Abstract
The article reports a case and review of the literature of endophthalmitis presenting as isolated retinal vasculitis. A 26-year-old male was observed to have white-centered retinal hemorrhages and retinal vasculitis following an occult scleral perforation. At presentation, the visual acuity was 20/60. With clinical suspicion of early endophthalmitis, he underwent wound exploration, scleral tear repair, vitreous biopsy and administration of intravitreal antibiotics. Microbiology evaluation revealed significant presence of methicillin-resistant coagulase-negative Staphylococcus epidermidis. Final visual acuity improved to 20/20 at 6 weeks postoperatively. Literature search revealed eight similar cases, all of them due to Staphylococcus species. Retinal vasculitis and white-centered retinal hemorrhages can be a presenting sign of early endophthalmitis, especially with non-fulminant pathogens like S. epidermidis.
Keywords: Endophthalmitis, retinal vasculitis, Staphylococcus epidermidis, white-centered retinal hemorrhages
Endophthalmitis is defined as a serious intraocular inflammatory disorder affecting the vitreous cavity, which can result from exogenous or endogenous spread of infecting organisms into the eye.[1] It can be a devastating condition leading to permanent visual loss even with prompt and appropriate therapy. In most cases, the presentation of endophthalmitis consists of reduced or blurred vision, red eye, pain, lid swelling, hypoyon, and progressive vitritis. Progression of the disease may lead to panophthalmitis, corneal infiltration, and perforation, affection of orbital structures, and eventually phthisis bulbi.[2] Isolated retinal periphlebitis/vasculitis and retinal hemorrhages are mentioned as an indicator of early endophthalmitis.[3] Detailed information on such cases has not been reviewed in the past.
We report a case of acute post-traumatic endophthalmitis where methicillin-resistant Staphylococcus epidermidis was isolated. The case was diagnosed in the early stages as endophthalmitis, based on the presence of isolated retinal vasculitis and white-centered hemorrhages. We did a Medline search for any similar cases reported in literature.
Case Report
A 26-year-old male presented with painless decrease of vision in the right eye following trauma with an iron particle 4 days prior to presentation. On examination, the visual acuity in the right eye was 20/60, intraocular pressure (IOP) was 12mmHg and there was localized conjunctival congestion superonasally [Fig. 1]. Anterior segment was unremarkable, while on fundus evaluation there was clear media with normal disc, few internal limiting membrane striae in the macular area, areas of retinal vasculitis associated with isolated “white-centered” retinal hemorrhages, and perivascular white-colored retinal exudates localized inferiorly [Fig. 1]. The protruding vitreous knuckle present beneath the insertion of the medial rectus muscle at its superior margin was cut with vitrector and the 2-mm-long scleral tear was sutured with 7-0-vicryl. After taking an undiluted vitreous biopsy with a 23-gauge vitrectomy cutter, intravitreal antibiotics, vancomycin 1 mg and ceftazidime 2.25 mg in 0.1 ml each was given. Based on the microbiological culture, biochemical tests and mini API ID 32 Staph strip, S. epidermidis was isolated. Antibiotic susceptibility testing of the isolate was done by the Kirby-Bauer disk diffusion method as per Clinical and Laboratory Standards Institute guidelines (CLSI, 2009).[4] The organism was found to be resistant to ciprofloxacin, ofloxacin, cefuroxime, oxacillin and cefoxitin (methicillin), and sensitive to amikacin, cefazoline, gentamicin, vancomicin, gatifloxacin, moxifloxacin and chloramphenicol. Postoperative treatment with tablet gatifloxacin (400 mg stat followed by 200 mg twice daily for 7 days), eye drop gatifloxacin 0.3% (12 times per day) and eye drop prednisolone acetate 1% (2 hourly initially, followed by tapering doses) resolved the infection. Final uncorrected visual acuity was 20/20 at 6 weeks postoperatively with resolution of all retinal signs [Fig. 2].
Figure 1.
