Abstract
Patients with Benign Prostatic Hyperplasia (BPH) commonly presents with lower urinary tract symptoms (LUTS), which can be of obstructive symptoms such as hesitancy, incomplete voiding, post void dribbling or of irritative symptoms such as urgency, frequency and nocturia. Various recent studies indicate that nocturia is a very important and bothersome lower urinary tract symptom especially among patients with Benign Prostatic Hyperplasia (BPH). The aims of the study was to determine the frequency of common urinary symptoms among patients with BPH in HUSM as well as to evaluate the extent of bothersomeness of each and every symptom to these patients. This study too was aimed at evaluating the success of TURP in resolving pre operative LUTS. This was a questionnaire-based survey using a validated ICSBPH model whereby patients with BPH were selected and quizzed personally by an investigator. A subset of patients who had undergone TURP were further questioned regarding their satisfaction with the procedure. When nocturia is defined as waking up at night once or more to pass urine, the prevalence of nocturia was about 90%, but only 1 in 6 patients considered this is a very serious symptom. Even if the definition was changed to waking up twice or more, the prevalence is still quite high at over 80%. Urgency were noted in half of the patients, but only a quarter of them consider it a serious problem. 1 in 5 patients experienced significant leak and almost all consider it serious. About one third of the studied population had to be catheterized due to urinary obstruction and interestingly only about half of them considered it as a very serious event. Overall, a great majority of these patients considered suffering from these urinary symptoms for the rest of their life as very devastating. This study conclude that although the prevalence of nocturia was high among BPH patients, but it was not considered serious by majority of them. In fact, LUTS in our BPH patients did not differ much from BPH patients elsewhere. On the whole, TURP resolved most of the LUTS effectively.
Keywords: Survey, lower urinary tract symptoms, benign prostatic hyperplasia, nocturia, bothersomeness
Introduction
Nocturia has been perceived as a very important lower urinary tract symptom especially among patients with Benign Prostatic Hyperplasia (BPH). A search in the biomedicine database PubMed, which contains more than 12 million references from reports in medicine, yielded 136 references to reports in 1992 and 360 for publications in 2002 when the search term “nocturia” was used and the search was restricted to papers in English with abstracts and concerning adults > 65 years of age (1). In the USA, a population-based survey of male urinary symptoms found that prevalence of nocturia increased with age from 42% for 60–69 years, 55% for 70–79 years and 86% for 80–89 years (2).
In another European study, nocturia is regarded as the most common LUTS, reported by 72% of elderly people, and is considered to be a very bothersome condition (3). Malmsten et al research study showed that among the various LUTS, nocturia is the third most bothersome symptoms after urgency and incontinence. The prevalence of nocturia increases with age from 30% in men aged 45 years to 80% in men aged more than 80 years (4). Nocturia has been reported as one of the two most common causes of a disturbed sleep pattern. In fact, sleep disorders in patients with nocturia have been recognized as a potential cause of both illness and premature death (5). In a study of nighttime falls of the elderly, those with nocturia were at a significantly greater risk of falling with an increase from 10% to 21% with 2 or more voids per night. Falling often leads to fractures, particularly hip fractures, which are serious consequences of an already bothersome condition (6). Nocturia is also associated with increased morbidity and mortality. (7)
Objectives
Nocturia have attracted greater clinical interest in recent years in view of its association with high prevalence, bothersomeness among patients, morbidity and mortality. However we wanted to challenge this idea because in our daily practice, we hardly encounter patients complaining of nocturia or proclaiming of its bothersomeness. Thus, we embarked on a questionnaire-based survey to address this question and to find out the actual situation among our patients in the Urology Clinic, HUSM.
The objectives of the survey were to determine the frequency of common urinary symptoms among patients with BPH in HUSM, evaluate the extent of bothersomeness of each and every symptom as well as the significance of nocturia and its bothersomeness and how successful TURP was in resolving pre-operative LUTS in these patients.
