Abstract
Background
Black Americans with depression were less likely to receive electroconvulsive therapy (ECT) than whites during the 1970’s and 80’s. This pattern was commonly attributed to treatment of blacks in lower quality hospitals where ECT was unavailable. We investigated whether a racial difference in receiving ECT persists, and, if so, whether it arises from lesser ECT availability or from lesser ECT use within hospitals conducting the procedure.
Methods
Black or white inpatient stays for recurrent major depression from 1993-2007 (N=419,686) were drawn from an annual sample of US community hospital discharges. The marginal disparity ratio estimated adjusted racial differences in the probabilities of (1) admission to a hospital capable of conducting ECT (availability), and (2) ECT utilization if treated where ECT is conducted (use).
Results
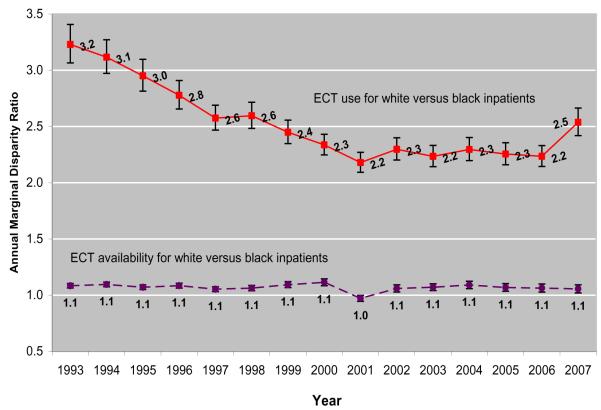
Across all hospitals, the probability of receiving ECT for depressed white inpatients (7.0%) greatly exceeded that for blacks (2.0%). Probability of ECT availability was slightly greater for whites than blacks (62.0% versus 57.8%), while probability of use was markedly greater (11.8% versus 3.9%). The white versus black marginal disparity ratio for ECT availability was 1.07 (95% confidence interval 1.06-1.07) and stable over the period, while the ratio for use fell from 3.2 (3.1-3.4) to 2.5 (2.4-2.7).
Limitations
Depressed persons treated in outpatient settings or who receive no care are excluded from analyses.
Conclusions
Depressed black inpatients continue to be far less likely than whites to receive ECT. The difference arises almost entirely from lesser use of ECT within hospitals where it is available.
Keywords: recurrent major depression, electroconvulsive therapy (ECT), racial disparities
INTRODUCTION
Black Americans with depression are less likely to receive care than their white counterparts (Gonzalez et al., 2010, Roy-Byrne et al., 2009). When depressed blacks do receive outpatient treatment, it is typically less intensive(Gonzalez et al., 2010, Olfson et al., 2009, Sue et al., 1994), of lower quality(Young et al., 2001), and less commonly provided by specialists.(Young et al., 2001) Little is known about whether comparable racial differences exist in the treatment of severe, chronic depressive illness, which is more likely than milder or transient depression to prompt recognition and treatment seeking(Kessler et al., 2003) and which may have the most dire health consequences. Further, almost nothing known about the causes of observed racial differences in depression care, which might arise from differences in access to high quality providers, in reimbursement practices, symptomatic presentation of depressive psychopathology(Wohi et al., 1997), health literacy, cultural values(Mojtabai, 2009), or provider bias.
One productive approach to documenting and understanding disparities in the care of severe medical illness is examining whether racial variation in hospital quality explains observed differences in treatment use and health outcomes. For example, studies have show that lesser black admissions to high quality cardiac and pulmonary care hospital units, rather than inferior treatment of blacks within these facilities, explains much of the racial differences observed in treatment of valvular disease, lung cancer, and myocardial infarction.(Neighbors et al., 2007, Popescu et al., 2011, Schelbert et al., 2005).
No comparable research on depression treatment has yet been conducted, but one promising opportunity for study is racial variation in the availability and use of electroconvulsive therapy (ECT). ECT availability is an objective and important measure of the quality of hospital care for depressed inpatients. ECT is the treatment of choice for treatment-resistant depression and depressive episodes with psychotic features, catatonia, severe suicidality, or food refusal with nutritional compromise(American Psychiatric Association, 2001). ECT is also widely regarded as the most efficacious treatment for major depressive disorder (Pagnin et al., 2004) and is no less effective in blacks than whites.(Williams et al., 2008). Further, ECT requires specialized equipment and personnel and is unavailable at many hospitals.(Hermann et al., 1995). Racial differences in the availability of ECT to depressed inpatients would provide a clear indication of racial differences in the quality of hospital care. In addition, research on receipt of ECT would allow for the first time an understanding of whether racial variation in the quality of treating hospitals explains some or all of observed racial differences in depression care.
