Abstract
Objective
To provide guidance for male circumcision programmes in Kenya by estimating the population of uncircumcised men and investigating the association between circumcision and infection with the human immunodeficiency virus (HIV), with particular reference to uncircumcised, HIV-uninfected men.
Methods
Data on men aged 15 to 64 years were derived from the 2007 Kenya AIDS Indicator Survey, which involved interviews and blood collection to test for HIV and herpes simplex virus 2 (HSV-2). The prevalence of HIV infection and circumcision in Kenyan provinces was calculated and the demographic characteristics and sexual behaviour of circumcised and uncircumcised, HIV-infected and HIV-uninfected men were recorded.
Findings
The national prevalence of HIV infection in uncircumcised men was 13.2% (95% confidence interval, CI: 10.8–15.7) compared with 3.9% (95% CI: 3.3–4.5) among circumcised men. Nyanza province had the largest estimated number of uncircumcised, HIV-uninfected men (i.e. 601 709), followed by Rift Valley, Nairobi and Western Province, respectively, and most belonged to the Luo ethnic tribe. Of these men, 77.8% did not know their HIV status and 33.2% were HSV-2-positive. In addition, 65.3% had had unprotected sex with a partner of discordant or unknown HIV status in the past 12 months and only 14.7% consistently used condoms with their most recent partner. However, only 21.8% of the uncircumcised, HIV-uninfected men aged 15 to 19 years were sexually active.
Conclusion
The Kenyan male circumcision strategy should focus on the provinces with the highest number of uncircumcised, HIV-uninfected men and target young men before or shortly after sexual debut.
Résumé
Objectif
Conseiller des programmes de circoncision masculine au Kenya en estimant le nombre d’hommes non circoncis et en recherchant l'association entre la circoncision et l’infection par le virus de l’immunodéficience humaine (VIH), avec une référence particulière aux hommes non circoncis et non infectés par le VIH.
Méthodes
Des données sur des hommes âgés de 15 à 64 ans ont été obtenues de l’enquête de 2007 sur les indicateurs du SIDA au Kenya, impliquant des entretiens et des prises de sang afin de rechercher la présence du VIH et du virus de l’herpès simplex 2 (VHS-2). La prévalence de l’infection par le VIH et la circoncision dans les provinces kenyanes a été calculée, et les caractéristiques démographiques ainsi que le comportement sexuel des hommes circoncis et non circoncis, des hommes infectés et non infectés par le VIH ont été enregistrés.
Résultats
La prévalence nationale de l’infection par le VIH chez les hommes non circoncis s’élevait à 13,2% (intervalle de confiance de 95%, IC: 10,8–15,7) par rapport à un pourcentage de 3,9% (IC de 95%: 3,3–4,5) chez les hommes circoncis. La province de Nyanza présentait l’estimation du plus grand nombre d’homme non circoncis et d’hommes non infectés par le VIH (601 709), suivie de la vallée du Rift, de Nairobi et de la province occidentale, respectivement, dont la plus grande partie appartenait à la tribu ethnique des Luo. Chez ces hommes, 77,8% ne connaissaient pas leur séropositivité et 33,2% étaient positifs au VHS-2. De plus, 65.3% d’entre eux avaient eu des rapports sexuels non protégés avec une partenaire de statut HIV inconnu ou discordant au cours des 12 derniers mois, et seuls 14,7% d’entre eux utilisaient constamment des préservatifs avec leur dernière partenaire. Cependant, seuls 21,8% des hommes non circoncis et non infectés par le VIH âgés de 15 à 19 ans étaient sexuellement actifs.
Conclusion
La stratégie de circoncision des hommes kenyans doit s’orienter sur les provinces présentant le plus grand nombre d'hommes non circoncis et non infectés par le VIH, mais aussi cibler les jeunes hommes avant ou peut de temps après leur première expérience sexuelle.
Resumen
Objetivo
Proporcionar orientación para los programas de circuncisión masculina en Kenia calculando la población de hombres circuncidados e investigando la relación entre la circuncisión y la infección con el virus de la inmunodeficiencia humana (VIH), haciendo alusión especial a los hombres no circuncidados ni infectados por el VIH.
Métodos
Los datos acerca de los hombres con edades comprendidas entre 15 y 64 años se obtuvieron de la Encuesta de indicadores del SIDA en Kenya del año 2007, que incluyó entrevistas y la recogida de muestras de sangre para realizar las pruebas del VIH y del virus del herpes simple de tipo 2 (VHS-2). Se calculó la prevalencia de la infección por el VIH y la circuncisión en las provincias de Kenia y se registraron las características demográficas y el comportamiento sexual de los hombres circuncidados y no circuncidados, infectados y no infectados con el VIH.
Resultados
La prevalencia nacional de la infección por VIH en los hombres circuncidados fue del 13,2% (intervalo de confianza del 95%, IC: 10,8 – 15,7) comparada con el 3,9% (IC 95%: 3,3 – 4,5) entre los hombres circuncidados. La provincia de Nyanza tuvo el mayor número estimado de hombres no circuncidados y no infectados por el VIH (esto es, 601 709), seguida por la provincia Rift Valley, Nairobi y la provincia Occidental, respectivamente, y la mayoría de ellos pertenecía a la tribu étnica Luo. De esos hombres, el 77,8% no conocía su estado serológico y el 33,2% estaba infectado con el VHS-2. Además, el 65,3% había mantenido relaciones sexuales sin protección con una pareja serodiscordante o que no conocía su estado serológico en los últimos 12 meses y sólo el 14,7% había empleado preservativos de manera sistemática con su pareja más reciente. No obstante, sólo el 21,8% de los hombres circuncidados e infectados por el VIH con edades entre los 15 y los 19 años era sexualmente activo.
Conclusión
La estrategia de circuncisión masculina en Kenya debería centrarse en las provincias con el mayor número de hombres no circuncidados y no infectados por el VIH y dirigirse a los hombres jóvenes antes o poco después de la primera relación sexual.
ملخص
الغرض
تقديم الإرشادات لبرامج ختان الذكور في كينيا من خلال تقدير عدد السكان من الرجال الذين لم يخضعوا للختان والتحقيق في الارتباط بين الختان والعدوى بفيروس العوز المناعي البشري (HIV)، بالإشارة على وجه الخصوص إلى الرجال الذين لم يخضعوا للختان غير المصابين بفيروس العوز المناعي البشري.
