Abstract
Study Objectives:
To evaluate the prevalence of severe insomnia symptoms and the extent to which they are associated with daytime impairments in comorbid mood and anxiety disorders.
Design:
Nationally representative cross-sectional survey.
Setting:
National Comorbidity Survey-Replication (NCS-R).
Participants:
There were 5,692 NCS-R respondents with no mood or anxiety disorder (n = 3,711), mood disorders only (n = 327), anxiety disorders only (n = 1,137), and coexisting mood and anxiety disorders (n = 517).
Interventions:
N/A.
Measurements and Results:
Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition disorders and severe insomnia symptoms in the past year were assessed using the World Health Organization (WHO) Composite International Diagnostic Interview. The World Health Organization Disability Assessment Schedule (WHO-DAS) indexed eight domains of daytime impairment in the past 30 days, which included self-care, mobility, cognition, social functioning, time out of role, and four components of productive role functioning. Respondents with comorbid mood and anxiety disorders had significantly higher rates of severe insomnia complaints (42.1-62.8%) relative to the three other groups. Severe insomnia complaints were also significantly more prevalent in individuals with mood (25.2-45.6%) or anxiety disorders only (24.9-45.5%) relative to those with no disorder (12.4-24.3%). Moreover, endorsing a severe insomnia complaint in the past year was associated with increased days of impairment across all past-month WHO-DAS domains for respondents with mood-anxiety comorbidity. For the remaining groups, severe insomnia complaints were related to increased days of impairment across all domains except self-care, and additionally mobility for the group with mood disorders only.
Conclusions:
Comorbid mood and anxiety disorders are associated with high rates of severe insomnia complaints, which were independently associated with substantial functional impairment.
Citation:
Soehner AM; Harvey AG. Prevalence and functional consequences of severe insomnia symptoms in mood and anxiety disorders: results from a nationally representative sample. SLEEP 2012;35(10):1367–1375.
Keywords: Mood disorders, anxiety disorders, insomnia
INTRODUCTION
In psychiatric illness it is clear that comorbidity, or co-occurrence of multiple psychiatric disorders, is the norm and not the exception.1–3 More than 60% of respondents in the Epidemiologic Catchment Area Study with at least one lifetime psychiatric disorder had two or more disorders,1 and the first National Comorbidity Survey found that individuals with a psychiatric diagnosis had an average of 2.1 Diagnostic and Statistical Manual of Mental Disorders, Third Edition (DSM-III) disorders.2 Hence, there is a keen need to study psychiatric comorbidity and factors exacerbating the course of these disorders. The current study aims to contribute to unlocking the puzzle of comorbidity by focusing on the functional ramifications of insomnia symptoms in the frequently comorbid conditions of mood and anxiety disorders.
Epidemiologic surveys from the United States and Europe have consistently shown high comorbidity rates for anxiety and mood disorders. Approximately 50-90% of individuals with the principal diagnosis of a mood disorder have anxiety disorder comorbidity4–6 and 60-70% with a primary diagnosis of an anxiety disorder have mood disorder comorbidity.7 Moreover, coexisting mood and anxiety disorders are associated with an earlier principal disorder onset, a more severe and chronic course of the principal disorder, greater functional impairment, greater healthcare utilization, and significantly poorer long-term outcomes.8–11 Thus, there is a great need to shed light on novel directions for improving current treatments to achieve more complete and sustained remission in individuals with comorbid mood and anxiety disorders.
The contribution of sleep disturbance to the onset, exacerbation, and maintenance of mood and anxiety disorders has received greater attention in the past decade. Notably, symptoms of insomnia are present in 20-40% of individuals with mental illness,12 with those meeting criteria for mood disorders or anxiety disorders exhibiting even higher rates of insomnia, approximately 50-70% and 70-90%, respectively.13–16 Returning to the issue of psychiatric comorbidity, individuals with multiple psychiatric disorders appear to be at greater risk of insomnia complaints.17 Yet, relatively little is known specifically about the prevalence of insomnia symptoms in coexisting mood and anxiety disorders. In a recent study examining insomnia complaints in residents of The Netherlands with major depression and anxiety disorders, Van Mill and colleagues13 found higher rates of insomnia in respondents with comorbid depression and anxiety disorders in comparison with those with major depression only or an anxiety disorder only. In a broader sample of the European population (United Kingdom, Germany, Italy, Portugal), Ohayon and Roth18 noted a similar finding, with severe insomnia being more common in participants with depression-anxiety comorbidity. However, these studies focused on major depression only, not the broader set of mood disorders. Notably, individuals with bipolar disorder and dysthymia experience high rates of anxiety comorbidity as well, with some studies noting rates higher than major depression.6,19,20 Therefore, we seek to expand upon the current literature by examining the prevalence of insomnia complaints in a more complete set of mood disorders, which includes major depressive disorder, bipolar disorders (types I and II), and dysthymia. The current study also extends a prior investigation of sleep related impairment in psychiatric disorders in the National Comorbidity Survey-Replication (NCS-R). Roth and colleagues17 reported the prevalence rates of insomnia symptoms in individual psychiatric disorders, as well as the prevalence of insomnia symptoms in 0, 1, 2, and 3 or more comorbid psychiatric disorders, and role impairment that occurred as a result of sleep problems. The current study expands upon that investigation by adopting a specific focus on mood-anxiety comorbidity and examining a broader range of functional impairments.
Investigating insomnia in coexisting mood and anxiety disorders is important because insomnia complaints can have a profound effect on the course of mood and anxiety disorders. In individuals with major depression, those with insomnia symptoms have poorer quality of life, higher rates of anxiety comorbidity, and greater risk of depression recurrence.14,21 Indeed, insomnia complaints are associated with greater daytime impairment in psychiatric disorders,17,22,23 are often a residual symptom after treatments for mood and anxiety,24–28 and serve as a predictor of mood and anxiety disorder onset and relapse.18,29–31 Previous studies examining the effect of insomnia complaints on impairment in psychiatric disorders often focus on broad categories of days lost/unproductive work days17,23,32–34 or general mental/physical health-related quality of life.23,33 To the best of our knowledge, no study has examined how insomnia complaints in the context of mood and anxiety disorders influence a broad set of functional domains, such as self-care, cognition, social functioning, and mobility, in addition to days out of role and facets of role impairment.
