Abstract
Context: Participants in a randomized trial of traditional Chinese medicine (TCM) for temporomandibular joint dysfunction (TMD) had a linear decline in pain over 16 TCM visits.
Objective: To investigate whether reductions in pain among participants receiving TCM can be explained by increased use of pain medications, or whether use of pain medications also declined in this group.
Design: One hundred sixty-eight participants with TMD were treated with TCM or enhanced self-care according to a stepped-care design. Those for whom self-care failed were sequentially randomized to further self-care or TCM. This report includes 111 participants during their first 16 TCM visits. The initial 8 visits occurred more than once a week; participants and practitioners determined the frequency of subsequent visits.
Outcome measures: Average pain (visual analog scale, range 0–10) and morphine and aspirin dose equivalents.
Results: The sample was 87% women and the average age was 44 ± 13 years. Average pain of narcotics users (n = 21) improved by 2.73 units over 16 visits (p < 0.001). Overall narcotics use trended downward until visit 11 (−3.27 doses/week, p = 0.156), and then trended upward until week 16 (+4.29 doses/week, p = 0.264). Among those using narcotics, use of nonsteroidal anti-inflammatory drugs (NSAIDs) declined linearly over visits 1–16 (−1.94 doses/week, p = 0.002).
Among the top quartile of NSAID-only users (n = 22), average pain decreased linearly over 16 visits (−1.52 units, p = 0.036). Overall NSAID doses/week declined between visits 1 and 7 (−9.95 doses/week, p < 0.001) and then remained stable through 16 visits. NSAID use also declined among the third quartile (n = 23) and remained low and stable among the lower half (sorted by total intake) of NSAID users.
Conclusions: Among the heaviest NSAID users, we observed a short-term reduction in NSAID use that was sustained as TCM visits became less frequent. There was no indication that pain reduction during TCM treatment was influenced by drug use.
Introduction
Chronic pain management is a growing challenge for both primary care physicians and specialists.1 Many of the pharmacologic agents commonly used to manage chronic pain, such as nonsteroidal anti-inflammatory drugs (NSAIDs), have the potential for serious toxicity, including gastrointestinal bleeding and renal failure.2 In addition, recent decades have seen a large increase in the use of long-acting opiates for ongoing pain management. Yet, the long-term efficacy of these agents is poorly documented, and there is significant potential for addiction and abuse.3 Clearly, additional strategies are needed for managing chronic pain, especially behavioral and low-risk interventions with the potential to reduce or even eliminate the need for ongoing pain medication.
Some complementary and alternative medicine (CAM) interventions may be efficacious in pain management, including chiropractic manipulation4 and acupuncture.5 Although the supporting evidence for these modalities has evolved to provide a basis for wider acceptance of CAM as an adjunct to standard interventions for chronic pain, it may be that, given the magnitude of the pain management conundrum, such CAM modalities remain substantially underutilized. Several deficiencies in the supporting evidence may partially account for this phenomenon. First, although acupuncture has been studied principally as an isolated modality, in practice it is frequently offered within the context of a broader traditional Chinese medicine (TCM) multimodal intervention.6 Failure to study acupuncture within the appropriate systemic diagnostic context, and instead in isolation from other potentially synergistic modalities such as herbs and Qigong,7,8 may have produced an inherent bias in the literature. In addition, acupuncture has often been compared with sham interventions in mechanistic studies, making it difficult to estimate what if any benefit might be rendered to a patient receiving community-based, standard TCM care. Finally, although acupuncture has proven effective for many pain syndromes,9,10 the question of whether acupuncture leads to reduced use of pain medications and other potentially toxic or invasive interventions has not been adequately studied. Indeed, changes in concomitant medication use in an acupuncture trial may confound estimates of the effectiveness of acupuncture.
In our previously published phase II clinical trial of 160 women with temporomandibular joint dysfunction (TMD),6 participants assigned to TCM experienced significantly greater improvements in worst and average facial pain compared with participants assigned to specialty care.
