Abstract
Background
We investigated recent loss of or separation from afamily member or friend and risk of sudden cardiac arrest.
Methods
Our case-crossover study included 490 apparently-healthy married residents of King County, Washington, who suffered sudden cardiac arrest between 1988 and 2005. We compared exposure to spouse-reported family/friend events occurring ≤ 1 month before sudden cardiac arrest with events occurring n the previous 5 months. We evaluated potential effect modification by habitual vigorous physical activity.
Results
Recent family/friend events were associated with a higher risk of sudden cardiac arrest (odds ratio (OR) = 1.6 [95% confidence interval (CI) = 1.1-2.4]). ORs for cases with and without habitual vigorous physical activity were 1.1 (0.6-2.2) and 2.0 (1.2-3.1), respectively, (interaction P = 0.02).
Conclusions
These results suggest family/friend events may trigger sudden cardiac arrest and raise the hypothesis that habitual vigorous physical activity may lower susceptibility to these potential triggers.
Episodes of anger, depressed mood, and stress may trigger cardiovascular events, including myocardial infarction and stroke.1-10 Whether these psychological states can trigger sudden cardiac arrest is unknown.
We sought to examine the relationship between recent family/friend events (e.g. loss of or separation from a relative or friend), as markers of recent psychological stress, and risk of sudden cardiac arrest. Our primary aim was to test the hypothesis that apparently healthy individuals who experience recent family/friend events are at higher risk of sudden cardiac arrest. Our secondary aim was to evaluate potential effect modification by habitual vigorous physical activity, because prior studies suggest that vigorous physical activity may reduce vulnerability to triggers of acute coronary events.11-16
Methods
We used data from a population-based case-control study of out-of-hospital sudden cardiac arrest in Seattle and suburban King County, Washington (for details, see eAppendix, http://links.lww.com).17-21 Briefly, we defined sudden cardiac arrest as a sudden pulseless condition in the absence of evidence of non-cardiac causes. Cases included married men and women who suffered sudden cardiac arrest between 1988 and 2005. Eligible cases were 29- to 74-year-old residents of King County, Washington, without history of clinically recognized heart disease or life-threatening comorbidity. Emergency Medical Service reports were used to identify cases. When available, information from death certificates and from medical examiner and autopsy reports was used to confirm absence of life-threatening non-cardiac causes of death. We excluded 24 cases without in-person spouse interviews, 19 with unknown exposure to family/friend events, and 19 cases who, according to their spouses, had been in poor health during the previous year. The response among eligible case spouses was 85%, providing 490 cases for analysis.
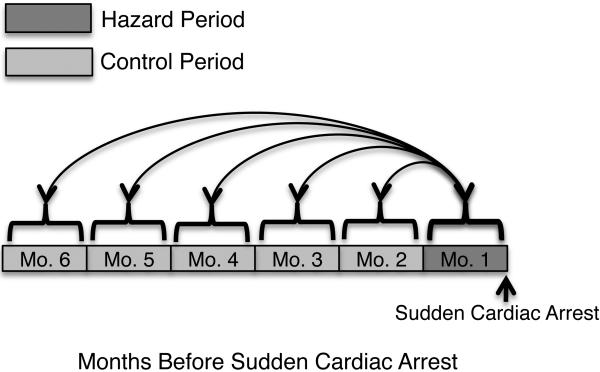
Because we hypothesized that risk associated with family/friend events might vary over time, we used a case-crossover design.22 We compared exposure to any family/friend event occurring ≤ 1 month before sudden cardiac arrest (hazard period) to five month-long subject-matched control periods extending from > 1 to ≤ 6 months before sudden cardiac arrest (Figure).
Figure.
Description of Case-Crossover Design
Case spouses were interviewed regarding major life events occurring during the year before the sudden cardiac arrest. We defined major life events involving family or friends as follows: death of a close family member, separation from a close family member, death of a close friend, separation from a close friend, move out of a household member, move in of a household member, and relocation of residence. Spouses were asked to estimate the time between these events and the sudden cardiac arrest.
The reliability of spouse responses to family/friend event questions was evaluated in interviews from 85 sudden-cardiac-arrest survivors and their spouses. Kappa statistics indicated moderate agreement between surviving cases and their spouses on the occurrence (unweighted kappa: 0.49) and timing (unweighted kappa: 0.48) of family/friend events. These calculations are described in the eAppendix, http://links.lww.com.
We considered potential confounding from seasonal variation in the timing of sudden cardiac arrest and family/friend events. To adjust for seasonal variation, we fit the sine and cosine of the day of the year on which the arrest occurred, scaled to one cycle per year.23 Because cases serve as their own controls, it was not necessary to adjust for non-time-varying-characteristics. We evaluated possible effect modification by habitual vigorous activity, defined as at least 20 minutes per week of high-intensity leisure-time activity, a level associated with a lower risk of sudden cardiac arrest in our prior reports.11,24,25 Activities were considered as high-intensity if the energy expended was approximately 6 kcal or more per minute (e.g. jogging, swimming).