الطريقة
تم استخلاص البيانات المتعلقة بالرجال الذين تتراوح أعمارهم بين 15 إلى 64 سنة من مسح مؤشر الإيدز في كينيا لعام 2007، والذي اشتمل على مقابلات وجمع عينات الدم لاختبارها بغية اكتشاف الإصابة بفيروس العوز المناعي البشري وفيروس الهربس البسيط النمط 2 (HSV-2). وتم حساب انتشار العدوى بفيروس العوز المناعي البشري والختان في المقاطعات الكينية وتم تسجيل الخصائص الديمغرافية والسلوك الجنسي للرجال المختونين وغير المختونين والمصابين بعدوى فيروس العوز المناعي البشري وغير المصابين بعدوى فيروس العوز المناعي البشري.
النتائج
بلغت نسبة انتشار العدوى بفيروس العوز المناعي البشري على الصعيد الوطني لدى الرجال غير المختونين 13.2 % (فاصل الثقة 95 %، فاصل الثقة: 10.8 إلى 15.7) مقارنة بنسبة 3.9 % (فاصل الثقة 95 %: 3.3 إلى 4.5) بين الرجال المختونين. وضمت مقاطعة نيانزا أعلى عدد للرجال غير المختونين غير المصابين بعدوى فيروس العوز المناعي البشري (601709 شخص)، تلتها مقاطعة ريفت فالي ونيروبي والمقاطعة الغربية على التوالي، وكان معظمهم ينتمي إلى قبيلة لوو العرقية. ولم يعرف 77.8 % من هؤلاء الرجال حالة فيروس العوز المناعي البشري لديهم، وكانت نسبة 33.2 % منهم إيجابية لفيروس الهربس البسيط النمط 2. وعلاوة على ذلك، تورطت نسبة 65.3 % في ممارسات جنسية غير محمية خلال الاثني عشر شهراً الماضية مع شريك حالة فيروس العوز المناعي البشري لديه غير متوافقة أو غير معروفة ولم يستخدم سوى 14.7 % العازل الذكري بانتظام مع أحدث شريك. بيد أنه لم تكن سوى نسبة 21.8 % من الرجال غير المختونين، وغير المصابين بعدوى فيروس العوز المناعي البشري، ممن تتراوح أعمارهم بين 15 إلى 19 سنة نشطاء جنسياً.
الاستنتاج
يتعين أن تركز استراتيجية ختان الذكور في كينيا على المقاطعات التي تضم أعلى عدد من الرجال غير المختونين وغير المصابين بعدوى فيروس العوز المناعي البشري وأن تستهدف الشباب قبل النشاط الجنسي أو بعده بفترة قصيرة.
摘要
目的
通过肯尼亚未进行包皮环切男性人群数据估测,以及特别以未进行包皮环切、未感染HIV男性人群为参照进行的包皮环切与艾滋病毒(HIV)感染相关性研究,为肯尼亚男性包皮环切计划提供指导。
方法
采用的15 岁至64 岁男性的数据来源于2007 年肯尼亚艾滋病指标调查,其中涉及访视和采血进行艾滋病毒和单纯疱疹病毒2 型(HSV-2)检测。计算肯尼亚各省艾滋病毒感染率和包皮环切普及率,记录进行包皮环切和未进行包皮环切、受艾滋病毒感染和未受艾滋病毒感染的男性人口特征和性行为。
结果
包皮环切的男性的HIV感染率为3.9%(95% 置信区间:3.3-4.5),未进行包皮环切的男性HIV感染率为13.2%(95% 置信区间:10.8-15.7)。尼安萨省未进行包皮环切、未感染HIV的男性估计人数最多(即601709),其次分别是东非大裂谷、内罗毕和西部省,大部分属于卢奥民族部落。这些男性中,77.8%的男性不知道自己的HIV感染状况,33.2%男性的HSV-2 为阳性。此外,65.3%男性在过去12 个月中与艾滋病毒单阳或未知的的性伙伴有过不安全的性行为,只有14.7%的男性在最近期与性伙伴的性行为中始终使用避孕套。然而,在未进行包皮环切、未感染艾滋病毒的15 至19 岁的男子中,只有21.8%男性处于性活跃状态。
结论
肯尼亚男性包皮环切战略应将重点放在未进行包皮环切、未感染HIV人数最高的各省,并以初次性行为之前或之后不久的年轻男性为目标。
Резюме
Цель
Обеспечить руководство программами по обрезанию крайней плоти у мужчин в Кении посредством оценки численности мужчин, не подвергшихся обрезанию, и исследование связи между обрезанием крайней плоти и инфицированием вирусом иммунодефицита человека (ВИЧ) с особым акцентом на ВИЧ-неинфицированных мужчинах, не подвергшихся обрезанию.
Методы
Данные по мужчинам возрастной группы от 15 до 64 лет были получены из Индикаторного исследования СПИДа в Кении, 2007 г., которое включало опросы и взятие крови для проведения теста на наличие ВИЧ и вируса простого герпеса 2 (ВПГ-2). Были собраны данные по распространенности ВИЧ-инфекции и обрезанию крайней плоти в провинциях Кении, а также регистрировались демографические показатели и сексуальное поведение мужчин, подвергшихся и не подвергшихся обрезанию крайней плоти, ВИЧ-инфицированных и ВИЧ-неинфицированных мужчин.
Результаты
Национальная распространенность ВИЧ-инфекции у мужчин, не подвергшихся обрезанию, составила 13,2% (95% доверительный интервал, ДИ: 10,8–15,7) в сравнении с 3,9% (95% ДИ: 3,3–4,5) среди мужчин, подвергшихся обрезанию. В провинции Ньянза зарегистрировано наибольшее число мужчин, подвергшихся обрезанию крайней плоти, ВИЧ-инфицированных мужчин (т. е. 601 709), за которой следуют долина Рифт, Найроби и Западная провинция, соответственно. Большинство мужчин из данного числа принадлежат этническому племени Луо. Из этого числа мужчин, 77,8% не знали о своем ВИЧ-статусе и 33,2% имели ВПГ-2 антитела положительных образцов. Кроме того, 65,3% вступали в незащищенный половой контакт с партнером с дискордантным или неизвестным ВИЧ статусом за последние 12 месяцев и только 14,7% постоянно использовали презервативы при половом контакте с последним партнером. Тем не менее, только 21,8% ВИЧ-неинфицированных мужчин, не подвергшихся обрезанию, в возрастном диапазоне от 15 до 19 лет вели активную половую жизнь.
Вывод
Кенийская стратегия по обрезанию крайней плоти у мужчин должна быть сконцентрирована на провинциях с высоким числом ВИЧ-неинфицированных мужчин, не подвергшихся обрезанию, и направлена на юношей до или вскоре после начала половой жизни.
