Summary
Serious complications related to percutaneous vertebral augmentation procedures, vertebroplasty and kyphoplasty, are rare and most often result from local cement leakage or venous embolization. We describe an adult patient who underwent multi-level, thoracic percutaneous vertebral augmentation procedures for painful osteoporotic compression fractures. The patient’s percutaneous vertebroplasty performed at the T9 level was complicated by the asymptomatic, direct embolization of the right T9 segmental artery with penetration of cement into the radicular artery beneath the pedicle. We review the literature regarding the unusual occurrence of direct arterial cement embolization during vertebral augmentation procedures, discuss possible pathomechanisms, and alert clinicians to this potentially catastrophic vascular complication.
Key words: vertebroplasty, vascular complications, cement embolization, artery of Adamkiewicz
Introduction
The percutaneous vertebral augmentation procedures with polymethylmethacrylate (PMMA), vertebroplasty and kyphoplasty, are increasingly popular options for the treatment of severe, refractory pain associated with vertebral compression fractures.
Originally described for the treatment of an aggressive cervical hemangioma, these procedures have gained widespread acceptance for the treatment of painful vertebral fractures secondary to osteoporosis and malignancy, albeit with some controversy regarding their overall efficacy 1-3.
The popularity of percutaneous vertebral augmentation procedures is twofold – nearly immediate pain relief and low complication rates – making them ideally suited for palliation. Serious adverse events are uncommon and most often a manifestation of extra-corporeal cement leakage with neural compression, or venous cement embolization with pulmonary emboli.
Isolated case reports of direct arterial injury have recently been described related to malpositioning of the needle during cannulation of the vertebral body 4,5. Direct arterial embolization of cement is exceptionally rare with only a handful of isolated case reports related to vertebral augmentation procedures (percutaneous and open) 6,7.
Herein, we describe an uncommon vascular complication of percutaneous vertebroplasty (PV) via a standard trans-pedicular approach for the treatment of a painful osteoporotic thoracic compression fracture – direct cement embolization of an intercostal segmental artery.
We provide a review of the literature, discuss possible pathomechanisms, and alert clinicians to this potentially catastrophic vascular complication.
Case Report
History and Examination. This 83-year-old woman presented with spontaneous, sudden onset, mid-thoracic back pain. Her medical history was significant for osteopenia. She was on bisphosphonate therapy. The pain was relieved by lying down, aggravated by standing up, and graded as 9/10 on a visual analogue scale. Subsequent investigations including spine MRI demonstrated a chronic vertebral compression fracture at T7, and acute compression fractures involving the T9 and T10 vertebral bodies with 70% and minimal loss of height, respectively.
Operation. The patient underwent successful right trans-pedicular PV and bi-pedicular percutaneous kyphoplasty procedures at the T9 and T10 levels, respectively. A PV procedure was selected at the uppermost level due to very hard bone and the perceived inability to effectively inflate the balloon tamps. For the PV, the pedicle was accessed with a 13G vertebroplasty needle (Cook Medical Inc., Bloomington, IN, USA). 1 cc Medallion syringes (Merit Medical Systems Inc., South Jordan, UT, USA) were used to inject PMMA bone cement (KyphX HV-R, Medtronic Inc., Minneapolis, MN, USA) under continuous lateral and intermittent anteroposterior (AP) fluoroscopy. The PV procedure was terminated when vascular extracorporeal cement leakage was documented during injection via the right T9 pedicle (Figure 1). The kyphoplasty procedure was performed using a Kyphon Balloon Kyphoplasty kit (Medtronic Inc., Minneapolis, MN, USA) according to the manufacturer's instructions. The percutaneous spine procedures were performed under conscious sedation. The patient benefitted from immediate and significant pain relief (improved to 5/10).