We estimated the relative risk of sudden cardiac arrest after a friend/family event, using conditional logistic regression to calculate odds ratios (ORs) and robust 95% confidence intervals (95% CIs). We explored variously defined control periods in a sensitivity analysis. The data were analyzed using STATA software (version 10.1; StataCorp LP, College Station, TX).
Results
Cases were on average 59 years old, 81% were men, and 93% were white. Mean length of marriage was 29 years. At least one family/friend event was experienced by 28% of cases in the 6 months before sudden cardiac arrest.
Compared with the control period, any family/friend event in the past month was associated with a higher risk of sudden cardiac arrest (OR = 1.6 [95% CI = 1 to 2.4]) (Table 1). Results were similar when the control period was defined as >1 to ≤ 3 months or > 3 to ≤ 6 months before sudden cardiac arrest (Table 1). Further exploration of various definitions of “recent” and “non-recent” time periods produced similar risk estimates (eTable1; eAppendix, http://links.lww.com). Adjustment for seasonal variation of sudden cardiac arrest affected the estimated relative risk only slightly (Table 2).
TABLE 1.
Association of “Recent” Relative to “No Recent” Family/Friend Events and Sudden Cardiac Arrest
| Control Months a | OR (95% CI) b |
|---|---|
| >1-6 | 1.6 (1.1 -2.4) |
| Sensitivity Analysis | |
| >1-3 | 1.5 (1.0-2.3) |
| >3-6 | 1.7(1.1 -2.5) |
Hazard Period: 0-1 month before sudden cardiac arrest.
ORs are adjusted for season.
TABLE 2.
Case-Crossover Analysis of Exposure to “Recent” Relative to “No Recent” Family/Friend Events Before Sudden Cardiac Arrest by Control Month
| Period |
OR (95% CI) |
||||
|---|---|---|---|---|---|
| Control Month | Hazard Only a No. Events | Control Only No. Events | Both No. Events | Unadjusted | Adjusted b |
| >1-2 | 35 | 29 | 5 | 1.2 (0.7 - 2.0) | 1.2 (0.7 - 2.0) |
| >2-3 | 38 | 19 | 2 | 2.0 (1.2 - 3.5) | 2.0 (1.1 - 3.4) |
| >3-4 | 38 | 19 | 2 | 2.0 (1.2 - 3.5) | 2.1 (1.2 - 3.5) |
| >4-5 | 35 | 19 | 5 | 1.8 (1.1 - 3.2) | 1.9 (1.1 - 3.3) |
| >5-6 | 36 | 27 | 4 | 1.3 (0.8 - 2.2) | 1.3 (0.8 - 2.2) |
Hazard Period: 0-1 month before sudden cardiac arrest.
Odds ratios are adjusted for season.
Risk associated with recent family/friend events was higher among people who did not engage in habitual vigorous physical activity (OR = 2.0 [95% CI = 1.2 to 3.1]) than among more active people (1.1 [95% CI, 0.6 to 2.2]) (Table 3), (interaction P-value = 0.2).
TABLE 3.
Association of “Recent” Relative to “No Recent” Family/Friend Events and Sudden Cardiac Arrest by Presence of Habitual Vigorous Physical Activity a
| Habitual Vigorous Physical Activity | No. Cases | OR (95% CI) b |
|---|---|---|
| Yes | 145 | 1.1 (0.6-2.2) |
| No | 345 | 2.0(1.2-3.1) |
| Relative OR c | 0.6 (0.3 - 1.3) |
Defined as ≥ 20 minutes/week of high-intensity leisure-time activity.
ORs are adjusted for season.
Relative OR= ORYes/ORNo, likelihood ratio test for interaction P = 0.2.
Discussion
Our findings suggest that recent loss or separation from family or friends may trigger sudden cardiac arrest, and that habitual vigorous physical activity may lower vulnerability to this trigger. The use of a case-crossover design enabled control of unmeasured non-time-varying person-specific confounding factors, and improved efficiency to estimate associations by use of multiple subject-matched control periods.26 Spouses reported family/friend events occurring during the year before the sudden cardiac arrest. We focused on the most recent 6 months (1 hazard month and 5 control months). Including additional control months (1 hazard month and 11 control months) did not materially affect our study's conclusions (eTable 1, http://links.lww.com).
Our findings should be interpreted in view of several potential limitations. The true hazard period for stressful events may be shorter than one month. Imprecise estimation of the hazard period tends to bias estimates of risk towards the null.27 Data were available to evaluate shorter hazard periods for a subset of cases (eTable 1; http://links.lww.com) results from these analyses were similar to our primary results.