The first aim of the current study was to use the NCS-R dataset to examine the relative prevalence of severe insomnia symptoms (difficulty falling asleep, difficulty maintaining sleep, early morning awakening, any one insomnia complaint) in respondents with comorbid mood and anxiety disorders, mood disorders only, anxiety disorders only, and neither mood nor anxiety disorder. It was predicted that the prevalence of self-reported severe insomnia symptoms would be lowest in respondents with neither disorder, significantly higher in respondents with mood disorders only or anxiety disorders only, and greatest in respondents endorsing mood-anxiety comorbidity. The second aim was to assess whether the presence of a severe insomnia complaint uniquely contributed to daytime impairment in each of the four previously mentioned diagnostic groups. To address this aim, our prediction was that across diagnostic groups insomnia would be independently associated with impairment across several domains of daytime functioning.
METHODS
Participants
Participants were identified from the NCS-R sample. The NCS-R is a nationally representative community household survey of mental illness that was conducted between February 2001 and April 2003.35 A total of 9,282 respondents participated in the 2-part survey, which had an overall response rate of 70.9%.35 Consent was verbal rather than written to be consistent with the recruitment procedures used in the original National Comorbidity Survey.36 The Human Participants Committees of Harvard Medical School and the University of Michigan approved all field procedures. A detailed description of the design and field procedures used in the NCS-R can be found elsewhere35 but are briefly described in the following paragraphs.
Sampling for the NCS-R included the contiguous 48 states and was limited to English speakers and persons living in noninstitutionalized households or on campuses where respondents had permanent addresses. In Part I of the NCS-R, respondents completed a diagnostic interview using the WHO Composite International Diagnostic Interview (CIDI 3.0).37 A probability subsample of 5,692 Part I respondents were reassessed in a second part of the survey. Part II consisted of all Part I respondents with any DSM-IV CIDI diagnosis and a probability subsample of those with no such diagnosis. The assessment of insomnia symptoms and impairment were included in Part II of the NCS-R.
Demographic Characteristics
Several sociodemographic characteristics were assessed, including age at interview (18-34, 35-49, 50-64, 65+ yr), sex (female, male), race (Caucasian, all others), marital status (married/cohabiting, divorced, other), education (< 12 yr, ≥ 12 yr) and household income (low, low-average, high-average, high). Household income was assessed relative to the federal poverty line, which was categorized as low income (< poverty line), low-average income (1-3 times the poverty line), high-average income (3-6 times the poverty line) and high income (> 6 times the poverty line).
12-Month Psychiatric Diagnoses
Psychiatric disorders in the year preceding the interview were based on the CIDI 3.0.37 Mood disorders (major depressive disorder, dysthymia, bipolar disorder) and anxiety disorders (panic disorder, agoraphobia, specific phobia, social phobia, generalized anxiety disorder, posttraumatic stress disorder) occurring in the past year were assessed using DSM-IV criteria. A sample of 5,692 respondents was divided into four non-overlapping groups: no mood or anxiety disorder (n = 3,711), mood disorder only (n = 327), anxiety disorders only (n = 1,137), and comorbid mood and anxiety disorders (n = 517). Participants were selected based on a 12-month diagnosis, given that sleep problems were assessed in the past year only. Substance (drug abuse and dependence) and alcohol use disorders (alcohol abuse and dependence) occurring in the past year were considered as covariates in analyses.
Chronic Physical Conditions
Given that comorbid physical conditions are associated with increased risk for sleep disturbance and impairment,23 for the current study we opted to control for the presence of chronic physical conditions. Fifteen physical disorders present in the past 12 months were assessed with a chronic conditions checklist based on the list in the US National Health Interview Survey.38 Five broad classes of physical disorders were assessed, including cardiovascular, musculoskeletal, respiratory, pain, and other conditions. These disorders were collapsed into a categorical variable to represent the presence of 0, 1, 2, or 3 or more physical conditions.
Insomnia Symptoms
In Part II of the NCS-R, respondents were asked a series of three yes-no questions related to the presence of severe insomnia symptoms. These questions focused on “periods lasting two weeks or longer in the past 12 months” when the respondent experienced (1) difficulty initiating sleep (“nearly every night it took you 2 hr or longer before you could fall asleep”), (2) difficulty maintaining sleep (“you woke up nearly every night and took an hour or more to get back to sleep”) and (3) early morning awakening (“you woke up nearly every morning at least 2 hr earlier than you wanted to”). Difficulty initiating sleep, difficulty maintaining sleep, and early morning awakening represent the three classic forms of sleep difficulties specified in the DSM-IV-Text Revision (TR) definition of insomnia. Note that a formal diagnosis of insomnia could not be made based on DSM-IV-TR39 or International Classification of Sleep Disorders, 2nd Edition40 criteria, as sleep-related distress and daytime impairment were not reported. An insomnia score (0-3) was derived to denote the number of different sleep symptoms endorsed.
Functional Impairment
Functional impairment in the past 30 days was assessed with eight measures taken from the World Health Organization Disability Assessment Schedule-II (WHO-DAS).41 This measure assesses the frequency of difficulties experienced over the past 30 days (range 0-30) in several domains of basic functioning. These domains included mobility (e.g., standing, walking), self-care (e.g., bathing, dressing), cognition (e.g., concentrating, remembering), social role performance (i.e., conversing, maintaining emotional control while around others), time out of role (i.e., unable to carry out normal daily activities or work), reduced quantity of work (i.e., able to carry out normal activities but had to cut down on what was done or unable to get as much done); reduced quality of work (i.e., reduced quality of work or how carefully work was completed) and extreme effort (i.e., needed to make an extreme effort carry out normal daily activities). Due to the difference in the time frames for insomnia symptoms (past 12 months) and impairment measures (past 30 days), estimates for these outcomes should be interpreted as days of impairment in the past month associated with insomnia symptoms in the past year. As a result, the effects in the current study are presumably lower than the effects of current insomnia symptoms on current daytime impairment.
Analysis Methods
All analyses were conducted with sample weighting from Part II of the NCS-R using Stata 12.0 (Stata Corporation, College Station, TX, 2011). Because the sample design used weighting and clustering, all parameters were estimated by using the Taylor series linearization method. Further information on NCS-R sample weighting procedures can be found elsewhere.35 Briefly, the Part II NCS-R sample was weighted to adjust for differences in probabilities of selection, differential non-response, and residual differences between the sample and the US population on a range of sociodemographic and geographic factors assessed in the 2000 census. Rao-Scott chi-square tests (which are converted to an F statistic by Stata) were used to detect design-corrected differences in categorical measures across groups. In the tables, categorical variables are expressed as weighted percentages and their standard errors. To test the first hypothesis, chi-square tests and logistic regression analyses assessed rates of insomnia symptoms in each of the diagnostic groups. To test the second hypothesis, a series of linear regression models were run to assess the independent association of an insomnia complaint to the eight WHO-DAS 30-day impairment domains. Statistical significance was evaluated using a 2-sided design with alpha set at 0.05. All regressions adjusted for demographic (age, sex, income status, education, employment status, marital status) and clinical (12-month alcohol use disorder, 12-month substance use disorder, smoking status, chronic conditions) covariates.
