Abstract
Objective
Family history contributes to risk for many common chronic diseases. Little research has investigated patient factors affecting communication of this information.
Methods
1061 adult community health center patients were surveyed. We examined factors related to frequency of discussions about family health history (FHH) with family members and doctors.
Results
Patients who talked frequently with family members about FHH were more likely to report a family history of cancer (p=.012) and heart disease (p<.001), seek health information frequently in newspapers (p<.001) and in general (p<.001), and be female (p<.001). Patients who talked frequently with doctors about FHH were more likely to report a family history of heart disease (p=.011), meet physical activity recommendations (p=.022), seek health information frequently in newspapers (p<.001) and in general (p<.001), be female (p<.001), and not have experienced racial discrimination in healthcare (p<.001).
Conclusion
Patients with a family history of some diseases, those not meeting physical activity recommendations, and those who do not frequently seek health information may not have ongoing FHH discussions.
Practice Implications
Interventions are needed to encourage providers to update patients’ family histories systematically and assist patients in initiating FHH conversations in order to use this information for disease prevention and control.
Keywords: Provider-patient communication, family history, health information seeking
1. Introduction
Family history is an important contributing risk factor for many common chronic diseases, reflecting shared genetic, behavioral, and environmental risk [1, 2]. Diseases that affect millions of U.S. adults (e.g., cardiovascular disease, diabetes, several cancers) are all influenced by family history [3–9]. For most common, chronic conditions, a moderate familial risk increases disease risk about two-fold compared to a weak familial risk; this figure rises to a three-fold or higher increase for those with a strong familial risk when compared to a weak familial risk [2, 10]. Although family history information has most often been used for risk assessments for rare, highly penetrant, hereditary conditions, this information may have the greatest impact when used for common diseases in population-based settings [11, 12]. Currently, family history can guide medical care (e.g., screening recommendations) for common conditions including diabetes, coronary heart disease, stroke, and several cancers [13, 14, 15]. Targeting disease prevention initiatives in primary care toward those with a moderate or strong familial risk may be an effective approach that could supplement initiatives targeting the general population [16–18].
The pathway by which family history information could be used in primary care for disease prevention is based on two domains of communication behaviors: patients’ collection of family health history (FHH) information from family members and discussion of the information with health care providers (see Figure 1). Optimally, such conversations would be repeated over time to develop and update an in-depth FHH. Research on communication about FHH information has mainly focused on provider and health care system factors that affect provider-patient communication. Prior research has shown that physicians often do not collect adequate FHH information from patients [19–21], and even those in primary care who believe that collection of family history information is important spend little time on this activity [22]. Most FHH information is collected in new patient visits, and this information is generally not discussed in subsequent visits [23, 24]. Potential barriers affecting provider-patient communication about FHH have been identified, including visit length, reimbursement criteria, and provider training, knowledge and skills [25–27].
Figure 1.
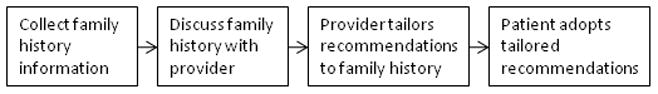
Steps to using family history information in primary care
However, less research has examined patient factors that affect communication about FHH with providers or with family members over time. The results of a national survey of U.S. adults showed that women, Whites, those with a personal history of diabetes, and those with higher educational attainment were more likely to engage in active collection of FHH information from family members [1]. Social network research conducted within families at high genetic risk of cancer has shown that women are more likely to gather health information [28], but limited research has considered this communication as an ongoing process.
A number of different patient factors could affect communication about FHH with family members or health care providers. Patients at increased risk of disease based on their family history or behavioral risk factors might be more likely to have such conversations in order to discuss possible disease prevention or control strategies [28, 29]. Health information seeking may also be related to these communication behaviors. Prior research based on a national sample of U.S. adults has shown that those who believed that knowledge of family history or genes could reduce cancer risk were more likely to have searched for cancer information [30], but the relationship between health information seeking and FHH communication behaviors has not been systematically investigated. In addition, the role of patient characteristics, such as race/ethnicity and gender, that are known to affect provider-patient communication related to other health topics [31–36], needs to be explored further. Research is also needed to examine factors affecting communication about FHH in diverse, underserved populations.
This study was therefore designed to examine predictors of communication about FHH with family members and doctors among a medically underserved population. We examined whether family history of chronic disease, behavioral risk factors, health information seeking behaviors, and patient characteristics were related to frequency of communication about FHH with family members and with doctors. We hypothesized that those with a family history of chronic disease, those at greater behavioral risk, more frequent health information seekers, and patients who were female, younger, and more highly educated would engage in these communication behaviors more frequently. Understanding how patient factors affect frequency of communication about FHH is critical to using this information effectively in disease prevention.