Reliance on spouse response may have introduced nondifferential misclassification. We focused on family/friend events rather than interpersonal conflicts or emotional states because we regarded such events as more likely to be recognized and accurately reported by spouses. Kappa statistics indicated moderate agreement between the subset of surviving cases and their spouses on the occurrence and timing of family/friend events.
Differential misclassification may exist if, for example, control periods of time more distant from the sudden cardiac arrest are more vulnerable to underreporting.28 We sought to address this potential limitation in several ways. First, using the case-crossover design, we estimated the relative risk with non-overlapping distant and recent control periods. Second, we explored the effect of restricting our case-crossover analysis to the events we considered most memorable: death of or separation from family members or friends (eTable 2, http://links.lww.com). Third, we conducted an analysis using a case-control design (eTables 3-4, http://links.lww.com). All these alternative analyses resulted in similar relative risk estimates, and support our study conclusions.
While the case-crossover study has the advantage of controlling confounding for fixed factors, our study may have inadequately identified and accounted for confounding by transient factors. We did control for seasonal variation in sudden cardiac arrest, which made little difference. Other possible triggers of cardiac arrest that potentially confounded the association include recent physical exertion, sexual activity, overeating, coffee consumption, lack of sleep, and recent exposure to air pollution.29,30
Generalizability of our findings may be limited, as all participants were married. We previously reported that being married is associated with a lower risk of sudden cardiac arrest.31 To the extent that being married contributes positively to social support, and social support mitigates the effects of stressors, we may have underestimated the risk associated with recent family/friend events.
Sudden cardiac arrest and myocardial infarction have many risk factors in common, and recent family/friend events have been associated with higher risk of myocardial infarction.32 Mittleman et al32 reported that “death of a significant person, friend or relative” increased acute risk for myocardial infarction 14-fold (95% CI = 7.2 to 28.2), where the hazard period was one day. When the hazard period was defined as 8 to 28 days, the estimated relative risk was 4.8 (95% CI = 3.5 to 6.6).
Based on animal experimental studies, excessive activation of the sympathetic nervous system can lead to increased heart rate, reduced vagal tone and heart rate variability, ischemia, and arrhythmia,33,34 all of which can contribute to increased risk for sudden cardiac arrest. Also, acute stress may trigger plaque rupture, leading to subsequent coronary thrombosis.35
Additional studies are warranted to confirm our findings, and to clarify mechanisms by which family/friend events may trigger sudden cardiac arrest. Further work is also needed to identify factors that reduce vulnerability to triggers of acute cardiovascular events. For example, aspirin and beta-blockers may lower susceptibility to triggers of myocardial infarction.3,6,36,37 Whether medications or lifestyle factors lower susceptibility to family/friend events as potential triggers of sudden cardiac arrest is unknown.
Acknowledgements
We appreciate the assistance of the paramedics of the Seattle Medic One Program and Seattle-King County Health Department Emergency Medical Services Division with the project.
Sources of Funding: The research reported in this article was supported by grants from the National Heart, Lung, and Blood Institute, Training Grant (I-T32-HL07902), the National Heart, Lung, and Blood Institute (HL091244, HL088456, HLA41993) and the University of Washington Clinical Nutrition Research Unit (DK-35816). Initial support was provided by the Medic One Foundation, Seattle, WA.
eAPPENDIX Major Life Events as Potential Triggers of Sudden Cardiac Arrest
METHODS
Study sample
We used data from the Cardiac Arrest Blood Study (CABS), a population-based case-control study of paramedic-attended out-of-hospital sudden cardiac arrest in Seattle and suburban King County, Washington. We defined sudden cardiac arrest as the occurrence of a sudden pulseless condition and the absence of evidence of a non-cardiac condition as the cause of the cardiac arrest. The determination of “sudden” was based on the circumstances surrounding the event indicated in the Emergency Medical Service incident reports. We did not use time between symptom onset and collapse because 1/3 of sudden cardiac arrests are not witnessed. We excluded study subjects with any evidence of a non-cardiac cause defined as any prior life-threatening comorbidities such as cancer, end-stage lung, liver, or renal disease. Nursing home patients were also excluded to avoid misclassification as to the cause of death. The primary aim of CABS was to investigate dietary determinants of cardiac arrest. To avoid the possibility that diet might have changed prior to the cardiac arrest, we also excluded subjects with a history of clinically recognized heart disease defined as history of angina, prior myocardial infarction, coronary artery bypass surgery, angioplasty, congestive heart failure, arrhythmias, cardiomyopathy, valvular, or congenital disease. We also excluded patients with any condition that would have altered usual diet.
