Abstract
Problem
Malawi has one of the world’s highest rates of human immunodeficiency virus (HIV) infection (10.6%), and southern Malawi, where Thyolo district is located, bears the highest burden in the country (14.5%). Tuberculosis, common among HIV-infected people, requires radiologic diagnosis, yet Malawi has no radiologists in public service. This hinders rapid and accurate diagnosis and increases morbidity and mortality.
Approach
Médecins Sans Frontières, in collaboration with Malawi’s Ministry of Health, implemented teleradiology in Thyolo district to assist clinical staff in radiologic image interpretation and diagnosis.
Local setting
Thyolo district’s 600 000 inhabitants are mostly subsistence-level or migrant farmers living in extreme poverty. Health facilities include one public hospital and 38 primary health centres. Understaffing and the absence of a radiologist make the diagnosis of tuberculosis difficult in a population where this disease affects 66% of patients with HIV infection.
Relevant changes
From September 2010–2011, 159 images (from 158 patients) were reviewed by teleradiology. Teleradiology changed patient management in 36 cases (23.5%). Two (1.3%) of them were cases of pulmonary tuberculosis not previously suspected by clinical staff. In addition, the radiologist’s review corrected the misdiagnosis of tuberculosis and averted inappropriate treatment in 16 patients (10.5%).
Lessons learnt
Teleradiology can improve tuberculosis diagnosis and case management, especially if criteria to identify the patients most suitable for referral are developed and the radiologist is conversant with local resources and health problems. Designating a clinical focal point for teleradiology ensures sustainability. Staff need time to adapt to a new teleradiology programme.
Résumé
Problème
Le Malawi connaît l'un des taux les plus élevés au monde d'infection par le virus de l'immunodéficience humaine (VIH) (10,6%), et le Sud du Malawi, où se trouve le district de Thyolo, porte le fardeau le plus lourd du pays (14,5%). La tuberculose, fréquente chez les personnes infectées par le VIH, nécessite un diagnostic radiologique. Pourtant, le Malawi ne dispose pas de radiologues dans le secteur public. Cela empêche un diagnostic rapide et précis et accroît la morbidité et la mortalité.
Approche
Médecins Sans Frontières, en collaboration avec le ministère de la Santé du Malawi, a mis en œuvre un service de téléradiologie dans le district de Thyolo, pour aider le personnel clinique à interpréter les images radiologiques et à établir un diagnostic.
Environnement local
Les 600 000 habitants du district de Thyolo sont, pour la plupart, des agriculteurs disposant du minimum vital, ou des migrants vivant dans l'extrême pauvreté. Les établissements sanitaires se composent d’un hôpital public et de 38 centres de santé primaires. Le manque de personnel et l'absence de radiologues rendent le diagnostic de la tuberculose difficile dans une population où cette maladie affecte 66% des patients atteints de l'infection par le VIH.
Changements significatifs
De septembre 2010 à 2011, 159 images (de 158 patients) ont été examinées par téléradiologie. La téléradiologie a changé la prise en charge de 36 patients (23,5% des cas). Deux (1,3%) d'entre eux étaient des cas de tuberculose pulmonaire que le personnel clinique ne soupçonnait pas auparavant. En outre, l'examen du radiologue a corrigé un diagnostic de tuberculose erroné et évité un traitement inapproprié chez 16 patients (10,5%).
Leçons tirées
La téléradiologie peut améliorer le diagnostic et la gestion des cas de tuberculose, en particulier si des critères d’identification sont développés pour les patients les plus adaptés à une orientation vers des centres spécialisés, et que le radiologue connaît bien les ressources et les problèmes de santé locaux. Désigner un point de convergence clinique pour la téléradiologie assure la pérennité du projet. Le personnel a besoin de temps pour s'adapter à un nouveau programme de téléradiologie.
Resumen
Situación
Malawi presenta una de las tasas más altas (10,6%) de infección por el virus de la inmunodeficiencia humana (VIH) del mundo, y el sur de Malawi, donde se encuentra el distrito de Thyolo, es la zona más afectada del país (14,5%). La tuberculosis, muy habitual entre los infectados por el VIH, requiere un diagnóstico radiológico, pero Malawi no tiene radiólogos en su servicio público, lo que impide diagnosticar la enfermedad de manera rápida y exacta y aumenta la morbilidad y la mortalidad.