The current data analyses come from an adequately powered randomized controlled trial of multimodal TCM care compared with a validated self-care intervention for participants with TMD,11 using a stepped-care design.12 One hundred sixty-eight TMD participants received TCM or enhanced self-care. Those for whom self-care failed were sequentially randomized to either further self-care or TCM. Previous analyses have shown a linear decline in pain over 16 TCM visits for the 121 participants allocated to TCM.13
Objective
We provide an observational analysis limited to those TMD participants who were treated with TCM. In particular, we investigate whether the reductions in pain observed in the TCM group can be explained by increased use of pain medications, or whether use of pain medications also declined in this group.
Methods
Study Design
In brief, participants who passed a phone screening were recruited, consented, and began a 4-step eligibility process that included 1) a baseline questionnaire, 2) clinical examination by a project dentist using the Research Diagnostic Criteria for Temporomandibular Disorders,14 3) a standardized diagnostic interview by the project TCM diagnostician,15 and 4) a 2-hour educational session. Interested and eligible individuals were enrolled and began participation according to a stepped-care design. Those in whom self-care failed were sequentially randomized to either further self-care or TCM. At each step, participant data were collected by telephone, allocations were made to the TCM or self-care arm, and participants were treated for another 8 weeks. This continued for 2 rounds of 8 weeks each; after the third data collection, all those who still had pain exceeding criterion were offered treatment with TCM. The TCM study protocol permitted up to 20 TCM visits. The results of the short-term randomized study (first 16 weeks) are reported elsewhere;13 here we provide an observational analysis of the average pain outcomes and medication use reported at every TCM visit, pooled across timing of initiation of TCM visits.
Study Setting and Recruitment
Participants were recruited from Tucson, AZ, and Portland, OR, and all assessments and interventions occurred at community practices. There was enthusiastic response to newspaper advertisements, because of high local interest in complementary therapies and lack of insurance coverage for TMD, which is generally considered a dental condition. All phone contact, screening, data collection, and appointment scheduling were managed through our call center in Tucson. The initial phone screening addressed eligibility with regard to TMD symptoms, age, and willingness to comply with the visit schedule. Those who were eligible were scheduled for a local consent visit, during which they completed the baseline questionnaire. They were then scheduled for the other eligibility evaluations (clinical examination by a project dentist using the Research Diagnostic Criteria for Temporomandibular Disorders; and TCM diagnostic interview by a TCM practitioner).
Participants
Inclusion criteria were age 18 to 70 years, worst facial pain ≥5, research diagnosis of TMD (based on the Research Diagnostic Criteria for Temporomandibular Disorders),14 one of 10 TCM diagnoses (that together account for 90% of cases in the earlier study),6 and completion of TMD education. Exclusion criteria, evaluated at the consent interview or TMD clinical evaluation, included 1) serious pathology of the temporomandibular joint; cancer or acute infection of the teeth, ears, eyes, nose, or throat, or ongoing orthodontic treatment; 2) serious psychiatric conditions; 3) surgical implants for treatment of TMD; 4) bleeding disorders; 5) other life-threatening conditions, eg cancer, or uncontrolled severe hypertension; 6) severe joint/disk displacement; 7) full dentures; 8) medications for which study herbs are contraindicated; and 9) current pregnancy or plans to become pregnant during active treatment, because pregnancy would require different treatment approaches that are outside the scope of this study.
Study dentists attended training sessions by one of the investigators (S Dworkin) to improve inter-rater reliability (calibration) and were recalibrated midway through the study. TCM diagnosticians and practitioners were calibrated for TCM diagnosis by another investigator (S Mist) and recalibrated midway through the study.15 TCM diagnosticians, one per city, participated throughout the entire study.
All eligible subjects participated in a two-hour class on the nature of TMD, its patterns of progression and nonprogression, precipitating and relieving factors, and suggestions to improve jaw relaxation. If still interested, participants advanced to on-study status and the first on-study data collection.
Interventions
The TCM intervention protocol, developed in a previous study6 to provide the best individualized TCM care within the confines of a research study, included acupuncture, moxibustion, Chinese herbs, massage (Tuina), and lifestyle and nutrition counseling. Briefly, participants were permitted 20 acupuncture visits and 20 weeks of herbs within a one-year period from the first treatment visit. The initial 8 visits occurred more than once a week; participants and practitioners determined the frequency of subsequent visits. This was intended to permit the treatment schedule to adjust to remissions and flare-ups throughout the year. The practitioner's initial diagnostic assessment of each participant included a detailed history, radial pulse assessment, and tongue examination. This diagnosis, which benefited from interpractitioner calibration,15 guided lifestyle recommendations and the selection of acupuncture points and herbal formulas.