Data from the 1970’s through the early 1990’s indicate that depressed black inpatients were a third to a tenth as likely as whites to receive ECT. (Breakey and Dunn, 2004, Kramer, 1985, 1990, 1999, Morrissey et al., 1981, Olfson et al., 1998, Thompson et al., 1994) Contemporary speculation about the cause of this difference largely focused on de facto racial segregation of black Americans into lower quality hospitals.(Asnis et al., 1978, Bailine and Rau, 1981, Kramer, 1990) This inference was supported indirectly by data demonstrating that psychiatric treatment of blacks has been disproportionately conducted in public facilities(Milazzo-Sayre et al., 2000), and that ECT availability was substantially lower in public than private hospitals during the period.(Asnis et al., 1978, Hermann et al., 1998, Kramer, 1990, Mills et al., 1984, Reid et al., 1998, Thompson et al., 1994) Despite these suggestive findings, the influence of hospital ECT availability on racial patterns in care has never been examined and no recent national data on racial differences in receipt of ECT exist. Further, a study from one hospital reported that the odds of receiving ECT for affective illness for whites was almost three times that of blacks, indicating large racial differences may exist even within hospitals offering the procedure.(Breakey and Dunn, 2004).
We now examine national trends in racial differences in the availability and use of inpatient ECT for recurrent major depressive disorder using data from a large, representative hospital sample over a fifteen-year period from 1993 to 2007. We test hypotheses regarding two putative sources of racial difference in receipt of ECT: 1) depressed black inpatients are less likely than whites to be treated in hospitals capable of conducting ECT, and 2) black inpatients experience lower use of ECT within facilities capable of conducting the procedure. We employ rigorous methods drawn from the growing health disparities literature(Duan et al., 2008) to adjust racial comparisons for clinical, socio-demographic, and hospital characteristics and to explore potential moderators of potential racial differences.
METHOD
Data Source
We analyzed data for the years 1993 to 2007 from the Nationwide Inpatient Sample (NIS) of the Healthcare Cost and Utilization Project, a nationally representative survey of US community hospitals conducted by the Agency for Healthcare Research and Quality (AHRQ). Community hospitals are designated annually as nonfederal, short-term, general, or specialty hospitals, including public hospitals and academic medical centers.(2002) Excluded from the survey are freestanding psychiatric and chemical dependency facilities, long-term hospitals, hospital units of institutions, and short-term rehabilitation hospitals. Annual NIS databases contain 5-8 million discharge abstracts from approximately 1,000 hospitals, including up to 15 diagnoses and procedures and other clinical, demographic, hospital, and treatment information. The NIS contains a 20% stratified hospital sample, with sampling probabilities proportional to the number of hospitals in each stratum. Following AHRQ recommendations, we examined years following 1992 using designated trend variables and weights.(Whalen et al., 2008)
ECT treatment
We conceptualized ECT treatment as the co-occurrence of two related events: admission to a hospital capable of conducting ECT (“ECT availability”); and, conditional on availability, receiving ECT (“ECT use”). Hospitals were considered to offer ECT if they conducted the procedure (ICD-9-CM code 94.27) during at least one visit in the calendar year.
Subjects
To examine ECT availability, we analyzed stays of black and white inpatients aged ≥18 years with a principal diagnosis of recurrent major depression (ICD-9-CM codes 296.30-.36). We adjusted sampling weights to maintain depression discharge population estimates for each stratum prior to excluding 152,306 discharges lacking race information. This yielded 419,686 sample discharges representing a national estimate of 2,933,646. To examine ECT use, we analyzed the subset of 252,346 sample discharges from hospitals offering ECT, representing an estimated 1,803,488 discharges.
Patient and Hospital Characteristics
Patient characteristics studied included race (derived from specification as black, white, Hispanic, Asian/Pacific Islander, Native American, or other), age, sex, depression severity, admission source, income in the patient’s ZIP code, and primary payer. From secondary diagnoses we also identified suicide attempts (E950-E959), psychiatric comorbidities (290-319), potential medical contraindications to ECT (2000, American Psychiatric Association, 2001) (diagnoses available on request), and general medical comorbidities (medical diagnoses not specified above). Hospital characteristics included census region and urbanicity, size, and teaching status. Patients were assumed to share their treating hospital’s region and urbanicity.
Statistical Analyses
We described patient and hospital characteristic distributions for black and white inpatient visits, omitting statistical contrasts since exceedingly large samples ensured the statistical significance of unimportant differences. We calculated ECT availability rates for all white and black visits and ECT use rates for visits in hospitals offering ECT.
We tested for racial differences in probabilities of ECT availabiltity and use, using the marginal disparity approach to adjust contrasts for differences in other visit characteristics.(Duan et al., 2008) In this approach predictor variables are classified as “allowable” or “non-allowable”. Allowable covariates characterize treatment preference or clinical need, cannot contribute to disparity, and are used to adjust disparity calculation. Non-allowable covariates are excluded from adjustment. We treated as potential measures of clinical need—and therefore allowable—age, sex, depression severity, psychiatric comorbidity, suicide attempt, potential medical contraindication to ECT, general medical comorbidity, admission source, and year. No covariates measured preference. The marginal disparity approach estimates outcome probabilities for black visits under the counterfactual assumption that they have the same allowable covariate distributions as whites. The marginal disparity ratio is the ratio of an outcome probability for white visits over that for counterfactually adjusted black visits.