2. Methods
2.1. Data collection
For this study, we administered a cross-sectional survey to a diverse patient population. We approached patients in the waiting rooms of eight community health centers located in medically underserved areas. These community health centers serve as safety net providers of health care, accepting Medicaid and providing no/low-cost care on a sliding scale for uninsured/underinsured patients. Surveys were administered at each of the health centers on different days of the week and at different times of the day based on a rotating schedule. Trained data collectors approached all patients in the waiting room while they were at the health center and asked them to complete a survey in either English or Spanish. Inclusion criteria were that patients be at least 18 years old and speak either English or Spanish. Approximately 65% of patients who were approached agreed to complete the survey. Of the 1,318 patients who agreed to participate, 1,061 (81%) completed all components of the survey; there were no significant differences in demographic characteristics between individuals with complete surveys and those with incomplete surveys. This study was approved by the Stony Brook University Committee on Research Involving Human Subjects, the Suffolk County Department of Health Services Institutional Review Board, and the National Institutes of Health Office of Human Subjects Research.
2.2. Measures
2.2.1. Outcome variables
Frequency of family health history discussions
We assessed how frequently patients talked with family members and with doctors about family health history using two Likert-scale items (e.g., “I talk with family members about our family health history: Not at all/not very often/somewhat often/very often”).
2.2.2. Predictor variables
Family history of chronic disease
We assessed family history of diabetes, heart disease and cancer with three items (“Does heart disease run in your family? yes/no/don’t know”) [37]. Responses of “no” and “don’t know” were combined for analyses.
Behavioral risk factors
We created a continuous measure of body mass index (BMI) based on self-reported height and weight. We characterized patients’ weight perceptions using one item (“Do you consider yourself to be at an average weight, underweight, or overweight?”) Physical activity was assessed using the activity scale of the Rapid Assessment of Physical Activity, which is a 7-item validated measure that asks patients to report their level and intensity of physical activity [38]. For analyses, respondents were classified as “active” (i.e., meeting current physical activity recommendations) vs. non-active.
Health information seeking
We assessed patients’ health information seeking through different media (i.e., newspaper, television, and Internet) using three items adapted from the Health Information National Trends Survey [39] (e.g., “In the past 12 months, how often have you watched health segments on local news? Would you say every day, several days a week, 2 or 3 times per month, about once a month, 5 to 10 times a year, less than 5 times a year”). In analyses, this measure was dichotomized as every day/several days a week vs. less frequent. We also asked patients about health information seeking in general using the item: “In the past 30 days, how often would you say you have looked for information about ways to stay healthy or to feel better? Would you say very often, somewhat often, not very often, not at all” [39]. This item was dichotomized (very often/somewhat often vs. less frequently) in analyses.
Racial discrimination in health care
We asked about patients’ perceptions of racial discrimination in health care using the Behavioral Risk Factor Surveillance System (BRFSS) item “Within the past 12 months, when seeking health care, do you feel your experiences were: worse than other races; the same as other races; better than other races; worse than some races, better than others” [40]. This item was dichotomized as worse than other races vs. other categories in analyses.
Patient characteristics
Health literacy was assessed using the Newest Vital Sign (NVS), a six-item measure requiring reading comprehension and numeracy skills [41, 42]. Participants received a score from 0 to 6 based on number of correct answers: scores from 0–1 reflect a high likelihood of limited literacy, 2–3 a possibility of limited literacy and 4–6 adequate health literacy [41]. We also asked patients to report their educational attainment, age, race/ethnicity, and gender. In analyses, educational attainment was categorized as less than high school; high school degree/GED/some college; or college degree or higher, and race/ethnicity as Black; White; Hispanic; or other. Age was treated as continuous.
2.2.3. Covariates
We assessed whether patients had a personal diagnosis of diabetes, heart disease, or cancer using three items (e.g., “Has a doctor ever told you that you have diabetes?”). We also recorded the language in which the survey was completed and country of birth.
2.3. Statistical analysis
Descriptive statistics were examined for all variables. Bivariate analyses were conducted to examine the associations between each outcome variable and possible predictor variables and covariates using chi-square tests and univariate logistic regression models. Possible predictors of frequency of discussion about FHH with family members and doctors (i.e., family history, behavioral risk factors, health information seeking, health care experiences, patient characteristics) were identified from a theoretical model of risk information seeking and processing [43] and prior empirical research on provider-patient communication and family health history, as described above. We then built two multivariable logistic regression models to examine the independent contributions of predictor variables found to have significant bivariate associations with the outcome variables. The outcome variables were dichotomized in the logistic regression models (very often/somewhat often vs. not very often/not at all). Data were analyzed using Stata 10 (College Station, TX: StataCorp LP 2007) and SAS/STAT® 9.2 for Windows (Cary, NC). Statistical significance was assessed as p<0.05.
3. Results
The majority of patients were female (75%) and 51% were 35 years of age or older (see Table 1). About 26% self identified as being non-Hispanic White, 31% as non-Hispanic Black, and 35% as Hispanic. A majority (60%) had been born in the U.S. Although 83% had at least a high school degree or GED, only 34% had adequate health literacy as measured by the NVS. A larger proportion had been diagnosed with diabetes (14%) than with heart disease (10%) or cancer (6%). More than half (57%) of patients reported that they had a family history of diabetes, while 41% reported a family history of heart disease and 44% a family history of cancer.
Table 1.