Enfoque
Médecins sans Frontières, en colaboración con el Ministerio de Sanidad de Malawi, han aplicado la radiología a distancia en el distrito de Thyolo para ayudar al personal clínico en la interpretación de imágenes radiológicas y el diagnóstico.
Marco regional
La mayoría de los 600 000 habitantes del distrito de Thyolo apenas pueden sustentarse o son granjeros inmigrantes que viven en la pobreza extrema. Las instalaciones sanitarias incluyen un hospital público y 38 centros de atención primaria. La escasez de personal y la ausencia de un radiólogo dificultan el diagnóstico de la tuberculosis en una población en la que dicha enfermedad afecta al 66% de los pacientes infectados por el VIH.
Cambios importantes
Por medio de la radiología a distancia se examinaron 159 imágenes (provenientes de 158 pacientes) desde septiembre de 2010 a 2011. La radiología a distancia supuso un cambio en la gestión de 36 casos (23,5%). Dos de ellos (1,3%) resultaron ser casos de tuberculosis pulmonar de la que el personal clínico no había sospechado antes. Además, el examen del radiólogo corrigió el error de diagnóstico de la tuberculosis y evitó un tratamiento inadecuado en 16 pacientes (10,5%).
Lecciones aprendidas
La radiología a distancia puede mejorar el diagnóstico de la tuberculosis y la gestión de los casos, en especial cuando se han desarrollado criterios para identificar a los pacientes más adecuados para derivarlos a un especialista y el radiólogo está versado en los recursos locales y los problemas sanitarios. La designación de un centro clínico de coordinación para la radiología a distancia garantiza la sostenibilidad. El personal necesita tiempo para adaptarse al programa nuevo de radiología a distancia.
ملخص
المشكلة
تحتوي ملاوي على واحد من أعلى معدلات الإصابة بعدوى فيروس العوز المناعي البشري (10.6 %) ويرزح جنوب ملاوي الذي تقع به مقاطعة ثيولو تحت أكبر عبء في البلد (14.5 %). ويتطلب السل الذي يشيع بين الأشخاص المصابين بعدوى فيروس العوز المناعي البشري تشخيصاً إشعاعياً، إلا أن ملاوي لا يوجد بها أخصائيو أشعة في الخدمة العمومية، وهو ما يعيق التشخيص السريع والدقيق ويزيد من معدلات المراضة والوفيات.
الأسلوب
نفذت منظمة "أطباء بلا حدود" بالتعاون مع وزارة الصحة في ملاوي، تشخيص الأشعة عن بعد في مقاطعة ثيولو بغية مساعدة العاملين في الطب السريري في تفسير وتشخيص الصور الإشعاعية.
المواقع المحلية
يعيش سكان مقاطعة ثيولو البالغ عددهم 600000 نسمة في الأغلب في مستوى الكفاف أو هم مزارعون مهاجرون يعيشون في فقر مدقع. وتتضمن المرافق الصحية مستشفى عمومي و38 مركزاً صحياً أولياً. ويؤدي نقص العاملين وغياب أخصائيي الأشعة إلى صعوبة تشخيص السل لدى السكان حيث يؤثر هذا المرض على نسبة 66 % من المرضى المصابين بعدوى فيروس العوز المناعي البشري.
التغيّرات ذات الصلة
تم استعراض 159 صورة (من 158 مريضاً) بواسطة تشخيص الأشعة عن بعد في الفترة من أيلول/سبتمبر 2010 إلى أيلول/سبتمبر 2011. وأدى تشخيص الأشعة عن بعد إلى تغيير التدبير العلاجي للمرضى في 36 حالة (23.5 %). وكانت حالتان (1.3 %) منهما تعانيان من سل رئوي لم يسبق الاشتباه فيه من جانب العاملين في الطب السريري. وعلاوة على ذلك، أدى استعراض أخصائي الأشعة إلى تصحيح التشخيص الخاطئ للسل وتفادي العلاج غير الملائم لدى 16 مريضاً (10.5 %).
