Abstract
Objective
To investigate prevalence, diagnostic patterns, and parallel use of daytime versus out-of-hours primary health care in a defined population (n = 23,607) in relation to mental illness including substance misuse.
Design
Cross-sectional observational study.
Setting
A Norwegian rural general practice cooperative providing out-of-hours care (i.e. casualty clinic) and regular general practitioners’ daytime practices (i.e. rGP surgeries) in the same catchment area.
Subjects
Patients seeking medical care during daytime and out-of-hours in 2006.
Main outcome measures
Patients’ diagnoses, age, gender, time of contact, and parallel use of the two services.
Results
Diagnoses related to mental illness were given in 2.2% (n = 265) of encounters at the casualty clinic and in 8.9% (n = 5799) of encounters at rGP surgeries. Proportions of diagnoses related to suicidal behaviour, substance misuse, or psychosis were twice as large at the casualty clinic than at rGP surgeries. More visits to the casualty clinic occurred in months with fewer visits to rGP surgeries. Most patients with a diagnosis related to mental illness at the casualty clinic had been in contact with their rGP during the study period.
Conclusion
Psychiatric illness and substance misuse have lower presentation rates at casualty clinics than at rGP surgeries. The distribution of psychiatric diagnoses differs between the services, and more serious mental illness is presented out-of-hours. The casualty clinic seems to be an important complement to other medical services for some patients with recognized mental problems.
Key Words: After-hours care, emergency medical services, family practice, physician's practice patterns, primary health care, psychiatry
Most mentally ill patients in Norway are dealt with by the primary health care system, and out-of-hours GP services are the main source of acute referrals to psychiatric wards. Differences between daytime and out-of-hours services regarding relative prevalence, diagnostic challenges, and parallel use have previously been unknown.
Prevalence of diagnoses related to mental illness is lower at out-of-hours services compared with daytime services. However, suicidal behaviour, substance misuse, and psychosis are more prevalent out-of-hours than during the daytime.
Use of out-of-hours services increases in periods with low use of daytime services.
Most patients with diagnoses related to mental illness out-of-hours had also seen their regular general practitioner during the study period.
Norway has a two-tier public health care system where regular general practitioners (rGPs) serve as gatekeepers for all specialized health services including psychiatric health care [1,2]. Most patients with mental illness are therefore dealt with by the primary health care system, with relatively few patients referred to psychiatrists [3,4].
Local municipalities (Norwegian kommuner) are responsible for providing all primary health care, including access to an rGP and 24-hour access to emergency health care [5,6]. Although optional, almost all Norwegians are listed with an rGP in their residing municipality. The rGPs provide emergency care to their listed patients during office hours. Out-of-hours, most municipalities organize the emergency care with one or more GPs on call, usually based in a casualty clinic. Depending on the size of the municipality and the population served, the casualty clinic might be cooperatively shared between several municipalities [1]. Henceforth casualty clinic is used as a general term for out-of-hours services, and rGP surgeries refer to rGPs’ work during normal office hours. At a national level, approximately 66% of inhabitants annually have at least one appointment with their rGP and 16% contact the casualty clinics [7].
International studies indicate that psychiatric patients are frequent users of emergency medical health services [12–14]. In Norway, however, diagnoses related to mental illness are given in only 2–5% of patient contacts with casualty clinics [7,9,10,15], while mental illness accounts for 5–12% of consultations at rGP surgeries [7–11]. Nevertheless, casualty clinics are the major source of acute referrals to psychiatric wards [16]. This raises the possibility that patients’ use of the two primary health care services may differ, and that casualty clinics mainly deal with more severe mental illness.
In this study we compared a defined population's use of daytime rGP appointments versus their use of the out-of-hours casualty clinic in relation to mental illness. Main measures were relative prevalence and diagnostic differences. We also studied patients’ parallel use of these two services.
Material and methods
A rural general practice cooperative serving seven municipalities was selected for the study. The rGP surgeries in the same municipalities were invited to participate. All surgeries in three of the municipalities and three out of four in a fourth municipality agreed to take part. In 2006 the 22 participating rGPs had a total of 23,607 inhabitants listed, corresponding to 89.6% of the population of the four participating municipalities.
A tailor-made computer program automatically searched the electronic medical patient records for any diagnosis filed in 2006. If a diagnosis was found, the following information was extracted from the patient's billing card: date and time of day for initiating the billing card, patient gender and birth year, municipality of residence, the first diagnosis listed, and reimbursement codes.