Poor health was assessed during the spouse interview. Spouses were asked to answer the following, “during the past 12 months, would you say, in general that your spouse's health was: excellent, very good, good, fair, poor, refused, or don't know.” Our study excluded 19 cases whose health was poor according to their spouse.
All patients were subjected to the same clinical definition of sudden cardiac arrest. The main clinical investigation was the same for all subjects and consisted of a review of the Emergency Medical Service incident report forms and structured spouse interviews. We supplemented this investigation with information from death certificates for fatal cases. When available, medical examiner, and/or autopsy reports were used to confirm absence of life-threatening non-cardiac causes of death.
Selection of married subjects
Our study included cases of sudden cardiac arrest only if they were married and living together for at least one year. Since a high percentage of cases die, 88% in our study, we relied on spouse interviews to obtain information on lifestyle and dietary habits during the year before the sudden cardiac arrest. We also relied on spouse interviews for the controls to standardize the quality of the data for cases and controls. We did not include other sources of information such as partners or siblings, because we were concerned that we would not get the same quality of data from these other sources.
Reliability of spouse-reported occurrence and timing of family/friend events
The unweighted kappa statistic for sudden cardiac arrest survivors and spouses regarding the occurrence of any family/friend event ≤ 6 months before sudden cardiac arrest, dichotomized as exposed or unexposed, was 0.49. We further evaluated the reliability of spouse reported timing of most recent family/friend event by assigning exposure into one of three mutually exclusive categories including most recent event ≤ 1 month, > 1 to ≤ 6 months, and no exposure 6 months before sudden cardiac arrest. The unweighted kappa statistic for the three categories of most recent family/friend event among survivors and spouses was 0.48.
Selection of control subjects for the case-control analysis
Control subjects were identified concurrently from the community using random-digit dialing. Control subjects were individually matched to cases at an approximate ratio of 2 to 1, by age (within 7 years), sex, and calendar year. Control subjects were selected using the same eligibility and exclusion criteria as the cases. We excluded 41 controls without in-person spouse interviews, 25 with unknown exposure to family/friend events, and 5 controls who, according to their spouses, were in poor health during the previous year. The response rate among eligible control spouses was 60%, leading to 870 controls for study inclusion.
Case-control analysis
For the case-control analysis, to estimate the relative risk of recent family/friend events, we used conditional logistic regression to calculate odds ratios (ORs) and robust 95% confidence intervals (95% CI). Subjects were considered exposed if they had experienced a family/friend event during the month before the sudden cardiac arrest/reference date and were considered unexposed if they did not indicate that they experienced a family/friend event during the month before the sudden cardiac arrest/reference date. Our fully adjusted model included variables for age (within 7 years), calendar year, sex, formal education beyond high school (yes/no), current and former cigarette smoking, physician-diagnosed diabetes mellitus and hypertension (ever/never), weight (kg), index of fat intake, total DHA and EPA consumed (g), and habitual vigorous physical activity.
RESULTS
Effect of including cases with poor health
We completed a sensitivity analysis that included subjects with poor health, since the interview question regarding poor health may be susceptible to recall bias and our primary analysis excluded cases with poor health according to the spouse interview. Our results for the case-crossover analysis that included cases reported to have been in poor health (n=509) were similar to our primary results. The adjusted OR was 1.6, 95% CI: 1.1-2.3.
Effect of including additional control months
Spouses reported family/friend events that occurred during the year before the sudden cardiac arrest. However, our primary results were based on the most recent 6 months (1 hazard and 5 control months) because we thought more distal time periods might have been more difficult to recall. Nevertheless we extended the analysis to 12 months (1 hazard and 11 control months) before sudden cardiac arrest. The estimated risk (OR) from this analysis was slightly larger than our primary results, which might be accounted for in part, by recall bias (eTable 1, top row). However, the difference in the estimated risk did not materially affect our study's conclusions.
Effect of shorter hazard periods
Subjects were asked to estimate the timing of the life events before the sudden cardiac arrest in two ways depending on the questionnaire version (see old versus new questionnaires, eAppendix). The older version asked subjects (n = 158/490) to report the month and year of the family/friend event. The newer version asked subjects (n = 332/490) to report the number of weeks before the sudden cardiac arrest that the family/friend event occurred. We examined shorter hazard periods of 1 week and 2 weeks before the sudden cardiac arrest for the subset who reported weeks (n = 332/490). Results from these analyses (bottom two rows of eTable 1) were consistent with our primary results.
Effect of restricting family/friend events to death/separation of a family member/friend
To explore the potential presence of recall bias in our analysis we restricted to family/friend events that we considered as more memorable. Family/friend events we considered to be less susceptible to recall bias included death of a family member/friend and separation from a family member/friend compared to the other questions including move in/out of a household member and relocation. The results of this sensitivity analysis are presented in eTable 2 and are consistent with our primary results.