Characteristics of participating community health center patients.
| Variable | N (%) |
|---|---|
| Family history | |
| Diabetes (n=1052) | 604 (57.4) |
| Heart disease (n=1047) | 429 (41.0) |
| Cancer (n=1040) | 458 (44.0) |
| Personal diagnosis | |
| Diabetes (n=1056) | 148 (14.0) |
| Heart disease (n=1038) | 107 (10.3) |
| Cancer (n=1039) | 60 (5.8) |
| Education (n=1038) | |
| Less than high school degree | 182 (17.5) |
| High school degree/GED or some college | 724 (69.8) |
| College degree or higher | 132 (12.7) |
| Gender (n=1048) | |
| Male | 266 (25.4) |
| Female | 782 (74.6) |
| Age (n=1016) | |
| Less than 35 | 495 (48.7) |
| 35 or greater | 521 (51.3) |
| Race/ethnicity (n=1006) | |
| White, non-Hispanic | 266 (26.4) |
| Black, non-Hispanic | 307 (30.5) |
| Hispanic | 347 (34.5) |
| Other | 86 (8.5) |
| Health literacy (n=1015) | |
| High likelihood of limited health literacy | 307 (30.3) |
| Possibility of limited health literacy | 362 (35.7) |
| Adequate health literacy | 346 (34.1) |
| Country of birth (n=1061) | |
| USA | 637 (60.0) |
| Outside USA | 424 (40.0) |
| Language of survey administration (n=1061) | |
| English | 873 (82.3) |
| Spanish | 188 (17.7) |
3.1. Discussion with family members
Overall, about 66% reported talking with family members about FHH somewhat or very often, only 9% said not at all (data not shown). Fifty-eight percent reported talking with a doctor somewhat or very often about FHH. As shown in Table 2, in bivariate analyses, those with a family history of diabetes (p=.002), heart disease (p<.001), and cancer (p<.001) were more likely to report talking frequently with family members about FHH. Patients who met physical activity recommendations reported talking more frequently with family members about FHH (p=.002). Patients who frequently sought health information through newspaper (p<.001), television (p<.001), and Internet sources (p=.004) were also more likely to report talking frequently with family members about FHH, as were those who frequently looked for health information in general (p<.001). Females (p<.001), those with higher educational attainment (p=.043), and those who were younger (p=.035) were more likely to frequently talk with family members about FHH. Experiences with racial discrimination in health care were not significantly associated with this outcome.
Table 2.
Bivariate associations between predictor variables and frequency of discussion about family health history with family members and doctors.
| Talking frequently with family members | Talking frequently with doctors | |||
|---|---|---|---|---|
| χ2 or t value | p-value | χ2 or t value | p-value | |
| Family history | ||||
| Diabetes | 10.0 | 0.002 | 5.3 | 0.022 |
| Heart disease | 14.9 | <0.001 | 6.8 | 0.009 |
| Cancer | 15.7 | <0.001 | 15.1 | <0.001 |
| Behavioral risk factors | ||||
| Body mass index | −0.20 | 0.84 | −0.29 | 0.77 |
| Perceived overweight | 0.22 | 0.64 | 0.17 | 0.68 |
| Meeting physical activity recommendations | 9.9 | 0.002 | 6.7 | 0.010 |
| Health information seeking | ||||
| Newspaper | 27.1 | <0.001 | 34.3 | <0.001 |
| Television | 18.1 | <0.001 | 22.8 | <0.001 |
| Internet | 8.5 | 0.004 | 6.2 | 0.012 |
| General | 62.3 | <0.001 | 55.9 | <0.001 |
| Health care discrimination | 0.04 | 0.84 | 3.6 | 0.059 |
| Patient characteristics | ||||
| Health literacy | 0.24 | 0.89 | 3.5 | 0.17 |
| Education | 6.3 | 0.043 | 1.6 | 0.44 |
| Age | −2.1 | 0.035 | −2.2 | 0.028 |
| Race/ethnicity | 0.51 | 0.92 | 1.8 | 0.60 |
| Female | 27.4 | <0.001 | 19.0 | <0.001 |
| Covariates | ||||
| Diagnosis of diabetes | 0.16 | 0.69 | 4.3 | 0.037 |
| Diagnosis of heart disease | 2.2 | 0.14 | 8.1 | 0.004 |
| Disease of cancer | 0.14 | 0.71 | 0.11 | 0.74 |
| Survey language | 0.18 | 0.67 | 0.29 | 0.59 |
| Country of birth | 0.02 | 0.88 | 0.75 | 0.78 |
In a multivariable model, talking frequently with family members about FHH was associated with reporting a family history of cancer (OR: 1.50; 95% CI: 1.09, 2.05) and a family history of heart disease (OR: 1.52; 95% CI: 1.10, 2.08), but not a family history of diabetes (see Table 3). Those who had frequently sought health information in newspapers (OR: 1.89; 95% CI: 1.30, 2.73) or in general (OR: 2.45; 95% CI: 1.75, 3.44) were also more likely to report talking frequently with family members about FHH. Women were more likely to talk frequently with family members about FHH than men (OR: 1.98; 95% CI: 1.42, 2.77).
Table 3.