To estimate marginal disparity ratios, ECT availability and use outcomes were first modeled in logistic regressions. The availability model was fit using all discharges, while the use model was fit using only discharges from hospitals offering ECT. To avoid tautological prediction of ECT availability by other hospital characteristics, we excluded hospital teaching status and size from the availability model. Variable selection began in bivariate models with each allowable and non-allowable covariate; those with coefficients differing from zero at p<.25 were included in a preliminary multivariate model. Backwards stepwise variable removal continued until remaining coefficients differed from zero at p<.05. Subsequently, race interaction terms for each retained predictor were similarly introduced and removed.
From the final models we calculated white versus black adjusted odds ratios (AORs) for significant interactions to examine moderation of race effects. We used published equations to calculate disparity ratios with 95% CIs for access and use from main and interaction effects.(Duan et al., 2008) Probability estimates for whites used the covariate distribution of the white sample; estimates for blacks used the non-allowable covariate distribution of the black sample and allowable covariate distribution of the whites.
We reported additional analyses to facilitate comparison with earlier studies: the unadjusted white versus black OR of ECT treatment across all hospitals; and for availability and use, the unadjusted OR of the race effect and the adjusted odds ratio of from the multivariate models prior to addition of race interaction terms. When reporting marginal disparity ratios for the period, we presented corresponding marginal ORs.
To explore whether lesser black ECT availability could be mitigated by transfers to hospitals outside the sample offering ECT, we compared white and black transfer rates from facilities not offering ECT.
Analyses were conducted using SAS 9.2 software.
Ethical Considerations
Analyses were conducted exclusively with publicly available, de-identified data, and were deemed not to be human subjects research by the Director of the Institutional Review Board of the Nathan Kline Institute for Psychiatric Research.
RESULTS
ECT Treatment across All Hospitals
Among depressed inpatients in all hospitals, 7.0% (95% CI 6.4-7.7) of white visits and 2.0% (1.6-2.4) of black visits received ECT, and the unadjusted white versus black OR of ECT treatment was 3.4 (2.8-4.1).
ECT Availability
ECT availability rates among white and black depressed inpatients were 62.0% (95% CI 60.5-63.5) and 57.8% (56.3-59.4), respectively. Characteristics predicting availability are presented in Table 1.
Table 1.
Characteristics and ECT availability rates of white and black inpatient stays for recurrent major depression in US community hospitals, by significant predictors of ECT availability
| % of patients with characteristic, by race |
Rate of ECT availability in %, by race |
|||
|---|---|---|---|---|
| Characteristic | white1 | black2 | white1 | black2 |
| All inpatient visits | 86.8 | 13.2 | 62.0 | 57.8 |
| Patient Characteristics | ||||
| Age, in years | ||||
| 18-34 | 25.2 | 32.4 | 58.6 | 55.6 |
| 35-44 | 25.1 | 34.6 | 62.0 | 58.5 |
| 45-54 | 19.9 | 20.8 | 60.9 | 57.3 |
| 55-64 | 9.7 | 6.1 | 61.2 | 59.7 |
| 65-74 | 9.0 | 3.5 | 66.6 | 64.8 |
| 75 and older | 11.1 | 2.6 | 68.7 | 67.6 |
| Potential medical contraindication to ECT | ||||
| No | 78.0 | 82.0 | 61.5 | 57.4 |
| Yes | 22.0 | 18.0 | 63.9 | 59.7 |
| Median household income in patient ZIP code† | ||||
| 0-25th percentile | 26.3 | 50.5 | 51.8 | 56.5 |
| 26th-50th percentile | 27.1 | 24.1 | 61.8 | 60.3 |
| 51st-75th percentile | 23.2 | 14.5 | 66.4 | 58.2 |
| 76th-100th percentile | 23.3 | 10.9 | 69.5 | 58.3 |
| Primary Payer | ||||
| Self pay or other | 11.7 | 15.6 | 48.9 | 43.6 |
| Medicaid | 17.5 | 39.1 | 53.8 | 56.6 |
| Medicare | 34.4 | 23.5 | 65.2 | 63.5 |
| Private | 36.4 | 21.9 | 67.2 | 64.1 |
| Hospital Characteristics | ||||
| Region† | ||||
| West | 11.9 | 9.3 | 46.1 | 35.8 |
| South | 33.8 | 46.6 | 57.0 | 49.2 |
| Northeast | 22.9 | 19.3 | 65.0 | 60.8 |
| Midwest | 31.4 | 24.8 | 71.3 | 80.1 |
| Urbanicity† | ||||
| Rural | 14.5 | 7.0 | 27.7 | 20.3 |
| Urban | 85.5 | 93.0 | 67.9 | 60.7 |
Unweighted sample of n=362,785 discharges.
