Abstract
Background/Aims
Home oxygen therapy (HOT) costs a great deal every year and demand for the service is growing. In Korea, health insurance has covered HOT since November 1, 2006. The objective of this study was to evaluate clinical features of patients who used long-term HOT due to chronic respiratory failure and to determine the appropriateness of oxygen prescriptions.
Methods
Between November 2006 and April 2010, patients prescribed long-term HOT were enrolled in the study at a tertiary university referral hospital and their medical records and telephone survey information were evaluated. In total, 340 patients were evaluated retrospectively.
Results
Regarding the initial indications for HOT, their mean PaO2 was 49.8 mmHg and mean SpO2 was 82.2%. Underlying diseases included chronic obstructive pulmonary disease (COPD, 19.8%), lung cancer (12.6%), and interstitial lung disease (11.2%). The admission rate within 1 year was 53.4% and the average number of admissions was 1.64/patient. Other underlying diseases for which oxygen was prescribed, despite not meeting the insurance coverage criteria, were lung cancer (36.6%) and interstitial pneumonia (16.6%).
Conclusions
Home oxygen prescriptions have increased since health insurance coverage was extended. However, cases of oxygen prescriptions frequently do not meet the coverage criteria. It is important to discuss extending the coverage criteria to other disease groups, such as interstitial lung disease and lung cancer, in terms of cost-effectiveness. Further, physicians prescribing oxygen therapy should be educated regarding the criteria.
Keywords: Chronic respiratory failure, Clinical feature, Compliance, Home oxygen therapy
INTRODUCTION
Chronic respiratory disease rates have continued to increase, and survival rates of patients with such diseases have also increased with advances in medical management and monitoring. The search for improvements in quality of life and reductions in healthcare costs is leading to the development of more home-based treatments. Home oxygen therapy (HOT) improves a patient's ability to exercise and reduces pulmonary arterial pressure, pulmonary artery resistance, and mortality [1-3]. Some studies have reported that long-term oxygen therapy decreased hospitalization, and that patients with good compliance tended to require less hospitalization [4,5]. Long-term oxygen therapy has been problematic due to poor compliance, and economic ability influences compliance [6-8]. Investigations into the realities of diseases, check-ups, and cooperation between specialists and clinics regarding HOT patients have been insufficient.
Since the national health insurance system extended insurance coverage to HOT patients with hypoxemia on November 1, 2006, in Korea, home oxygen prescriptions have increased. In this study, we investigated the clinical features of patients who were prescribed HOT. We evaluated admission rates, causes of admission, emergency room (ER) visit rates, causes of ER visits, mortality, and underlying diseases. We also assessed the appropriateness of prescribing and compliance with long-term oxygen therapy in a large group of patients.
METHODS
Patients
This retrospective clinical study initially included 340 patients over the age of 16 with a first HOT prescription at a tertiary referral university hospital between November 2006 and April 2009. We excluded patients who did not meet the HOT criteria (n = 91), so the medical records of 249 patients were reviewed and telephone surveys were performed to ask patients about compliance with HOT.
Indications for HOT
Indications for HOT are patients with PaO2 less than or equal to 55 mmHg or with SpO2 less than or equal to 88%; patients with PaO2 between 56 and 59 or SpO2 below 89%, must also have congestive heart failure, erythrocytosis (hematocrit > 55%), or pulmonary hypertension to qualify. Patients with SpO2 below 88% at exercise but SpO2 above or equal to 88% at rest also qualify.
Study design
We reviewed medical records for the following characteristics: gender; age; underlying diseases such as chronic liver disease, hypertension, and diabetes mellitus; smoking history; arterial blood gas analysis results; SpO2 as measured by pulse oximetry; admission rates and causes; ER visit rates and causes; mortality rates; and causes and dates of death. We also conducted telephone surveys about oxygen inhalation rates, inhalation methods, use of oxygen when moving, average use time of oxygen per day, symptom changes after HOT, termination of oxygen therapy, and the cause of termination.