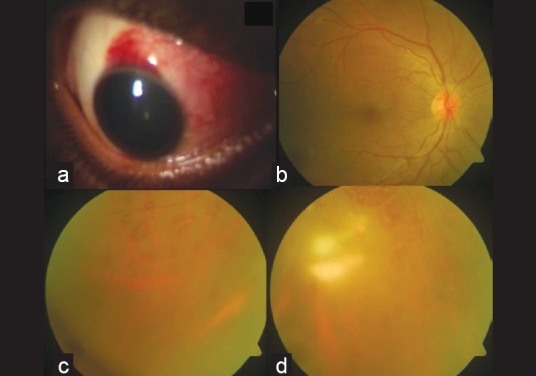
Clinical signs at presentation. (a) Area of occult scleral injury marked by localized congestion and chemosis; (b) fundus photograph showing macular internal limiting membrane striae; (c) white-centered retinal hemorrhages; (d) midperipheral and peripheral retinal vasculitis
Figure 2.
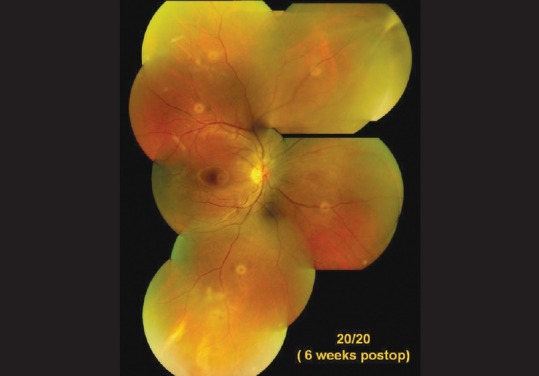
Postoperative fundus photograph showing resolution of retinal signs. Note the area of vitreous incarceration at the site of injury superonasally. Photographic artifacts (yellow circular) are seen
Discussion
Various authors[3,5–7] have documented the appearance of hemorrhages and vasculitis as an early feature of bacterial endophthalmitis. A case of fungal endophthalmitis[7] with vasculitis was reported earlier. Experimental inoculation of bacteria into the vitreous cavity revealed retinal periphlebitis to be the first clinical feature observed.[6] The pathogenesis of hemorrhages and periphlebitis is attributed to the breakdown of blood–retinal barrier, and thus perivascular exudation of plasma proteins and white blood cells.[8]
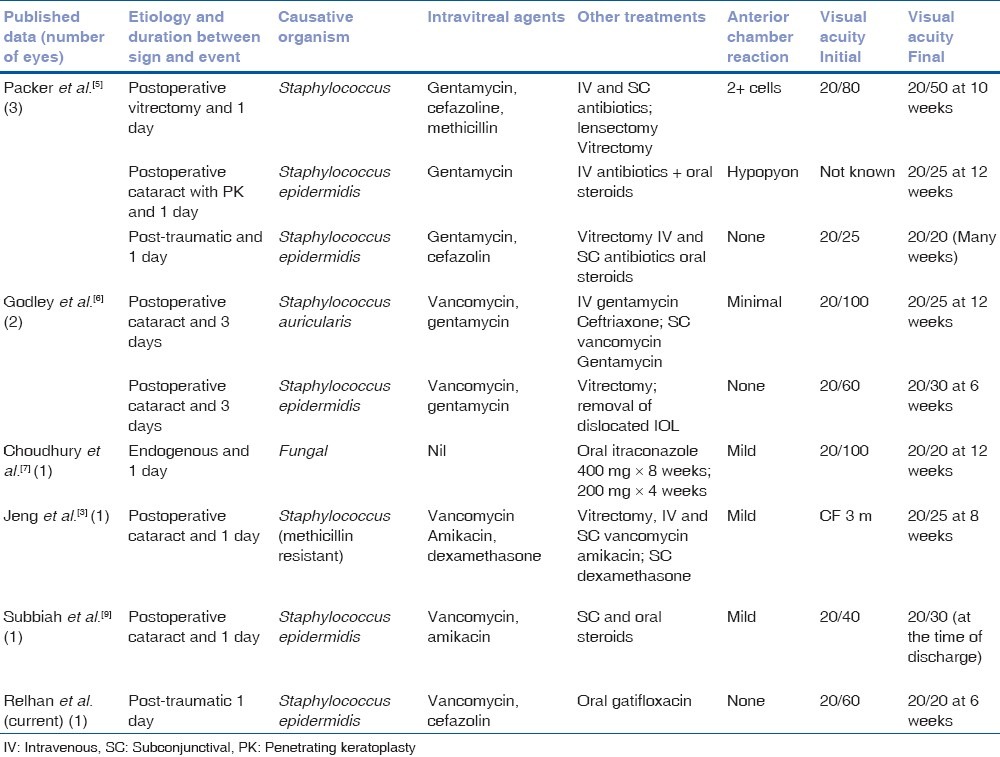
Retinal vasculitis as an isolated sign of endophthalmitis has been rarely reported in literature. This could be because of the lack of awareness, rarity of this sign, more fulminant cases or delayed diagnosis or delayed presentation leading to a poor view of fundus. A Medline search revealed only eight similar cases reported so far [Table 1]. Of these, only one case was post-traumatic. These findings may mimic the picture of retinal vein occlusion, Eales’ disease, Behcet's, sarcoidosis, pars planitis, infectious retinochoroiditis and non-specific uveitis, but a history of recent open globe trauma or surgery or systemic infection should indicate the possibility of an infectious etiology. In post-surgical eyes with increased anterior chamber reaction, dilated inferior retinal examination should be done to look for such white-centered retinal hemorrhages and vasculitis to rule out early endophthalmitis. A delay in the diagnosis and treatment of endophthalmitis is associated with poor visual recovery. All cases reviewed, including ours, had good visual outcomes with treatment.