Study population characteristics
Characteristics of cases and controls are described in eTable 3. Subjects in this study included 490 cases and 870 controls. Briefly, compared to controls, cases were more likely to be current smokers, have physician-diagnosed diabetes mellitus and hypertension, have family history of myocardial infarction or sudden death, fair or good health, and more alcohol and caffeine consumption. Fewer cases engaged in habitual physical activity compared to controls.
Case-control analysis results
Results of the case-control analysis are described in eTable 4. Similar to the results from the case-crossover analysis, higher risk was associated with any family/friend event in the past month (OR = 1.4, 95% CI, 0.8 to 2.5). There was strong evidence that the elevated risk associated with any family/friend event was primarily among people who did not engage in habitual vigorous physical activity (OR = 2.4, 95% CI, 1.3 to 4.4) and was less evident among more active people (OR = 0.7, 95% CI, 0.3 to 1.7), the interaction p-value was 0.03.
Appendix
eTABLE 1.
Association of “Recent” Relative to “No Recent” Family/Friend Events and Sudden Cardiac Arrest: Use of Additional Control Periods and Shorter Hazard Periods
| Hazard Period | Control Periods | OR (95% CI) a |
|---|---|---|
| 1 month | >1-2, >2-3, ..., >11-12 months (11 month long periods) | 2.1 (1.5, 3.0) |
| 1 week | 2, 3, ..., 24 weeks (23 week long periods) | 2.1 (1.1, 3.9)b |
| ≥1-2 weeks | ≥3-4, ≥5-6, ..., ≥23-24 weeks (11 two-week long periods) | 1.5 (0.9, 2.6)b |
ORs are adjusted for season.
Results are restricted to the subset of subjects who reported the number of weeks before the sudden cardiac arrest for the family/friend events (n = 332/490).
Appendix
eTABLE 2.
Association of “Recent” Relative to “No Recent” Death/Separation of a Family Member/Friend and Sudden Cardiac Arrest
| Control Months a | OR (95% CI) b |
|---|---|
| >1-2, >2-3, >3-4, >4-5, >5-6 | 1.8 (1.1, 2.8) |
| Sensitivity Analysis | |
| >1-2, >2-3 | 1.7(1.0, 3.0) |
| >3-4, >4-5, >5-6 | 1.7(1.1, 2.8) |
Hazard Period: 0-1 month before sudden cardiac arrest.
ORs are adjusted for season.
Appendix
eTABLE 3.
Study Population Characteristics
| Characteristic | Cases a N = 490 | Controls b N = 870 |
|---|---|---|
| Age (years, mean(SD)) | 58.6 (10.2) | 57.1 (10.6) |
| Men (%) | 80.6 | 78.7 |
| White (%) | 93.0 | 93.5 |
| Years married (mean(SD)) | 29.4 (14.0) | 27.3 (14.4) |
| Formal education beyond high-school (%) | 67.1 | 79.5 |
| Currently employed (%) | 59.8 | 66.3 |
| Current smoker (%) | 31.3 | 9.5 |
| Former smoker (%) | 37.0 | 42.5 |
| Diabetes mellitus (%) | 12.1 | 4.5 |
| Hypertension (%) | 35.7 | 22.1 |
| Hypercholesterolemia (%) | 24.3 | 21.3 |
| Weight (kg, mean(SD)) | 83.3 (17.2) | 81.4 (16.1) |
| Height (cm, mean(SD)) | 176.4 (9.3) | 176.2 (9.2) |
| Family history of myocardial infarction or sudden death (%) | 54.9 | 40.3 |
| Early family history of same (%) | 25.4 | 13.7 |
| Self-perceived health (%) | ||
| Excellent | 25.0 | 36.0 |
| Very good | 29.5 | 39.4 |
| Good | 28.9 | 20.1 |
| Fair | 16.7 | 4.5 |
| Dietary eicosapentaenoic acid and | ||
| docosahexaenoic acid (g/mo, mean (25th, 75th percentiles)) | 4.5 (0.9, 6.1) | 5.8 (1.6, 7.7) |
| Fat Intake Scale score | 21.8 (3.8) | 21.2 (3.9) |
| One or more alcoholic beverages/day | 28.0 | 26.8 |
| Aspirin user (%) | 46.5 | 44.3 |
| Caffeine (mg/d, mean (25th, 75th percentiles)) | 437.0 (104.2, 562.0) | 306.0 (45.5, 426.6) |
| Habitual vigorous physical activity (%) | 29.6 | 42.6 |
Missing values for white race (n = 4), years married (n = 2), current smoker (n = 1), former smoker (n = 1), diabetes mellitus (n = 2), hypertension (n = 6), hypercholesterolemia (n = 13), weight (n = 9), family history of myocardial infarction or sudden death (n = 9), early family history of myocardial infarction or sudden death (n = 9), self-perceived health (n = 5), dietary eicosapentaenoic acid and docosahexaenoic acid (n = 10), Fat Intake Scale score (n = 15), aspirin use (n = 56).