RESULTS
Demographic and Clinical Characteristics
Table 1 describes the demographic characteristics of each diagnostic group. Race, income, and education level did not significantly differ among the four groups. In comparison with the group with neither disorder, a greater proportion of individuals with mood, anxiety, or comorbid disorders were younger (18-35 yr), female, unmarried, current smokers, and had more chronic physical conditions (P < 0.05). Relative to respondents with mood disorders only or anxiety disorders only, participants with comorbid disorders were more frequently in the 35-49 yr age range and were more likely to be unmarried, endorse a greater number of chronic physical conditions, and be unemployed (P < 0.05). Respondents with comorbid disorders or mood disorders only tended to have a lower income than participants with neither disorder (P < 0.05). Finally, respondents with anxiety disorders less frequently endorsed smoking than those with comorbid disorders (P < 0.05).
Table 1.
Demographic and health characteristics by diagnostic group
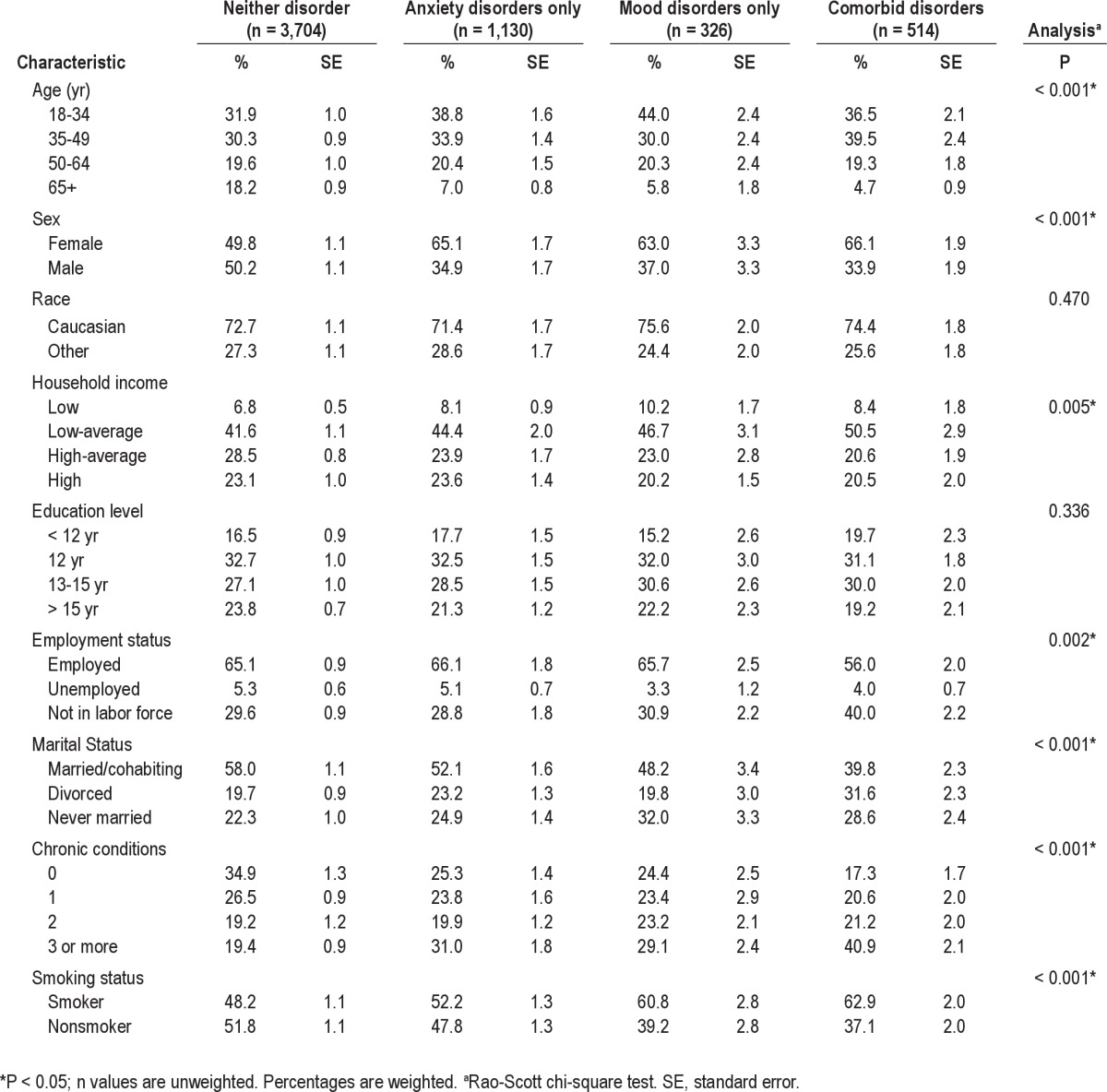
Differences in the distribution of specific mood and anxiety disorders were also assessed across the diagnostic groups. Taking mood disorders first, the comorbid group was composed of higher rates of dysthymia and bipolar disorder type II, and lower rates of major depressive disorder, in comparison with the mood disorder-only group (P < 0.05). Bipolar disorder type I prevalence did not differ between groups. Regarding anxiety disorders, the comorbid disorders group was made up of a higher proportion of individuals with panic disorder, agoraphobia without panic disorder, specific social phobia, generalized anxiety disorder, and posttraumatic stress disorder than the anxiety disorders-only group (P < 0.05). Rates of agoraphobia with panic disorder did not differ between the comorbid and anxiety disorder groups (P > 0.05). The greater proportion of anxiety disorders in the comorbid group may be related to the fact that, compared with the anxiety disorders-only group, respondents with comorbid disorders reported a significantly greater number of anxiety disorders per person (1.78 versus 1.37; P < 0.001). Alcohol use disorder prevalence in the mood disorders-only group did not significantly differ from the anxiety disorders-only group; however, both groups more frequently endorsed alcohol use disorders relative to respondents with no such diagnosis (P < 0.05). Participants with comorbid disorders endorsed significantly higher rates of alcohol use disorders than each of the three other groups (P < 0.05). Substance use disorders were more prevalent in the mood disorders-only group and comorbid disorders group compared with that of respondents with neither disorder (P < 0.05). Finally, respondents with comorbid disorders also more frequently met criteria for substance use disorders than the anxiety disorders-only group (P < 0.05).