Table 1.
Literature review of endophthalmitis presenting as retinal vasculitis and white-centered retinal hemorrhages
Conclusion
Awareness about retinal vasculitis being an early presenting feature could lead to early diagnosis of endophthalmitis and good visual outcome.
References
- 1.Mamalis N. Endophthalmitis. J Cataract Refract Surg. 2002;28:729–30. doi: 10.1016/s0886-3350(02)01350-0. [DOI] [PubMed] [Google Scholar]
- 2.Kernt M, Kampik A. Endophthalmitis: Pathogenesis, clinical presentation, management, and perspectives. Clin Ophthalmol. 2010;24:121–35. doi: 10.2147/opth.s6461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jeng BH, Kaiser PK, Lowder CY. Retinal vasculitis and posterior pole “hypopyons” as early signs of acute bacterial endophthalmitis. Am J Ophthalmol. 2001;131:800–2. doi: 10.1016/s0002-9394(00)00929-6. [DOI] [PubMed] [Google Scholar]
- 4.10th edition. Wayne, PA: Clinical and Laboratory Standards Institute; [Last accessed on 2010 Dec 20]. CLSI. Performance Standards for Antimicrobial Disk Susceptibility Tests, Approved Standard. Available from: http://www.clsi.org/source/orders/free/m02-a10.pdf.2009. MO2-A10 . [Google Scholar]
- 5.Packer AJ, Weingeist TA, Abrams GW. Retinal periphlebitis as an early sign of bacterial endophthalmitis. Am J Ophthalmol. 1983;96:66–71. doi: 10.1016/0002-9394(83)90456-7. [DOI] [PubMed] [Google Scholar]
- 6.Godley BF, Folk JC. Retinal hemorrhages as an early sign of acute bacterial endophthalmitis. Am J Ophthalmol. 1993;116:247–9. doi: 10.1016/s0002-9394(14)71301-7. [DOI] [PubMed] [Google Scholar]
- 7.Chowdhury T, Jalali S, Majji AB. Successful treatment of fungal retinitis and retinal vasculitis with oral itraconazole. Retina. 2002;22:800–2. doi: 10.1097/00006982-200212000-00020. [DOI] [PubMed] [Google Scholar]
- 8.Forster RK. Endophthalmitis. In: Duane TD, editor. Clinical Ophthalmology. Hagerstown: Harper and Row; 1981. p. 1. [Google Scholar]
- 9.Subbiah S, McAvoy CE, Best JL. Retinal vasculitis as an early sign of bacterial post-operative endophthalmitis. Eye (Lond) 2010;24:1410–1. doi: 10.1038/eye.2010.18. [DOI] [PubMed] [Google Scholar]