Missing values for white race (n = 7), years married (n = 2), current smoker (n = 8), former smoker (n = 8), diabetes mellitus (n = 2), hypertension (n = 11), hypercholesterolemia (n = 9), weight (n = 66), height (n = 4), family history of myocardial infarction or sudden death (n = 6), early family history of myocardial infarction or sudden death (n = 6), self-perceived health (n = 1), dietary eicosapentaenoic acid and docosahexaenoic acid (n = 23), Fat Intake Scale score (n = 33), alcohol (n = 1), aspirin use (n = 71), caffeine (n = 1).
Appendix
eTABLE 4.
Association of “Recent” Relative to “No Recent” Family/Friend Events and Sudden Cardiac Arrest by Habitual Vigorous Physical Activity Using the Case-Control Design
| OR (95% CI) |
||||
|---|---|---|---|---|
| Exposed a Cases/Controls | Unexposed Cases/Controls | Model 1 b | Model 2 c | |
| All Subjects a | 40/75 | 450/795 | 1.1(0.7, 1.6) | 1.4(0.8, 2.5) |
| Habitual Vigorous Physical Activityd | ||||
| Yes | 11/35 | 134/336 | 0.7(0.3, 1.7) | |
| No | 29/40 | 316/459 | 2.3(1.2, 4.4) | |
Exposure to family/friend events during 0-1 month before sudden cardiac arrest or control reference date.
Model 1 is adjusted for matching variables only including, age (within 7 years), calendar year, and sex.
Model 2 is additionally adjusted for formal education beyond high school (yes/no), current and former cigarette smoking, physician-diagnosed diabetes mellitus and hypertension (ever/never), weight (kg), index of fat intake, total DHA and EPA consumed (g), and habitual vigorous physical activity.
Likelihood ratio test for interaction p-value: 0.03
Footnotes
Conflicts of Interest
We have no conflicts of interest to report.
SDC Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article (www.epidem.com). This content is not peer-reviewed or copy-edited; it is the sole responsibility of the author.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Steptoe A, Strike PC, Perkins-Porras L, McEwan JR, Whitehead DL. Acute depressed mood as a trigger of acute coronary syndromes. Biol Psychiatry. 2006;60(8):837–42. doi: 10.1016/j.biopsych.2006.03.041. [DOI] [PubMed] [Google Scholar]
- 2.Tofler GH, Stone PH, Maclure M, Edelman E, Davis VG, Robertson T, Antman EM, Muller JE. Analysis of possible triggers of acute myocardial infarction (the MILIS study). The American journal of cardiology. 1990;66(1):22–7. doi: 10.1016/0002-9149(90)90729-k. [DOI] [PubMed] [Google Scholar]
- 3.Moller J, Hallqvist J, Diderichsen F, Theorell T, Reuterwall C, Ahlbom A. Do episodes of anger trigger myocardial infarction? A case-crossover analysis in the Stockholm Heart Epidemiology Program (SHEEP). Psychosom Med. 1999;61(6):842–9. doi: 10.1097/00006842-199911000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Nawrot TS, Perez L, Kunzli N, Munters E, Nemery B. Public health importance of triggers of myocardial infarction: a comparative risk assessment. Lancet. 2011;377(9767):732–40. doi: 10.1016/S0140-6736(10)62296-9. [DOI] [PubMed] [Google Scholar]
- 5.Strike PC, Perkins-Porras L, Whitehead DL, McEwan J, Steptoe A. Triggering of acute coronary syndromes by physical exertion and anger: clinical and sociodemographic characteristics. Heart. 2006;92(8):1035–40. doi: 10.1136/hrt.2005.077362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mittleman MA, Maclure M, Sherwood JB, Mulry RP, Tofler GH, Jacobs SC, Friedman R, Benson H, Muller JE. Triggering of acute myocardial infarction onset by episodes of anger. Determinants of Myocardial Infarction Onset Study Investigators. Circulation. 1995;92(7):1720–5. doi: 10.1161/01.cir.92.7.1720. [DOI] [PubMed] [Google Scholar]
- 7.Koton S, Tanne D, Bornstein NM, Green MS. Triggering risk factors for ischemic stroke: a case-crossover study. Neurology. 2004;63(11):2006–10. doi: 10.1212/01.wnl.0000145842.25520.a2. [DOI] [PubMed] [Google Scholar]