Acupuncture treatments included a core set of points congruent with those identified in the literature,16 supplemented by diagnosis-specific points, not to exceed 20 points per visit. Herbal formulas were based on a core formula for each diagnosis that could be modified according to individual presentation. Practitioners documented the exact formulation prepared on each occasion, and participants were asked to keep a log of their herbal ingestion. The herbal protocol was submitted to the US Food and Drug Administration (FDA) as an investigational new drug (IND) application. The FDA determined that the trial design was not targeted at a specific formula for a specific indication and approved the protocol exclusively for evaluation of safety. All herbs were granules (Mayway Corporation; Oakland, CA). They were GMP (Good Manufacturing Practices) certified. Samples were retained from each lot for examination if problems were detected (none were). Per FDA requirements for investigational new drug approval, participants underwent laboratory tests for aspartate aminotransferase, alanine aminotransferase, total bilirubin, creatinine, blood urea nitrogen, INR (protime), complete blood count, and urinalysis upon assignment to the TCM protocol. Laboratory tests were repeated twice, at 6 weeks and at 1 year after beginning TCM treatment. Study Medical Directors at each site reviewed laboratory test results for out-of-range values and provided guidance to the principal investigator and (when needed) participants when any remediation or additional treatment was necessary.
… using data reported at treatment visits … permits us to directly relate changes in pain and medication use to treatment visits.
Traditional Chinese Medicine Practitioner Qualifications and Training
The eight TCM practitioners who provided treatment (four at each site) had a minimum of five years' experience with acupuncture and herbs; the two diagnosing practitioners each had more than ten years' experience and were faculty members at collaborating TCM schools. Practitioners met in person or by conference call every three months with S Mist to review the protocol and discuss any unusual circumstances that were encountered.15
Outcome Measures
Self-reported data were collected via study-administered questionnaires at prescribed intervals as well as at every treatment visit. We report the pain and medication data collected at each treatment visit. Participants completed standard self-report forms before the start of every visit, and the forms were immediately available for review by the practitioners. Participants summarized their pain and medication use over the past week. They rated their average pain when having pain on a visual analog scale with a range of 0 to 10, and reported use of “any medications for your pain” (not further defined). Reported data for pain medication were the name of the medication, amount per pill, pills per day, and number of days used in the past week. In the data analysis phase, all drugs were converted to their generic formulas. For aspirin, NSAID, and acetaminophen, we used the amount per pill, pills per day, and days per week to determine medication dose/week, which we then converted to equivalent weekly doses of aspirin (one dose of aspirin = 325 mg). For narcotic analgesics, we converted similar drug-specific intake into equivalent weekly doses of oral morphine (one dose of morphine = 7.5 mg). The advantage of using data reported at treatment visits is that they were collected much more frequently than the standard study-administered questionnaires; they therefore permit us to directly relate changes in pain and medication use to treatment visits. We report the first 16 visits, because 70% of participants made 16 or more visits, but sample sizes decrease and point estimates become increasingly unstable beyond 16 visits.
Statistical Methods
Trajectories of average pain, narcotics use, and NSAID use were analyzed over the first 16 TCM visits. Since the trends in average pain were linear, ordinary linear regression of pain on visit number was used, with random effects terms that took into account within-participant correlation. In contrast, medication use had a highly positively skewed distribution within each visit, so medication doses were analyzed using the same approach, after log transformation (ln [1 + x]). Moreover, the trajectories of medication use were either flat or included an early drop followed by a rise. Consequently, the dose outcomes were analyzed using a quadratic spline, with one quadratic to model the early fall and a second to model the later rise, and with the knot near the minimum drug dose. Fitted values were transformed back to the original scale (x –> exp[x] - 1) for plotting and interpretation. All reported average doses were geometric mean doses, computed on the transformed scale and then untransformed, and changes over several visits were estimated from the fitted regressions, again untransformed back to the original scale. All analyses were carried out with Stata (version 9; College Station, TX).