Insomnia Symptoms
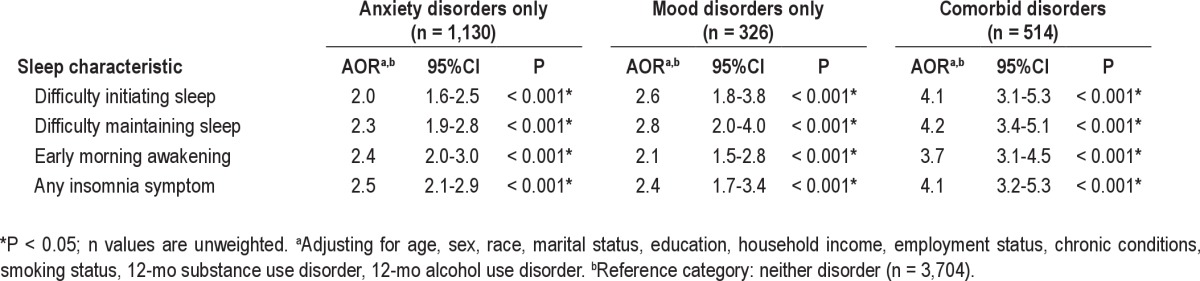
To address the first aim, the prevalence of severe insomnia symptoms was compared across diagnostic groups. As presented in Table 2, respondents with comorbid mood and anxiety disorders had significantly higher rates of at least one insomnia symptom, as well as each of the specific insomnia symptoms (difficulty falling asleep, difficulty staying asleep, and early morning awakening) in comparison with the other three groups. Insomnia symptom prevalence in the mood disorders-only group did not significantly differ from that of the anxiety disorders-only group; however, both groups more frequently endorsed insomnia symptoms compared with respondents with neither disorder (P < 0.05). Finally, participants with comorbid disorders endorsed a significantly higher number of insomnia symptoms than each of the three other groups (P < 0.05). Respondents in the mood and anxiety disorders-only groups did not significantly differ their average number of insomnia symptoms, but both groups endorsed more symptoms than respondents with neither disorder (P < 0.05). As presented in Table 3, this pattern of results remained after controlling for sociodemographic and clinical factors in logistic regression analyses (P < 0.05). The odds ratios presented are from the additive interaction model (Table 4). We did not find evidence of synergistic nor multiplicative effects of diagnostic status on insomnia symptoms (data not shown; available upon request). Prevalence of insomnia symptoms in each psychiatric disorder can be found in previously published work.17
Table 2.
Prevalence of 12-mo DSM-IV disorders by diagnostic group
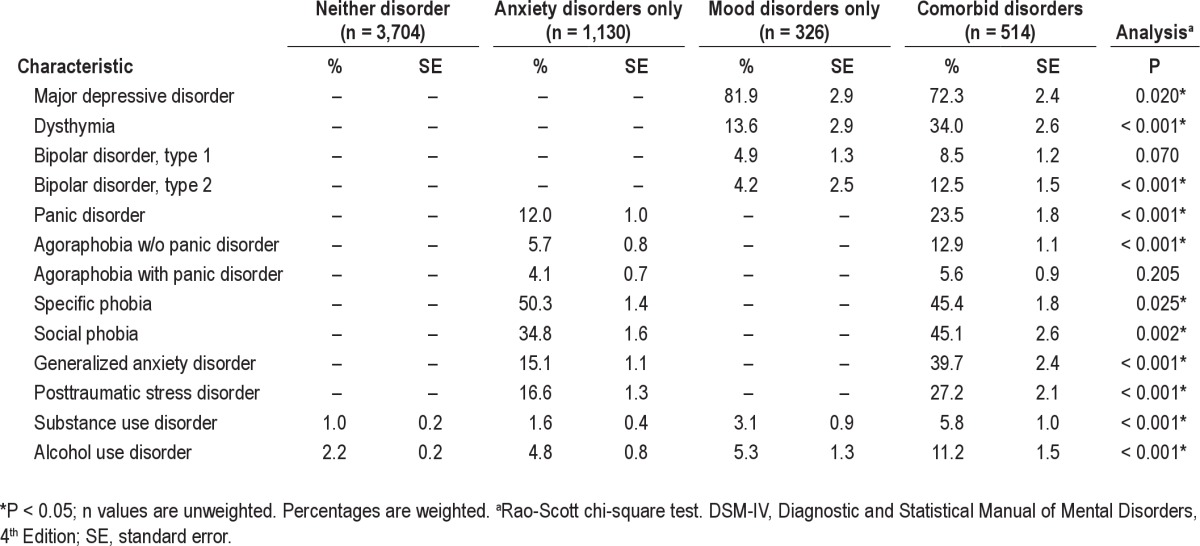
Table 3.
Prevalence of insomnia symptoms by diagnostic group
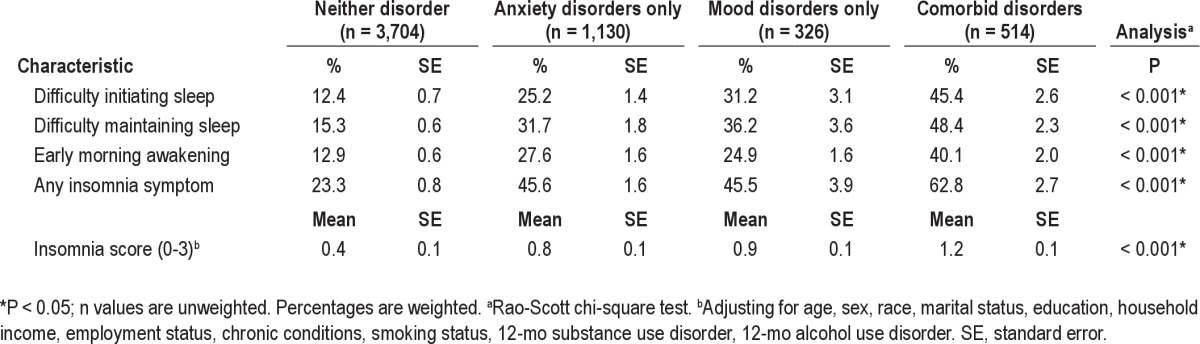
Table 4.