- 8.Lipovetzky N, Hod H, Roth A, Kishon Y, Sclarovsky S, Green MS. Emotional events and anger at the workplace as triggers for a first event of the acute coronary syndrome: a case-crossover study. The Israel Medical Association journal : IMAJ. 2007;9(4):310–5. [PubMed] [Google Scholar]
- 9.Moller J, Theorell T, de Faire U, Ahlbom A, Hallqvist J. Work related stressful life events and the risk of myocardial infarction. Case-control and case-crossover analyses within the Stockholm heart epidemiology programme (SHEEP). Journal of epidemiology and community health. 2005;59(1):23–30. doi: 10.1136/jech.2003.019349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guiraud V, Amor MB, Mas JL, Touze E. Triggers of ischemic stroke: a systematic review. Stroke; a journal of cerebral circulation. 2010;41(11):2669–77. doi: 10.1161/STROKEAHA.110.597443. [DOI] [PubMed] [Google Scholar]
- 11.Siscovick DS, Weiss NS, Fletcher RH, Lasky T. The incidence of primary cardiac arrest during vigorous exercise. N Engl J Med. 1984;311(14):874–7. doi: 10.1056/NEJM198410043111402. [DOI] [PubMed] [Google Scholar]
- 12.Albert CM, Mittleman MA, Chae CU, Lee IM, Hennekens CH, Manson JE. Triggering of sudden death from cardiac causes by vigorous exertion. N Engl J Med. 2000;343(19):1355–61. doi: 10.1056/NEJM200011093431902. [DOI] [PubMed] [Google Scholar]
- 13.Mittleman MA, Maclure M, Tofler GH, Sherwood JB, Goldberg RJ, Muller JE. Triggering of acute myocardial infarction by heavy physical exertion. Protection against triggering by regular exertion. Determinants of Myocardial Infarction Onset Study Investigators. N Engl J Med. 1993;329(23):1677–83. doi: 10.1056/NEJM199312023292301. [DOI] [PubMed] [Google Scholar]
- 14.Muller JE, Mittleman MA, Maclure M, Sherwood JB, Tofler GH. Triggering myocardial infarction by sexual activity. Low absolute risk and prevention by regular physical exertion. Determinants of Myocardial Infarction Onset Study Investigators. JAMA. 1996;275(18):1405–9. doi: 10.1001/jama.275.18.1405. [DOI] [PubMed] [Google Scholar]
- 15.Willich SN, Lewis M, Lowel H, Arntz HR, Schubert F, Schroder R. Physical exertion as a trigger of acute myocardial infarction. Triggers and Mechanisms of Myocardial Infarction Study Group. The New England journal of medicine. 1993;329(23):1684–90. doi: 10.1056/NEJM199312023292302. [DOI] [PubMed] [Google Scholar]
- 16.Dahabreh IJ, Paulus JK. Association of episodic physical and sexual activity with triggering of acute cardiac events: systematic review and meta-analysis. JAMA : the journal of the American Medical Association. 2011;305(12):1225–33. doi: 10.1001/jama.2011.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Siscovick DS, Raghunathan TE, King I, Weinmann S, Wicklund KG, Albright J, Bovbjerg V, Arbogast P, Smith H, Kushi LH, et al. Dietary intake and cell membrane levels of long-chain n-3 polyunsaturated fatty acids and the risk of primary cardiac arrest. JAMA : the journal of the American Medical Association. 1995;274(17):1363–7. doi: 10.1001/jama.1995.03530170043030. [DOI] [PubMed] [Google Scholar]
- 18.Sotoodehnia N, Siscovick DS, Vatta M, Psaty BM, Tracy RP, Towbin JA, Lemaitre RN, Rea TD, Durda JP, Chang JM, Lumley TS, Kuller LH, Burke GL, Heckbert SR. Beta2-adrenergic receptor genetic variants and risk of sudden cardiac death. Circulation. 2006;113(15):1842–8. doi: 10.1161/CIRCULATIONAHA.105.582833. [DOI] [PubMed] [Google Scholar]
- 19.Lemaitre RN, King IB, Mozaffarian D, Sotoodehnia N, Rea TD, Kuller LH, Tracy RP, Siscovick DS. Plasma phospholipid trans fatty acids, fatal ischemic heart disease, and sudden cardiac death in older adults: the cardiovascular health study. Circulation. 2006;114(3):209–15. doi: 10.1161/CIRCULATIONAHA.106.620336. [DOI] [PubMed] [Google Scholar]
- 20.Lemaitre RN, King IB, Raghunathan TE, Pearce RM, Weinmann S, Knopp RH, Copass MK, Cobb LA, Siscovick DS. Cell membrane trans-fatty acids and the risk of primary cardiac arrest. Circulation. 2002;105(6):697–701. doi: 10.1161/hc0602.103583. [DOI] [PubMed] [Google Scholar]