Study Approvals and Safety
The human subjects protection programs at the University of Arizona and the Oregon College of Oriental Medicine approved all procedures affecting participants. The Office of Clinical and Regulatory Affairs at the National Center for Complementary and Alternative Medicine approved the overall protocol. The herbal protocol operated under investigational new drug status through the FDA. The study was run under the guidance of the Data and Safety Monitoring Board, an independent body that met twice yearly and reported its deliberations and findings to the study team, the National Center for Complementary and Alternative Medicine, and the institutional review boards. Protocols for reporting and adjudicating adverse events were approved by the institutional review boards and the Data and Safety Monitoring Board and were in place at both study sites.
Results
Descriptive Baseline Data
TCM treatment was provided to 121 participants; sufficient data were available for 111 (Figure 1). We classified the 111 participants as narcotics users (who reported use during TCM visits, n = 21) or NSAID users (who reported use of NSAID but not narcotics during TCM visits, n = 90). Table 1 summarizes overall and group-specific demographics and pain history at baseline. The overall average and standard deviation of pain before the first TCM treatment visit was 5.2 ± 1.9. Throughout all the visits, participants reported using a wide variety of medications for their pain (Table 2).
Figure 1.
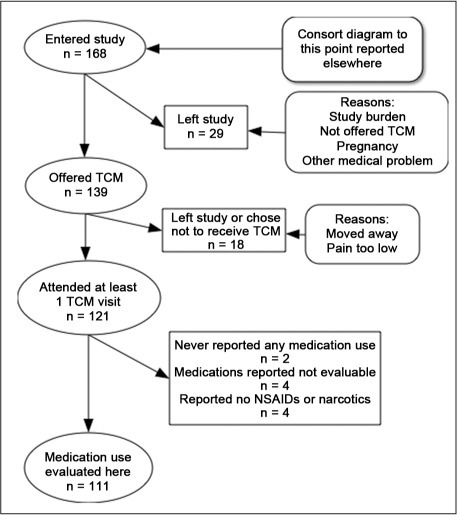
Consort diagram.
NSAID = nonsteroidal anti-inflammatory drugs; TCM = traditional Chinese medicine.
Table 1.
Baseline demographics and pain history for patients with TMD using narcotics or NSAID
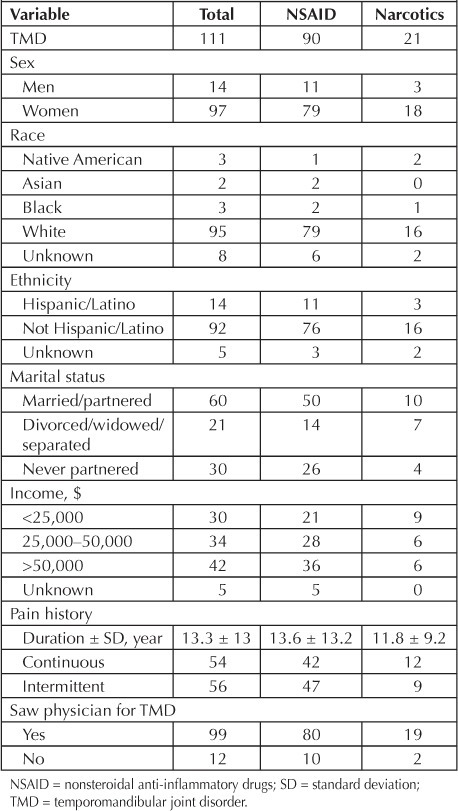
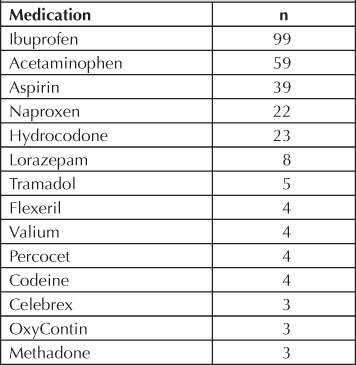
Table 2.