The information was gathered anonymously. However, the computer program assigned a unique code to each patient based on their 11-digit national identity number consisting of date of birth and a five-digit personal number which is unique to each registered Norwegian resident. Usually the assigned code could be traced between medical records from different sites. However, if the patient's record contained only information on date of birth (i.e. not the full identity number) the patient was still assigned a unique code allowing us to recognize multiple contacts during 2006 within the same medical record, but not in medical records from different sites.
Patients registered as living in non-participating municipalities were excluded. Billing cards issued for the same patient at less than a two-hour interval were considered duplicates and only the card with the most complete information was used. However, if duplicates had different diagnoses then both billing cards were retained and regarded as unique. From information in the reimbursement codes we distinguished consultations, home visits, and out-of-building emergency responses. Henceforth we refer to contacts between doctor and patient as events and the subset of home visits and emergency responses as out-of-office events.
The International Classification of Primary Care-2 (ICPC-2) [17] was used. Chapter P of ICPC-2 consists of 26 codes for psychological symptoms and complaints and 17 codes for psychiatric diagnoses. After initial frequency analyses we grouped the codes in the following clusters in accordance with the type or group of symptoms they reflected: depression (P03, P76), substance abuse (P15, P16, P17, P18, P19), anxiety (P01, P27, P74, P75, P79, P82), acute stress reaction (P02), unspecified P-diagnoses (P28, P29, P99), psychosis (P71, P72, P73, P98), sleep disturbance (P06), suicidal behaviour (P77), memory disturbance (P20, P70), and others (P04, P05, P07, P08, P09, P10, P11, P12, P13, P22, P23, P24, P25, P78, P80, P81, P85, P86).
Data were analysed using SPSS 15.0. Group differences were tested with two-tailed Pearson's chi-squared test. Correlation between number of monthly events at the casualty clinic and the rGP surgeries were tested with Pearson's r. Due to a skewed distribution, correlation between visits to the casualty clinic and the rGP surgeries at an individual level were tested with Spearman's rho. Statistical significance was accepted at p < 0.05.
The project was approved by the Regional Committee for Medical Research Ethics and the Norwegian Social Science Data Services. The Norwegian Directorate for Health Affairs gave permission to use patient information.
Results
Relative prevalence and diagnostic differences
We identified 73 759 events, 11 976 at the casualty clinic and 61 783 at rGP surgeries. A diagnosis from the chapter P of ICPC-2 was given in 2.2% (n = 265) of events at the casualty clinic and 8.8% (n = 5416) of events at the surgeries (χ2(1) = 607.22, p < 0.001). Table I gives frequencies of total events and events with a diagnosis from chapter P for the casualty clinic and surgeries by out-of-office events, gender, and age. When a psychiatric diagnosis was given, this was more likely to be at an out-of-office event, both at the casualty clinic (χ2(1) = 29.74, p < 0.001) and rGP surgeries (χ2(1) = 80.80, p < 0.001). At the casualty clinic men accounted for a high proportion of events with a psychiatric diagnosis.
Table I.
Out-of-office events, gender, and age for all events and events with a first diagnosis from chapter P of ICPC-2 at the casualty clinic and the rGP surgeries.