Predictors of talking frequently with family members about family health history in a multivariable model (n=881).
| Variable | Odds ratio | 95% confidence interval | p-value |
|---|---|---|---|
| Family history | |||
| Cancer | 1.50 | (1.09, 2.05) | 0.012 |
| Heart disease | 1.52 | (1.10, 2.08) | 0.010 |
| Health information seeking | |||
| Newspaper | 1.89 | (1.30, 2.73) | 0.010 |
| General | 2.45 | (1.75, 3.44) | <0.001 |
| Gendera | 1.98 | (1.42, 2.77) | <0.001 |
| Age | 1.00 | (0.99, 1.01) | 0.74 |
| Educational attainmentb | |||
| Less than high school degree | 0.72 | (0.46, 1.10) | 0.23 |
| High school degree/GED or some college | 0.84 | (0.60, 1.16) | 0.94 |
| Race/ethnicityc | |||
| White | 0.91 | (0.51, 1.65) | 0.29 |
| Black | 1.13 | (0.64, 2.01) | 0.62 |
| Hispanic | 1.22 | (0.69, 2.16) | 0.29 |
Male is comparison category
College degree or higher is comparison category
“Other” is comparison category
3.2. Discussion with doctors
In bivariate analyses, a similar pattern was observed for the outcome variable of talking frequently with doctors about FHH (see Table 2). Patients with a family history of diabetes (p=.022), heart disease (p=.009), and cancer (p<.001) were more likely to report talking frequently with doctors about FHH. Patients who met physical activity recommendations reported talking more frequently with doctors about FHH (p=.010). This outcome was also significantly associated with having frequently sought health information through newspaper (p<.001), television (p<.001), and Internet sources (p=.0012) and with frequently looking for health information in general (p<.001). Females (p<.001) and younger patients (p=.028) were more likely to talk frequently with doctors about FHH. There was a marginal association with experiences of racial discrimination in health care (p=.059).
As shown in Table 4, in a multivariable model, talking frequently with doctors about FHH was associated with reporting a family history of heart disease (OR: 1.66; 95% CI: 1.22, 2.24), but not a family history of cancer or of diabetes. Patients who reported meeting physical activity recommendations were more likely to report talking frequently with doctors than those who did not meet recommendations (OR: 1.43, 95% CI: 1.05, 1.93). Those who had frequently looked for health information in newspapers (OR: 1.96; 95% CI: 1.37, 2.82) or were more frequent health information seekers in general (OR: 2.46; 95% CI: 1.73, 3.49) were more likely to talk frequently with doctors about FHH. Women were more likely to talk frequently with doctors about FHH than men (OR: 1.86; 95% CI: 1.32, 2.60). Patients who reported experiencing racial discrimination in health care were significantly less likely to report talking frequently with doctors about FHH (OR: 0.47; 95% CI: 0.29, 0.78).
Table 4.
Predictors of talking frequently with doctors about family health history in a multivariable model (n=844).
| Variable | Odds ratio | 95% confidence interval | p-value |
|---|---|---|---|
| Family history | |||
| Heart disease | 1.66 | (1.22, 2.24) | 0.011 |
| Meeting physical activity recommendations | 1.43 | (1.05, 1.93) | 0.022 |
| Health information seeking | |||
| Newspaper | 1.96 | (1.37, 2.82) | <0.001 |
| General | 2.46 | (1.73, 3.49) | <0.001 |
| Health care discriminationa | 0.47 | (0.29, 0.78) | <0.001 |
| Genderb | 1.86 | (1.32, 2.60) | <0.001 |
“Worse than other races” compared to other categories
Male is comparison category
4. Discussion and conclusion
4.1. Discussion
The findings presented here show that multiple domains of patient factors impact frequency of discussion about FHH with family members and with doctors in a medically underserved population of community health center patients. Patients reporting a family history of heart disease talked more often about FHH with family members and doctors. In addition, reporting a family history of cancer was related to more frequent communication about FHH with family members, but not with doctors. The results therefore indicate that reporting a positive family history of diabetes prompted less conversation about FHH than did a positive family history of other common, chronic health conditions, despite the large proportion of patients with a family history of diabetes in our sample.
These family history findings are in contrast to results from the 2005 Oregon BRFSS, which showed that respondents with a positive family history of diabetes were more likely to report that their health care provider collected family history information about diabetes, discussed the risk of developing diabetes, and made dietary or exercise recommendations to reduce diabetes risk [44]. In addition, Hariri et al. (2006) found that, among non-diabetics, those with familial risk were most likely to talk with family members about diabetes [45]. The difference in results between these studies and the present study may be because of differences in populations or because our measure was intended to capture ongoing communication about FHH. It is also notable that, in our study, provider-patient communication about FHH was not related to reporting a family history of cancer, since current screening recommendations for breast, colorectal, ovarian, and prostate cancer are based at least in part on family history [15, 46]. These findings therefore suggest that strategies are needed to encourage more systematic collection and follow-up of FHH information in clinical settings in order to tailor disease prevention and screening recommendations to patients’ family history.
These findings provided partial support for our hypothesis of a relationship between behavioral risk factors and discussions of FHH with family members and with doctors. We found a relationship between physical activity and discussions of FHH with doctors, in that individuals meeting physical activity recommendations were more likely to have these discussions, but did not find a relationship between BMI or weight perceptions and this communication variable. The physical activity finding suggests that despite the advantage of family history capturing shared genetic, behavioral, and environmental risk within families [1, 2], FHH might not be used by providers to develop integrated prevention recommendations (e.g., to increase physical activity for those not meeting recommendations) based on both familial and behavioral risk. Prior research has shown that as behavioral risk increased in a sample of primary care patients, inclination toward genetic explanations also increased, while interest in how health habits affect disease risk decreased [47], suggesting that those at greatest need for behavior change may hold disease attributions that diminish their interest in receiving behavior change information. These findings, together with our results, suggest that patients at increased behavioral risk may have less inclination toward collecting and discussing FHH information.