Introduction
Of an estimated 33.4 million people living with human immunodeficiency virus (HIV) infections worldwide, approximately 22.4 million live in sub-Saharan Africa and, of these, 1.5 million live in Kenya.1 Most HIV transmission in sub-Saharan Africa and Kenya is heterosexual. In the past two decades, observational studies have provided evidence that male circumcision has a protective effect against HIV infection and sexually transmitted infections in general.2,3 In addition, three randomized controlled trials indicated that male circumcision reduces the acquisition rate for HIV infection by approximately 60%.4–6 Consequently, the World Health Organization (WHO) and the Joint United Nations Programme on HIV/AIDS (UNAIDS) recommended that countries include male circumcision as part of HIV prevention interventions and expand its implementation, prioritizing areas with a low male circumcision rate and a high prevalence of HIV infection.7
Kenya’s population comprises over 40 ethnic groups, many of which have a cultural tradition of male circumcision. However, despite a high rate of migration from rural to urban areas and the resulting heterogeneous mixing of people with different ethnic and cultural practices, individuals’ cultural and religious practices, including their attitude to circumcision, tend to remain unchanged. The 2003 Kenya Demographic Health Survey estimated that 84% of men in the country were circumcised: the rate ranged from 46.4% in Nyanza province to 100% in North Eastern Province.8
Optimizing the expansion of male circumcision services depends on having nationally representative data on the size of the population and the distribution of uncircumcised men and on their demographic characteristics and sexual behaviour. Suitable data only became available with the 2007 Kenya AIDS Indicator Survey, which was used by the Kenyan Ministry of Public Health and Sanitation to develop a national strategy for male circumcision in 2009.9 The aim was to circumcise 80% of all eligible men aged 15 to 49 years between 2009 and 2013 and, consequently, to avert an estimated 100 000 HIV infections over 10 years.10 The male circumcision strategy targets men in four provinces with relatively large male adult populations where traditionally few men are circumcised (i.e. Nairobi, Nyanza, Rift Valley and Western Province).9 The strategy involves a phased approach over more than 10 years in which progressively younger males are circumcised, starting with men aged 15 years and older in regions with a high prevalence of HIV infection and a low circumcision rate and concluding with infant circumcision, where acceptable (personal communication, Kenyan Ministry of Public Health and Sanitation).
We conducted an in-depth analysis of national male circumcision data from the 2007 Kenya AIDS Indicator Survey with the aim of: (i) describing the prevalence of male circumcision in Kenya and the association between the prevalence of circumcision and the prevalence of HIV infection; (ii) describing the demographic characteristics and sexual behaviour of circumcised, uncircumcised, and uncircumcised HIV-uninfected men in Kenya; (iii) estimating the number of circumcised, uncircumcised, and uncircumcised HIV-uninfected men in Kenya; and (iv) deriving implications for male circumcision planning in Kenya. Although the national circumcision strategy targets both HIV-infected and HIV-uninfected men,9 our analysis paid particular attention to uncircumcised, HIV-uninfected men since there is little evidence that circumcising uncircumcised HIV-infected men reduces the risk of HIV transmission to sexual partners.11
Methods
The 2007 Kenya AIDS Indicator Survey involved a representative sample of households from all eight provinces in Kenya and was carried out between August and December 2007.12 It was designed to provide national and provincial data on the sociodemographic, behavioural and biological correlates of HIV infection.13 All individuals aged 15 to 64 years who were either usually resident in the selected households or visiting the household on the night before the survey were eligible to participate. Interviewers obtained information on the participants’ demographic characteristics and sexual behaviour using a structured questionnaire. In addition, a venous blood sample was taken to test for the presence of HIV or herpes simplex virus 2 (HSV-2) infection. All those who participated in the interview and gave a blood sample provided informed consent. The study was approved by the Kenya Medical Research Institute’s ethical review committee and the institutional review board of the Centers for Disease Control and Prevention in the United States of America (USA).
The interviewers obtained information on: (i) male circumcision, including whether, where and by whom it had been performed and age at circumcision; (ii) self-reported HIV status, based on the results of previous HIV testing; (iii) consistent condom use with the most recent sexual partner in the last 12 months, where consistent use was defined as using a condom each time the respondent had sexual intercourse with this partner; (iv) the number of sexual partners of unknown or discordant HIV status, based on the self-reported HIV status of partners, in the last 12 months; and (v) unprotected sex with a partner of unknown or discordant HIV status during at least one of the three most recent sex acts in the last 12 months. Individuals who performed male circumcision were classified as either medical practitioners, traditional practitioners or home health workers. No physical examination was conducted to verify circumcision.
Laboratory tests were performed by the Kenya National Public Health Laboratories12 and quality assurance was carried out at the laboratory of the Centers for Disease Control and Prevention and the Kenya Medical Research Institute in Nairobi. The Vironostika HIV-1/2 test (Bio-Mérieux Diagnostics, Marcy l’Etoile, France) was used to screen for HIV infection and all samples that tested positive were confirmed using the Murex HIV.1.2.O enzyme immunoassay (Abbott Laboratories, Abbott Park, USA). Samples that gave discordant results on the two tests were retested using the two assays and, if there were two sets of discordant results, the Roche HIV DNA version 1.5 polymerase chain reaction test (Hoffmann La Roche, Basel, Switzerland) was performed. All samples that tested positive for HIV and 5% of those that tested negative were retested at the quality assurance laboratory using the same procedure. Testing for HSV 2 was carried out using the Kalon enzyme immunoassay (Kalon Biological Limited, Guildford, United Kingdom of Great Britain and Northern Ireland). All samples that tested positive were retested using the Kalon test by a second laboratory technician. For quality control, all samples that tested positive for HSV 2, 5% of those that tested negative and all those that gave indeterminate results were retested at the quality assurance laboratory using the same procedure. Samples that gave discordant results at the two laboratories were reported as indeterminate.
We calculated the number of men in Kenya who had not been circumcised from estimates of the population and of the prevalence of circumcision and HIV infection in each province. We used the 1999 Kenyan Population and Household Census to estimate the size of the adult population.14 However, because data from the 2007 Kenya AIDS Indicator Survey on the number of uncircumcised men in some provinces included fewer than 25 observations, we calculated uncertainty bounds for the population estimates based on 95% confidence intervals (CIs) derived from survey data. All analyses were performed using the procedures for surveys in SAS software version 9.2 (SAS Institute Inc., Cary, USA). The analysis took into account the stratified cluster design of the survey and each response was weighted to take its sampling probability into account and to adjust for the nonresponse rate.