Methodology
Our inclusion criteria were patients who had been diagnosed with benign prostatic enlargement clinically and are under the HUSM urology team follow-up. A questionnaire-based survey using a validated ICS-BPH model was used whereby patients with BPH were selected and interviewed personally by an investigator when they attended the Urology outpatient clinics or were traced from the medical records and interviewed via telephone calls. The patients interviewed via telephone calls were chosen at random. Their responses were then analyzed. A subset of patients who had undergone TURP were further questioned regarding their satisfaction with the procedure
The exclusion criterias were patients with diseases associated with edema (i.e. congestive cardiac failure, renal disease), diabetes mellitus, reduced renal concentrating capacity (i.e. diabetes insipidus and renal insufficiency), irritative bladder symptoms caused by bacterial cystitis, bladder calculi or bladder cancer.
Results
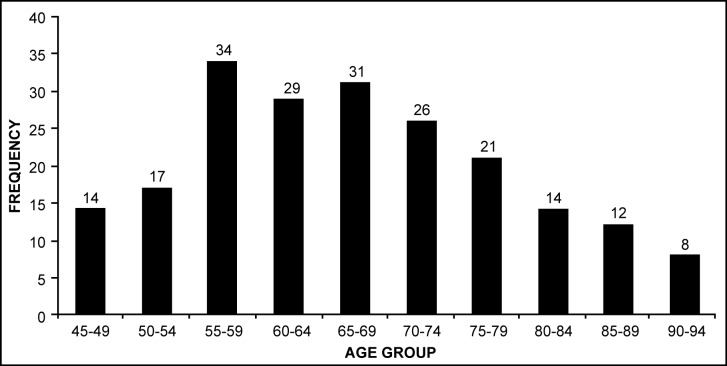
A total of 206 patients were recruited for the BPH survey and 78 patients were questioned for the TURP survey. The ages of the patients range between 45 to 90 years old with a mean age of 63 years old. (Figure 1).
Figure 1 :
Distribution of patients by Age Groups
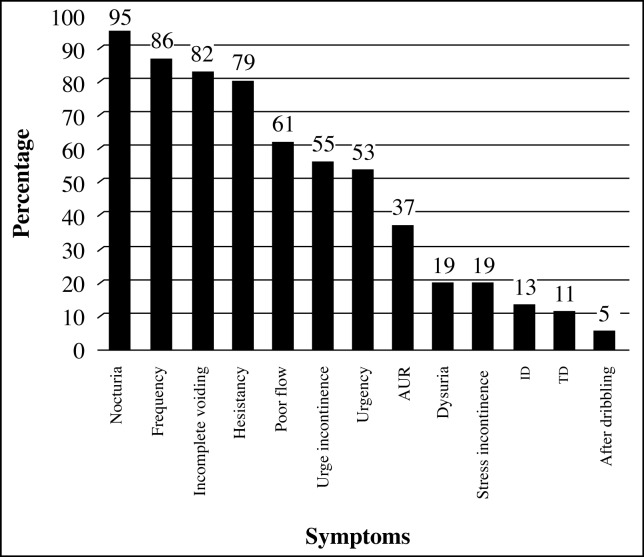
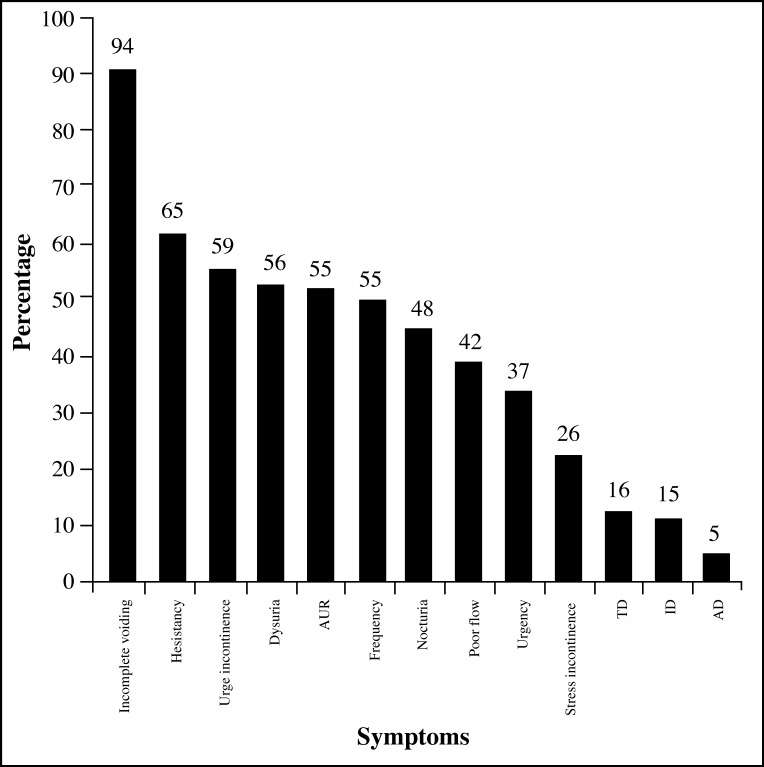