Adjusted odds ratios (AORs)a,b and 95% confidence intervals (CI) for insomnia symptoms across diagnostic groups
Functional Impairment
To address the second aim, we examined whether endorsing at least one severe insomnia complaint in the past year uniquely related to 30-day impairment for each diagnostic group (comorbid mood and anxiety disorder, anxiety disorder only, mood disorder only, neither disorder). Table 5 illustrates the effect of an insomnia symptom on each of the eight WHO-DAS impairment domains (mobility, cognition, self-care, social functioning, reduced quality of work, reduced quantity of work, time out of role, and extreme effort) by diagnostic group.
Table 5.
Adjusteda mean days of functional impairment in each of the 8 WHO-DAS domains, by diagnostic group and insomnia symptom subgroup
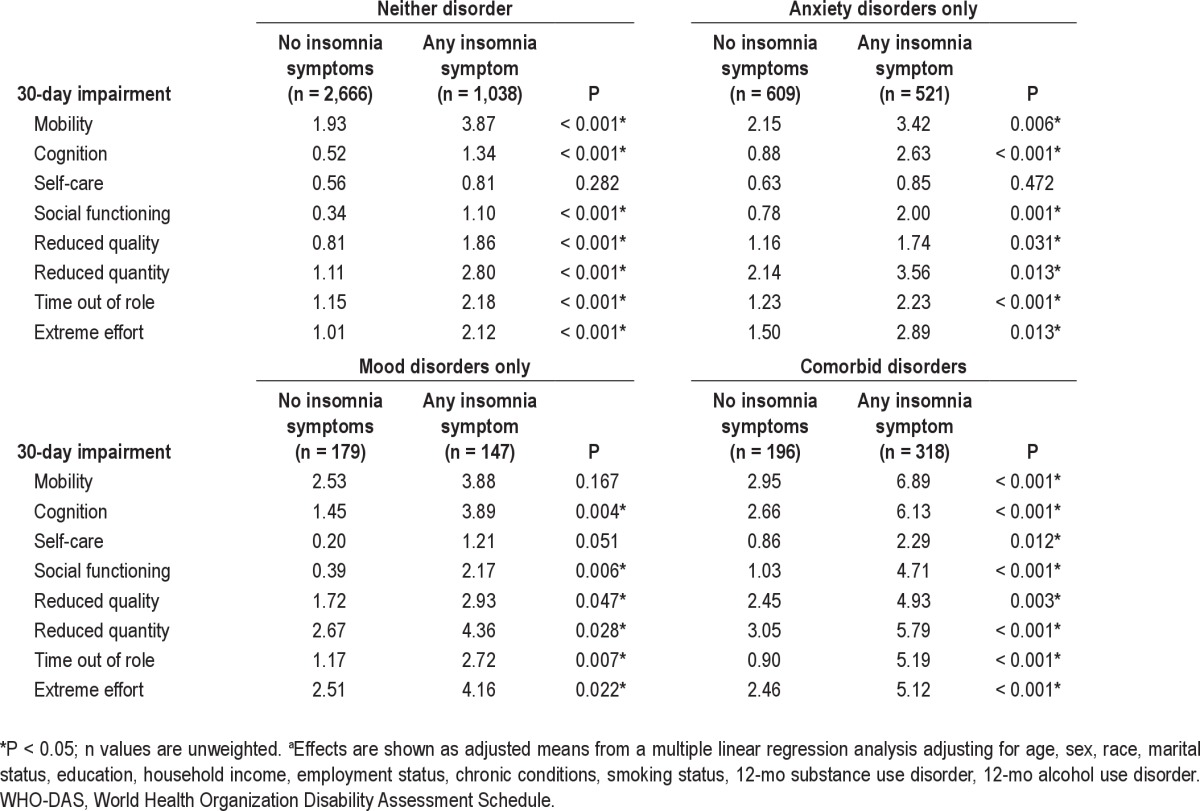
The presence of at least one insomnia symptom in the past year was associated with significantly greater days of impairment across all WHO-DAS domains for respondents with comorbid disorders. Additionally, for the group with anxiety disorders only and the group with neither disorder, insomnia symptoms were associated with more days of impairment across all domains except self-care. Finally, in the mood disorders-only group, insomnia symptoms were associated with significant impairment in all domains except mobility and self-care.
DISCUSSION
This study is the first, to the best of our knowledge, to evaluate the prevalence of severe insomnia symptoms and the extent to which they are associated with specific daytime impairments in comorbid mood and anxiety disorders. The first aim was to examine the prevalence rates of severe insomnia symptoms across four diagnostic groups, NCS-R respondents with comorbid mood and anxiety disorders, mood disorders only, anxiety disorders only, and neither disorder. Consistent with our hypothesis, the rates of individual insomnia symptoms, as well as any one insomnia complaint, were lowest in respondents with neither disorder, significantly higher in respondents with a mood disorder only or anxiety disorders only, and greatest in respondents endorsing mood-anxiety comorbidity. This pattern of findings remained even after controlling for sociodemographic and clinical characteristics. Interestingly, approximately 60% of individuals with comorbid mood and anxiety disorders endorsed at least one insomnia complaint, whereas the prevalence in individuals with mood disorders only or anxiety disorders only was approximately 45%. However, although the trend of insomnia symptom prevalence rates in the current study were in the predicted direction, the prevalence of insomnia symptoms in the anxiety and mood disorders-only groups were slightly lower than previous studies.13–16 This is not surprising as the NCS-R examined severe insomnia symptoms, with duration criteria of 2 or more hours to fall asleep, 1 or more hours awake at night and waking up 2 or more hours early. These findings seem justified given that severe insomnia complaints confer a more deleterious effect on daytime functioning42 and make the prevalence rates of insomnia symptoms across the mood, anxiety, and comorbid disorders observed in this study all the more striking.
The second aim of the current study was to assess whether a severe insomnia complaint in the past year was associated with more days of impairment across eight domains (mobility, cognition, self-care, social functioning, reduced quality of work, reduced quantity of work, time out of role, and extreme effort) in the past month for each of the four diagnostic groups. Consistent with previous research, insomnia symptoms were related to significantly reduced productive role functioning and increased time out of role across all diagnostic groups.17,23,33 In a unique contribution, the current study found that, even after controlling for a host of sociodemographic and clinical covariates, respondents with insomnia complaints were significantly more impaired across several additional domains; namely social functioning, cognition, self-care, and mobility. These results underscore the public health imperative to better identify and address insomnia comorbidity with the aim of reducing both societal and individual impact.