Results
Of the 19 840 individuals eligible to participate in the survey, 91% were interviewed and 80% gave blood samples. In total, 8883 were men. Of these, 7701 (86.7%) participated in the interview: 6586 (74.1%) reported being circumcised and 1092 (12.3%) reported being uncircumcised, whereas 23 (0.26%) did not report their circumcision status. Of the 1092 uncircumcised men, 979 (89.7%) were tested for HIV infection during the survey.
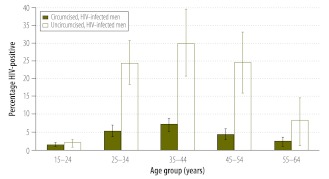
The overall prevalence of HIV infection in uncircumcised men was 13.2% compared with 3.9% in circumcised men Table 1. The prevalence was substantially higher among uncircumcised men aged 25 to 54 years than in those aged 15 to 24 years and peaked among men aged 35 to 44 years at 30.2% (Fig. 1).
Table 1. Circumcised and uncircumcised men aged 15–64 years, Kenya AIDS Indicator Survey 2007.
| Variable | Circumcised men (n = 6 586) |
Uncircumcised men (n = 1 092) |
|||
|---|---|---|---|---|---|
| No. | Weighted %a (95% CI) | No. | Weighted %a (95% CI) | ||
| Total | 6586 | 3.9 (3.3–4.5) | 1092 | 13.2 (10.8–15.7) | |
| Age group, years | |||||
| 15–24 | 2008 | 31.6 (30.0–33.3) | 505 | 48.8 (45.2–52.4) | |
| 25–34 | 1654 | 24.5 (23.1–25.9) | 227 | 20.1 (17.3–22.8) | |
| 35–44 | 1249 | 19.0 (17.8–20.2) | 161 | 14.4 (12.1–16.7) | |
| 45–54 | 953 | 13.8 (12.9–14.7) | 125 | 10.2 (8.3–12.1) | |
| 55–64 | 722 | 11.0 (10.1–11.9) | 74 | 6.6 (4.8–8.3) | |
| Total | 6586 | 100 (NA) | 1092 | 100 (NA) | |
| Province | |||||
| Nairobi | 792 | 8.9 (7.3–10.5) | 133 | 10.2 (5.7–14.7) | |
| Central | 1072 | 16.0 (14.4–17.7) | 49 | 4.3 (2.6–6.0) | |
| Coast | 794 | 8.6 (7.3–9.9) | 28 | 1.5 (0.8–2.3) | |
| Eastern | 1243 | 20.6 (18.0–23.3) | 52 | 4.5 (2.4–6.6) | |
| North-Eastern | 325 | 2.0 (1.6–2.4) | 9 | 0.3 (0.0–0.6) | |
| Nyanza | 533 | 8.6 (7.2–10.1) | 566 | 52.9 (46.3–59.4) | |
| Rift Valley | 970 | 23.0 (20.3–25.6) | 120 | 16.7 (12.2–21.2) | |
| Western | 857 | 12.2 (10.6–13.8) | 135 | 9.7 (5.2–14.1) | |
| Total | 6586 | 100 (NA) | 1092 | 100 (NA) | |
| Area of residence | |||||
| Rural | 4880 | 77.2 (74.1–80.3) | 836 | 79.8 (74.2–85.4) | |
| Urban | 1706 | 22.8 (19.7–25.9) | 256 | 20.2 (14.6–25.8) | |
| Total | 6586 | 100 (NA) | 1092 | 100 (NA) | |
| Educational level | |||||
| No primary | 605 | 6.5 (5.4–7.6) | 54 | 6.4 (3.7–9.1) | |
| Incomplete primary | 1696 | 27.2 (25.3–29.1) | 429 | 41.1 (36.5–45.6) | |
| Complete primary | 1580 | 24.6 (23.2–26.1) | 259 | 23.5 (20.4–26.5) | |
| Secondary or higher | 2705 | 41.7 (39.3–44.1) | 350 | 29.0 (24.8–33.3) | |
| Total | 6586 | 100 (NA) | 1092 | 100 (NA) | |
| Marital status | |||||
| Never married or cohabited | 2301 | 35.3 (33.6–37.0) | 489 | 46.9 (43.1–50.8) | |
| Currently married or cohabiting | 3918 | 58.8 (57.0–60.7) | 551 | 48.6 (44.9–52.3) | |
| Separated or divorced | 288 | 4.5 (3.9–5.1) | 34 | 2.8 (1.6–3.9) | |
| Widowed | 79 | 1.3 (1.0–1.7) | 18 | 1.7 (0.8–2.5) | |
| Total | 6586 | 100 (NA) | 1092 | 100 (NA) | |
| Ethnic tribe | |||||
| Embu | 101 | 1.6 (0.9–2.3) | 2 | 0.2 (0.0–0.5) | |
| Kalenjin | 545 | 11.0 (8.8–13.1) | 41 | 5.9 (2.4–9.3) | |
| Kamba | 809 | 13.6 (10.5–16.8) | 6 | 0.8 (0.0–1.8) | |
| Kikuyu | 1590 | 25.2 (22.6–27.7) | 54 | 4.8 (2.8–6.9) | |
| Kisii | 509 | 8.2 (6.8–9.5) | 5 | 0.4 (0.0–0.8) | |
| Luhya | 1161 | 17.0 (15.0–18.9) | 81 | 5.7 (2.1–9.2) | |
| Luo | 147 | 2.3 (1.6–2.9) | 739 | 66.7 (60.5–72.9) | |
| Masai | 68 | 2.0 (0.7–3.3) | 3 | 0.4 (0.0–0.8) | |
| Meru | 438 | 7.5 (6.3–8.7) | 32 | 3.1 (1.5–4.8) | |
| Mijikenda | 448 | 5.0 (4.0–6.0) | 0 | ||
| Somali | 383 | 2.4(2.0–2.9) | 5 | 0.2 (0.0–0.4) | |
| Taita/Taveta | 110 | 1.0 (0.7–1.3) | 2 | 0.1 (0.0–0.2) | |
| Swahili | 10 | 0.1 (0.0–0.1) | 0 | ||
| Other | 267 | 3.2 (2.2–4.2) | 122 | 11.7 (7.3–16.1) | |
| Total | 6586 | 100 (NA) | 1092 | 100 (NA) | |
| Self-reported HIV status | |||||
| Never tested or unknownb | 4833 | 76.2 (74.6–77.8) | 791 | 75.7 (71.8–79.5) | |
| Negative | 1530 | 23.3 (21.7–24.9) | 239 | 22.0 (18.2–25.9) | |
| Positive | 29 | 0.5 (0.3–0.7) | 27 | 2.3 (1.3–3.3) | |
| Total | 6392 | 100 (NA) | 1057 | 100 (NA) | |
| HSV-2 infection | |||||
| No | 4355 | 75.8 (74.3–77.4) | 546 | 59.3 (55.6–63.1) | |
| Yes | 1320 | 24.2 (22.6–25.7) | 396 | 40.7 (36.9–44.4) | |
| Total | 5675 | 100 (NA) | 942 | 100 (NA) | |
| Consistent condom use with most recent partner in the last 12 months | |||||
| Yes | 601 | 12.3 (11.1–13.5) | 124 | 16.1 (12.7–19.4) | |