Our study was approved by the Institutional Review Board at Seoul National University Hospital.
Statistical analysis
Data are expressed as averages and standard deviations. Survival curves were prepared using the Kaplan-Meier method. Comparison of survival curves was carried out using the log rank test. All statistical analyses were performed using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
Patient characteristics
The mean age at the time of the first prescription for oxygen therapy was 64 years. Men accounted for 63% (157/249) of the patients (Table 1). Underlying diseases included chronic obstructive pulmonary disease (COPD, 19.8%), lung cancer (12.6%), interstitial lung disease (11.2%), and tuberculosis-destroyed lung (6.9%) (Fig. 1). Physicians who prescribed oxygen therapy included pulmonologists (71.0%), oncologists (12.0%), and thoracic surgeons (3.8%). The average follow-up period was 351 days after the patients were prescribed HOT.
Table 1.
Baseline characteristics of home oxygen therapy patients
Values are presented as median (range) or number (%).
Figure 1.
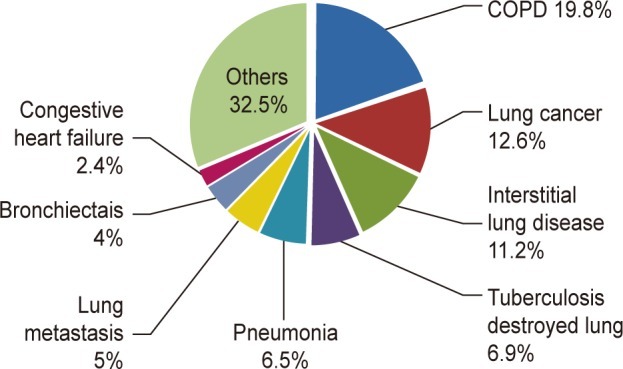
Underlying disease of home oxygen therapy patients. COPD, chronic obstructive lung disease.
Laboratory and clinical findings
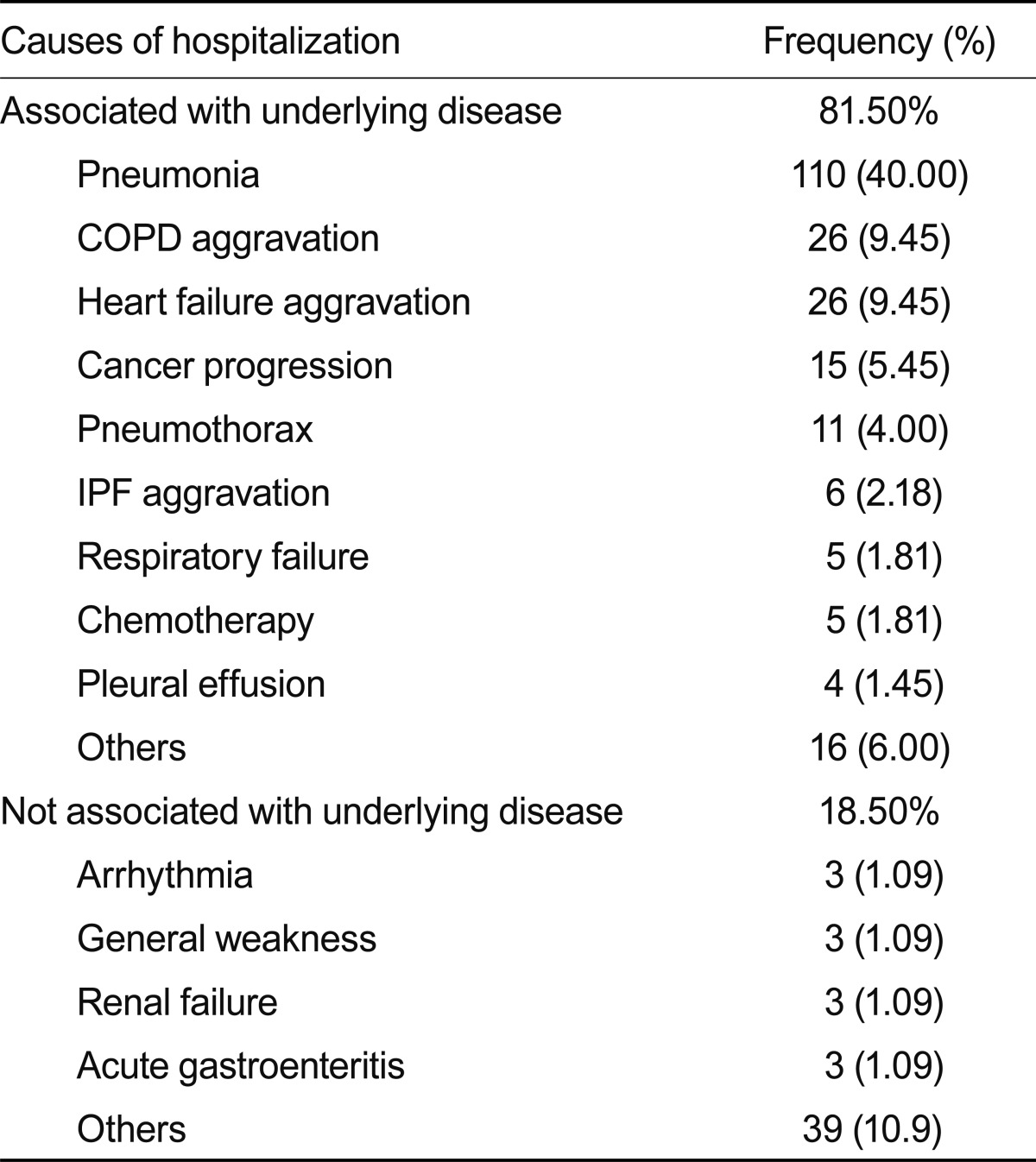
According to arterial blood gas analysis, the mean arterial partial pressure of oxygen was 49.8 ± 10.5 mmHg, and the mean arterial oxygen saturation was 82.2 ± 9.31%. After receiving a prescription for HOT, the hospitalization rate within 1 year was 53.4% and the average number of admissions of patients hospitalized at least once was 1.64/patient. The average period was 2.6 months from prescription to admission. Causes of admission included pneumonia (40.0%), acute aggravation of COPD (9.5%), acute decompensated heart failure (9.5%), progression of cancer (5.5%), and others (Table 2).
Table 2.
The cause of hospitalization
COPD, chronic obstructive lung disease; IPF, idiopathic pulmonary fibrosis.
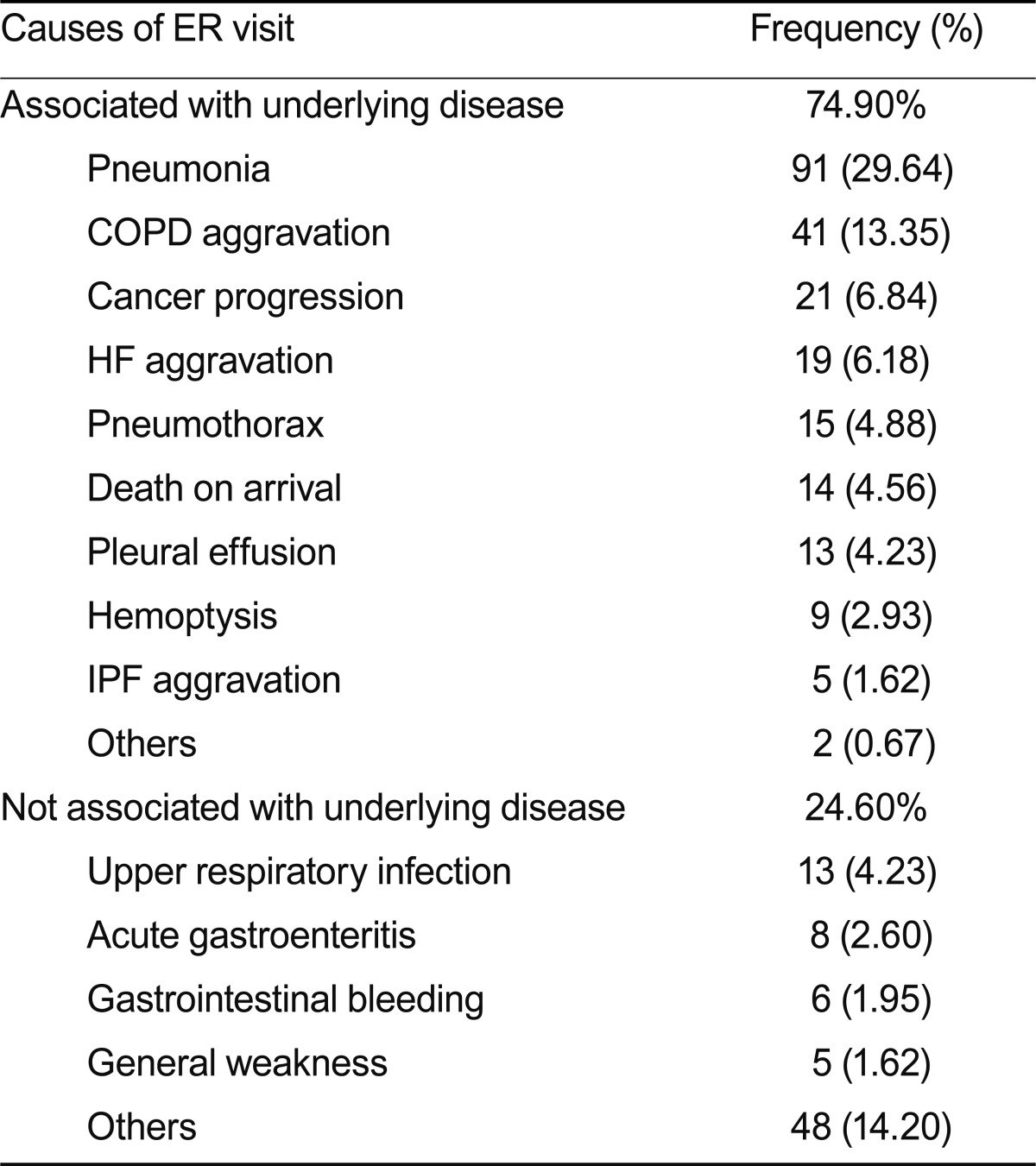
After receiving a prescription for HOT, the ER visit rate within 1 year was 54.2% and the average number of ER visits in patients who visited the ER at least once was 2.01/patient. The average time was 2.67 months from prescription to ER visit. The causes of ER visits included pneumonia (29.6%), acute aggravation of COPD (13.4%), progression of an underlying cancer 6.8%, acute decompensated heart failure (6.2%), and others (Table 3).
Table 3.
The cause of emergency room (ER) visit
COPD, chronic obstructive lung disease; HF, heart failure; IPF, idiopathic pulmonary fibrosis.