Unweighted sample of n=56,901 discharges.
Variable signficantly interacted with race to predict ECT availability; see Table 3 for white versus black odds ratios of interaction contrasts from the model. Results based on HCUP-NIS weighted sampling of a total of 419,686 discharges of inpatients aged ≥18 with a principal ICD-9-CM diagnosis 296.3x, representing a weighted total of 2,933,646 discharges. ECT availability defined as treatment in a hospital where at least one inpatient received ECT during the calendar year. See text for variable definitions.
Depressed black inpatients in US community hospitals were younger, from poorer neighborhoods, and were more likely to be uninsured or covered by Medicaid and to be treated in the South, characteristics associated with lower ECT availability rates. Blacks were also more likely to be urban, a characteristic associated with greater availability.
Median household income, region, and urbanicity significantly moderated the association between race and availability (Supplemental Table 1). Higher median income and, to a lesser extent, rural location were associated with larger white versus black AORs for ECT availability, indicating greater racial differences in wealthier and rural neighborhoods. For inpatients treated in the Northeast, South, and West, availability probabilities trended higher for whites than blacks; AORs ranged from 1.0 for low-income, urban Northeastern patients to 1.7 for high income, rural Western patients. Midwestern blacks experienced a trend towards greater ECT availability than whites; AORs ranged from 0.6 in low income, urban neighborhoods to 0.9 in high income, rural settings.
Annual white versus black marginal disparity ratios of ECT availability are presented below in Figure 1. White inpatients experienced minimally greater availability than clinically comparable blacks throughout the 15 year period, with an overall marginal disparity ratio of 1.07 (1.06-1.07, equivalent to a marginal odds ratio of 1.17).
Figure.
Annual marginal disparity ratios of ECT availability and use for white versus black inpatients treated for recurrent major depression in US community hospitals, 1993-2007
Marginal disparity ratios calculated using terms from logistic models of ECT access and use. See text for specification of allowable and non-allowable covariates and Tables 1 and 3 for variables included in the models. Above 1, higher ratios indicate greater racial differences. All adjusted risk ratios signficantly different from 1 at p<.05 except for access in 2001. Results based on HCUP-NIS weighted sampling of 480,463 discharges of inpatients aged 18 and older with a principal ICD-9-CM diagnosis 296.3x. ECT availability defined as treatment in a hospital where at least one inpatient received ECT during the calendar year.
The black rate of transfer from hospitals not offering ECT (8.8%) did not exceed the white rate (12.2%). Additional calculations to facilitate comparison with prior studies were as follows: the unadjusted OR for ECT availability was 1.2 (0.9-1.5), while the AOR from the multivariate logistic model excluding interaction terms was 1.1 (0.9-1.4).
ECT Use
ECT use in hospitals offering the procedure was far higher for whites (11.8%, 95% CI 8.4-14.0) than blacks (3.9%, 3.1-4.6), reflecting conduct of ECT during an estimated 187,000 and 8,500 stays of depressed white and black inpatients, respectively. Characteristics predicting use are presented in Table 2.
Table 2.
Characteristics and ECT use rates of white and black inpatients stays for recurrent major depression in US community hospitals that offer ECT, by significant predictors of ECT
| % of patients with characteristic, by race |
Rate of ECT use in %, by race |
|||
|---|---|---|---|---|
| Characteristic | white1 | black2 | white1 | black2 |