To our knowledge, the current investigation is also the first to systematically examine the relationship between insomnia symptoms and functional impairment in individuals with comorbid mood and anxiety disorders. Interestingly, insomnia complaints were associated with substantially increased days of impairment across all domains for the group with comorbid disorders. In contrast, insomnia symptoms were not significantly related to self-care in the other three groups and mobility was not impaired in the mood disorders group. The pattern of impairment across a wide variety of domains linked to insomnia symptoms may highlight the fact that sleep problems in individuals with mood-anxiety comorbidity could either be a marker or risk factor for a more severe course of illness. Indeed, yearly insomnia complaints were associated with an extra 4.29 days out of role in the past month for the comorbid disorders group, compared with approximately 1-1.2 days for the other diagnostic groups. Thus, these findings also point to the possibility that addressing insomnia complaints in comorbid mood and anxiety disorders may be particularly important to fully restore daytime functioning.
Although the current study was not designed to examine the mechanisms underlying the elevated prevalence of insomnia symptoms and resulting impairment in comorbid mood and anxiety disorders, there are several potential contributors. First, one disorder may serve as a risk factor for the other. There is evidence that insomnia is a predictor of mood and anxiety disorder onset18,29–31 and that, likewise, mood and anxiety disorders serve as risk factors for the onset of insomnia.18,21,31 Another possibility is that insomnia, mood, and anxiety disorders are all characterized by common vulnerabilities. Drawing from the Research Domain Criteria framework, these vulnerabilities could be related to negative or positive valence systems, arousal, cognitive systems, or social processes and manifest at different levels of explanation (i.e., genes, molecules, cells, circuits, behavior and self-reports).43
Similarly, psychological processes maintaining mood or anxiety disorders could be transdiagnostic and thereby mutually sustain or exacerbate insomnia symptoms, or vice versa.44 One study found that compared with individuals with primary insomnia, participants with insomnia due to a mental disorder (depression and anxiety disorders) exhibited similar levels of dysfunctional beliefs about sleep, yet exhibited poorer sleep hygiene practices as well as higher self-report pre-sleep somatic and cognitive arousal.45 Regarding biological maintaining processes, neurobiologic, neuroendocrine, and electroencephalographic studies suggest that heightened levels of arousal play a role in each of these conditions, e.g., insomnia, mood disorders, and anxiety disorders.46
Finally, the higher rates of insomnia symptoms found in the comorbid disorders group could be attributable to overlap with diagnostic criteria for major depression, generalized anxiety disorder, or posttraumatic stress disorder. In the current study, differences in diagnosis rates between the comorbid and single disorder groups could have been related to poor discriminant validity between the DSM-IV diagnoses. Specifically, rates of dysthymia, bipolar disorder type II, and most anxiety disorders were more common in the comorbid disorders group. However, previous research has found good discriminant validity between mood and anxiety disorders.47
These findings should be interpreted with consideration to both the strengths and limitations. First, the NCS-R is a large epidemiologic sample representative of the US population that is not limited by sampling biases found in large treatment-seeking samples, such as the STAR*D14 or STEP-BD.48 This is particularly important given that individuals with insomnia complaints are more likely to seek treatment for psychologic problems,49 thus biasing results in those datasets. Additionally, this study was able to address specific questions about the association of insomnia symptoms with impairment, not a more general assessment of sleep quality, which has been the focus of other studies examining the effect of sleep disturbance in psychiatric comorbidity.23,33 The use of past-month impairment measures reduced probability of recall errors, but perhaps led to underestimation of the yearly consequences of insomnia complaints (as previously discussed17). Therefore, the current study should be only be interpreted as days of impairment in the past month associated with insomnia symptoms in the past year. Given that insomnia complaints were assessed in the past year, there is also the possibility that a proportion of respondents who had endorsed insomnia symptoms in the past year were not experiencing insomnia symptoms during the 30-day period when impairment was assessed. Thus, the current study cannot be used to infer the proportion of respondents with mood and anxiety disorders that are in current need of insomnia treatment, only the proportion that experienced insomnia symptoms in the past year. Because individuals with psychiatric disorders who endorse concurrent insomnia are those who might benefit most from a separate insomnia-focused treatment, future studies should strive to use methods that allow for simultaneous assessment of insomnia and impairment. Finally, although the NCS-R provides a fairly comprehensive set of daytime functioning domains, the cross-sectional survey design does not allow one to address the mechanisms by which insomnia may contribute to functional impairment, nor the examination of the temporal sequencing of the onset of mood or anxiety disorders and insomnia. However, several studies have already addressed the latter point.21,31
In terms of treatment implications, previous research has demonstrated that in approximately 50% of cases, insomnia does not remit after a disorder-focused treatment for anxiety and depression.24,26–28 Several studies have found hypnotic medications to be beneficial adjunct treatments for insomnia comorbid with anxiety and mood disorders.52–58 Furthermore, there is some evidence that cognitive behavioral interventions for insomnia are effective in mood or anxiety disorders50 and can enhance outcomes when augmenting disorder-focused pharmacologic or psychologic interventions.51,52 However, more research is needed to further refine approaches for sequencing or interweaving interventions for cases of insomnia in patients with complex psychiatric comorbidity.
In conclusion, the current study demonstrates that insomnia complaints are frequent and impairing in the context of comorbid mood and anxiety disorders. These findings raise the important question of whether better identification and treatment of insomnia in patients with comorbid psychiatric disorders can improve long-term prognosis.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This project was supported by National Institute of Mental Health Grant No. R34MH080958 awarded to Allison G. Harvey, PhD and National Institute of Mental Health NRSA Institutional Training Grant No. T32MH089919-01A1 awarded to Adriane M. Soehner, MA.