- 21.Friedlander Y, Siscovick DS, Weinmann S, Austin MA, Psaty BM, Lemaitre RN, Arbogast P, Raghunathan TE, Cobb LA. Family history as a risk factor for primary cardiac arrest. Circulation. 1998;97(2):155–60. doi: 10.1161/01.cir.97.2.155. [DOI] [PubMed] [Google Scholar]
- 22.Maclure M, Mittleman MA. Should we use a case-crossover design? Annu Rev Public Health. 2000;21:193–221. doi: 10.1146/annurev.publhealth.21.1.193. [DOI] [PubMed] [Google Scholar]
- 23.Stolwijk AM, Straatman H, Zielhuis GA. Studying seasonality by using sine and cosine functions in regression analysis. J Epidemiol Community Health. 1999;53(4):235–8. doi: 10.1136/jech.53.4.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Siscovick DS, Weiss NS, Fletcher RH, Schoenbach VJ, Wagner EH. Habitual vigorous exercise and primary cardiac arrest: effect of other risk factors on the relationship. J Chronic Dis. 1984;37(8):625–31. doi: 10.1016/0021-9681(84)90112-7. [DOI] [PubMed] [Google Scholar]
- 25.Lemaitre RN, Siscovick DS, Raghunathan TE, Weinmann S, Arbogast P, Lin DY. Leisure-time physical activity and the risk of primary cardiac arrest. Arch Intern Med. 1999;159(7):686–90. doi: 10.1001/archinte.159.7.686. [DOI] [PubMed] [Google Scholar]
- 26.Mittleman MA, Maclure M, Robins JM. Control sampling strategies for case-crossover studies: an assessment of relative efficiency. Am J Epidemiol. 1995;142(1):91–8. doi: 10.1093/oxfordjournals.aje.a117550. [DOI] [PubMed] [Google Scholar]
- 27.Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991;133(2):144–53. doi: 10.1093/oxfordjournals.aje.a115853. [DOI] [PubMed] [Google Scholar]
- 28.Moller J, Hessen-Soderman AC, Hallqvist J. Differential misclassification of exposure in case-crossover studies. Epidemiology. 2004;15(5):589–96. doi: 10.1097/01.ede.0000135177.10332.42. [DOI] [PubMed] [Google Scholar]
- 29.Siscovick DS. Triggers of clinical coronary heart disease. Epidemiology. 2006;17(5):495–7. doi: 10.1097/01.ede.0000231372.34197.2a. [DOI] [PubMed] [Google Scholar]
- 30.Tofler GH, Muller JE. Triggering of acute cardiovascular disease and potential preventive strategies. Circulation. 2006;114(17):1863–72. doi: 10.1161/CIRCULATIONAHA.105.596189. [DOI] [PubMed] [Google Scholar]
- 31.Empana JP, Jouven X, Lemaitre R, Sotoodehnia N, Rea T, Raghunathan T, Simon G, Siscovick D. Marital status and risk of out-of-hospital sudden cardiac arrest in the population. Eur J Cardiovasc Prev Rehabil. 2008;15(5):577–82. doi: 10.1097/HJR.0b013e3283083e04. [DOI] [PubMed] [Google Scholar]
- 32.Mittleman MA, Maclure M, Sherwood JB, Kondo NI. G.H. T. Death of a significant person increases the risk of acute MI onset. Circulation. 1996;93(631) [Google Scholar]
- 33.Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99(16):2192–217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 34.Tofler G. Psychosocial factors in sudden cardiac arrest. In: Basow DS, editor. UpToDate. UpToDate; Waltham, MA: 2011. [Google Scholar]
- 35.Muller JE, Abela GS, Nesto RW, Tofler GH. Triggers, acute risk factors and vulnerable plaques: the lexicon of a new frontier. J Am Coll Cardiol. 1994;23(3):809–13. doi: 10.1016/0735-1097(94)90772-2. [DOI] [PubMed] [Google Scholar]
- 36.Culic V, Eterovic D, Miric D, Rumboldt Z, Hozo I. Gender differences in triggering of acute myocardial infarction. The American journal of cardiology. 2000;85(6):753–6, A8. doi: 10.1016/s0002-9149(99)00854-1. [DOI] [PubMed] [Google Scholar]
- 37.Tofler GH, Muller JE, Stone PH, Forman S, Solomon RE, Knatterud GL, Braunwald E. Modifiers of timing and possible triggers of acute myocardial infarction in the Thrombolysis in Myocardial Infarction Phase II (TIMI II) Study Group. Journal of the American College of Cardiology. 1992;20(5):1049–55. doi: 10.1016/0735-1097(92)90356-r. [DOI] [PubMed] [Google Scholar]