الدروس المستفادة
من الممكن أن يؤدي تشخيص الأشعة عن بعد إلى تحسين تشخيص السل والتدبير العلاجي لحالاته، ولاسيما إذا ما تم وضع معايير لتحديد المرضى الأكثر ملائمة للإحالة وأعتاد أخصائي الأشعة على الموارد المحلية والمشكلات الصحية. ومن شأن تعيين نقطة اتصال سريرية لتشخيص الأشعة عن بعد أن يضمن الاستدامة. ويحتاج العاملون إلى التكيف مع البرنامج الجديد لتشخيص الأشعة عن بعد.
摘要
问题
马拉维是世界上艾滋病病毒(HIV)感染率(10.6%)最高的地区之一,而乔洛区所在的南部马拉维则背负着该国的最高发病率(14.5%)。艾滋病毒感染者中常见的肺结核病需要放射诊断,但马拉维公共服务没有放射科医师。这阻碍了快速准确的诊断,使发病率和死亡率增加。
方法
无国界医生组织与马拉维卫生部合作,在乔洛区实施远程放射学,协助临床工作人员进行放射影像解译和诊断。
当地状况
乔洛区的60 万居民大多是处于维持生计水平或进城务工的农民,生活在极端贫困状态中。卫生设施包括一所公立医院和38 个初级卫生中心。在艾滋病毒感染患者有66%受结核病影响的人群中,由于人手不足和缺乏放射科医师,这种疾病的诊断非常困难。
相关变化
从2010-2011 年9 月起,对159 份影像(来自158 名患者)通过远程放射学进行了审查。远程放射学改变 了36 个病 例(23.5%)的患者管理。其中两例(1.3%)是之前未被临床工作人员怀疑的肺结核病例。此外,放射科医师的审查纠正了16 名(10.5%)肺结核误诊并避免了不适当的治疗。
经验教训
远程放射学可以改善结核病的诊断和病例管理,在制订了确定最适合转诊的病人的标准且放射科医师熟悉当地资源和卫生问题的情况下尤其如此。指定远程放射学的临床联络点确保了可持续性。工作人员需要时间来适应新的远程放射学计划。
Резюме
Вопрос
В Республике Малави зарегистрирован один из самых высоких уровней заболеваемости вирусом иммунодефицита человека (ВИЧ) в мире (10.6%), причем наибольшее число инфицированных приходится на южную часть Малави, с расположенным там районом Тиоло (14.5%). Туберкулез, часто встречающийся у ВИЧ-инфицированных людей, требует рентгенодиагностики, однако же, в государственной службе здравоохранения Малави пока нет врачей-рентгенологов. Это препятствует быстрой и точной диагностике и увеличивает заболеваемость и смертность.
Подход
"Врачи без границ", в сотрудничестве с Министерством здравоохранения Малави, осуществляли телерентгенологию в районе Тиоло в целях оказания помощи медицинскому персоналу в интерпретации рентгеновских изображений и диагностике.
Местные условия
Шестисоттысячное население района Тиоло, в основном, состоит из ведущих натуральное хозяйство или мигрирующих крестьян, живущих в крайней нищете. Медицинские учреждения включают одну государственную больницу и 38 отделений скорой помощи. Недоукомплектованность штата и отсутствие врачей рентгенологов затрудняют диагностику туберкулеза у населения, у которого это заболевание поражает 66% ВИЧ-инфицированных пациентов.
Соответствующие изменения
Начиная с сентября 2010 г. по 2011 г., с помощью телерентгенологии было изучено 159 снимков (158 пациентов). Благодаря телерентгенологии было изменено ведение пациентов в 36 случаях (23,5%). В двух случаях (1,3%) из этого числа был выявлен туберкулез легких, ранее не предполагаемый медицинским персоналом. Кроме того, благодаря проверке, проведенной врачами-рентгенологами, был исправлен ошибочный диагноз туберкулеза и предотвращено неправильное лечение у 16 пациентов (10,5%).
Извлеченные уроки
Телерентгенология может улучшить диагностику туберкулеза и ведение пациентов, особенно, если разрабатываются критерии определения пациентов, наиболее подходящих для направления к врачу, и врачи-рентгенологи осведомлены о местных ресурсах и проблемах со здоровьем. Определение клинического фокуса для телерентгенологии гарантирует устойчивое развитие. Персоналу требуется время для адаптации к новой программе телерентгенологии.