| Out-of-office events |
Men |
Age |
||||
| n | % | n | % | mean | SD | |
| Total events | ||||||
| Casualty clinic, n = 11,976 | 292 | 2.4 | 5518 | 46.1 | 33 | 25 |
| rGP surgeries, n = 61,783 | 1131 | 1.8 | 26,303 | 42.6 | 48 | 24 |
| Events with first diagnosis from chapter P | ||||||
| Casualty clinic, n = 265 | 20 | 7.5 | 171 | 64.5 | 38 | 18 |
| rGP surgeries, n = 5416 | 184 | 3.4 | 2471 | 45.6 | 45 | 19 |
At the casualty clinic 24 of 43 possible diagnoses in the chapter P were used, while at rGP surgeries nearly all diagnoses were used (41/43). A larger proportion of the psychiatric diagnoses given at the surgeries were from the 17 disease-specific diagnoses (61.4%, n = 3325), compared with at the casualty clinic (46.8%, n = 124) (χ2(1) = 22.55, p < 0.001). Although total number of events with a psychiatric diagnosis at the casualty clinic corresponded to a twentieth of total psychiatric events at the surgeries, some diagnoses were given more frequently at the casualty clinic. P16 (acute alcohol abuse) was the second most common single diagnosis at the casualty clinic (n = 38, 14.3%), but was hardly used at rGP surgeries (n = 5, 0.1%) (χ2(1) = 682.69, p < 0.001). P77 (suicide and suicide attempt) was used in eight events at the casualty clinic (3.0%) and two events at the surgeries (0.0%) (χ2(1) = 127.85, p < 0.001). P98 (psychosis not otherwise specified) was used in 11 events at the casualty clinic (4.2%) and five events at the surgeries (0.1%) (χ2(1) = 149.18, p < 0.001). In the same manner the relative distribution of clustered subgroups of psychiatric diagnoses differed between the casualty clinic and rGP surgeries, with a significantly higher proportion of diagnoses involving either suicidal behaviour, substance abuse, or psychosis at the casualty clinic (Table II) compared with at the surgeries. Diagnoses describing behavioural problems were not used at the casualty clinic, but accounted for 7.6% (n = 414) of diagnoses given at the surgeries.
Table II.
Subgroups of psychiatric diagnoses (ICPC-2 P-diagnoses) at the casualty clinic (n = 265) and the rGP surgeries (n = 5 799).1
| Casualty clinic |
rGP surgeries |
|||||
| Diagnostic subgroups | n | % | n | % | RR | p-value |
| Substance abuse | 62 | 23.4 | 627 | 11.6 | 2.0 | < 0.001 |
| Depression | 55 | 20.8 | 1759 | 32.5 | 0.6 | < 0.001 |
| Anxiety | 42 | 15.8 | 704 | 13.0 | 1.2 | 0.18 |
| Acute stress reaction | 29 | 10.9 | 446 | 8.2 | 1.3 | 0.12 |
| Unspecified P-diagnoses | 29 | 10.9 | 735 | 13.6 | 0.8 | 0.22 |
| Psychosis | 21 | 7.9 | 169 | 3.1 | 2.5 | < 0.001 |
| Sleep disturbance | 12 | 4.5 | 314 | 5.8 | 0.8 | 0.39 |
| Suicidal behaviour | 8 | 3.0 | 2 | 0.0 | 81.8 | < 0.001 |
| Memory disturbance | 5 | 2.0 | 243 | 4.5 | 0.4 | 0.04 |
| Others | 2 | 0.8 | 417 | 7.7 | 0.1 | < 0.001 |
| Total | 265 | 100 | 5416 | 100 | ||
Note: 1Relative risk (RR) denotes the ratio of percentage diagnosis at the casualty clinic to rGP surgeries. Pearson's chi-squared test was used for statistical analysis of each subgroup.
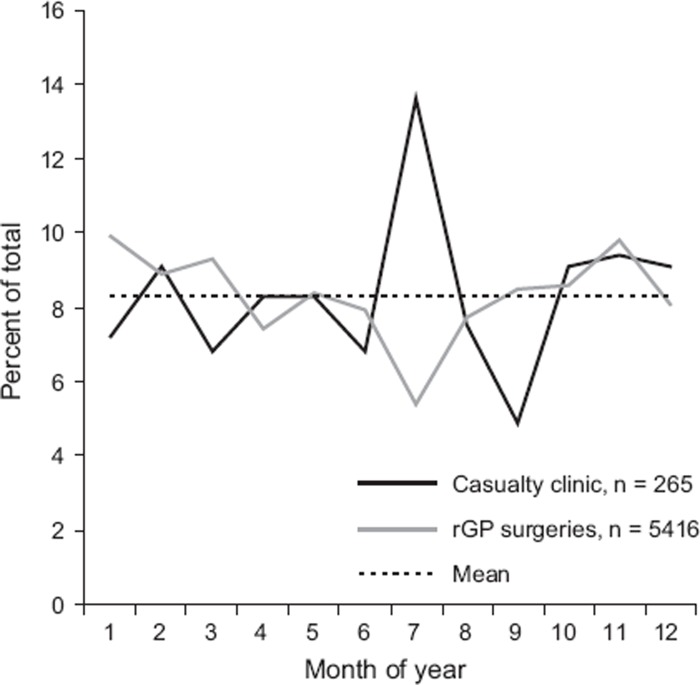
Events with psychiatric diagnoses were not evenly distributed over the year (χ2(11) = 38.63, p < 0.001) (Figure 1). Most visits to the casualty clinic were in July. There was a negative correlation between number of events at the casualty clinic and the surgeries (r = –0.59, p = 0.05).