Medications reported by 111 participants at baseline or during traditional Chinese medicine treatment
Participants Using Narcotics
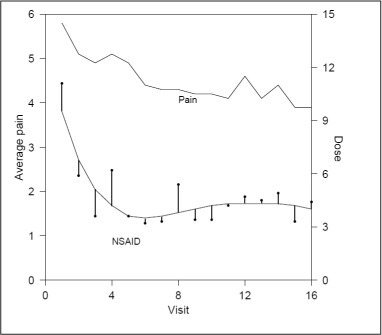
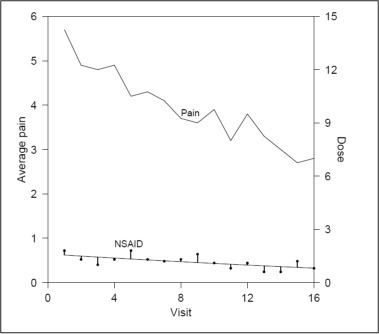
For the 21 narcotics users, average pain at the first TCM visit was 5.7 ± 2.0 (standard deviation [SD]). The fitted geometric mean narcotics dose at the first treatment visit was 6.0 morphine dose equivalents (dose equivalent = 7.5 mg morphine). The average pain scores and smoothed trajectories of mean narcotics use across 16 TCM visits are shown in Figure 2. Average pain decreased at the rate of −0.16 units per visit (p < 0.001), for a total decrease of −2.73 (48%) over 16 visits. Although there were no significant changes in narcotics use from visit 1 through visit 16, the best-fitting model shows narcotics use trending downward until about visit 11 (the knot for the quadratic spline), for a change of −3.27 (p = 0.156) morphine dose equivalents per week, and then trending upward across visits 11 to 16 (+4.29, p = 0.264). Methadone use among the 3 methadone users remained static. NSAID use among these same participants declined linearly, with a decrease of 1.94 doses from 2.5 doses (fitted geometric mean) over the 16 visits (p = 0.002, Figure 3).
Figure 2.
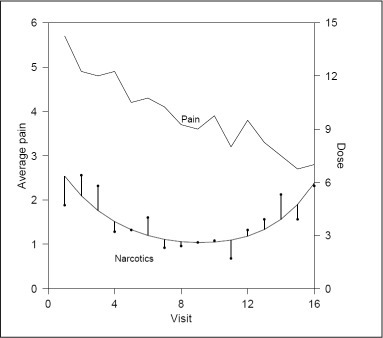
Changes in pain (upper line) and narcotics dosages (lower line) per week among participants ever using narcotics (n = 21).
Figure 3.
Changes in pain (upper line) and NSAID dosages (lower line) per week among participants ever using narcotics (n = 21).
NSAID = nonsteroidal anti-inflammatory drugs.
Participants Using Nonsteroidal Anti-Inflammatory Drugs Only
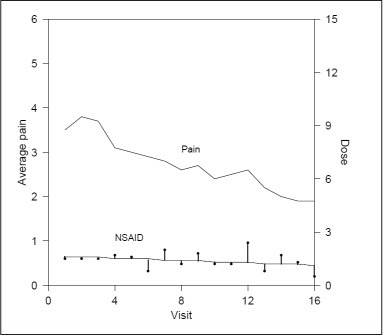
The distribution of NSAID use was also highly skewed, with many participants reporting little or no use at baseline. The fitted geometric mean weekly NSAID doses corresponding to the midpoints of the top (fourth) quartile (n = 22) and third quartile (n = 23) and the lower half of the distribution (n = 45) at the start of TCM treatment were 13.2, 2.4, and 1.3 doses, respectively (1 NSAID dose equivalent = 325 mg aspirin). Figure 4 shows the changes in pain and NSAID use for the 22 participants in the fourth quartile of NSAID use at start of treatment. Average pain before TCM was 5.9 ± 1.9 (SD) and declined linearly across 16 visits (−1.52, p = 0.036 [26%]). The minimum mean NSAID dose was taken to occur near visit 7 for the spline analysis. Drug use dropped by 9.95 doses/week (p < 0.001) across visits 1 to 7 and was stable for the remaining visits (overall increase of 0.49 doses/week from visit 7 through 16, p = 0.567). Significant declines in average pain over 16 visits were also seen in the third quartile (−2.08 units, p < 0.001 [65%]) and in the lower half (−1.39 units, p < 0.001 [34%]) of participants reporting NSAID use at the first visit. Average NSAID use for those in the third quartile also decreased linearly and significantly (−1.60 doses/week, p = 0.001, Figure 5). NSAID use did not change among those in the lower half of the distribution.
Figure 4.