Background
Approximately 600 000 people inhabit Thyolo district in southern Malawi. Most are subsistence-level or migrant farmers who live in extreme poverty and have very little formal education.1,2 Thyolo district has one public hospital and 38 primary health centres.3 Although Malawi’s public health-care facilities provide care free of charge, staffing levels, particularly for higher-level clinical cadres, remain exceptionally low.3 The World Health Organization (WHO) recommends a ratio of 228 health professionals per 100 000 population.4 However, in 2010, Thyolo district had a health worker density of only 100 to 150 per 100 000 population.3
Médecins Sans Frontières (MSF) has been supporting Thyolo District Hospital and other health-care facilities in the surrounding area since 1997 with a focus on the care of patients with human immunodeficiency virus (HIV) infection and tuberculosis. Malawi has one of the highest prevalences of HIV infection in the world. Approximately 10.6% of the country’s population between the ages of 15 and 49 years is HIV-positive, and the infection rate in the southern region is especially high at 14.5%.5 Of patients in Malawi who are HIV-positive, an estimated 66% also have tuberculosis.6 However, diagnosing tuberculosis in HIV-infected patients remains difficult, especially among children or patients with sputum-smear-negative or extrapulmonary tuberculosis. At Thyolo District Hospital tuberculosis detection rates fall below expected WHO estimates due to lack of diagnostic capacity, including expert X-ray interpretation.7,8
Lack of accurate radiologic interpretation, which is common in countries of the African region,8 ultimately results in higher patient morbidity and mortality.8,9 In sub-Saharan Africa, 14 countries, including Malawi, do not have a single radiologist in public service.3,5 In light of staff shortages and in the absence of an in-hospital radiologist in Thyolo District Hospital, MSF implemented a teleradiology programme to improve the quality, timeliness and accessibility of tuberculosis screening among patients with or without HIV infection. The objective of the present study was to assess the feasibility of conducting such a programme in a low-resource setting. The authors describe the effect of teleradiology on diagnostic rates and patient management, with a focus on tuberculosis.
Methods
Teleradiology initiative
In September 2010, MSF implemented teleradiology in Thyolo District Hospital after the district health authority granted permission for its use and approved the credentials of the radiologist reading the images tele-transmitted for teleradiologic diagnosis. Cases were proposed for teleradiology by three expatriate physicians working at the hospital (one employed by MSF and two by Voluntary Services Overseas), none of whom was a radiologist, and by 27 Malawian clinical officers (three employed by MSF and 24 by the Ministry of Health). The expatriate physician working with MSF was appointed as the teleradiology focal person, responsible for the final selection of cases for teleradiology referral and for the transmission of digitized radiographic images. The antiretroviral technical supervisor, one of the Malawian clinical officers, was assigned the task of digitizing the selected radiographic images. All hospital inpatients undergoing radiologic testing as part of routine medical care were eligible for teleradiology referral, irrespective of their HIV status. However, only images that clinical staff felt unable to accurately interpret were sent for teleradiology. Patients signed a medical release form authorizing tele-transmission of their X-ray images. These were sent anonymously after being assigned a unique identification number. An electronic database was created to record teleradiology request forms, digital images and summaries of patient histories.
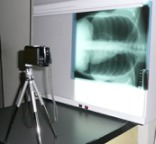
For digitization, the antiretroviral technical supervisor placed X-rays on a standard light box and photographed them using a Sony 10.1 megapixel digital camera (settings: flash OFF, self-timer, auto-exposure, exposure compensation set manually to +1.3EV) fixed to a tripod placed 70 cm from the light box exactly perpendicular to the film (Fig. 1). Photographs were downloaded to a computer as 100–200 KB JPEG digital images. JPEG images and patient histories, which included differential diagnoses proposed by Thyolo District Hospital clinical staff, were transmitted electronically from the teleradiology focal person to a radiologist (co-author WEB) in the University of Virginia, United States of America. Information was exchanged initially via e-mail and subsequently through a web-based telemedicine service (Médecins Sans Frontières/Swinfen Charitable Trust) that allowed data uploading and downloading directly to and from a web site with e-mail notification of postings by the telemedicine service.