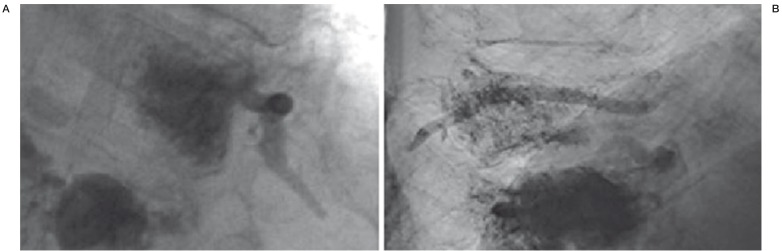
Figure 1.
A) AP view, real-time fluoroscopic image demonstrating extracorporeal leakage of cement into the T9 intercostal artery beneath the 9th rib. B) Lateral view, corresponding real-time fluoroscopic image demonstrating direct arterial cement embolization of the T9 segmental artery extending from the anterior vertebral body wall to the neural foramina beneath its pedicle.
Postoperative Course. One month later, the patient again complained of severe, mid- to lower thoracic back pain. A repeat MRI spine demonstrated a new T11 compression fracture involving her superior endplate. A bi-pedicular PV was performed with excellent pain relief. During the subsequent diagnostic evaluation of her underlying osteopenia, a CT spine was performed that demonstrated cement embolization of her right T9 intercostal segmental artery (Figure 2). There was also penetration of cement into the radicular artery beneath the right T9 pedicle. In retrospect, what was interpreted during the PV as venous extracorporeal cement embolization was in fact direct embolization of a segmental artery. No active intervention was warranted and the patient remained asymptomatic.
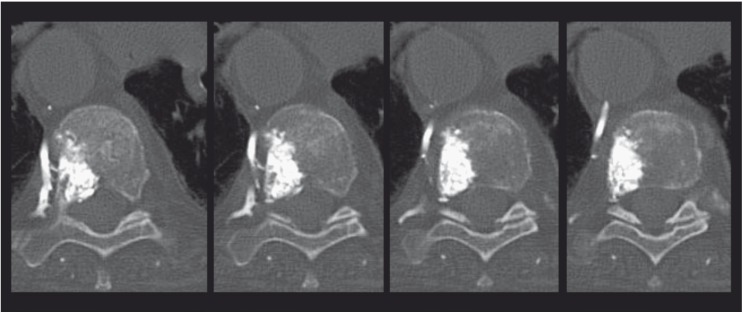
Figure 2.
Non-contrast spine CT, axial plane, demonstrating arterial cement embolization of the right T9 segmental artery. Note the direct communications of the pedicle and vertebral body with the segmental artery via multiple, small somatic branches. Also note cement migration in a retrograde fashion toward the posterior wall of the thoracic aorta.
Discussion
Percutaneous vertebral augmentation procedures, vertebroplasty and kyphoplasty are important tools in the treatment of painful vertebral fractures secondary to osteoporosis and malignancy. The often immediate pain relief and low complication rates have added to the popularity of the procedures.
Serious adverse events are uncommon and generally related to inadvertent extracorporeal leakage of cement. In the recent VERTOS II trial, 72% of injected vertebrae demonstrated cement leakage, most commonly into the disc space or segmental veins 2. All patients remained asymptomatic. Pulmonary emboli are more common than previously appreciated, but rarely symptomatic. Notwithstanding, neurologic deficit following percutaneous vertebral augmentation procedures is well documented 4.