Changes in pain (upper line) and NSAID dosages (lower line) per week among participants in the highest quartile of NSAID use (n = 22).
NSAID = nonsteroidal anti-inflammatory drugs.
Figure 5.
Changes in pain (upper line) and NSAIDs dosages (lower line) per week among participants in the 3rd quartile of NSAID use (n = 23).
NSAID = nonsteroidal anti-inflammatory drugs.
Discussion
Clinicians are under increasing pressure to curtail prescriptions for chronic pain medications. In the case of opiates, there are concerns about potential habituation and even diversion of drugs. NSAIDs can often be contraindicated in the presence of cardiovascular, renal, or gastrointestinal disease. Withdrawal of pain medication, however, can be difficult when the patient is indeed suffering from chronic pain. Viable, effective alternatives, possibly including behavioral modalities and CAM therapies, are needed. Paradoxically, although health care organizations advocate for reduced pain medication use, a major obstacle to this transition can be the very structure of the health benefits provided to patients. Chronic drug therapy is commonly covered by benefits, whereas behavioral, CAM, or self-care interventions may have severe benefit limitations, or not be covered at all. This pattern provides strong economic and cultural incentives for the clinician and patient to favor drug therapy. A frequently cited justification for this pattern of coverage is lack of evidence supporting CAM interventions. Even when clinical evidence for efficacy exists (eg, acupuncture5,10 for back pain), it has been difficult to document concurrent reductions in use of traditional medication or other clinical resources as economic justification.
In this paper we provide preliminary evidence that whole-system TCM care may be associated with reductions in pain medication use among participants with chronic pain and TMD. Average pain decreased in association with TCM care for the overall study sample and for all subgroups. The improvements in pain cannot be attributed to increased medication use. Indeed, some medication use appeared to decrease over the course of treatment. Average narcotics use appeared to decrease during the early period of TCM treatment, when TCM visits were most frequent. This decline was offset during the later period of treatment, when TCM visits grew less frequent. In contrast, the substantial early decline in NSAID use among the heaviest users was essentially sustained through 16 visits. This finding is, potentially, of clinical significance in view of the high toxicity profile of NSAID agents, and the costs associated with managing gastrointestinal bleeding and other complications. This study was not explicitly designed to evaluate reductions in medication usage. However, the data suggest that TCM may contribute to reductions in both pain and pain medication use, at least during active treatment. The findings also warrant further research on the integration of TCM into efforts to reduce pain medication.
This study has multiple limitations, and the results are considered indicative rather than definitive. Although the data were collected within the context of a randomized controlled trial, the analyses presented here pertain only to TCM treatment, because the corresponding self-care comparison groups could not be followed up for 16 visits. This is because of the nature of the treatment and the stepped-care design. It is thus possible that the patterns of change in medication use are attributable to the Hawthorne effect (the participants' response to observation and assessment), to some other study-induced effect, or to the natural course of TMD. Although our data suggest that medication use decreased early in the course of TCM treatment, data from the standardized questionnaire may indicate whether these changes persisted beyond the conclusion of therapy. At this time there appear to be few cures for chronic pain, and long-term TCM maintenance therapy may be an option for some patients. This issue is outside the scope of the present study.
Finally, drug use data were based soley upon participant self-report. These data were ambiguous for a few participants, and their reliability is uncertain. For these reasons, results should be interpreted with caution. Further research in more controlled settings, such as within health maintenance organizations and integrative care clinics, is warranted.
Conclusion
Pain reported by TMD participants at TCM treatment visits declined linearly over the treatment period of 16 visits. Changes in reported pain medication use cannot explain the pain reduction. Among narcotics users, pain declined while narcotic drug use remained steady. Among heavier NSAID users, there was clear evidence of a sharp decline in NSAID use followed by a plateau, with NSAID use remaining substantially below baseline for up to 16 weeks.
Disclosure
Clinical Trials Identifier #: NCT00856167. This work was funded by a grant (U01-AT002570) from the National Center for Complementary and Alternative Medicine, National Institutes of Health. The author(s) have no other conflicts of interest to disclose.
Acknowledgments
Leslie Parker, ELS, provided editorial assistance.