Figure 1.
Distribution by months of the year of events given a P-diagnosis as first diagnosis at the casualty clinic and the rGP surgeries.
Parallel use of daytime and out-of-hours services
There were 7 304 separate individuals using the casualty clinic and 15,842 using rGP surgeries. Table III gives median number of events per individual, proportion of men and proportion of patients who could be traced as contacting both services. Pooling across diagnoses, use of both services was found for 3 525 patients, which equals 66.0% of individuals who attended the casualty clinic and 22.3% of individuals who attended the surgeries. There was a negative correlation between number of visits to the casualty clinic and number of visits to the surgeries (rs = –0.32, p < 0.001).
Table III.
Total number of individual patients, median number of events per individual, proportion of men, and number of individuals with complete information on personal identity numbers at the casualty clinic and the rGP surgeries respectively.
| Total |
No. of events |
Men |
Complete identity numbers |
||||
| n | median | range | n | % | n | % | |
| Unique individuals | |||||||
| Casualty clinic | 7304 | 1 | 1–27 | 3370 | 46.1 | 5338 | 73.1 |
| rGP surgeries | 15842 | 2 | 1–172 | 7165 | 45.2 | 15721 | 99.2 |
| Individuals with at least one psychiatric diagnosis | |||||||
| Casualty clinic | 179 | 2 | 1–15 | 100 | 55.9 | 154 | 86.0 |
| rGP surgeries | 1808 | 5 | 1–171 | 810 | 44.8 | 1803 | 99.7 |
Of 154 individual casualty clinic patients with at least one psychiatric diagnosis and computer codes that allowed records from different services to be cross-linked, 114 had also been in contact with their rGP. The patients not retrieved in the data files from the rGP surgeries (n = 40) included 32 individuals residing in the municipality where one surgery refused to participate in the study. These individuals could therefore have contacted a GP at this surgery without us knowing it. Of the 114 individuals with established parallel use of the services, 82 had been given at least one psychiatric diagnosis at the rGP surgery. Their median number of events at the rGP surgery was three (range 1–52). There was a small correlation between number of visits to the casualty clinic and number of visits to rGP surgeries (rs = 0.28, p < 0.001). More than half of individuals with psychiatric diagnoses were men (see Table III).
Of 1 803 individual surgery patients with at least one psychiatric diagnosis and cross-linkable codes, 506 (28%) had been in contact with the casualty clinic. The median number of events at the clinic was one (range 1–15). There was a small correlation between visits to the rGP surgeries and the casualty clinic (rs = 0.20, p < 0.001). In their contact with the casualty clinic, the patients had most frequently been given diagnoses related to the respiratory system (21.3%), psychiatry (16.2%), the musculoskeletal system (15.3%), and the digestive system (13.6%).
Discussion
As far as we know, this is the first comparison of a defined population's use of daytime rGP appointments versus out-of-hours casualty clinic contacts in relation to mental illness. The study showed differences in relative prevalence and the spectrum of psychiatric diagnoses given at the casualty clinic and the rGP surgeries. At the level of individual patients, it showed parallel use of the two services.
As a group, psychiatric diagnoses were relatively less prevalent at the casualty clinic than at rGP surgeries. Despite a relatively small study population, and despite focusing on first diagnosis, which could underestimate actual prevalence, our findings compare well with previously reported numbers from studies looking at casualty clinics and surgeries separately [7–11,15]. Psychiatric diagnoses represented a larger proportion of diagnoses used in out-of-office events compared with consultations at both the casualty clinic and the rGP surgeries. This might imply that GPs still decide to see psychiatric patients in their homes, although the GPs make fewer home visits than some years ago [18].
The higher absolute frequency of the diagnoses for suicidal behaviour, acute alcohol abuse, and unspecified psychosis at the casualty clinic compared with rGP surgeries suggests that psychiatric conditions seen out-of-hours are more serious than psychiatric conditions seen during the daytime. Since the doctors on call were mostly rGPs, the data most likely reflect a real difference in the problems the patients presented and not a difference between GPs in diagnostic preferences or use of ICPC diagnoses. The higher presentation rate for serious mental illness out-of-hours raises the issue of whether these conditions are adequately handled by rGPs in their daytime practice. Are rGPs accessible in situations of acute crisis? Are signs of severe mental illness detected and acted upon? Or do the patients need to contact out-of-hours services to receive the required help?