Vascular arterial complications related to percutaneous vertebral augmentation procedures have been reported, but are confined to isolated case reports. Puri et al. reported two cases of lumbar artery pseudoaneurysm related to malpositioning of the needle during cannulation of the vertebral body 6. Direct arterial migration of cement is also infrequent, and potentially catastrophic. These cases are summarized in Table 1. Tsai et al. reported direct embolization of the left T10 segmental artery during open vertebroplasty for decompression and stabilization of a vertebral body fracture secondary to metastatic adenocarcinoma 8. This patient awoke from her anesthesia paraplegic with an anterior cord syndrome secondary to cement embolization of the anterior spinal artery. Soultanis et al. described a patient with ankylosing spondylitis who underwent cement-augmented pedicle screw revision after failure of posterior spinal instrumentation 9. The patient awoke from his anesthesia with acute right leg ischemia secondary to cement embolization of the left L3 lumbar artery, aorta, and infragenicular arteries of the right leg. Amoretti et al. reported the asymptomatic cement embolization of the right L3 lumbar artery and aorta after PV via an extra-pedicular approach for the treatment of an L3 compression fracture secondary to metastatic breast cancer 10. Taken together, these cases demonstrate that direct arterial embolization of cement during percutaneous vertebral augmentation procedures is possible, albeit rare, and can have dire consequences. The mechanism of arterial cement embolization, however, remains poorly understood.
Table 1.
Literature review of direct arterial cement embolization during spine procedures.
| Authors & Year | Age (yrs), Sex |
Spine Procedure |
Pathology | Side, Segmental Artery, Final Embolized Artery |
Symptoms |
|---|---|---|---|---|---|
| Matouk et al., present study |
83, F | PV (TP) | osteoporosis | R, T9 → aorta & intercostal art. |
asymptomatic |
| Tsai et al., 2010 | 63, F | OV | metastasis (adenocarcinoma) |
L, T10 → aorta & ASA |
anterior cord syndrome |
| Soultanis et al., 2009 | 47, M | CAPSR | AS-related spinal pseudoarthrosis |
L, L3 → aorta → infra. gen. art. |
limb ischemia |
| Amoretti et al., 2007 | 72, F | PV (EP) | metastasis (breast cancer) |
R, L3 → aorta | asymptomatic |
| Baumann et al.*, 2007 | 77, F | osseous phlebography |
osteoporosis | L4 | NA |
|
* This is a report of osseous phlebography that demonstrated opacification of a lumbar artery. As a result, PV was successfully performed via the contralateral pedicle without arterial cement embolization. Abbreviations: AS = ankylosing spondylitis; ASA = anterior spinal artery; CAPSR = cement-augmented pedicle screw revision; EP = extra-pedicular approach; infra. gen. art. = infragenicular arteries; NA = not applicable; OV = open vertebroplasty; PV = percutaneous vertebroplasty; TP = trans-pedicular approach. | |||||
In the adult configuration, each spinal segmental artery continues to supply blood to the vertebral bodies (via multiple, intraosseous, somatic branches) and nerve roots, but only a few reach the spinal cord. An injury to somatic branches by the needle, or inciting pathology, can provide a route for direct arterial cement embolization during vertebral augmentation procedures. Similarly, deposition of cement under pressure into vertebral sinusoids can result in retrograde migration of cement into the segmental arterial system, as has previously been described in cases of fibrocartilaginous embolism to the spinal cord. It is not necessary to invoke a requirement for pathologic intratumoral arteriovenous shunting, as some authors have suggested. This is consistent with the observation of direct arterial cement embolization during vertebral augmentation procedures for non-neoplastic pathologies, as was seen in our case. The spinal cord supply will only variably be at risk depending on the origin of the artery of Adamkiewicz, and penetration of cement in an antegrade fashion toward the neural foramen.
Several technical aspects should be considered to prevent vascular embolization (arterial or venous) during vertebral augmentation procedures. First, excellent, real-time visualization, preferably with biplane fluoroscopy during the cement injection is a requisite for the safe performance of percutaneous vertebral augmentation procedures. Typically, segmental arteries course along the mid-portion of thoraco-lumbar vertebral bodies. On the AP view, extension of cement lateral to the pedicle should provoke a pause in injection. Similarly, on the lateral view, extension of cement anterior to the vertebral body, or posteriorly toward the neural foramen, should terminate the procedure. The rate of injection should be slow enough to allow the operator time to react to the real-time radiographic output. Second, the viscosity of the PMMA cement and injection pressures are likely important considerations. Finally, consideration should be given to the use of intra-procedural osseous phlebography, which can document opacification of a segmental artery with contrast (Table 1), and thereby allow repositioning of the needle prior to cement injection.