Health information seeking in general and specifically from newspaper sources was positively related to more frequent discussions about FHH with both family members and doctors. Strikingly, health information seeking variables were more important predictors of the frequency of FHH discussions than were demographic or illness-related variables. These findings suggest that FHH may be one of many types of health information sought by those individuals who frequently search for health information. In previous research, health information seeking has been associated not only with sociodemographic, health care access, and cancer history variables [48, 49] but also with colonoscopy and prostate cancer screening behaviors [49], suggesting a possible prevention orientation to those who frequently engage in health information seeking behaviors. A recent Internet-based survey revealed that different patterns of motivations may underlie health information seeking behaviors related to wellness as compared to illness [50], indicating that it will be important to examine which type of information seeking pattern best describes health information seeking related to the domain of FHH. Patients who are interested in discussing FHH information may generally have a positive wellness orientation. Investigation of motivations for discussing FHH with family members and doctors may be a fruitful area of research in developing family history-based prevention initiatives. In addition, it may be critical to develop novel ways of motivating patients who are not frequent health information seekers to discuss FHH information.
Patients who reported having experienced racial discrimination in health care were less likely to have frequently discussed FHH with their doctors, but this variable was not related to discussions with family members. Racial and ethnic disparities in health care have been documented, and death rates for most common, chronic diseases are significantly higher among racial and ethnic minorities than among Whites [51]. Individual and institutional measures of racial discrimination have been associated with individual health status [52]. In addressing this issue, the role of culturally competent communication in reducing ethnic and racial healthcare disparities has been highlighted [53, 54]. The findings from the present study highlight the importance of developing culturally competent FHH disease prevention initiatives, an area that has not yet received sufficient attention in the family history literature. Interventions to improve provider-patient communication generally may also improve communication about FHH.
In the present study, women were more likely to discuss FHH frequently with both family members and with doctors, which is consistent with other studies of communication related to family history and genetic susceptibility information [1, 28, 55]. Gender has also been found to be a predictor of differences in provider-patient communication behaviors [56]. However, we did not observe the differences in communication by educational attainment or race/ethnicity that have been found in other studies on family history [1, 42]. This difference may be because most research on communication about family history or genetic susceptibility has not included diverse or underserved populations [57]. Factors predicting communication about FHH information may well differ in a medically underserved population of patients served by community health centers. These findings also highlight that in order to use FHH information for disease prevention on a population level, it will be critical to develop strategies to engage men.
This study had a number of limitations that should be considered in interpreting the results. First, qualitative studies have suggested that factors such as emotional closeness and personal likeness, as well as biological relatedness, may affect how individuals understand their family history of disease [58–60], and, therefore, their perceptions of their family history may differ from their objective family history. Second, our outcome variables assessed patients’ perceptions of the frequency of discussions about FHH, but we were not able to examine these conversations objectively or over time. Patients may have found it socially desirable to report having frequent discussions about family health history with their doctors or family members, or, conversely, may not have recalled some discussions about family health history, which could affect their responses about the frequency of these discussions. In addition, we were unable to examine the content of the communication occurring between patients and their family members or providers, and investigating whether these discussions are initiated by patients or providers is an important issue for future research. Third, the included measures of behavioral risk only captured a subset of possible risk factors. Fourth, because of the cross-sectional design of this study, the direction of observed associations is not clear. Fifth, while we were able to gather responses from a racially and socioeconomically diverse group of community health center patients, the results of this study may not be generalizable to other populations as factors unique to community health centers could have influenced the observed results.
4.2. Conclusion
The findings from this study indicate that having ongoing discussions about FHH with family members and doctors may be related to patients having a family history of some common chronic diseases, but not others. Those patients who are frequent health information seekers also report engaging in conversations about FHH more frequently. However, patients who may be most in need of discussion about disease prevention and control strategies based on an increased behavioral risk (e.g., not meeting physical activity recommendations) might be less inclined to have frequent conversations about FHH. Patients who have experienced racial discrimination in health care also talk less with providers about FHH. These results therefore add to our understanding of patient factors that might affect the collection and use of FHH in disease prevention and control initiatives in primary care. Important next steps include investigating whether and how these communication behaviors affect the adoption of tailored behavioral recommendations by patients. Understanding the mechanisms that underlie how discussion of FHH information might influence downstream behaviors is essential to planning effective clinical intervention approaches that can improve the health of patients.
4.3. Practice implications
The results presented here indicate that interventions might be needed to encourage providers to follow up on patients’ family history more systematically and to assist patients in initiating these conversations with their family members and doctors. These findings suggest that it will be particularly important to target interventions to increase discussion of FHH to patients with a family history of diabetes, those who are not meeting physical activity recommendations or do not generally seek health information, and men. The results also point to the importance of developing culturally competent interventions to improve provider-patient communication about FHH. In order for FHH information to be used to tailor disease prevention and control recommendations to improve patients’ health, providers will need to discuss and update this information with patients over time and to reach those patients who might not initiate these conversations.
