sigmoid sinuses as well as the right internal jugular vein. There was good filling in the deep venous system.
Clinically, the patient's headache improved and facial swelling resolved. Her discharge mRS was 0 and her total hospital stay was 15 days.
Discussion
Use of endovascular techniques for direct thrombolytic infusion was first reported by Scott et al. in 1988 4. Dowd et al. described the first case of using a mechanical thrombectomy device to treat CVST 5. Mechanical thrombectomy devices are broadly classified into five groups, including clot retrievers, aspiration/suction devices, snare-like devices, ultrasonography technologies, and lasers. The aspiration/suction devices include the Amplatz Thrombectomy, AngioJet, NeuroJet, Oasis Thrombectomy, Penumbra System, and Vasco +35. The best data on aspiration/suction devices is on AngioJet (MEDRAD, Inc, Warrendale, PA, USA) considering that it is also the oldest device on the market. The AngioJet uses hydrodynamic thrombolytic action occurring at the tip of the catheter via the Venturi effect from high-velocity saline jets. The jets cause disruption of the thrombus which is pushed down to the second lumen of the device. The advantages of AngioJet catheter include a quicker rate of recanalization of the major dural sinuses compared to locally delivered thrombolytic agents that can require a substantial amount of time to completely lyse a massive clot. Major disadvantages of the device include bulkiness and stiffness, making it tougher to access smaller sinuses and possibility of perforation of venous sinus wall 2,6,7.
The Penumbra System (Penumbra, Inc, Alameda, CA, USA) is a new-generation thrombo-aspiration device. It uses a reperfusion catheter that aspirates thrombus while passing a wire-based separator within the catheter to break up the clot and facilitate aspiration. The major advantages of the Penumbra system over other aspiration devices are the smaller size and the bulk removal of a thrombus with suction aspiration without a need to completely withdraw the catheter 8. Choulakian et al. reported the first use of Penumbra system for lysing cerebral venous thrombosis in four patients. All cases were performed with the Penumbra 0.41 which has a smaller lumen and required a simultaneous use of balloon angioplasty in three cases to augment thrombolysis 6.
Most of the case reports and series on mechanical thrombectomy devices have used local intra-sinus tPA either during the procedure or as continuous catheter infusion for a longer duration 9.
Very few cases of simultaneous use of the Penumbra system and local tPA infusion are reported in literature with good clinical recovery 8,10. One case from our institution also used glycoprotein IIb/IIIa inhibitors infusion along with local tPA infusion. In all cases a Penumbra 041 catheter was used.
The Penumbra 054 is a novel device that has a larger lumen which provides compatibility with other microcatheters if additional therapies are required. The larger internal diameter of this catheter also allows for stronger thrombo-aspiration, potentially effecting more rapid sinus recanalization. The same catheter can be used for local tPA infusion and thrombo-aspiration minimizing the use of re-catheterization.
Conclusion
We describe two cases in which the Penumbra system 054 was used in conjunction with tPA infusion with excellent technical and clinical success. This is the first reported use of Penumbra system 054 in conjunction with tPA infusion.
New devices such as the Penumbra system may offer additional therapeutic options in the treatment of multifocal CVST.
References
- 1.Stam J. Thrombosis of the cerebral veins and sinuses. New Eng J Med. 2005;352:1791–1798. doi: 10.1056/NEJMra042354. [DOI] [PubMed] [Google Scholar]
- 2.Saposnik G, Barinagarrementeria F, Brown RD, Jr, et al. Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:1158–1192. doi: 10.1161/STR.0b013e31820a8364. [DOI] [PubMed] [Google Scholar]
- 3.Canhao P, Falcao F, Ferro JM, et al. Thrombolytics for cerebral sinus thrombosis: a systematic review. Cerebrovasc Dis. 2003;15:159–166. doi: 10.1159/000068833. [DOI] [PubMed] [Google Scholar]
- 4.Scott JA, Pascuzzi RM, Hall PV, et al. Treatment of dural sinus thrombosis with local urokinase infusion. Case report. J Neurosurg. 1988;68:284–287. doi: 10.3171/jns.1988.68.2.0284. [DOI] [PubMed] [Google Scholar]
- 5.Dowd CF, Malek AM, Phatouros CC, et al. Application of a rheolytic thrombectomy device in the treatment of dural sinus thrombosis: a new technique. Am J Neuroradiol. 1999;20:568–570. [PMC free article] [PubMed] [Google Scholar]
- 6.Choulakian A, Alexander MJ. Mechanical thrombectomy with the penumbra system for treatment of venous sinus thrombosis. J Neurointervent Surg. 2010;2:153–156. doi: 10.1136/jnis.2009.001651. [DOI] [PubMed] [Google Scholar]
- 7.Chow K, Gobin YP, Saver J, et al. Endovascular treatment of dural sinus thrombosis with rheolytic thrombectomy and intra-arterial thrombolysis. Stroke. 2000;31:1420–1425. doi: 10.1161/01.str.31.6.1420. [DOI] [PubMed] [Google Scholar]
- 8.Rickert KL, Purdy PD, Welch BG. Mechanical and chemical thrombolysis of cerebral sinus thrombosis: evolution of a technique. J Neurosurg. 2011;114:136–139. doi: 10.3171/2010.2.JNS09685. [DOI] [PubMed] [Google Scholar]
- 9.Rahman M, Velat GJ, Hoh BL, et al. Direct thrombolysis for cerebral venous sinus thrombosis. Neurosurg Focus. 2009;27:E7. doi: 10.3171/2009.7.FOCUS09146. [DOI] [PubMed] [Google Scholar]
- 10.Kulcsar Z, Marosfoi M, Berentei Z, et al. Continuous thrombolysis and repeated thrombectomy with the Penumbra System in a child with hemorrhagic sinus thrombosis: technical note. Acta Neurochirurg. 2010;152:911–916. doi: 10.1007/s00701-009-0570-4. [DOI] [PubMed] [Google Scholar]