In summary, we describe a woman with osteoporotic compression fractures whose T9 level PV was complicated by the asymptomatic, direct arterial cement embolization of a segmental artery. We alert clinicians to this potentially catastrophic vascular complication and suggest technical considerations to prevent its occurrence. Importantly, this complication can occur in the context of neoplastic and non-neoplastic disease.
Acknowledgments
The authors thank the members of the Division of Neuroradiology, Toronto Western Hospital, for many fruitful discussions and critical review of the manuscript.
References
- 1.Galibert P, Deramond H, Rosat P, et al. [Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty] Neurochirurgie. 1987;33:166–168. [PubMed] [Google Scholar]
- 2.Klazen CA, Lohle PN, de Vries J, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet. 2010;376:1085–1092. doi: 10.1016/S0140-6736(10)60954-3. [DOI] [PubMed] [Google Scholar]
- 3.Berenson J, Pflugmacher R, Jarzem P, et al. Balloon kyphoplasty versus non-surgical fracture management for treatment of painful vertebral body compression fractures in patients with cancer: a multicentre, randomised controlled trial. Lancet Oncol. 2011;12:225–235. doi: 10.1016/S1470-2045(11)70008-0. [DOI] [PubMed] [Google Scholar]
- 4.Patel AA, Vaccaro AR, Martyak GG, et al. Neurologic deficit following percutaneous vertebral stabilization. Spine. 2007;32:1728–1734. doi: 10.1097/BRS.0b013e3180dc9c36. [DOI] [PubMed] [Google Scholar]
- 5.Luetmer MT, Bartholmai BJ, Rad AE, et al. Asymptomatic and unrecognized cement pulmonary embolism commonly occurs with vertebroplasty. Am J Neuroradiol. 2011;32:654–657. doi: 10.3174/ajnr.A2368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Puri AS, Colen RR, Reddy AS, et al. Lumbar artery pseudoaneurysm after percutaneous vertebroplasty: a unique vascular complication. J Neurosurg Spine. 2011;14:296–299. doi: 10.3171/2010.10.SPINE1082. [DOI] [PubMed] [Google Scholar]
- 7.Hard JM, Gonda RL, Kadakia SR. A novel approach to treatment of unexpected vertebroplasty complication. Cardiovasc Intervent Radiol. 2008;31:1249–1251. doi: 10.1007/s00270-008-9353-1. [DOI] [PubMed] [Google Scholar]
- 8.Tsai YD, Liliang PC, Chen HJ, et al. Anterior spinal artery syndrome following vertebroplasty: a case report. Spine. 2010;35:E134–136. doi: 10.1097/BRS.0b013e3181b52221. [DOI] [PubMed] [Google Scholar]
- 9.Soultanis K, Kakisis JD, Pyrovolou N, et al. Peripheral arterial embolization of cement during revision spine surgery. Ann Vasc Surg. 2009;23:413–e9-12. doi: 10.1016/j.avsg.2008.08.027. [DOI] [PubMed] [Google Scholar]
- 10.Amoretti N, Hovorka I, Marcy PY, et al. Aortic embolism of cement: a rare complication of lumbar percutaneous vertebroplasty. Skeletal Radiol. 2007;36:685–687. doi: 10.1007/s00256-006-0261-7. [DOI] [PubMed] [Google Scholar]
- 11.Scroop R, Eskridge J, Britz GW. Paradoxical cerebral arterial embolization of cement during intraoperative vertebroplasty: case report. Am J Neuroradiol. 2002;23:868–870. [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 12.Tosi L, Rigoli G, Beltramello A. Fibrocartilaginous embolism of the spinal cord: a clinical and pathogenetic reconsideration. J Neurol Neurosurg Psychiatry. 1996;60:55–60. doi: 10.1136/jnnp.60.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]