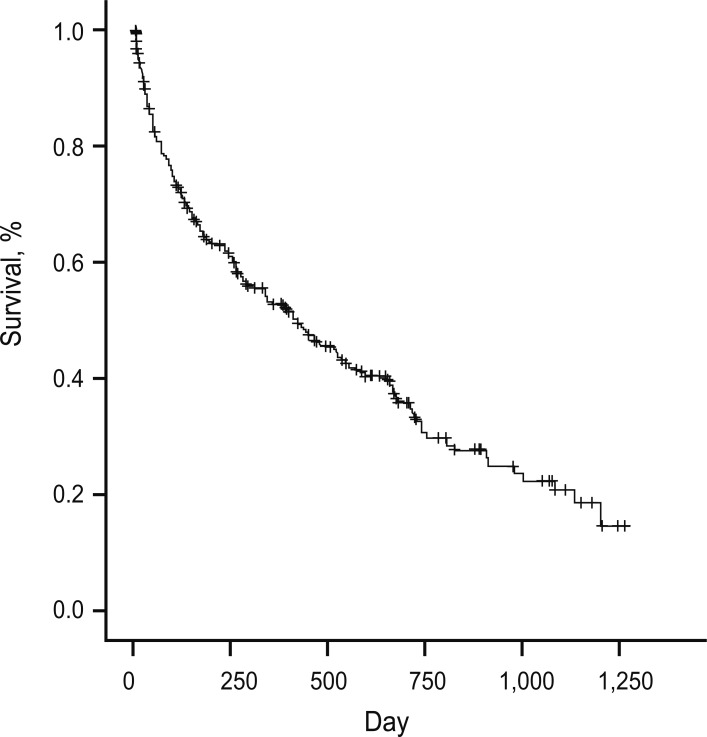
Mortality and causes of death
At the time of the telephone survey, 150 of 249 patients (60.2%) had died. Among the patients who had died, 72% (108/150) had died within 1 year, and 92% (138/150) had died within 2 years. After receiving a prescription for HOT, the 1-year mortality rate was 43.4% (108/249) and the 2-year mortality rate was 55.4% (138/249) (Fig. 2).
Figure 2.
Survival of home oxygen therapy patients (Kaplan-Meier analysis).
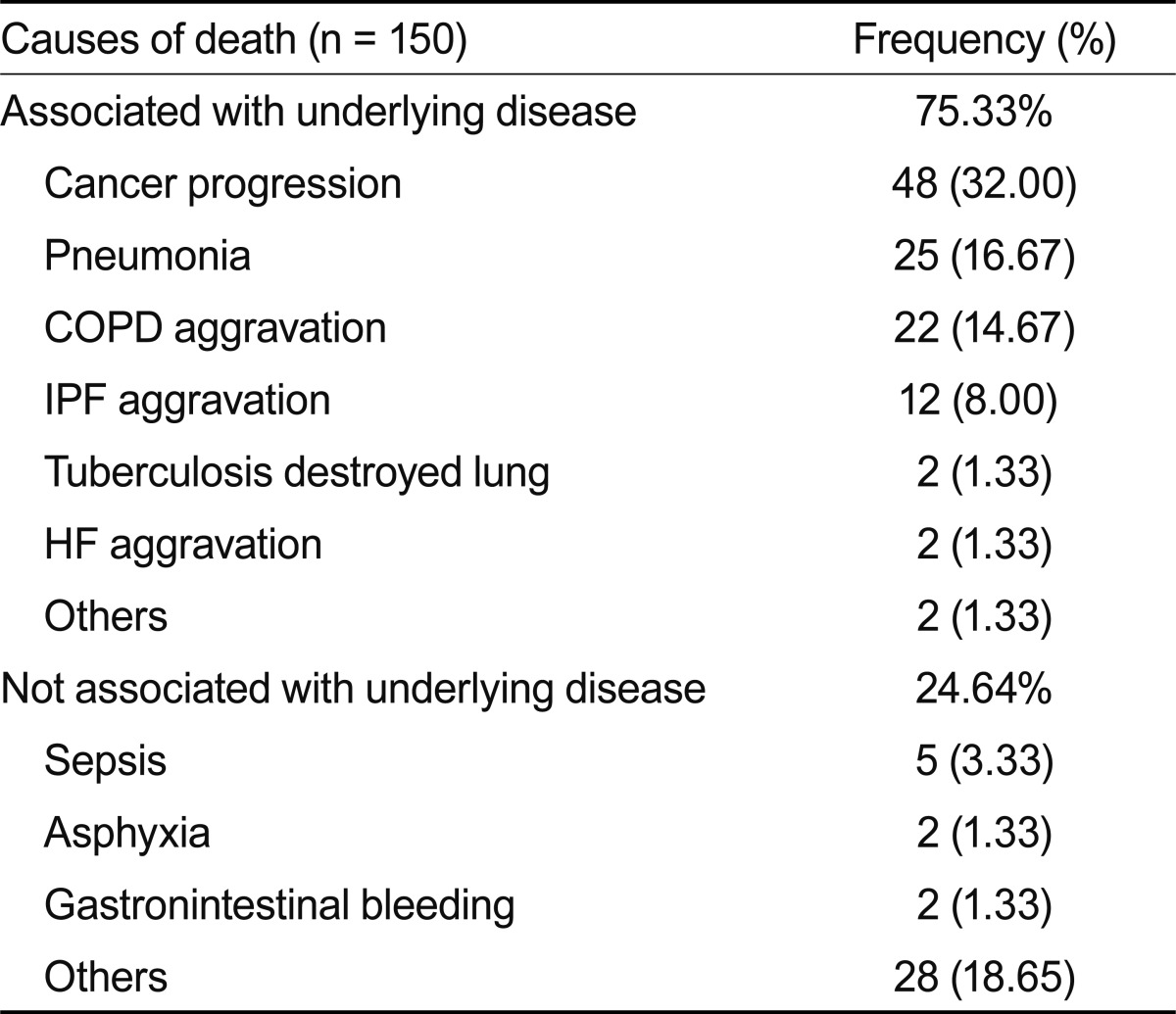
Major causes of death included progression of underlying cancers (32%, 48/150), pneumonia (16.7%, 25/150), and acute aggravation of COPD (14.7%, 22/150) (Table 4).
Table 4.
The cause of death
Values are presented as number (%).
COPD, chronic obstructive lung disease; IPF, idiopathic pulmonary fibrosis; HF, heart failure.
Compliance with HOT
We contacted the 74 patients being followed as outpatients regarding our survey about compliance. A total of 9 patients could not be reached by telephone, and 1 patient refused to participate in the telephone survey.