| All inpatient visits | 87.7 | 12.3 | 11.8 | 3.9 |
| Patient Characteristics | ||||
| Age, in years† | ||||
| 18-34 | 23.8 | 30.7 | 4.6 | 1.8 |
| 35-44 | 25.2 | 35.3 | 8.1 | 2.5 |
| 45-54 | 19.7 | 20.8 | 10.2 | 4.5 |
| 55-64 | 9.5 | 6.2 | 14.0 | 6.6 |
| 65-74 | 9.6 | 3.9 | 23.4 | 12.4 |
| 75 and older | 12.2 | 3.0 | 25.6 | 20.2 |
| Sex† | ||||
| Male | 34.0 | 39.2 | 10.8 | 2.7 |
| Female | 66.0 | 60.8 | 12.4 | 4.6 |
| Depression episode severity | ||||
| Moderate, mild, or in remission | 7.1 | 5.5 | 5.4 | 2.4 |
| Unspecified | 31.2 | 31.2 | 9.8 | 2.9 |
| Severe without psychotic features | 42.5 | 30.9 | 12.5 | 3.8 |
| Severe with psychotic features | 19.2 | 32.4 | 16.1 | 5.0 |
| Suicide attempt | ||||
| No | 94.9 | 96.3 | 12.2 | 3.9 |
| Yes | 5.1 | 3.7 | 5.1 | 2.0 |
| Psychiatric comorbidity | ||||
| No | 20.4 | 18.4 | 16.5 | 5.1 |
| Yes | 79.6 | 81.6 | 10.6 | 3.6 |
| Potential medical contraindication to ECT | ||||
| No | 22.8 | 18.7 | 11.0 | 3.7 |
| Yes | 77.3 | 81.3 | 14.6 | 4.8 |
| Admission source | ||||
| Emergency department | 38.2 | 51.1 | 6.7 | 2.4 |
| Other hospital or facility | 9.9 | 8.6 | 10.5 | 4.1 |
| Routine | 51.8 | 40.3 | 15.9 | 5.7 |
| Primary Payer | ||||
| Self pay or other | 9.1 | 11.4 | 4.7 | 1.5 |
| Medicaid | 15.2 | 38.6 | 5.5 | 2.1 |
| Medicare | 36.0 | 25.7 | 18.3 | 7.3 |
| Private | 39.6 | 24.3 | 10.0 | 4.2 |
| Hospital Characteristics | ||||
| Region† | ||||
| West | 8.8 | 5.8 | 9.7 | 4.1 |
| Northeast | 24.1 | 20.6 | 13.2 | 3.1 |
| South | 30.9 | 40.1 | 10.3 | 3.7 |
| Midwest | 36.2 | 33.5 | 12.7 | 4.5 |
| Urbanicity† | ||||
| Rural | 6.1 | 2.5 | 12.4 | 5.6 |
| Urban | 93.9 | 97.5 | 11.8 | 3.8 |
Unweighted sample of n=225,526 discharges.
Unweighted sample of n=26,820 discharges.
Variable signficantly interacted with race to predict ECT access; see Table 4 for white versus black odds ratios of interaction contrasts from the model. Results based on HCUP-NIS weighted sampling of a total of 252,346 discharges of inpatients aged ≥18 with a principal ICD-9-CM diagnosis 296.3x, representing an estimated 1,803,488 discharges. Hospitals offering ECT defined as those which performed ECT at least once during the calendar year. See text for variable definitions.
Compared to whites, depressed black inpatients in hospitals offering ECT were younger, were more likely to be male, to have been admitted through the emergency department, to be uninsured or covered by Medicaid, and to be treated in the Southern and urban hospitals, characteristics associated with lower use rates. Blacks were also more likely to be diagnosed with severe depression with psychotic features, a characteristic associated with greater use.
Patient age and sex and hospital region and urbanicity significantly moderated the association between race and odds of ECT use (Supplemental Table 2). Racial differences were smaller in older patients. Male sex, Northeast region, and urban location were associated with greater racial treatment differences. AORs of use ranged from 5.0 in 35-44 year old men treated in urban, Northeastern hospitals to 0.7 in women aged ≥75 years treated in rural, Southern hospitals.
Annual white versus black marginal disparity ratios for ECT use are presented in Figure 1.
Ratios fell from 3.2 (3.1-3.4) in 1993 to 2.3 (2.3-2.4) in 2000, remained stable through 2006, and rose to 2.5 (2.4-2.7) in 2007. A marginal disparity ratio of 2.5 (2.4-2.6, equivalent to a marginal odds ratio of 2.7) was observed for the period. Because treatment year was not retained in the final model, disparity trends reflected underlying relative decline among whites of two characteristics predicting high probability of ECT use: older age and routine admission source.
The unadjusted OR for ECT use was 3.3 (2.8-3.9), while AOR from a model excluding interaction terms was 2.2 (1.9-2.6).