| No | 4389 | 87.7 (86.5–88.9) | 633 | 83.9 (80.6–87.3) | |
| Total | 4990 | 100 (NA) | 757 | 100 (NA) | |
| Number of sexual partners of unknown or discordant HIV status in the last 12 months | |||||
| 0 | 1037 | 23.4 (21.8–25.0) | 136 | 20.2 (15.5–24.9) | |
| 1 | 2962 | 66.8 (65.1–68.5) | 423 | 63.2 (58.1–68.2) | |
| 2 | 371 | 8.5 (7.5–9.5) | 92 | 12.9 (9.9–15.8) | |
| 3 or more | 56 | 1.3 (0.9–1.7) | 29 | 3.8 (2.3–5.3) | |
| Total | 4426 | 100 (NA) | 680 | 100 (NA) | |
| Unprotected sex in the last 12 monthsc | |||||
| With partner of unknown or discordant status | 3143 | 65.0 (62.9–67.0) | 463 | 63.1 (56.8–69.3) | |
| With partner of concordant status | 1137 | 23.3 (21.5–25.1) | 156 | 21.1 (17.0–25.2) | |
| Did not have unprotected sex | 566 | 11.7 (10.5–13.0) | 118 | 15.8 (12.4–19.3) | |
| Total | 4846 | 100 (NA) | 737 | 100 (NA) | |
CI, confidence interval; HIV, human immunodeficiency virus; HSV-2, herpes simplex virus 2; NA, not applicable.
a Each man’s response was weighted to take its sampling probability into account and to adjust for the nonresponse rate.
b In total, 74 circumcised men and 26 uncircumcised men had been tested but did not know their HIV status.
c An individual was classified as having had unprotected sex in the last 12 months if he had unprotected sex during at least one of the three most recent sex acts in the last 12 months.
Fig. 1.
Prevalence of HIV infection among men aged 15–64 years, by circumcision status and age, Kenya AIDS Indicator Survey 2007
Note: The bars represent 95% confidence intervals.
Table 2 shows the estimated number of men aged 15 to 64 years in the eight provinces in Kenya who were or were not circumcised or infected with HIV. The number of HIV-uninfected men who were uncircumcised at the time of the survey was estimated to be around 1.2 million, which corresponded to 13% of the total male population in Kenya aged 15 to 64 years. Nyanza and Rift Valley Provinces had the highest estimated number of uncircumcised, HIV-uninfected men (601 709 and 235 688, respectively), followed by Nairobi Province with 135 271 and Western Province with 113 692 (Table 2). These four provinces accounted for nearly 90% of all uncircumcised, HIV-uninfected men in the country.
Table 2. Male population aged 15–64 years in Kenya, by province, circumcision status and HIV infection status, 2007.
| Province | No. of m en aged 15–64 yearsa | % male circumcision rateb | No. of circumcised men aged 15–64 years | No. of uncircumcised men aged 15–64 years | HIV infection in uncircumcised men aged 15–64 yearsc |
No. of uncircumcised, HIV-infected men aged 15–64 years | Uncircumcised, HIV-uninfected men aged 15–64 years |
||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of HIV-infected men/ total no.d | % (95% CI) | No. | Uncertainty bounde | ||||||||
| Nairobi | 1 009 000 | 83.2 | 839 488 | 169 512 | 21/122 | 20.2 (12.8–27.5) | 34 241 | 135 271 | 122 896–147 814 | ||
| Central | 1 160 000 | 95.5 | 1 107 800 | 52 200 | 0/43 | 0 (NA) | 0 | NA | NA | ||
| Coast | 759 000 | 97.0 | 736 230 | 22 770 | 5/24 | 15.3 (6.9–23.6) | 3 461 | 19 309 | 17 396–21 199 | ||
| Eastern | 1 380 000 | 96.3 | 1 328 940 | 51 060 | 1/49 | 0.9 (0.0–2.6) | 511 | 50 549 | 49 732–51 060 | ||
| North-Eastern | 361 000 | 97.3 | 351 253 | 9 747 | 1/9 | 7.2 (0.0–18.5) | 692 | 9 055 | 7 944–9 747 | ||
| Nyanza | 1 408 000 | 48.2 | 678 656 | 729 344 | 96/501 | 17.3 (13.3–21.2) | 127 635 | 601 709 | 572 535–632 341 | ||
| Rift Valley | 2 242 000 | 88.7 | 1 988 654 | 253 346 | 12/112 | 7.0 (2.0–11.9) | 17 658 | 235 688 | 223 198–248 279 | ||
| Western | 1 000 000 | 87.8 | 878 000 | 122 000 | 8/119 | 6.8 (2.0–11.6) | 8 308 | 113 692 | 107 848–119 560 | ||
| Total | 9 319 000 | 85.0 | 7 909 021 | 1 409 997 | 144/979 | 13.2 (10.8–15.7) | 186 120 | 1 223 877 | 1 188 627–1 257 717 | ||
CI, confidence interval; HIV, human immunodeficiency virus; NA, not applicable.
a Estimated using data from the Kenyan 1999 Population and Household Census.
b Derived from the Kenya AIDS Indicator Survey 2007.
c Derived from the Kenya AIDS Indicator Survey 2007.
d The number of HIV-infected, uncircumcised men and the total number of uncircumcised men were those included in the Kenya AIDS Indicator Survey 2007 for each province.
e The uncertainty bounds were based on the 95% confidence intervals from the Kenya AIDS Indicator Survey 2007.