Fig. 1.
Set up of digital camera, tripod and medical light box for photographing X-ray images in preparation for digitization and tele-transmission
For interpretation, all images were optimized using Adobe Photoshop CS4 on a Macintosh computer and viewed on a 69-cm monitor (1920 × 1200 pixel display) by the radiologist. Image manipulation included conversion of colour images to greyscale, edge enhancement/sharpening and brightness and contrast controls to “window” radiographic images for optimal viewing of lungs, soft tissues and bones. A teleradiology report based on image characteristics and patient history was returned by the radiologist in the United States to the physician from MSF free of charge by e-mail or text entry on the telemedicine web site. The expatriate physician from MSF notified the clinical staff member attending to the patient that the teleradiology report was available; this staff member then presented all patient information, including the teleradiology report, at a clinical meeting where final case management decisions were reached. Ours is one of very few studies assessing teleradiology services using JPEG image formats for tuberculosis screening in routine health-care service delivery.10–13
Analysis
We carried out a descriptive analysis of data for patients in Thyolo District Hospital whose radiologic images were referred to teleradiology between September 2010 and September 2011. We used Microsoft Excel 2003 and Stata 9.0 (Stata Corporation, College Station, USA) for data entering and analysis. Descriptive analyses included means and interquartile ranges for numerical variables, frequencies and proportions for categorical variables. Binomial and Fisher’s exact tests were used to generate 95% confidence intervals (CIs) and P-values, respectively. The data entered included patients’ routine demographic variables, the radiologist’s assessment of radiologic image quality (good or poor based on lung, soft tissue and bone visibility) and interpretability (conclusive or inconclusive for a definite diagnosis), and rate of agreement between the clinicians’ and the radiologist’s diagnoses. If the radiologist and clinical staff coincided on at least one differential diagnosis, we classified that as a diagnostic agreement. After presenting a case at the clinical meeting, the treating clinician in Thyolo District Hospital made a final treatment decision based on all available data (e.g. patient histories, clinical examinations, laboratory results and the teleradiology report). The clinician was free to base his final choice of treatment on his own clinical judgment, even if not supported by the radiologist’s diagnosis. Thus, all clinical staff worked as a team towards decision-making, and the radiologist was seen as a member of the team. We categorized final treatment decisions as being consistent with the radiologist’s diagnosis (i.e. clinical staff agreed with the diagnosis proposed by the radiologist and treated the patient accordingly) or consistent with the clinical staff’s diagnosis (i.e. the staff and the radiologist did not agree on any differential diagnosis or selected one diagnosis from several proposed by the radiologist but treated the patient in light of additional information, such as new symptoms or laboratory results not present before teleradiology referral). Clinical patient outcomes, evaluated from 48 hours to 4 weeks after hospital admission and treatment initiation, were defined as follows: “improved after initiating treatment”, “unchanged after initiating treatment”, “death” or “transfer”. Transfers were sent to Queen Elizabeth Central Hospital, outside of Thyolo district, when tests or treatments unavailable within the district were required. We also assessed the days that transpired between the taking of the X-rays and the request for teleradiology, and between the request and the receipt of the teleradiology reading.
Ethics
The use and evaluation of teleradiology at Thyolo District Hospital were approved by the Ministry of Health of Malawi. The analysis was presented to MSF’s ethics review board and not considered for further ethical review, since routinely collected programme data were used.
Results
From September 2010 to September 2011, 159 X-ray images from 158 patients at the Thyolo District Hospital were sent for teleradiology. The characteristics of the patients and images are listed in Table 1. Of the X-rays sent for teleradiology, 95.6% were chest radiographs, 3.8% were spine radiographs and 0.6% was not documented in the database as either chest or spine. Only four X-rays had to be repeated to improve image quality; 83.6% of the images were of good quality and 58.2% were considered conclusive for a final diagnosis based on image alone.