DISCUSSION
We found that marked racial differences in receipt of inpatient ECT for recurrent major depression have persisted over the past 15 years. These differences do not arise, as has been speculated, from de facto racial segregation African Americans into hospitals incapable of providing ECT, but rather from lower use of ECT by black than white inpatients in hospitals where the procedure is conducted. Our findings are reassuring insofar as they preclude one ethically noxious source of racial disparity and suggest equity in an important measure of the quality of hospital care for depression, but they nonetheless provoke concerning questions about the persisting role of race in shaping depression care. Despite declining during the 1990s, the effect of race on use of ECT remains large, comparable to that of important clinical indications such as illness severity, and cannot be explained by racial variation in our measures of depression severity, comorbidity, payer type, or a number of other patient and hospital characteristics. These treatment differences occur against a scientific background of mounting evidence for ECT’s superior efficacy(Pagnin et al., 2004) and distinctive role in severe depression.(2000, Fochtmann and Gelenberg, 2005)
If availability does not explain racial differences in receipt of inpatient ECT, what does? Unmeasured racial differences in prior treatment, illness presentation, or provider characteristics may have contributed to the patterns we observed. Even severely depressed black inpatients may be less likely than whites with comparable diagnoses to be perceived as ECT candidates since depressed blacks tend to have histories of less extensive(Olfson et al., 2009, Roy-Byrne et al., 2009, Sue et al., 1994, Sussman et al., 1987) and clinically appropriate(Young et al., 2001) depression treatment. The decline in race effects we observed with increasing patient age— similar to that reported in a prior study(Breakey and Dunn, 2004)—may reflect “catch-up” in the accumulation of treatment histories by older black Americans. However, in our sample black inpatients were almost twice as likely as whites to be diagnosed with psychotic depression, suggesting providers were more likely to perceive symptoms in blacks which promote, rather than discourage, ECT selection. An ECT trial for unipolar depression similarly found higher rates of psychotic symptoms among black (59%) than white (27%) subjects.(Williams et al., 2008)
As in the majority of large studies on racial and ethnic treatment differences, we could not explore whether differences in provider training and attitudes towards ECT(Hermann et al., 1995)—or providers’ racial biases—contributed to our findings. Although we did not have data on the race of providers, a survey of US psychiatrists found that psychiatrist race did not predict whether she or he performed ECT.(Hermann et al., 1998) Racial differences in patient preference for ECT may exist and account for observed treatment differences. In one study of depressed inpatients, those viewing ECT favorably were more likely to receive it, suggesting patient preference influences inpatient ECT use.(Pettinati et al., 1994) No data exist on racial attitudes towards ECT, but black population survey respondents report less willingness than whites to consider medication for hypothetical panic or depressive symptoms and greater concern about treatment risks.(Mojtabai, 2009) Limited data indicate that those who receive ECT develop more positive impressions of the procedure(Kalayam and Steinhart, 1981, Pettinati et al., 1994) and imply that longstanding patterns of inexperience with ECT among black Americans may influence their treatment choices. Disparity research from other fields suggests similar racial patterns in attitudes towards treatment may reflect discrepant information received, driven by differential availability to providers or other racial differences in care quality or volume.(Rich et al., 2009)
Our study has several important limitations. In contrast to some prior studies reporting racial differences in receipt of ECT(Hermann et al., 1998, Kramer, 1985, 1990, 1999), our nationally representative sample excluded freestanding psychiatric facilities. Because black and white use of psychiatric hospitals is comparable(Milazzo-Sayre et al., 2000) and ECT rates in specialty facilities are low(Thompson and Blaine, 1987), their inclusion would have had little impact on our results. Our findings of large regional and urban versus rural effects on ECT availability are consistent with prior work showing extensive geographic variation in ECT availability(Harris, 2006, Hermann et al., 1995), but we could not evaluate some important potential explanations of this variation, such as restrictiveness of state ECT regulations.(Harris, 2006) Lack of health insurance and Medicaid coverage were associated with lower ECT availability and use in our data, but we could not determine the role of managed care on our findings. Because our data excluded depressed persons who were untreated or treated outside inpatient settings, our measures of treatment differences do not account for under-diagnosis of depressive illness in blacks(Neighbors et al., 2003, Snowden, 2003, Strakowski et al., 1996) or racial patterns in use of outpatient ECT. A substantial number of depression discharges were excluded from analysis because they lacked race information, and hospitals’ methods of attributing race were not specified. Finally, we did not examine treatment of other racial / ethnic groups who may experience disparities.(McGuire and Miranda, 2008)
Marked racial differences persist in the treatment of depression with ECT, and our work suggests that efforts are needed to improve equity in care for the most severe, chronic, and disabling depressive illness. Data on racial and ethnic patterns in the information patients receive about depression care and in prior treatment experiences, as well as preferences and attitudes, are critical to understanding and remediating disparities. Refining the conceptualization of disparities to distinguish preferences based on differential community values from poorer quality of medical information or care may further clarify the causes of differences in mental health treatment and reveal new targets for disparity reduction.