Circumcised versus uncircumcised men
The median age of the 6586 circumcised men included in the survey was 32 years (interquartile range, IQR: 23–45) and their median age at the time of circumcision was 13 years (IQR: 10–16 years). The median time since circumcision was 20 years (IQR: 10–32). Overall, 83.9% (95% CI: 82.5–85.3) were circumcised under the age of 25 years and 1.7% reported being circumcised at 1 year of age or younger. Most circumcised men lived in rural areas, had completed at least primary education, were currently married or cohabiting with a partner and had never been tested for HIV (Table 1). More of these men belonged to the Kikuyu ethnic tribe than to any other ethnic tribe. Nearly one quarter had an HSV-2 infection. In total, 87.7% of sexually-active, circumcised men reported that they had not consistently used a condom with their most recent partner in the last 12 months, 76.6% had had at least one partner of unknown or discordant HIV status in the last 12 months and 65.0% reported that they had unprotected sex with a partner of unknown or discordant HIV status in the last 12 months.
Among circumcised men, 45.5% (95% CI: 43.0–48.1) reported having been circumcised at a health facility, whereas 52.4% (95% CI: 49.9–54.9) were circumcised at home (data not shown). Only 2.1% (95% CI: 1.5–2.7) were circumcised at another location or did not know who circumcised them. Of those circumcised at home, 21.8% (95% CI: 19.3–24.3) were circumcised by a home health worker or medical practitioner and 77.7% (95% CI: 75.2–80.2) were circumcised by a traditional practitioner. Overall, 57.1% (95% CI: 54.8–59.4) had been circumcised by a health worker or medical practitioner, irrespective of whether it took place at home or at a health facility, whereas 42.7% (95% CI: 40.2–44.7) had been circumcised by a traditional practitioner.
The median age of the 1092 uncircumcised men included in the survey was 26 years (IQR: 18–40). The majority lived in rural areas and almost half did not complete primary education (Table 1). In addition, almost half of all uncircumcised men were unmarried, the majority came from the Luo ethnic tribe and most had never been tested for HIV. Overall, 40.7% were infected with HSV 2. Among sexually-active, uncircumcised men, 83.9% reported that they did not consistently use a condom with their most recent partner, 79.8% had at least one partner of unknown or discordant HIV status in the last 12 months and 63.1% had unprotected sex with a partner of unknown or discordant status in the last 12 months.
Compared with circumcised men, uncircumcised men were younger, less well educated, less likely to be married or cohabitating with a partner and more likely to be infected with HSV 2 (P < 0.0001 for all; Table 1). Uncircumcised men were more likely to report consistent condom use with their most recent partner in the last 12 months (P = 0.0212) and having had two or more partners of unknown or discordant HIV status in the last 12 months (P = 0.0012). They were less likely to report unprotected sex and unprotected sex with a partner of unknown or discordant HIV status in the last 12 months (P = 0.0087).
Although some sociodemographic differences between circumcised and uncircumcised men, such as marital status, were influenced by the difference in median age between the groups, some differences remained statistically significant even when age was taken into account. For example, circumcised men aged 15 to 34 years were less likely than uncircumcised men of the same age to be from Nyanza province (9.4% [95% CI: 7.7–11.0] versus 49.3% [95% CI: 42.2–56.4], respectively), to belong to the Luo ethnic tribe (2.4% [95% CI: 1.6–3.1] versus 64.0% [95% CI: 57.2–70.7], respectively) and to have an HSV-2 infection (12.1% [95% CI: 10.7–13.5] versus 26.4% [95% CI: 22.0–30.9], respectively).
Uncircumcised, HIV-uninfected men
Table 3 shows the sociodemographic characteristics and reported sexual behaviour of the 835 uncircumcised, HIV-uninfected men in the survey. These men are representative of the priority target group for voluntary medical male circumcision in Kenya. The median age of this group was 26 years (IQR: 18–40): 55.0% were aged under 25 years and 72.5% were aged under 35 years (Table 3). Overall, 80.2% lived in rural areas and 93.7% had been educated to primary school level at least. In addition, 52.5% were neither married nor cohabiting with a partner at the time of the survey. Among those who were married or cohabitating, 13.7% (95% CI: 9.9–17.6) were in a polygamous marriage. In total, 63.1% were from the Luo ethnic tribe, whereas 5.5% and 6.7% were from the Luhya and Kalenjin ethnic tribes, respectively. The Kikuyu ethnic tribe, a community in which circumcision predominates, accounted for 5.8%.
Table 3. Uncircumcised, HIV-uninfected men aged 15–64 years, Kenya AIDS Indicator Survey 2007.
| Variable | Uncircumcised, HIV-uninfected men (n = 835) |
|
|---|---|---|
| No. | Weighted %a (95% CI) | |
| Age group, years | ||
| 15–24 | 439 | 55.0 (51.2–58.9) |
| 25–34 | 155 | 17.5 (14.2–20.8) |
| 35–44 | 94 | 11.1 (8.9–13.4) |
| 45–54 | 86 | 9.2 (7.2–11.1) |
| 55–64 | 61 | 7.2 (5.1–9.3) |
| Total | 835 | 100 (NA) |
| Province | ||
| Nairobi | 101 | 9.9 (5.5–14.3) |
| Central | 43 | 4.9 (2.9–6.9) |
| Coast | 19 | 1.4 (0.5–2.3) |
| Eastern | 48 | 5.3 (2.8–7.9) |
| North-Eastern | 8 | 0.4 (0.0–0.7) |
| Nyanza | 405 | 49.3 (42.4–56.3) |
| Rift Valley | 100 | 18.4 (13.1–23.8) |
| Western | 111 | 10.3 (5.8–14.9) |
| Total | 835 | 100 (NA) |
| Area of residence | ||
| Rural | 640 | 80.2 (74.6–85.8) |
| Urban | 195 | 19.8 (14.2–25.4) |
| Total | 835 | 100 (NA) |
| Educational level | ||
| No primary | 40 | 6.3 (3.3–9.2) |
| Incomplete primary | 341 | 42.5 (37.7–47.2) |
| Complete primary | 191 | 22.5 (19.2–25.7) |
| Secondary or higher | 263 | 28.8 (24.4–33.1) |
| Total | 835 | 100 (NA) |
| Marital status | ||
| Never married or cohabited | 421 | 52.5 (48.6–56.5) |
| Currently married or cohabiting | 382 | 44.1 (40.4–47.7) |
| Separated or divorced | 22 | 2.2 (1.1–3.3) |
| Widowed | 10 | 1.2 (0.2–2.2) |
| Total | 835 | 100 (NA) |
| Ethnic tribe | ||
| Embu | 2 | 0.3 (0.0–0.6) |
| Kalenjin | 36 | 6.7 (2.2–11.2) |
| Kamba | 6 | 1.1 (0.0–2.3) |
| Kikuyu | 47 | 5.8 (3.2–8.3) |