References
- 1.Verhaak PF, Kerssens JJ, Dekker J, Sorbi MJ, Bensing JM. Prevalence of chronic benign pain disorder among adults: a review of the literature. Pain. 1998 Sep;77(3):231–9. doi: 10.1016/S0304-3959(98)00117-1. [DOI] [PubMed] [Google Scholar]
- 2.Beebe FA, Barkin RL, Barkin S. A clinical and pharmacologic review of skeletal muscle relaxants for musculoskeletal conditions. Am J Ther. 2005 Mar–Apr;12(2):151–71. doi: 10.1097/01.mjt.0000134786.50087.d8. [DOI] [PubMed] [Google Scholar]
- 3.Von Korff M, Kolodny A, Deyo RA, Chou R. Long-term opioid therapy reconsidered. Ann Intern Med. 2011 Sep 6;155(5):325–8. doi: 10.1059/0003-4819-155-5-201109060-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cherkin DC, Deyo RA, Battié M, Street J, Barlow W. A comparison of physical therapy, chiropractic manipulation, and provision of an educational booklet for the treatment of patients with low back pain. N Engl J Med. 1998 Oct 8;339(15):1021–9. doi: 10.1056/NEJM199810083391502. [DOI] [PubMed] [Google Scholar]
- 5.Cherkin DC, Sherman KJ, Avins AL, et al. A randomized trial comparing acupuncture, simulated acupuncture, and usual care for chronic low back pain. Arch Intern Med. 2009 May 11;169(9):858–66. doi: 10.1001/archinternmed.2009.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ritenbaugh C, Hammerschlag R, Calabrese C, et al. A pilot whole systems clinical trial of traditional Chinese medicine and naturopathic medicine for the treatment of temporomandibular disorders. J Altern Complement Med. 2008 Jun;14(5):475–87. doi: 10.1089/acm.2007.0738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elder C, Aickin M, Bell IR, et al. Methodological challenges in whole systems research. J Altern Complement Med. 2006 Nov;12(9):843–50. doi: 10.1089/acm.2006.12.843. [DOI] [PubMed] [Google Scholar]
- 8.Ritenbaugh C, Verhoef M, Fleishman S, Boon H, Leis A. Whole systems research: a discipline for studying complementary and alternative medicine. Altern Ther Health Med. 2003 Jul–Aug;9(4):32–6. [PubMed] [Google Scholar]
- 9.Witt C, Brinkhaus B, Jena S, et al. Acupuncture in patients with osteoarthritis of the knee: a randomised trial. Lancet. 2005 Jul 9–15;366(9480):136–43. doi: 10.1016/S0140-6736(05)66871-7. [DOI] [PubMed] [Google Scholar]
- 10.Witt CM, Jena S, Selim D, et al. Pragmatic randomized trial evaluating the clinical and economic effectiveness of acupuncture for chronic low back pain. Am J Epidemiol. 2006 Sep 1;164(5):487–96. doi: 10.1093/aje/kwj224. [DOI] [PubMed] [Google Scholar]
- 11.Dworkin SF, Huggins KH, Wilson L, et al. A randomized clinical trial using research diagnostic criteria for temporomandibular disorders-axis II to target clinic cases for a tailored self-care TMD treatment program. J Orofac Pain. 2002 Winter;16(1):48–63. [PubMed] [Google Scholar]
- 12.Huggins KH, Truelove E, Mancl L, LeResche L, Dworkin SF. RCT for TMD utilizing case manager: long term clinical findings (Abstract) J Dent Res. 2004;83:133. [Google Scholar]
- 13.Ritenbaugh C, Aickin M, Hammerschlag R, Mist S. The impact of US-based traditional Chinese medicine on TMD: a phase II whole systems trial (Abstract) J Tradit Chin Med. 2011;31:10–1. [Google Scholar]
- 14.Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992 Fall;6(4):301–55. [PubMed] [Google Scholar]
- 15.Mist S, Ritenbaugh C, Aickin M. Effects of questionnaire-based diagnosis and training on inter-rater reliability among practitioners of traditional Chinese medicine. J Altern Complement Med. 2009 Jul;15(7):703–9. doi: 10.1089/acm.2008.0488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosted P. Practical recommendations for the use of acupuncture in the treatment of temporomandibular disorders based on the outcome of published controlled studies. Oral Dis. 2001 Mar;7(2):109–15. [PubMed] [Google Scholar]