REFERENCES
- 1.Robins LN, Locke BZ, Regier DA. An overview of psychiatric disorders in America. In: Robins LN, Regier DA, editors. Psychiatric disorders in America: the epidemiologic catchment area study. New York, NY: Free Press; 1991. pp. 328–66. [Google Scholar]
- 2.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 3.Regier DA, Rae DS, Narrow WE, Kaelber CT, Schatzberg AF. Prevalence of anxiety disorders and their comorbidity with mood and addictive disorders. Br J Psychiatry Suppl. 1998;34:24–8. [PubMed] [Google Scholar]
- 4.Zimmerman M, Chelminski I, McDermut W. Major depressive disorder and axis I diagnostic comorbidity. J Clin Psychiatry. 2002;63:187–93. doi: 10.4088/jcp.v63n0303. [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 6.Krishnan KR. Psychiatric and medical comorbidities in bipolar disorder. Psychosomatic Med. 2005;67:1–8. doi: 10.1097/01.psy.0000151489.36347.18. [DOI] [PubMed] [Google Scholar]
- 7.Lamers F, van Oppen P, Comjis HC, et al. Comorbidity patterns of anxiety and depressive disorders in a large cohort study: the Netherlands Study of Depression and Anxiety (NESDA) J Clin Psychiatry. 2011;72:341–8. doi: 10.4088/JCP.10m06176blu. [DOI] [PubMed] [Google Scholar]
- 8.Belzer K, Schneier FR. Comorbidity of anxiety and depressive disorders: issues in conceptualization, assessment, and treatment. J Psychiatr Pract. 2004;10:296–306. doi: 10.1097/00131746-200409000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Emmanuel J, Simonds D, Tyrer P. Systematic review of the outcome of anxiety and depressive disorders. Br J Psychiatry Suppl. 1998;34:35–41. [PubMed] [Google Scholar]
- 10.Goldenberg IM, White K, Yonkers K, et al. The infrequency of “pure culture” diagnoses among the anxiety disorders. J Clin Psychiatry. 1996;57:528–33. doi: 10.4088/jcp.v57n1105. [DOI] [PubMed] [Google Scholar]
- 11.McDermut W, Mattia J, Zimmerman M. Comorbidity burden and its impact on psychosocial morbidity in depressed outpatients. J Affec Disord. 2001;65:289–95. doi: 10.1016/s0165-0327(00)00220-2. [DOI] [PubMed] [Google Scholar]
- 12.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 13.Van Mill JG, Hoogendijk WJ, Vogelzangs N, van Dyck R, Penninx BW. Insomnia and sleep duration in a large cohort of patients with major depressive disorder and anxiety disorders. J Clin Psychiatry. 2010;71:239–46. doi: 10.4088/JCP.09m05218gry. [DOI] [PubMed] [Google Scholar]
- 14.Sunderjan P, Gaynes BN, Wisiewski SR, et al. Insomnia in patients with depression: A STAR*D Report. CNS Drugs. 2010;15:394–404. doi: 10.1017/s1092852900029266. [DOI] [PubMed] [Google Scholar]
- 15.Uhde TW, Cortese BM, Vedeniapin A. Anxiety and sleep problems: emerging concepts and theoretical treatment implications. Curr Psychiatry Rep. 2009;11:269–76. doi: 10.1007/s11920-009-0039-4. [DOI] [PubMed] [Google Scholar]
- 16.Harvey AG, Schmidt DA, Scarna A, Semler CN, Goodwin GM. Sleep-related functioning in euthymic patients with bipolar disorder, patients with insomnia and subjects without sleep problems. Am J Psychiatry. 2005;162:50–7. doi: 10.1176/appi.ajp.162.1.50. [DOI] [PubMed] [Google Scholar]
- 17.Roth T, Jaeger S, Jin R, et al. Sleep problems, comorbid mental disorders and role functioning in the National Comorbidity Survey-Replication (NCS-R) Biol Psychiatry. 2006;60:1364–71. doi: 10.1016/j.biopsych.2006.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ohayon MM, Roth T. Place of insomnia in the course of depressive and anxiety disorders. J Psychiatr Res. 2003;27:9–15. doi: 10.1016/s0022-3956(02)00052-3. [DOI] [PubMed] [Google Scholar]
- 19.Merikangas KR, Akiskal HS, Angst J, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2007;64:543–52. doi: 10.1001/archpsyc.64.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rhebergen D, Beekman AT, Graaf R, et al. The three-year naturalistic course of major depressive disorder, dysthymic disorder and double depression. J Affect Disord. 2009;115:450–9. doi: 10.1016/j.jad.2008.10.018. [DOI] [PubMed] [Google Scholar]
- 21.Baglioni C, Battagliese G, Fiege B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of epidemiological studies. J Affect Disord. 2011;135:10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 22.McCall WV. A psychiatric perspective on insomnia. J Clin Psychiatry. 2001;24:451–66. [PubMed] [Google Scholar]
- 23.Stein MB, Belik SL, Jacobi F, Sareen J. Impairment associated with sleep problems in the community: relationship to physical and mental health comorbidity. Psychosom Med. 2008;70:913–9. doi: 10.1097/PSY.0b013e3181871405. [DOI] [PubMed] [Google Scholar]
- 24.Carney CE, Segal ZV, Edinger JD, Krystal AD. A comparison of rates of residual insomnia symptoms following pharmacotherapy or cognitive-behavioral therapy for major depressive disorder. J Clin Psychiatry. 2007;68:254–60. doi: 10.4088/jcp.v68n0211. [DOI] [PubMed] [Google Scholar]
- 25.Hauri P, Chernik D, Hawkins D, Mendels J. Sleep of depressed patients in remission. Arch Gen Psychiatry. 1974;31:386–91. doi: 10.1001/archpsyc.1974.01760150090013. [DOI] [PubMed] [Google Scholar]
- 26.Nierenberg AA, Keefe BR, Leslie VC, et al. Residual symptoms in depressed patients who respond acutely to fluoxetine. J Clin Psychiatry. 1999;60:221–5. doi: 10.4088/jcp.v60n0403. [DOI] [PubMed] [Google Scholar]
- 27.Cervena K, Matousek M, Prasko J, Brunovsky M, Paskova B. Sleep disturbances in patients treated for panic disorder. Sleep Med. 2005;6:149–53. doi: 10.1016/j.sleep.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 28.Zayfert C, DeViva JC. Residual insomnia following cognitive behavioral therapy for PTSD. J Trauma Stress. 2004;17:69–73. doi: 10.1023/B:JOTS.0000014679.31799.e7. [DOI] [PubMed] [Google Scholar]
- 29.Perlis ML, Giles DE, Buysse DJ, Tu X, Kupfer DJ. Self-reported sleep disturbance as a prodromal symptom in recurrent depression. J Affect Disord. 1997;42:209–12. doi: 10.1016/s0165-0327(96)01411-5. [DOI] [PubMed] [Google Scholar]