Table 1. Characteristics of patients studied and teleradiology images, Thyolo District Hospital, Malawi, 2010–2011.
| Variable of interest | No. | % | 95% CI |
|---|---|---|---|
| Age (years) | |||
| < 15 | 22 | 13.9 | – |
| 15–24 | 15 | 9.5 | – |
| 25–34 | 40 | 25.3 | – |
| 35–44 | 30 | 19.0 | – |
| 45–54 | 31 | 19.6 | – |
| 55+ | 20 | 12.7 | – |
| Total | 158 | 100.0 | – |
| Sex | |||
| Male | 77 | 48.7 | – |
| Female | 80 | 50.6 | – |
| Unknown | 1 | 0.6 | – |
| Total | 158 | 100.0 | – |
| HIV status | |||
| HIV-infected | 112 | 70.9 | – |
| HIV-negative | 39 | 24.7 | – |
| Unknown | 7 | 4.4 | – |
| Total | 158 | 100.0 | – |
| Type of X-ray | |||
| Chest | 152 | 95.6 | – |
| Spine | 6 | 3.8 | – |
| Unknown | 1 | 0.6 | – |
| Total | 159a | 100.0 | – |
| Diagnostic agreementb | |||
| Yes | 112 | 70.9 | 63.1–77.8 |
| No | 46 | 29.1 | 22.2–36.9 |
| Total | 158a,c | 100.0 | – |
| Image quality | |||
| Good | 133 | 83.6 | 77.0–89.0 |
| Poor | 26 | 16.4 | 11.0–23.0 |
| Total | 159a | 100.0 | – |
| Image interpretabilityd | |||
| Conclusive | 89 | 58.2 | 49.9–66.1 |
| Inconclusive | 64 | 41.8 | 33.9–50.1 |
| Total | 153a,e | 100.0 | – |
| Treatment | |||
| Consistent with radiologist's readingf | 133 | 85.3 | 78.7–90.4 |
| Consistent with reading by TDH clinical staffg | 23 | 14.7 | 9.6–21.3 |
| Total | 156a,h | 100.0 | – |
| Patient outcome | |||
| Improved with treatment | 99 | 65.1 | 57.0–72.7 |
| Unchanged with treatment | 0 | 0.0 | 0.0–2.4 |
| Death | 23 | 15.1 | 9.8–21.8 |
| Transfer | 30 | 19.7 | 13.7–27.0 |
| Total | 152a,i | 100.0 | – |
CI, confidence interval; HIV, human immunodeficiency virus; TDH, Thyolo District Hospital.
a One patient presented with two distinct medical conditions on hospital admissions five months apart.
b Whether the radiologist reported at least one diagnosis also proposed by clinical staff.
c Diagnostic agreement not documented for one case.
d Whether the radiographic image alone allowed for a definitive diagnosis.
e Image interpretability not documented for six cases.
f Clinical staff agreed with the radiologist’s diagnosis.
g Clinical staff reached a diagnosis that disagreed with the radiologist’s.
h Three patients lost to follow-up before treatment initiation.
i Outcome of seven patients unknown.
Overall, 70.9% of the radiologist’s diagnoses coincided with at least one diagnosis proposed by clinical staff.
Teleradiology changed the patient management initially proposed by Thyolo District Hospital clinical staff in 36 patients (23.5%); some had tuberculosis and others had other ailments (e.g. pulmonary fibrosis, cancer, chronic obstructive pulmonary disease). Two patients (1.3%) were diagnosed with pulmonary tuberculosis not suspected by clinical staff before teleradiology. Both were initiated on anti-tuberculosis treatment. In addition, the radiologist’s review corrected a misdiagnosis of tuberculosis and averted inappropriate treatment in 16 patients (10.5%).
Overall, 1.9% of the patients were lost to follow-up before treatment initiation (1 died; 1 left; 1 was transferred to Queen Elizabeth Central Hospital for further diagnostics and the final treatment received was unknown). Treatment was consistent with the diagnosis made by the radiologist in 85.3% of the patients and with the diagnosis made by the physician from MSF and by clinical staff at Thyolo District Hospital in 14.7% of the patients. In 1.9% of these patients anti-tuberculosis treatment had been initiated before the radiologist’s reading and could not be suspended because according to Malawi’s national health policy, patients on anti-tuberculosis treatment must complete the full course of therapy even if data pointing to a different diagnosis become subsequently available. Patients who had been placed on anti-tuberculosis treatment before hospital admission showed no improvement. Thus, in these cases teleradiology still proved valuable in identifying the correct ailment. Additional information became available following the radiologist’s reading for another 1.9% of patients. In 7.0% of the cases, clinical staff disagreed with the radiologist’s reading and decided on patient treatment on the basis of their own clinical experience with similar complex cases in Malawi. In another 3.8% of the cases, clinical staff agreed with one of the differential diagnoses proposed by the radiologist and treated the patients accordingly.