Acknowledgments
This research was supported by the Intramural Research Program of the National Human Genome Research Institute, National Institutes of Health. We would like to thank the Suffolk County Department of Health Services, the Health Center Administrators, the data collectors, and the patients who agreed to participate in this study.
Footnotes
Conflicts of interest
The authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Yoon PW, Scheuner MT, Gwinn M, Khoury MJ, Jorgensen C, Hariri S, Lyn S. Awareness of family history as a risk factor for disease -- United States, 2004. MMWR Morb Mortal Wkly Rep. 2004;53:1044–7. [PubMed] [Google Scholar]
- 2.Yoon PW, Scheuner MT, Jorgensen C, Khoury MJ. Developing Family Healthware, a family history screening tool to prevent common chronic diseases. Prev Chronic Dis. 2009;6:1–11. [PMC free article] [PubMed] [Google Scholar]
- 3.Fuchs C, Giovannucci E, Colditz G, Hunter D, Speizer F, Willett W. A prospective study of family history and the risk of colorectal cancer. N Engl J Med. 1994;331:1669–74. doi: 10.1056/NEJM199412223312501. [DOI] [PubMed] [Google Scholar]
- 4.Cerhan J, Parker A, Putnam S, Chiu BC, Lynch CF, Cohen MB, Torner JC, Cantor KP. Family history and prostate cancer risk in a population-based cohort of Iowa men. Cancer Epidemiol Biomarkers Prev. 1999;8:53–60. [PubMed] [Google Scholar]
- 5.Collaborative Group on Hormonal Factors in Breast Cancer. Familial breast cancer: Collaborative reanalysis of individual data from 52 epidemiological studies including 58,209 women with breast cancer and 101,986 women without the disease. Lancet. 2001;358:1389–99. doi: 10.1016/S0140-6736(01)06524-2. [DOI] [PubMed] [Google Scholar]
- 6.Johns L, Houlston R. A systematic review and meta-analysis of familial colorectal cancer risk. Am J Gastroenterol. 2001;96:2992–3003. doi: 10.1111/j.1572-0241.2001.04677.x. [DOI] [PubMed] [Google Scholar]
- 7.Pharoah P, Ponder B. The genetics of ovarian cancer. Best Pract Res Clin Obstet Gynaecol. 2002;16:449–68. doi: 10.1053/beog.2002.0296. [DOI] [PubMed] [Google Scholar]
- 8.Murabito J, Pencina M, Nam B, et al. Sibling cardiovascular disease as a risk factor for cardiovascular disease in middle-aged adults. J Am Med Assoc. 2005;294:3117–23. doi: 10.1001/jama.294.24.3117. [DOI] [PubMed] [Google Scholar]
- 9.Valdez R, Yoon PW, Liu T, Khoury MJ. Family history and prevalence of diabetes in the US population: the 6-year results from the National Health and Nutrition Examination Survey (1999–2004) Diabetes. 2007;30:2517–22. doi: 10.2337/dc07-0720. [DOI] [PubMed] [Google Scholar]
- 10.Scheuner MT, Wang S-J, Raffel LJ, Larabell SK, Rotter JI. Family history: A comprehensive genetic risk assessment method for the chronic conditions of adulthood. Am J Med Genet. 1997;71:315–24. doi: 10.1002/(sici)1096-8628(19970822)71:3<315::aid-ajmg12>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 11.Yoon PW, Scheuner MT, Khoury MJ. Research priorities for evaluating family history in the prevention of common chronic diseases. Am J Prev Med. 2003;24:128–35. doi: 10.1016/s0749-3797(02)00585-8. [DOI] [PubMed] [Google Scholar]
- 12.Yoon PW, Scheuner MT, Peterson-Oehlke KL, Gwinn M, Faucett A, Khoury MJ. Can family history be used as a tool for public health and preventive medicine? Genet Med. 2002;4(4):304–10. doi: 10.1097/00125817-200207000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Guttmacher AE, Collins FS, Carmona RH. The family history - More important than ever. N Engl J Med. 2004;351:2333–36. doi: 10.1056/NEJMsb042979. [DOI] [PubMed] [Google Scholar]
- 14.Zoorob R, Anderson R, Cefalu C, Sidani M. Cancer screening guidelines. Am Fam Physician. 2001;63:1101–12. [PubMed] [Google Scholar]
- 15.American Cancer Society. [Accessed 02/28/11];American Cancer Society guidelines for the early detection of cancer. 2010 http://www.cancer.org/docroot/ped/content/ped_2_3x_acs_cancer_detection_guidelines_36.asp.