- 30.Neckelmann D, Mykletun A, Dahl AA. Chronic insomnia as a risk factor for developing anxiety and depression. Sleep. 2007;30:873–80. doi: 10.1093/sleep/30.7.873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johnson EO, Roth T, Beslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res. 2006;40:700–8. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 32.Bolge SC, Joish VN, Balkrishnan R, Kannan H, Drake CL. Burden of chronic sleep maintenance insomnia characterized by nighttime awakenings among anxiety and depression sufferers: results of a national survey. Prim Care Companion. J Clin Psychiatry. 2010;12:e1–7. doi: 10.4088/PCC.09m00824gry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ramsawh HJ, Stein MB, Belik SL, Jacobi F, Sareen J. Relationship of anxiety disorders, sleep quality, and functional impairment in a community sample. J Psychiatr Res. 2009;43:926–33. doi: 10.1016/j.jpsychires.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 34.Gureje O, Makanjuola VA, Kola L. Insomnia and role impairment in the community: results from the Nigerian survey of mental health and wellbeing. Soc Psychiatry Psychiatr Epidemiol. 2007;42:495–501. doi: 10.1007/s00127-007-0183-2. [DOI] [PubMed] [Google Scholar]
- 35.Kessler RC, Merikangas KR. The National Comorbidity Survey Replication (NCS-R): background and aims. Int J Methods Psychiatr Res. 2004;13:60–8. doi: 10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 37.Kessler RC, Ustün TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schoenborn CA, Adams PF, Schiller JS. Summary health statistics for the U.S. population: National Health Interview Survey, 2000. Vital and Health Statistics. 2003;10:1–83. [PubMed] [Google Scholar]
- 39.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th edition, text revision) Washington, D.C.: American Psychiatric Association; 2000. [Google Scholar]
- 40.American Academy of Sleep Medicine. International classification of sleep disorders, 2nd edition: diagnostic and coding manual. Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 41.Chwastiak LA, Von Korff M. Disability in depression and back pain: evaluation of the World Health Organization Disability Assessment Schedule (WHO DAS II) in a primary care setting. J Clin Epidemiol. 2003;56:507–14. doi: 10.1016/s0895-4356(03)00051-9. [DOI] [PubMed] [Google Scholar]
- 42.Lee M, Choh AC, Demerath EW, et al. Sleep disturbance in relation to health-related quality of life in adults: the Fels Longitudinal Study. J Nutr Health Aging. 2009;13:576–83. doi: 10.1007/s12603-009-0110-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Insel T, Cuthbert B, Garvey M, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167:748–51. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- 44.Harvey AG, Watkins E, Mandsell W, Shafran R. Cognitive behavioural processes across psychological disorders: a transdiagnostic approach to research and treatment. Oxford, UK: Oxford University Press; 2004. [Google Scholar]
- 45.Kohn L, Espie CA. Sensitivity and specificity of measures of the insomnia experience: a comparative study of psychophysiologic insomnia, insomnia associated with mental disorder and good sleepers. Sleep. 2005;28:104–12. doi: 10.1093/sleep/28.1.104. [DOI] [PubMed] [Google Scholar]
- 46.Benca RM, Peterson MJ. Insomnia and depression. Sleep Med. 2008;9:S3–9. doi: 10.1016/S1389-9457(08)70010-8. [DOI] [PubMed] [Google Scholar]
- 47.Brown TA, Barlow DH, Chorpita BF. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect and autonomic arousal. J Abnorm Psychol. 1998;107:179–92. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- 48.Sachs GS, Thase ME, Otto MW, Bauer M, Miklowitz D, Wisniewski SR, et al. Rationale, design, and methods of the systematic treatment enhancement program for bipolar disorder (STEP-BD) Biological Psychiatry. 2003;53:1028–42. doi: 10.1016/s0006-3223(03)00165-3. [DOI] [PubMed] [Google Scholar]
- 49.Angst J, Gamma A, Clarke D, Ajdacic-Gross V, Rössler W, Regier D. Subjective distress predicts treatment seeking for depression, bipolar, anxiety, panic, neurasthenia and insomnia severity spectra. Acta Psychiatr Scand. 2010;122:488–98. doi: 10.1111/j.1600-0447.2010.01580.x. [DOI] [PubMed] [Google Scholar]
- 50.Edinger JD, Olsen MK, Stechuchak KM, et al. Cognitive behavioral therapy for patients with primary insomnia or insomnia associated predominantly with mixed psychiatric disorders: a randomized clinical trial. Sleep. 2009;32:499–510. doi: 10.1093/sleep/32.4.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Manber R, Edinger JD, Gress JL, San Pedro-Salcedo MG, Kuo TF, Kalista T. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. 2008;31:489–95. doi: 10.1093/sleep/31.4.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.DeViva JC, Zayfert C, Pigeon WR, Mellman TA. Treatment of residual insomnia after CBT for PTSD: case studies. J Trauma Stress. 2005;18:155–9. doi: 10.1002/jts.20015. [DOI] [PubMed] [Google Scholar]
- 53.Fava M, McCall WV, Krystal A, et al. Eszopiclone co-administered with fluoxetine in patients with insomnia coexisting with major depressive disorder. Biol Psychiatry. 2006;59:1052–60. doi: 10.1016/j.biopsych.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 54.Fava M, Asnis GM, Shrivstava, et al. Improved insomnia symptoms and sleep-related next day functioning in patients with comorbid major depressive disorder and insomnia following concomitant zolpidem extended-release 12.5 and escitalopram treatment: A randomized controlled trial. J Clin Psychiatry. 2011;72:914–28. doi: 10.4088/JCP.09m05571gry. [DOI] [PubMed] [Google Scholar]
- 55.Fava M, Schaefer K, Huang H, et al. A post hoc analysis of the effect of nightly administration of eszopiclone and a selective serotonin reuptake inhibitor in patients with insomnia and anxious depression. J Clin Psychiatry. 2011;72:473–9. doi: 10.4088/JCP.09m05131gry. [DOI] [PubMed] [Google Scholar]
- 56.Pollack M, Kinrys G, Krystal A, et al. Eszopiclone coadministered with escitalopram in patients with insomnia and comorbid generalized anxiety disorder. Arch Gen Psychiatry. 2008;65:551–62. doi: 10.1001/archpsyc.65.5.551. [DOI] [PubMed] [Google Scholar]
- 57.Pollack M, Hoge E, Worthington JJ, et al. Eszopiclone for the treatment of posttraumatic stress disorder and associated insomnia: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2011;72:892–7. doi: 10.4088/JCP.09m05607gry. [DOI] [PubMed] [Google Scholar]
- 58.Schaffer CB, Schaffer LC, Miller AR, Hang E, Nordahl TW. Efficacy and safety of nonbenzodiazepine hypnotics for chronic insomnia in patients with bipolar disorder. J Affect Disord. 2011;128:305–8. doi: 10.1016/j.jad.2010.07.018. [DOI] [PubMed] [Google Scholar]