Of the 64 respondents, 44 patients were using HOT and 20 were not using HOT. Among the 20 patients who did not use HOT, 7 patients had not used it from the beginning. Among the 13 patients who had discontinued HOT, 12 patients had stopped using it because of symptomatic improvement, and 1 patient had stopped treatment because HOT was ineffective in relieving dyspnea. The mean duration of oxygen use was 6.8 ± 4.2 months.
Among the 44 patients who were using HOT, the mean oxygen usage time per day was 14.2 ± 8.8 hours and the mean amount of oxygen used per day was 1.8 ± 0.9 L/min; 55% of patients used oxygen for longer than 15 hr/day, and 32.8% of patients used portable oxygen when moving around.
Appropriateness of HOT prescribing
Among the patients we assessed, 91 did not meet the insurance criteria for oxygen therapy. Their underlying diseases included lung cancer 36.2% (33/91), interstitial lung disease 16.5% (15/91), and asthma 4.4% (4/91) (Fig. 3). The physicians who prescribed oxygen, despite patients not meeting the insurance coverage criteria, included thoracic surgeons (69.2%), oncologists (46.3%), and pulmonologists (21.6%).
Figure 3.
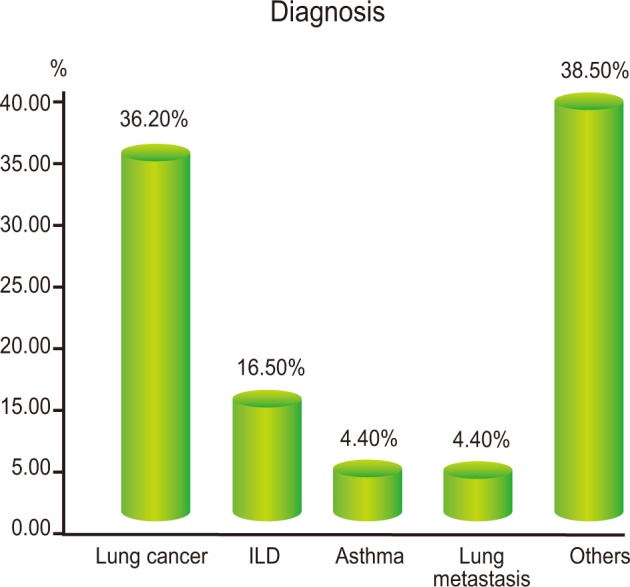
Underlying diseases did not meet the insurance criteria for home oxygen therapy. ILD, interstitial lung disease.