- 16.Audrain-McGovern J, Hughes C, Patterson F. Effecting behavior change: Awareness of Family History. Am J Prev Med. 2003;24:183–9. doi: 10.1016/s0749-3797(02)00592-5. [DOI] [PubMed] [Google Scholar]
- 17.Kelly KM, Ferketich AK, Sturm AC, Porter K, Sweet K, Kemp K, Schwirian P, Westman J. Cancer risk and risk communication in urban, lower-income neighborhoods. Prev Med. 2009;48:392–6. doi: 10.1016/j.ypmed.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 18.Kaphingst KA, Lachance CR, Gepp A, D’Anna LH, Rios-Ellis B. Educating underserved Latino communities about family health history using lay health advisors. Public Health Genomics. doi: 10.1159/000272456. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schroy I, Paul S, Barrison AF, Ling BS, Wilson S, Geller AC. Family history and colorectal cancer screening: A survey of physician knowledge and practice patterns. Am J Gastroenterol. 2002;97:1031–6. doi: 10.1111/j.1572-0241.2002.05624.x. [DOI] [PubMed] [Google Scholar]
- 20.Sweet K, Bradley T, Westman JA. Identification and referral of families at high risk for cancer susceptibility. J Clin Oncol. 2002;20:528–37. doi: 10.1200/JCO.2002.20.2.528. [DOI] [PubMed] [Google Scholar]
- 21.Acton R, Burst N, LC, et al. Knowledge, attitudes, and behaviors of Alabama’s primary care physicians regarding cancer genetics. Acad Med. 2000;75:850–2. doi: 10.1097/00001888-200008000-00021. [DOI] [PubMed] [Google Scholar]
- 22.Fuller M, Myers M, Webb T, Tabangin M, Prows C. Primary care providers’ responses to patient-centered family history. J Genet Couns. 2010;19:84–96. doi: 10.1007/s10897-009-9264-6. [DOI] [PubMed] [Google Scholar]
- 23.Medalie JH, Zyzanski SJ, Langa D, Stange KC. The family in family practice: is it a reality? J Fam Pract. 1998;46:390–6. [PubMed] [Google Scholar]
- 24.Acheson LS, Weisner GL, Zyzanski SJ, Goodwin MA, Stange KC. Family history-taking in community family practice: Implications for genetic screening. Genet Med. 2000;2:180–5. doi: 10.1097/00125817-200005000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Acheson L. Fostering applications of genetics in primary care: What will it take? Genet Med. 2003;5:63–5. doi: 10.1097/01.GIM.0000056946.67707.67. [DOI] [PubMed] [Google Scholar]
- 26.Rich EC, Burke W, Heaton CJ, Haga S, Pinsky L, Short P, Acheson L. Reconsidering the family history in primary care. J Gen Intern Med. 2004;19:273–80. doi: 10.1111/j.1525-1497.2004.30401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Green RF, Olney RS. Connecting generations: Family history an important tool in pediatrics, public health. AAP News. 2007;28:26. [Google Scholar]
- 28.Koehly LM, Peters JA, Kenen R, Hoskins LM, Ersig AL, Kuhn NR, Loud JT, Greene MH. Characteristics of health information gatherers, disseminators, and blockers within families at risk of hereditary cancer: Implications for family health communication interventions. Am J Public Health. 2009;99:2203–9. doi: 10.2105/AJPH.2008.154096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ersig AL, Williams JK, Hadley DW, Koehly LM. Communication, encouragement, and cancer screening in families with and without mutations for hereditary nonpolyposis colorectal cancer: A pilot study. Genet Med. 2009;11:728–34. doi: 10.1097/GIM.0b013e3181b3f42d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kaphingst KA, Lachance CR, Condit CM. Beliefs about heritability of cancer and health information seeking and preventive behaviors. J Cancer Educ. 2009;24:351–6. doi: 10.1080/08858190902876304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bertakis K, Helms L, Callahan E, Azari R, Robbins J. The influence of gender on physician practice style. Med Care. 1995;33:407–16. doi: 10.1097/00005650-199504000-00007. [DOI] [PubMed] [Google Scholar]
- 32.Waitzkin J. Information giving in medical care. J Health Soc Behav. 1985;26:81–101. [PubMed] [Google Scholar]
- 33.Roter D, Hall J. Why physician gender matters in shaping the physician-patient relationship. J Womens Health. 1998;7:1093–7. doi: 10.1089/jwh.1998.7.1093. [DOI] [PubMed] [Google Scholar]
- 34.Gordon H, Street RL, Jr, Sharf B, Kelly PA, Souchek J. Racial differences in trust and lung cancer patients’ perceptions of physician communication. J Clin Oncol. 2006;24:904–9. doi: 10.1200/JCO.2005.03.1955. [DOI] [PubMed] [Google Scholar]
- 35.Salkeld G, Solomon M, Short L, Butow P. A matter of trust - patient’s views on decision-making in colorectal cancer. Health Expect. 2004;7:104–11. doi: 10.1111/j.1369-7625.2004.00257.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lerman C, Daly M, Walsh W, et al. Communication between patient with breast cancer andhealth care providers. Determinants and implications. Cancer. 1993;72:2612–20. doi: 10.1002/1097-0142(19931101)72:9<2612::aid-cncr2820720916>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 37.McBride CM, Alford SH, Reid RJ, Larson EB, Baxevanis AD, Brody LC. Characteristics of users of online personalized genomic risk assessments: Implications for physician-patient interactions. Genet Med. 2009;11:582–7. doi: 10.1097/GIM.0b013e3181b22c3a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Topolski TD, LoGerfo J, Patrick DL, Williams B, Walwick J, Patrick MB. The Rapid Assessment of Physical Activity (RAPA) among older adults. Prev Chronic Dis. 2006;3:A118. [PMC free article] [PubMed] [Google Scholar]
- 39.National Cancer Institute. [Accessed 5/25/11];Health Information National Trends Survey. 2007 http://hints.cancer.gov/questions/index.jsp.