| Kisii | 4 | 0.4 (0.0–1.0) |
| Luhya | 62 | 5.5 (2.1–8.9) |
| Luo | 540 | 63.1 (56.5–69.6) |
| Masai | 3 | 0.5 (0.0–1.1) |
| Meru | 29 | 3.6 (1.6–5.6) |
| Mijikenda | 0 | 0 (NA) |
| Somali | 5 | 0.3 (0.0–0.6) |
| Taita/Taveta | 2 | 0.1 (0.0–0.2) |
| Swahili | 0 | 0 (NA) |
| Other | 99 | 12.8 (7.9–17.7) |
| Total | 835 | 100 (NA) |
| Self-reported HIV statusb | ||
| Never tested or unknownc | 627 | 77.8 (73.9–81.8) |
| Negative | 185 | 22.1 (18.1–26.1) |
| Positive | 1 | 0.1 (0.0–0.3) |
| Total | 813 | 100 (NA) |
| HSV-2 infection | ||
| No | 526 | 66.8 (63.4–70.3) |
| Yes | 275 | 33.2 (29.7–36.6) |
| Total | 801 | 100 (NA) |
| Consistent condom use with most recent partner in the last 12 months | ||
| Yes | 83 | 14.7 (11.2–18.1) |
| No | 465 | 85.3 (81.9–88.8) |
| Total | 548 | 100 (NA) |
| No. of sexual partners of unknown or discordant HIV status in last 12 months | ||
| 0 | 120 | 21.8 (16.2–27.5) |
| 1 | 340 | 62.9 (56.5–69.3) |
| 2 | 65 | 11.6 (8.5–14.6) |
| 3+ | 23 | 3.7 (2.0–5.3) |
| Total | 548 | 100 (NA) |
| Had unprotected sex in the last 12 monthsd | ||
| With partner of unknown or discordant HIV status | 345 | 65.3 (58.8–71.8) |
| With partner of concordant HIV status | 108 | 19.8 (15.2–24.5) |
| Did not have unprotected sex | 80 | 14.9 (11.3–18.4) |
| Total | 533 | 100 (NA) |
CI, confidence interval; HIV, human immunodeficiency virus; HSV-2, herpes simplex virus 2; NA, not applicable.
a Each man’s response was weighted to take its sampling probability into account and to adjust for the nonresponse rate.
b Only 813 of the 835 uncircumcised, HIV-uninfected men responded to the question regarding known HIV status.
c HIV status was unknown for 16 men.
d An individual was classified as having had unprotected sex in the last 12 months if he had sex without protection during at least one of the three most recent sex acts in the last 12 months.
Of the 835 uncircumcised, HIV-uninfected men, 22 (2.6%) did not respond to the question on HIV status, and 77.8% reported that they did not know their HIV status (Table 3). However, 33.2% had HSV-2 infections. In addition, 63.4% (95% CI: 58.8–68.1) of those aged 15 to 64 years and 21.8% (95% CI: 16.2–27.4) of those aged 15 to 19 years were sexually active. Of the sexually-active, uncircumcised, HIV-uninfected men aged 15 to 64 years, 14.7% reported that they had consistently used a condom with their last partner and 78.2% reported they had at least one sexual partner of unknown or discordant HIV status in the 12 months before the survey. In addition, 65.3% reported unprotected sex with a partner of unknown or discordant HIV status during the three most recent sex acts in the last 12 months (Table 3).
Discussion
We found that the prevalence of HIV infection was three times lower in uncircumcised men than in circumcised men, which provides evidence for a strong association between circumcision and HIV infection and confirms the need for interventions to expand male circumcision in Kenya. Overall, 15% of men aged 15 to 64 years in Kenya were not circumcised in 2007 and an estimated 90% of these men lived in the Nyanza, Rift Valley, Nairobi or Western Province, which are the main target regions of the national strategy for male circumcision.
Uncircumcised, HIV-uninfected men were typically young and lived in a rural area. The majority were educated to at least primary school level, were not married or cohabiting, belonged to the Luo ethnic tribe and had never been tested for HIV. Almost 80% reported having had sex with a partner of unknown or discordant HIV status in the last 12 months and few used condoms during these high-risk sex acts. However, there was a low level of sexual activity among HIV-uninfected men under 20 years of age, suggesting that, to reduce HIV transmission among newly sexually-active individuals, this age group should be targeted by the national programme for male circumcision and HIV testing, preferably before or soon after the men’s sexual debut.
We found that circumcision was mainly performed during adolescence and at home, with a high proportion being performed by traditional providers. However, traditional circumcision in a nonmedical setting has been associated with a high rate of adverse events, such as bleeding or infection.15,16 The national strategy for male circumcision includes plans to increase the use of safer surgical practices by trained health-care workers. This will involve engaging traditional male circumcision providers and educating communities and parents on the safety benefits for preadolescent boys.
We found that the prevalence of HSV-2 infection was significantly higher in uncircumcised than circumcised men. Although it has been shown that male circumcision has a protective effect against HSV-2 and human papillomavirus infections,3 approximately one third of uncircumcised, HIV-uninfected men in Kenya in 2007 were already infected with HSV 2. Given that the risk of infection increases with age, performing male circumcision before young men become sexually active could help reduce the risk of acquiring both HSV-2 and HIV infections. Finally, since the majority of uncircumcised men were from the Luo ethnic group, continuous engagement with elders and leaders of the Luo community could facilitate cultural acceptance of male circumcision.
Our study had limitations. First, cross-sectional surveys cannot establish a direct relationship between cause and effect. Second, physical examinations were not performed to determine whether there was any bias in the reporting of male circumcision. Third, we recorded information on whether circumcision was performed at home or in a health-care facility but not on whether it was performed as part of a community ritual, which is common practice in traditionally circumcising communities. Fourth, since sexual behaviour was self-reported, participants may have been reluctant to disclose some sexual risk factors. Fifth, some subgroup comparisons were limited by small sample sizes. Finally, due to cultural sensitivity concerning ethnicity and provinces in Kenya, we did not amalgamate ethnic tribes and provinces with small sample sizes. As a result, uncertainty in estimates derived using these samples may be large and the figures should be interpreted with caution.