DISCUSSION
The Medical Research Council study and the Nocturnal Oxygen Therapy Trial demonstrated that long-term oxygen therapy treatment improved survival in patients with hypoxic COPD [1]. Oxygen therapy must be provided for at least 15 hours to be effective. HOT improves a patient's ability to exercise and reduces pulmonary artery pressure [9,10], pulmonary artery resistance, and mortality [11]. In Korea, insurance now covers some HOT. In this study, we sought to determine underlying diseases, clinical features, and compliance among patients who received home oxygen prescriptions. Using these data, we evaluated whether current oxygen prescriptions are appropriate and whether the insurance coverage criteria are appropriate.
A domestic study reported that the average oxygen usage time was 14.5 ± 7.9 hours and patients using oxygen less than 8 hr/day accounted for 34% of cases [12]. Compliance might be expected to increase after insurance coverage, but no significant differences were reported by another study conducted after insurance coverage began [13]. In that study, the average oxygen usage time was 9.8 ± 7.3 hours. In contrast, we found that the average oxygen usage time was 14.2 ± 8.8 hours and that 55% of patients used it for longer than 15 hours. When compared with the former study, our respondents exhibited improved compliance. Also, in the previous domestic study, no patient used portable oxygen [13], whereas 32.8% of our respondents used portable oxygen. This finding seemed to be due to improvements in patient awareness and the education of patients over time.
Ringbaek et al. [4] reported that HOT reduced hospital admission rates from 92.7% to 63.8% among COPD patients. This effect was particularly notable among the compliant group. Silverman et al. [14] demonstrated that the most common causes of hospitalization in patients on long-term oxygen therapy were heart failure, COPD exacerbations, and lung infections [12,14]. In the present study, the admission rate within 1 year was 53.4%. Our results correspond well with those of an earlier study on the causes of admission [4]. We found that most common causes of hospital admission were pneumonia (40.0%), acute aggravation of COPD (9.5%), and acute decompensated heart failure (9.5%).
Huh et al. [12] reported that the 1-year mortality rate was 21% and the 3-year mortality rate was 46%. In the present study, the 1-year mortality rate was 43.4% and the 2-year mortality rate was 55.4%. Among the patients who died, 72% of patients died within 1 year and 92% died within 2 years. This was the result of many advanced lung cancer and severe COPD patients at this tertiary hospital.
The insurance coverage criteria were based on studies of COPD patients. However, we investigated underlying diseases with HOT, and found that COPD patients represented only 19.8% of oxygen prescriptions. The major underlying diseases were lung cancer, interstitial lung disease, and tuberculosis-destroyed lung. Furthermore, diseases not meeting the insurance criteria-lung cancer, interstitial lung disease, and asthma-accounted for 57.1% of all prescriptions. These patients were considered to need oxygen therapy as a result of their physicians' decisions or their own complaints of dyspnea, even though they did not meet the insurance criteria. It is important to discuss increasing the coverage criteria for certain diseases, such as lung cancer and interstitial lung disease.
Koo et al. [13] reported that the 36% of patients voluntarily discontinued oxygen therapy. Causes of discontinuance included discomfort with oxygen therapy, difficulty with oxygen prescriptions, and economic problems. These findings differed from the symptomatic improvement observed in the present study: of the 13 patients who discontinued oxygen therapy, 12 did so because of symptomatic improvement.