Overall, 65.1% of patients improved with treatment, 15.1% died and 19.7% were transferred to the central hospital.
The mean number of days between the X-ray and the request for teleradiology was 3.3 (interquartile range, IQR: 0–4.5). The mean number of days between the request for teleradiology and the teleradiology reading was 0.4 (IQR: 0–1).
Discussion
In our experience, teleradiology changed patient management in some cases by reducing the time to a definite diagnosis and preventing misdiagnosis. Thus, teleradiology enhanced the quality of patient care. It also served as an educational tool during the clinical meetings where final treatment decisions were reached. Agreement between the image interpretation of the clinical staff and the readings of the radiologist increased progressively from the first to the last quarter of images: from 66.7% among the first quarter, to 62.5% in the second, 70.0 % in the third and 84.6% in the fourth (P = 0.138). This increase was not significant, probably because of the relatively small number of patients contributing to this analysis. The utilization of teleradiology as a teaching tool during clinical meetings and training sessions contributed to its acceptability.
Our analysis adds to the sparse body of literature demonstrating the feasibility of using teleradiology, which requires simple equipment, for tuberculosis screening during routine health-care service delivery in rural Africa. Our findings are consistent with those of other studies in resource-limited settings.10–12,14
Our study has several limitations. We established no specific criteria for requesting teleradiology. Clinicians selected cases for teleradiology according to their level of confidence in their own X-ray interpretation. This could have influenced the results by making consultation a function of clinician self-assurance rather than case complexity. However, the physician from MSF who was appointed as the focal point for teleradiology made the final selection of cases for referral, potentially reducing this effect.
A second limitation is that most diagnoses of tuberculosis were presumptive for lack of confirmatory non-radiologic diagnostic methods, such as sputum culture, which is unavailable in Thyolo District Hospital. However, most patients improved with treatment, which suggests that the presumptive diagnoses made after the teleradiology reading were accurate. A third limitation is that image quality could have reduced diagnostic accuracy. JPEG compression, essential for transmission with slow or unreliable internet connections, decreases image file size, which leads, in turn, to poor image quality. Notably, several studies have demonstrated that JPEGs obtained by digital photography of film radiographs using limited image compression are sufficient for diagnosis in most instances; additionally, rates of discrepancy between radiologists are the same whether teleradiology images or regular X-ray images are being interpreted.10,12,15 In our experience, most images were classified as good and conclusive. Importantly, final diagnoses and case management were not based solely on the radiologist’s report. Rather, they involved complex decision-making processes using all available data.
Lessons learnt
In summary, our findings demonstrate the feasibility and utility of teleradiology in a hospital in rural Malawi and suggest that other resource-limited settings, particularly those with a similarly high burden of patients with HIV and tuberculosis co-infection, may also benefit from this service. To inform others, we highlight several lessons we have learnt (Box 1). First, to maximize its full potential and enhance equity of care, we recommend establishing specific criteria to guide clinical staff in identifying patients most likely to benefit from teleradiology. Despite access to teleradiology, several of our patients died; this points to the need for prompt teleradiology referral by clinical staff, which would be facilitated by such criteria. Second, the collaboration of radiologists who are familiar with the resources available locally and with the health conditions seen most often in the population of interest is very important. Third, a focal point for teleradiology should be selected from among local senior clinical staff members. Finally, staff should be allowed enough time to familiarize themselves with teleradiology to improve the acceptability of the method.
Box 1. Summary of main lessons learnt.
Staffing shortages in sub-Saharan Africa, particularly the absence of radiologists, often result in the delayed and inaccurate diagnosis of tuberculosis, leading to improper case management and increased morbidity and mortality.