In this survey, nocturia was found to be the most common lower urinary tract symptoms. When nocturia is defined as waking up at night once or more to pass urine, the prevalence of nocturia is about 95% (Figure 2). Even if the definition was modified to waking up twice or more, the prevalence was still quite high at over 80%. This was followed by frequency, incomplete voiding, hesitancy, poor flow, urge incontinence, urgency, acute urinary retention, dysuria, stress incontinence, intermittent dribbling, terminal dribbling and after dribbling. In terms of bothersomeness, incomplete voiding was the most bothersome symptom among these patients, followed by hesitancy and urge incontinence (Figure 3).
Figure 2 :
Prevalence of LUTS among patients with BPH in HUSM
Figure 3 :
Prevalence of bothersomeness of lower urinary tract symptoms (LUTS) in patients with BPH in HUSM
Surprisingly, less than half of patients who had nocturia considered it a bothersome symptom. If we further analyzed this group of patients with nocturia, only 7% of them considered nocturia as a very serious bothersome problem. (Figure 4).
Figure 4 :
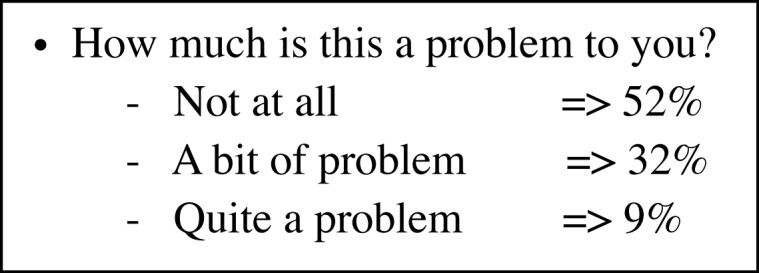
Result ; Bothersomeness of nocturia
Prevalence of nocturia and weak stream were noted to be increasing with age in this group of patients (Table 1). Urgency were noted in more than half of the patients, but only a third of them consider it a serious problem. About one third of the studied population had to be catheterized due to urinary obstruction and interestingly about half of them consider it as a very serious event.