Supplementary Material
Acknowledgements
The authors would like to acknowledge helpful editorial commentary by Kenneth B. Wells, M.D., M.P.H, Daniel P. Dickstein, M.D., and Peter D. Friedmann, M.D., M.P.H.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Practice guideline for the treatment of patients with major depressive disorder (revision). American Psychiatric Association. Am J Psychiatry. 2000;157:1–45. [PubMed] [Google Scholar]
- Design of the HCUP Nationwide Inpatient Sample, 2000. Agency for Healthcare Research and Quality; Rockville, Maryland: 2002. [Google Scholar]
- American Psychiatric Association . The Practice of Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging. American Psychiatric Publishing, Inc.; Washington, D.C.: 2001. [Google Scholar]
- Asnis GM, Fink M, Saferstein S. ECT in metropolitan New York hospitals: a survey of practice, 1975-1976. The American journal of psychiatry. 1978;135:479–82. doi: 10.1176/ajp.135.4.479. [DOI] [PubMed] [Google Scholar]
- Bailine SH, Rau JH. The decision to use ECT: a retrospective study. Comprehensive psychiatry. 1981;22:274–81. doi: 10.1016/0010-440x(81)90085-7. [DOI] [PubMed] [Google Scholar]
- Breakey WR, Dunn GJ. Racial disparity in the use of ECT for affective disorders. Am J Psychiatry. 2004;161:1635–41. doi: 10.1176/appi.ajp.161.9.1635. [DOI] [PubMed] [Google Scholar]
- Duan N, Meng XL, Lin JY, Chen CN, Alegria M. Disparities in defining disparities: statistical conceptual frameworks. Stat Med. 2008;27:3941–56. doi: 10.1002/sim.3283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fochtmann l. J., Gelenberg AJ. Guideline Watch: Practice Guideline for the Treatment of Patients With Major Depressive Disorder. 2nd Edition American Psychiatric Association; Arlington, VA: 2005. [Google Scholar]
- Gonzalez HM, Vega WA, Williams DR, Tarraf W, West BT, Neighbors HW. Depression care in the United States: too little for too few. Arch Gen Psychiatry. 2010;67:37–46. doi: 10.1001/archgenpsychiatry.2009.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris V. Electroconvulsive therapy: administrative codes, legislation, and professional recommendations. J Am Acad Psychiatry Law. 2006;34:406–11. [PubMed] [Google Scholar]
- Hermann RC, Dorwart RA, Hoover CW, Brody J. Variation in ECT use in the United States. Am J Psychiatry. 1995;152:869–75. doi: 10.1176/ajp.152.6.869. [DOI] [PubMed] [Google Scholar]
- Hermann RC, Ettner SL, Dorwart RA, Hoover CW, Yeung E. Characteristics of psychiatrists who perform ECT. Am J Psychiatry. 1998;155:889–94. doi: 10.1176/ajp.155.7.889. [DOI] [PubMed] [Google Scholar]
- Kalayam B, Steinhart MJ. A survey of attitudes on the use of electroconvulsive therapy. Hosp Community Psychiatry. 1981;32:185–8. doi: 10.1176/ps.32.3.185. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA : the journal of the American Medical Association. 2003;289:3095–105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kramer BA. Use of ECT in California, 1977-1983. Am J Psychiatry. 1985;142:1190–2. doi: 10.1176/ajp.142.10.1190. [DOI] [PubMed] [Google Scholar]
- Kramer BA. ECT use in the public sector: California. Psychiatr Q. 1990;61:97–103. doi: 10.1007/BF01064910. [DOI] [PubMed] [Google Scholar]
- Kramer BA. Use of ECT in California, revisited: 1984-1994. J Ect. 1999;15:245–51. [PubMed] [Google Scholar]
- McGuire TG, Miranda J. New evidence regarding racial and ethnic disparities in mental health: policy implications. Health Aff (Millwood) 2008;27:393–403. doi: 10.1377/hlthaff.27.2.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milazzo-Sayre LJ, Henderson MJ, Manderscheid RW, Bokossa MC, Evans C, Male AA. Chapter 15: Persons Treated in Specialty Mental Heath Care Programs, United States, 1997. In: Manderscheid RW, Henderson MJ, editors. Mental Health, United States, 2000. Center for Mental Health Services; Washington, DC: 2000. [Google Scholar]
- Mills MJ, Pearsall DT, Yesavage JA, Salzman C. Electroconvulsive therapy in Massachusetts. The American journal of psychiatry. 1984;141:534–8. doi: 10.1176/ajp.141.4.534. [DOI] [PubMed] [Google Scholar]
- Mojtabai R. Americans’ attitudes toward psychiatric medications: 1998-2006. Psychiatr Serv. 2009;60:1015–23. doi: 10.1176/ps.2009.60.8.1015. [DOI] [PubMed] [Google Scholar]
- Morrissey JP, Steadman HJ, Burton NM. A profile of ECT recipients in New York State during 1972 and 1977. Am J Psychiatry. 1981;138:618–22. doi: 10.1176/ajp.138.5.618. [DOI] [PubMed] [Google Scholar]
- Neighbors CJ, Rogers ML, Shenassa ED, Sciamanna CN, Clark MA, Novak SP. Ethnic/racial disparities in hospital procedure volume for lung resection for lung cancer. Medical care. 2007;45:655–63. doi: 10.1097/MLR.0b013e3180326110. [DOI] [PubMed] [Google Scholar]