The 2009 national male circumcision strategy stipulates that 80% of men in Kenya should be circumcised by 2014.9,17 In Nyanza province, implementation began in October 2008 and, by the end of September 2011, approximately 210 000 men had been circumcised, which is 50% of the target for 2014 (Athanasius Ochieng, personal communication). The use of outreach and mobile units involving dedicated teams has been recommended as the best approach for reaching men aged between 15 and 49 years in the first phase of the national strategy.18 However, efforts will be required to increase the acceptability of male circumcision since only 65% (range: 29–87) of uncircumcised men in sub-Saharan Africa find the procedure aceptable.19
In summary, our findings confirm that male circumcision programmes in Kenya should focus on four specific provinces, that circumcision by medical providers in traditionally circumcising regions should be increased and that comprehensive messages about the prevention of HIV transmission should be provided at the time of circumcision. In addition, our results suggest that circumcision programmes should specifically target younger men before or shortly after their sexual debut when they may still be free of HIV and HSV-2 infections. National survey data on sexual behaviour and the prevalence of HIV infection can be useful for resource allocation and for planning male circumcision programmes in sub-Saharan Africa in addition to providing essential data for HIV prevention. The 2007 Kenya AIDS Indicator Survey provided baseline data for the national male circumcision strategy for 2009 to 2014. It is anticipated that the 2012 Kenya AIDS Indicator Survey will inform the development of the new strategy for 2014 to 2019.
Acknowledgements
We thank Eddas Bennett, US Centers for Disease Control and Prevention; Willi McFarland, University of California San Francisco; and Michael Arnold, Godfrey Baltazar, Isack Baya, John Bore, Sufia Dadabhai, Helen Dale, Tura Galgalo, Catherine Gichimu, Allen Hightower, Jared Ichwara, George Kichamu, Andrea Kim, Evelyn Kim, Samuel Kipruto, George K’opiyo, Ernest Makokha, Barbara Marston, Lawrence Marum, Margaret Mburu, Jonathan Mermin, Joy Mirjahangir, Rex Mpazanje, Ibrahim Mohamed, Patrick Muriithi, James Muttunga, Carol Ngare, Raymond Nyoka, Linus Odawo, Samuel Ogola, Christopher Omolo, Ray Shiraishi, John Wanyungu and Anthony Waruru, 2007 Kenya AIDS Indicator Survey study group.
Funding:
This study was funded by the US President’s Emergency Plan for AIDS Relief through the US Centers for Disease Control and Prevention, US Department of Health and Human Services.
Competing interests:
None declared.
References
- 1.AIDS epidemic update 2009 Geneva: World Health Organization & Joint United Nations Programme on HIV/AIDS; 2009. [Google Scholar]
- 2.Weiss HA, Quigley MA, Hayes RJ. Male circumcision and risk of HIV infection in sub-Saharan Africa: a systematic review and meta-analysis. AIDS. 2000;14:2361–70. doi: 10.1097/00002030-200010200-00018. [DOI] [PubMed] [Google Scholar]
- 3.Tobian AA, Serwadda D, Quinn TC, Kigozi G, Gravitt PE, Laeyendecker O, et al. Male circumcision for the prevention of HSV-2 and HPV infections and syphilis. N Engl J Med. 2009;360:1298–309. doi: 10.1056/NEJMoa0802556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med. 2005;2:e298. doi: 10.1371/journal.pmed.0020298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bailey RC, Moses S, Parker CB, Agot K, Maclean I, Krieger JN, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007;369:643–56. doi: 10.1016/S0140-6736(07)60312-2. [DOI] [PubMed] [Google Scholar]
- 6.Gray RH, Kigozi G, Serwadda D, Makumbi F, Watya S, Nalugoda F, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369:657–66. doi: 10.1016/S0140-6736(07)60313-4. [DOI] [PubMed] [Google Scholar]
- 7.New data on male circumcision and HIV prevention: policy and programme implications WHO/UNAIDS Technical Consultation. Geneva: World Health Organization & Joint United Nations Programme on HIV/AIDS; 2007.
- 8.Central Bureau of Statistics. Kenya Demographic and Health Survey. Calverton: ORC Macro; 2003. [Google Scholar]
- 9.Kenya national strategy for voluntary medical male circumcision. Nairobi: Kenya Ministry of Public Health and Sanitation; 2009. [Google Scholar]
- 10.Bollinger L, DeCormier Plosky W, Stover J. Male circumcision: decision makers’ program planning tool, calculating the costs and impacts of a male circumcision program Washington: Futures Group; 2009. [Google Scholar]
- 11.Weiss HA, Hankins CA, Dickson K. Male circumcision and risk of HIV infection in women: a systematic review and meta-analysis. Lancet Infect Dis. 2009;9:669–77. doi: 10.1016/S1473-3099(09)70235-X. [DOI] [PubMed] [Google Scholar]
- 12.National AIDS and STI Control Programme. 2007 Kenya AIDS Indicator Survey: final report. Nairobi: Ministry of Health; 2009. [Google Scholar]
- 13.Oluoch T, Mohammed I, Bunnell R, Kaiser R, Kim AA, Gichangi A, et al. Risk factors for HIV infection in Kenya: a national population-based survey. Open AIDS J. 2011;5:125–34. doi: 10.2174/1874613601105010125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The 1999 population and household census Nairobi: Kenya National Bureau of Statistics; 1999. [Google Scholar]
- 15.Eaton L, Kalichman SC. Behavioral aspects of male circumcision for the prevention of HIV infection. Curr HIV/AIDS Rep. 2009;6:187–93. doi: 10.1007/s11904-009-0025-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bailey RC, Egesah O, Rosenberg S. Male circumcision for HIV prevention: a prospective study of complications in clinical and traditional settings in Bungoma, Kenya. Bull World Health Organ. 2008;86:669–77. doi: 10.2471/BLT.08.051482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mwandi Z, Murphy A, Reed J, Chesang K, Njeuhmeli E, Agot K, et al. Voluntary medical male circumcision: translating research into the rapid expansion of services in Kenya, 2008–2011. PLoS Med. 2011;8:e1001130. doi: 10.1371/journal.pmed.1001130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Considerations for implementing models for optimizing the volume and efficiency of male circumcision services Field testing ed. Geneva: World Health Organization; 2010. [Google Scholar]
- 19.Westercamp N, Bailey RC. Acceptability of male circumcision for prevention of HIV/AIDS in sub-Saharan Africa: a review. AIDS Behav. 2007;11:341–55. doi: 10.1007/s10461-006-9169-4. [DOI] [PMC free article] [PubMed] [Google Scholar]