The higher absolute frequency of acute alcohol abuse (P16) is striking. Often substance misuse remains undetected in daytime practice [19], even if it has implications for the general health of the patient. Information from visits to the casualty clinic might therefore be helpful for rGPs in their work with individual patients.
The peak in casualty clinic attendance in July and the negative correlation between number of monthly events at the surgeries and the casualty clinic suggest the casualty clinic is needed as a complementary service for psychiatric patients. This impression is strengthened by the finding that most individuals given a psychiatric diagnosis at the casualty clinic also used daytime medical services.
The parallel use at an individual level could be somewhat underestimated in our study due to the proportion of non-cross-linkable assigned codes at the casualty clinic. However, this does not affect our main conclusion concerning patients with a psychiatric diagnosis at the casualty clinic. The level of concurrent use for individuals with a psychiatric diagnosis at the rGP surgeries is more uncertain. Still, our data suggest that only a subgroup of patients with a psychiatric diagnosis at the rGP surgeries used the casualty clinic. This cautions interpretation of earlier findings from international studies in the context of emergency medical care, which have concluded that psychiatric patients in general put an increased demand on emergency medical services [12–14].
Men were over-represented among patients with psychiatric diagnoses at the casualty clinic, when focusing both on events and on individual patients. A slight over-representation of men has previously been reported in acute psychiatric admissions from a casualty clinic [20], although not in acute psychiatric admissions in general [16,21]. Contrasted with the established pattern that females dominate use of daytime medical services [7,22], this over-representation could reflect gender differences in help-seeking behaviour [23].
In conclusion, GPs should be prepared for more serious diagnostic challenges in psychiatry when they work out-of-hours compared with daytime practice. We need to explore why this is the case. Further research is therefore required to establish the appropriateness and quality of psychiatric primary care both in and out-of-hours, and attention should be given to possible gender differences in services needed.
Acknowledgements
The project was funded by the National Centre for Emergency Primary Health Care, Uni Health, Bergen. IHJ had a research grant from the Norwegian Medical Association's fund for Research in General Practice.
Conflict of interest
None.
References
- 1.Nieber T, Hansen EH, Bondevik GT, Hunskår S, Blinkenberg J, Thesen J, et al. Organisering av legevakt (Organization of Norwegian out-of-hours primary health care services English version) Tidsskr Nor Laegeforen. 2007;127:1335–8. [PubMed] [Google Scholar]
- 2.Hansen EH, Hunskaar S. Development, implementation, and pilot study of a sentinel network (“The Watchtowers”) for monitoring emergency primary health care activity in Norway. BMC Health Serv Res. 2008;8:62. doi: 10.1186/1472-6963-8-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldberg D. Epidemiology of mental disorders in primary care settings. Epidemiol Rev. 1995;17:182–90. doi: 10.1093/oxfordjournals.epirev.a036174. [DOI] [PubMed] [Google Scholar]
- 4.Munk-Jorgensen P, Fink P, Brevik JI, Dalgard OS, Engberg M, Hansson L, et al. Psychiatric morbidity in primary public health care: A multicentre investigation. Part II. Hidden morbidity and choice of treatment. Acta Psychiatr Scand. 1997;95:6–12. doi: 10.1111/j.1600-0447.1997.tb00366.x. [DOI] [PubMed] [Google Scholar]
- 5.Forskrift om fastlegeordning i kommunene (Regulation relating to a municipal regular GP scheme. English version) 14.04.2000 No. 328. Available at: http://www.ub.uio.no/cgi-bin/ujur/ulov/sok.cgi?type = FORSKRIFT (accessed 9 June 2009)
- 6.Kommunehelsetjenesteloven (Act relating to the municipal health services. English version) 19.11.1982 No. 66. Available at: http://www.ub.uio.no/cgi-bin/ujur/ulov/sok.cgi?type = LOV (accessed 9 June 2009)