- 40.Centers for Disease Control and Prevention. [Accessed 5/25/11];Behavioral Risk Factor Surveillance System: Turning information into health. http://www.cdc.gov/BRFSS/
- 41.Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, Mockbee J, Hale FA. Quick assessment of literacy in primary care: the Newest Vital Sign. Annals Fam Med. 2005;3:514–22. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Osborn CY, Weiss BD, Davis TC, Skripkauskas S, Rodrigue C, Bass PF, III, Wolf MS. Measuring adult literacy in health care: Performance of the Newest Vital Sign. Am J Health Behav. 2007;31:S36–46. doi: 10.5555/ajhb.2007.31.supp.S36. [DOI] [PubMed] [Google Scholar]
- 43.Griffin RJ, Dunwoody S, Neuwirth K. Proposed model of the relationship of risk information seeking and processing to the development of preventive behaviors. Environ Res. 1999;80:S230–45. doi: 10.1006/enrs.1998.3940. [DOI] [PubMed] [Google Scholar]
- 44.Zlot AI, Bland MP, Silvey K, Epstein B, Mielke B, Leman RF. Influence of family history of diabetes on health care provider practice and patient behavior among nondiabetic Oregonians. Prev Chronic Dis. 2009;6(1) 07_0022.htm. [PMC free article] [PubMed] [Google Scholar]
- 45.Hariri S, Yoon PW, Qureshi N, Valdez R, Scheuner MT, Khoury MJ. Family history of type 2 diabetes: A population-based screening tool for prevention? Genet Med. 2006;8(2):102–8. doi: 10.1097/01.gim.0000200949.52795.df. [DOI] [PubMed] [Google Scholar]
- 46.National Comprehensive Cancer Network. [Accessed 2/28/2011];NCCN Guidelines for Detection, Prevention, & Risk Reduction. 2011 http://www.nccn.org/professionals/physician_gls/f_guidelines.asp#detection.
- 47.O’Neill SC, McBride CM, Hensley Alford S, Kaphingst KA. Preferences for genetic and behavioral health information: The impact of risk factors and disease attributions. Ann Behav Med. 2010;40:127–37. doi: 10.1007/s12160-010-9197-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rutten LJF, Squiers L, Hesse B. Cancer-related information seeking: Hints from the 2003 Health Information National Trends Survey (HINTS) J Health Commun. 2006;11:147–156. doi: 10.1080/10810730600637574. [DOI] [PubMed] [Google Scholar]
- 49.Shim M, Kelly B, Hornik R. Cancer information scanning and seeking behavior is associated with knowledge, lifestyle choices, and screening. J Health Commun. 2006;11:157–72. doi: 10.1080/10810730600637475. [DOI] [PubMed] [Google Scholar]
- 50.Weaver JB, III, Mays D, Sargent Weaver S, Hopkins GL, Eroglu D, Bernhardt JM. Health information-seeking behaviors, health indicators, and health risks. Am J Public Health. 2010;100:1520–5. doi: 10.2105/AJPH.2009.180521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Institute of Medicine. Unequal Treatment: Understanding Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002. [Google Scholar]
- 52.Gee GC. A multilevel analysis of the relationship between institutional and individual racial discrimination and health status. Am J Public Health. 2002;92:615–23. doi: 10.2105/ajph.92.4.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Taylor SL, Lurie N. The role of culturally competent communication in reducing ethnic and racial healthcare disparities. Am J Manag Care. 2004;10:SP1–4. [PubMed] [Google Scholar]
- 54.Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O., 2nd Defining cultural competence: A practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 2003;118:293–302. doi: 10.1016/S0033-3549(04)50253-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ashida S, Koehly LM, Roberts JS, Chen CA, Hiraki S, Green RC. Disclosing the disclosure: Factors associated with communicating the results of genetic susceptibility testing for Alzheimer’s Disease. J Health Commun. 2009;14:768–84. doi: 10.1080/10810730903295518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Street RL., Jr Gender differences in health care provider-patient communication: Are they due to style, stereotypes, or accommodation? Patient Educ Couns. 2002;48:201–206. doi: 10.1016/s0738-3991(02)00171-4. [DOI] [PubMed] [Google Scholar]
- 57.Lea DH, Kaphingst KA, Bowen D, Lipkus I, Hadley DW. Communicating genetic information and genetic risk: An emerging role for health educators. Public Health Genomics. 2010 doi: 10.1159/000294191. ePub before press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hunt K, Emslie C, Watt G. Lay constructions of a family history of heart disease: potential for misunderstandings in the clinical encounter? Lancet. 2001;357:1168–1171. doi: 10.1016/S0140-6736(00)04334-8. [DOI] [PubMed] [Google Scholar]
- 59.Walter FM, Emery J. ‘Coming down the line’ - Patients’ understanding of their family history of common chronic disease. Ann Fam Med. 2005;3:405–8. doi: 10.1370/afm.368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Walter FM, Emery J, Braithwaite D, Marteau TM. Lay understanding of familial risk of common chronic diseases: A systematic review and synthesis of qualitative research. Ann Fam Med. 2004;2:583–94. doi: 10.1370/afm.242. [DOI] [PMC free article] [PubMed] [Google Scholar]