Table 1 :
Percentage of 206 men with BPH complained with voiding difficulties, grouped according to age
| Age | voiding disturbances | ||||
|---|---|---|---|---|---|
| % Nocturia | % Hesitancy | % Dribbling | % Weak stream | % Incomplete voiding | |
| 45 | 27.3 | 4.3 | 29.4 | 9.1 | 15.2 |
| 50 | 34.6 | 4.7 | 30.7 | 17.6 | 19.7 |
| 55 | 47.8 | 6.2 | 35.8 | 26.4 | 24.6 |
| 60 | 55.8 | 14.6 | 36.9 | 34.8 | 29.4 |
| 65 | 62.3 | 10.4 | 34.7 | 40.7 | 34.6 |
| 70 | 67.9 | 11.5 | 39.5 | 45.8 | 28.5 |
| 75 | 74.6 | 16.3 | 33.8 | 56.8 | 39.7 |
| 80 | 77.4 | 12.8 | 32.6 | 59.6 | 26.1 |
| 85 | 83.8 | 8.3 | 41.9 | 61.6 | 19.8 |
| >90 | 91.6 | 47.6 | 34.6 | 82.8 | 41.6 |
Prevalence of hesitancy (p <0.001), dribbling (p <.001), incomplete voiding (p <0.001); Weak stream (p <0.001), and nocturia (p <0.001), increased with increasing age (Pitman’s permutation test)
1 in 5 patients experienced dysuria and more than half of them considered it serious. Overall, a great majority of these patients did consider suffering from these urinary symptoms for the rest of their life as very devastating. Most patients with BPH who had undergone TURP in HUSM noted that TURP had effectively resolved most of their lower urinary tract symptoms (Table 2).
Table 2 :
LUTS in patients post TURP
| Post TURP | Nocturia | Hesitancy | Dribbling | Weak Stream | Incomplete veiding | Urgency | Frequency | Dysuria | Incontineno |
|---|---|---|---|---|---|---|---|---|---|
| Not a problem anymore | 72 | 78 | 78 | 78 | 74 | 74 | 76 | 78 | 75 |
| Symptoms are still here but much better now | 60 | 0 | 0 | 0 | 4 | 4 | 2 | 0 | 3 |
| No improvement at all | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| My condition got worse | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Conclusion
The prevalence of nocturia was high amongst BPH patients, but a was not considered serious by the majority of them, while LUTS in our BPH patients did not differ much from BPH patients in other studies. On the whole, TURP resolved most of the LUTS effectively.
Acknowledgments
This survey was presented during the 14th National Urology Conference in Eden Garden Hotel, Johor Bharu and won the prestigious Sanofi-Synthelabo Prostate Reseach Award.
References
- 1.Asplund R. Nocturia, Nocturnal polyuria, and sleep quality in the elderly. Journal of Psychosomatic Research. 2004;56:517–525. doi: 10.1016/j.jpsychores.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 2.Chute CG, Panser LA, et al. The prevalence of prostatism : a population based survey of urinary symptoms. J Urol. 1993;150:85–9. doi: 10.1016/s0022-5347(17)35405-8. [DOI] [PubMed] [Google Scholar]
- 3.Peters TJ, Kay HE. The International Continence Society ‘Benign Prostatic Hyperplasia’ study: The bothersome of urinary symptoms. J Urol. 1997;157:885–9. [PubMed] [Google Scholar]
- 4.Malmsten UGH, Milson I, Molander U, et al. urinary incontinence and lower urinary tract symptoms : an epidemiological study of men aged 45–99 years. J Urol. 1997;158:1733–1737. doi: 10.1016/s0022-5347(01)64113-2. [DOI] [PubMed] [Google Scholar]
- 5.Epstein SR, Deverka PA, Chute CG, et al. Urinary symptoms and quality of life questions indicative of obstructive prostatic hyperplasia: Result of pilot study. Urology. 38:20–6. doi: 10.1016/0090-4295(91)80194-c. [DOI] [PubMed] [Google Scholar]
- 6.Barker JC, ad Mitteness LS. Nocturia in the elderly. Gerontologist. 1988;28:99. doi: 10.1093/geront/28.1.99. [DOI] [PubMed] [Google Scholar]
- 7.Asplund R. Mortality in the elderly in relation to nocturnal micturition. BJU Int. 1999;84:297–301. doi: 10.1046/j.1464-410x.1999.00157.x. [DOI] [PubMed] [Google Scholar]