- Neighbors HW, Trierweiler SJ, Ford BC, Muroff JR. Racial differences in DSM diagnosis using a semi-structured instrument: the importance of clinical judgment in the diagnosis of African Americans. J Health Soc Behav. 2003;44:237–56. [PubMed] [Google Scholar]
- Olfson M, Cherry DK, Lewis-Fernandez R. Racial differences in visit duration of outpatient psychiatric visits. Arch Gen Psychiatry. 2009;66:214–21. doi: 10.1001/archgenpsychiatry.2008.523. [DOI] [PubMed] [Google Scholar]
- Olfson M, Marcus S, Sackeim HA, Thompson J, Pincus HA. Use of ECT for the inpatient treatment of recurrent major depression. Am J Psychiatry. 1998;155:22–9. doi: 10.1176/ajp.155.1.22. [DOI] [PubMed] [Google Scholar]
- Pagnin D, de Queiroz V, Pini S, Cassano GB. Efficacy of ECT in depression: a meta-analytic review. J Ect. 2004;20:13–20. doi: 10.1097/00124509-200403000-00004. [DOI] [PubMed] [Google Scholar]
- Pettinati HM, Tamburello TA, Ruetsch CR, Kaplan FN. Patient attitudes toward electroconvulsive therapy. Psychopharmacol Bull. 1994;30:471–5. [PubMed] [Google Scholar]
- Popescu I, Cram P, Vaughan-Sarrazin MS. Differences in admitting hospital characteristics for black and white medicare beneficiaries with acute myocardial infarction. Circulation. 2011;123:2710–6. doi: 10.1161/CIRCULATIONAHA.110.973628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid WH, Keller S, Leatherman M, Mason M. ECT in Texas: 19 months of mandatory reporting. J Clin Psychiatry. 1998;59:8–13. [PubMed] [Google Scholar]
- Rich SE, Gruber-Baldini AL, Quinn CC, Zimmerman SI. Discussion as a factor in racial disparity in advance directive completion at nursing home admission. J Am Geriatr Soc. 2009;57:146–52. doi: 10.1111/j.1532-5415.2008.02090.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy-Byrne PP, Joesch JM, Wang PS, Kessler RC. Low socioeconomic status and mental health care use among respondents with anxiety and depression in the NCS-R. Psychiatr Serv. 2009;60:1190–7. doi: 10.1176/ps.2009.60.9.1190. [DOI] [PubMed] [Google Scholar]
- Schelbert EB, Rosenthal GE, Welke KF, Vaughan-Sarrazin MS. Treatment variation in older black and white patients undergoing aortic valve replacement. Circulation. 2005;112:2347–53. doi: 10.1161/CIRCULATIONAHA.104.530550. [DOI] [PubMed] [Google Scholar]
- Snowden LR. Bias in mental health assessment and intervention: theory and evidence. Am J Public Health. 2003;93:239–43. doi: 10.2105/ajph.93.2.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strakowski SM, Flaum M, Amador X, Bracha HS, Pandurangi AK, Robinson D, Tohen M. Racial differences in the diagnosis of psychosis. Schizophr Res. 1996;21:117–24. doi: 10.1016/0920-9964(96)00041-2. [DOI] [PubMed] [Google Scholar]
- Sue S, Zane N, Young K. Research on Psychotherapywith Culturally Diverse Populations. In: Bergin AE, Garfield SL, editors. Handbook of Psychotherapy and Behavior Change. Wiley and Sons; New York: 1994. pp. 783–820. [Google Scholar]
- Sussman LK, Robins LN, Earls F. Treatment-seeking for depression by black and white Americans. Soc Sci Med. 1987;24:187–96. doi: 10.1016/0277-9536(87)90046-3. [DOI] [PubMed] [Google Scholar]
- Thompson JW, Blaine JD. Use of ECT in the United States in 1975 and 1980. Am J Psychiatry. 1987;144:557–62. doi: 10.1176/ajp.144.5.557. [DOI] [PubMed] [Google Scholar]
- Thompson JW, Weiner RD, Myers CP. Use of ECT in the United States in 1975, 1980, and 1986. Am J Psychiatry. 1994;151:1657–61. doi: 10.1176/ajp.151.11.1657. [DOI] [PubMed] [Google Scholar]
- Whalen D, Houchens R, Elixhauser R. 2005 HCUP Nationwide Inpatient Sample (NIS) Comparison Report. U.S. Agency for Healthcare Research and Quality; 2008. (HCUP Methods Series Report # 2008-01). [Google Scholar]
- Williams MD, Rummans T, Sampson S, Knapp R, Mueller M, Husain MM, Fink M, Rasmussen K, O’Connor K, Smith G, Petrides G, Kellner CH. Outcome of electroconvulsive therapy by race in the Consortium for Research on Electroconvulsive Therapy multisite study. J Ect. 2008;24:117–21. doi: 10.1097/YCT.0b013e31815c6641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wohi M, Lesser I, Smith M. Clinical presentations of depression in African American and white outpatients. Cult Divers Ment Health. 1997;3:279–84. doi: 10.1037/1099-9809.3.4.279. [DOI] [PubMed] [Google Scholar]
- Young AS, Klap R, Sherbourne CD, Wells KB. The quality of care for depressive and anxiety disorders in the United States. Arch Gen Psychiatry. 2001;58:55–61. doi: 10.1001/archpsyc.58.1.55. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.