In rural, resource-limited settings with a high rate of tuberculosis among patients infected with HIV, teleradiology can help to promptly confirm or correct diagnoses, enhance quality and equity in patient care and facilitate clinical staff training.
To maximize the potential of teleradiology, we recommend: (i) establishing criteria to help clinical staff identify patients most likely to benefit from referral; (ii) collaborating with a radiologist who is familiar with local resources and with the most frequent health problems in the population of interest; (iii) assigning the role of teleradiology focal point to a senior clinical officer at the health-care facility; and (iv) allowing enough time for clinical staff to adapt to the new teleradiology programme.
HIV, human immunodeficiency virus.
Implemented judiciously, teleradiology appears to improve the diagnosis of tuberculosis, especially in settings with a high burden of HIV infection, where the increased likelihood of sputum smear-negative tuberculosis necessitates a combination of diagnostic measures that include X-rays.8
Acknowledgements
We thank the Ministry of Health Malawi for its collaboration. In addition, we thank Tony Reid for his assistance with the editing of the manuscript.
Competing interests:
None declared.
References
- 1.Malawi Demographic and Health Survey 2010. Zomba and Calverton: NSO and ICF Macro; 2011. [Google Scholar]
- 2.2008 Population and Housing Census Zomba; National Statistical Office; 2008.
- 3.Malawi Health Workforce Observatory. Human resources for health country profile for Malawi. Geneva: World Health Organization; 2010.
- 4.The world health report 2006: working together for health. Geneva: World Health Organization; 2012. Available from: http://www.who.int/whr/2006/en/ [accessed 16 June 2012].
- 5.Jarvis L, Stanberry B. Teleradiology: threat or opportunity? Clin Radiol. 2005;60:840–5. doi: 10.1016/j.crad.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 6.Quarterly HIV programme report: October–December 2010 Lilongwe: Ministry of Health; 2010. [Google Scholar]
- 7.WHO report 2011: global tuberculosis control Geneva: World Health Organization; 2011. [Google Scholar]
- 8.Lawn SD, Ayles H, Egwaga S, Williams B, Mukadi YD, Santos Filho ED, et al. Potential utility of empirical tuberculosis treatment for HIV-infected patients with advanced immunodeficiency in high TB-HIV burden settings. Int J Tuberc Lung Dis. 2011;15:287–95. [PubMed] [Google Scholar]
- 9.Treatment of tuberculosis guidelines 4th ed. Geneva: World Health Organization; 2010. [PubMed] [Google Scholar]
- 10.Andronikou S, McHugh K, Abdurahman N, Khoury B, Mngomezulu V, Brant WE, et al. Paediatric radiology seen from Africa. Part I: providing diagnostic imaging to a young population. Pediatr Radiol. 2011;41:811–25. doi: 10.1007/s00247-011-2081-8. [DOI] [PubMed] [Google Scholar]
- 11.Corr P. Teleradiology in KwaZulu-Natal. A pilot project. S Afr Med J. 1998;88:48–9. [PubMed] [Google Scholar]
- 12.Corr P, Couper I, Beningfield SJ, Mars M. A simple telemedicine system using a digital camera. J Telemed Telecare. 2000;6:233–6. doi: 10.1258/1357633001935293. [DOI] [PubMed] [Google Scholar]
- 13.Uldal SB, Nikishova E, Rakova N, Mariandyshev A, Bye SM, Nisovtszevat N. Using e-mail in the management of tuberculosis patients, north-west Russia. Int J Tuberc Lung Dis. 2005;9:1367–72. [PubMed] [Google Scholar]
- 14.Marcelo A, Fatmi Z, Firaza PN, Shaikh S, Dandan AJ, Irfan M, et al. An online method for diagnosis of difficult TB cases for developing countries. Stud Health Technol Inform. 2011;164:168–73. [PubMed] [Google Scholar]
- 15.Szot A, Jacobson FL, Munn S, Jazayeri D, Nardell E, Harrison D, et al. Diagnostic accuracy of chest X-rays acquired using a digital camera for low-cost teleradiology. Int J Med Inform. 2004;73:65–73. doi: 10.1016/j.ijmedinf.2003.10.002. [DOI] [PubMed] [Google Scholar]