In conclusion, oxygen prescriptions have increased since the extension of insurance, and patient compliance is improving over time. However, many patients with diseases that do not meet the insurance coverage criteria are being treated with HOT. Indeed, we found that lung cancer, interstitial lung disease, and asthma accounted for more than half of all cases. It is important to discuss extending the medical insurance coverage criteria to certain other disease groups.
Footnotes
No potential conflict of interest relevant to this article is reported.
References
- 1.Long term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema: report of the Medical Research Council Working Party. Lancet. 1981;1:681–686. [PubMed] [Google Scholar]
- 2.Nocturnal Oxygen Therapy Trial Group. Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: a clinical trial. Ann Intern Med. 1980;93:391–398. doi: 10.7326/0003-4819-93-3-391. [DOI] [PubMed] [Google Scholar]
- 3.Miyamoto K, Aoi K, Kawakami Y. Effect of home oxygen therapy on prognosis of patients with chronic pulmonary disease associated with pulmonary hypertension. Nihon Kyobu Shikkan Gakkai Zasshi. 1992;30(Suppl):175–179. [PubMed] [Google Scholar]
- 4.Ringbaek TJ, Viskum K, Lange P. Does long-term oxygen therapy reduce hospitalisation in hypoxaemic chronic obstructive pulmonary disease? Eur Respir J. 2002;20:38–42. doi: 10.1183/09031936.02.00284202. [DOI] [PubMed] [Google Scholar]
- 5.Crockett AJ, Moss JR, Cranston JM, Alpers JH. The effects of home oxygen therapy on hospital admission rates in chronic obstructive airways disease. Monaldi Arch Chest Dis. 1993;48:445–446. [PubMed] [Google Scholar]
- 6.Barjhoux C, Pepin JL, Deschaux-Blanc C, et al. Long-term oxygen therapy at home: compliance with the medical prescription and observance of the daily duration of at least 15 hours. Rev Mal Respir. 1994;11:37–45. [PubMed] [Google Scholar]
- 7.Demirel H, Demir T, Umut S. Retrospective evaluation of patient compliance in continuous oxygen therapy. Respiration. 2003;70:149–153. doi: 10.1159/000070061. [DOI] [PubMed] [Google Scholar]
- 8.Costello RW, Liston R, McNicholas WT. Compliance at night with low flow oxygen therapy: a comparison of nasal cannulae and venturi face masks. Thorax. 1995;50:405–406. doi: 10.1136/thx.50.4.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nonoyama ML, Brooks D, Lacasse Y, Guyatt GH, Goldstein RS. Oxygen therapy during exercise training in chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2007;(2):CD005372. doi: 10.1002/14651858.CD005372.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Toyama T, Seki R, Kasama S, et al. Effectiveness of nocturnal home oxygen therapy to improve exercise capacity, cardiac function and cardiac sympathetic nerve activity in patients with chronic heart failure and central sleep apnea. Circ J. 2009;73:299–304. doi: 10.1253/circj.cj-07-0297. [DOI] [PubMed] [Google Scholar]
- 11.Weitzenblum E, Sautegeau A, Ehrhart M, Mammosser M, Pelletier A. Long-term oxygen therapy can reverse the progression of pulmonary hypertension in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis. 1985;131:493–498. doi: 10.1164/arrd.1985.131.4.493. [DOI] [PubMed] [Google Scholar]
- 12.Huh JW, Lee JY, Hong SB, et al. Long-term oxygen therapy in patients with chronic respiratory failure in one university hospital. Tuberc Respir Dis. 2005;58:160–166. [Google Scholar]
- 13.Koo HS, Song YJ, Lee SH, et al. Clinical characteristics and adherence of patients who were prescribed home oxygen therapy due to chronic respiratory failure in one university hospital: survey after national health insurance coverage. Tuberc Respir Dis. 2009;66:192–197. [Google Scholar]
- 14.Silverman BG, Gross TP, Babish JD. Home oxygen therapy in medicare beneficiaries, 1991 and 1992. Chest. 1997;112:380–386. doi: 10.1378/chest.112.2.380. [DOI] [PubMed] [Google Scholar]