- 7.Nossen JP Hva foregår på legekontorene? Consultation statistics for 2006) Oslo: Norwegian Labour and Welfare Administration; 2007. Konsultasjonsstatistikk for 2006 (What happens at the GPs’ surgeries? Report No. 4/2007. [Google Scholar]
- 8.Grimsmo A, Hagman E, Faiko E, Matthiessen L, Njalsson T. Patients, diagnoses and processes in general practice in the Nordic countries: An attempt to make data from computerised medical records available for comparable statistics. Scand J Prim Health Care. 2001;19:76–82. doi: 10.1080/028134301750235277. [DOI] [PubMed] [Google Scholar]
- 9.Iveland E, Straand J. 337 sykebesøk på dagtid fra Oslo Legevakt (337 home calls during daytime from the emergency medical centre in Oslo) Tidsskr Nor Laegeforen. 2004;124:354–7. [PubMed] [Google Scholar]
- 10.Straand J, Sandvik H. Home visits in general practice – most often for elderly patients: A report from the Møre & Romsdal Prescription Study. Nor J Epidemiol. 1998;8:127–32. [Google Scholar]
- 11.Brøyn N, Lunde ES, Kvalstad I SEDA – Sentrale data fra allmennlegetjenesten 2004–2006. New statistics from the GPs’ services?) Oslo-Kongsvinger: Statistics Norway; 2007. Ny statistikk fra allmennlegetjenesten? (SEDA – Central information from the general practitioners’ services 2004–2006. Report No. 15/2007. [Google Scholar]
- 12.Kne T, Young R, Spillane L. Frequent ED users: Patterns of use over time. Am J Emerg Med. 1998;16:648–52. doi: 10.1016/s0735-6757(98)90166-8. [DOI] [PubMed] [Google Scholar]
- 13.Curran GM, Sullivan G, Williams K, Han X, Allee E, Kotrla KJ. The association of psychiatric comorbidity and use of the emergency department among persons with substance use disorders: An observational cohort study. BMC Emerg Med. 2008;8:17. doi: 10.1186/1471-227X-8-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kennedy D, Ardagh M. Frequent attenders at Christchurch Hospital's Emergency Department: A 4-year study of attendance patterns. N Z Med J. 2004;117:U871. [PubMed] [Google Scholar]
- 15.Johansen IH, Morken T, Hunskaar S. Contacts related to psychiatry and substance abuse in Norwegian casualty clinics: A cross-sectional study. Scand J Prim Health Care. 2009;27:180–5. doi: 10.1080/02813430903075473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ruud T, Gråwe RW, Hatling T. Supported by the Norwegian Directorate of Health. Oslo: SINTEF; 2006. Akuttpsykiatrisk behandling i Norge – resultater fra en multisenterstudie (Emergency psychiatric treatment in Norway – results from a multicentre study). Report No. A310/2006. [Google Scholar]
- 17.International Classification of Primary Care. Available at: http://www.kith.no/templates/kith_WebPage____1186.aspx (accessed 20 November 2006)
- 18.Halvorsen I, Meland E, Bærheim A. Bruk av legevakt før og etter fastlegeordningen (Use of out-of-hours services before and after introduction of a patient list system. English version) Tidsskr Nor Laegeforen. 2007;127:15–17. [PubMed] [Google Scholar]
- 19.Aasland OG, Bruusgaard D, Rutle O. Alcohol problems in general practice. Br J Addict. 1987;82:197–201. doi: 10.1111/j.1360-0443.1987.tb01461.x. [DOI] [PubMed] [Google Scholar]
- 20.Deraas TS, Hansen V, Giaever A, Olstad R. Acute psychiatric admissions from an out-of-hours casualty clinic: How do referring doctors and admitting specialists agree? BMC Health Serv Res. 2006;6:41. doi: 10.1186/1472-6963-6-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tørrissen T. Tvangsinnleggelser i en akuttpsykiatrisk post (Involuntary admissions to an acute psychiatric ward. English version) Tidsskr Nor Laegeforen. 2007;127:2086–9. [PubMed] [Google Scholar]
- 22.Backman AS, Blomqvist P, Lagerlund M, Carlsson-Holm E, Adami J. Characteristics of non-urgent patients: Cross-sectional study of emergency department and primary care patients. Scand J Prim Health Care. 2008;26:181–7. doi: 10.1080/02813430802095838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Myrvold TM. Oslo: Norwegian Institute for Urban and Regional Research; 2008. Psykisk helse og psykisk sykdom: Innbyggernes kunnskaper og holdninger (Mental health and psychiatric disorders: Openness, knowledge and attitudes. English summary). Report No. 16/2008. [Google Scholar]