Abstract
Purpose
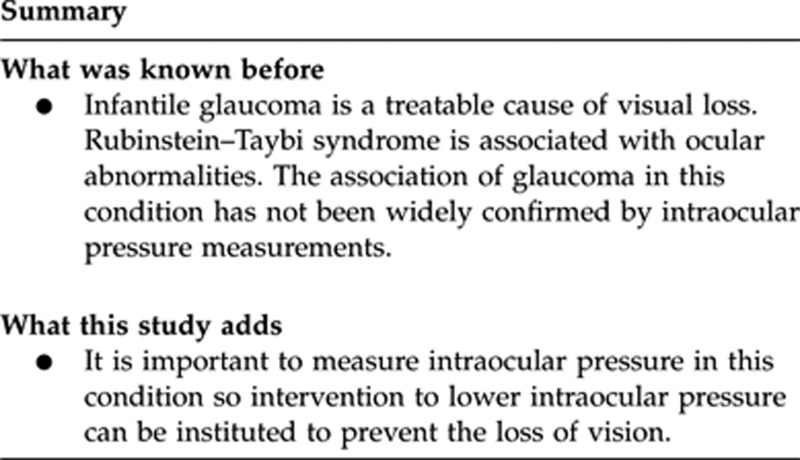
Long-term follow-up of patients with Rubinstein–Taybi-associated infantile glaucoma.
Methods
Case series.
Results
Three cases of infantile glaucoma in association with Rubinstein–Taybi syndrome are presented.
Discussion
This report highlights the importance of measuring intraocular pressure in this condition, as glaucoma is one of the major preventable causes of blindness in childhood.
Keywords: glaucoma, infantile, Rubinstein–Taybi syndrome
Introduction
Multiple ocular abnormalities have been described in Rubinstein Taybi syndrome. This case series describes long-term follow-up of patients with this condition associated with infantile glaucoma.
Case Reports
Case 1
A 5-month-old boy with intraocular pressures in the mid-thirties with dysplastic irides, ectropion uvea, and subluxated lenses. Multiple procedures were attempted including bilateral trabeculotomies and trabeculectomies. By the age of 14, vision was perception of light caused by a combination of glaucomatous optic neuropathy, previous retinal detachment, and corneal scarring.
Case 2
A 4-month-old boy born at 36 weeks. Dysmorphic skeletal features were present consistent with the diagnosis of Rubinstein–Taybi syndrome. Nystagmus, enophthalmos, right exotropia, unilateral axial myopia, increased horizontal corneal diameters, and corneal oedema were present. Intraocular pressures were 45 mm Hg on the right and 28 mm Hg on the left with advanced optic disc cupping. Bilateral goniotomies were performed and this controlled intraocular pressure in combination with topical treatment. Vision was 6/96 on the right and 6/19 on the left at the age of 3 years.
Case 3
A 5-month-old boy with micrognathia and broad thumbs. The left corneal diameter was increased with corneal oedema. Previously, goniotomy had been attempted. Intraocular pressure was not controlled with topical therapy, and Baerveldt tube surgery was performed. Eighteen months after surgery, intraocular pressure was controlled and vision was 6/76 on the right and 6/96 on the left.
Discussion
Rubinstein and Taybi1 were the first to describe this condition in a report of seven patients with physical characteristics such as beaked nose, broad thumbs, and angulation deformity of the big toes. Associated ocular findings include glaucoma, nystagmus, strabismus, enophthalmos, iris atropy, high myopia, and optic atrophy. The condition has been found to be caused by mutations in either the CREBBP2 or the EP3003, 4 genes. Patients with these mutations do not differ clinically from patients without a detectable mutation.5 In about 35–45% of patients with the clinical phenotype no mutation is detectable. None of the patients in this case series were genetically characterised. In their original paper,1 Rubinstein and Taybi failed to report on intraocular pressure despite describing the presence of optic atrophy in two (or 28%) of seven patients. It was unclear whether optic atrophy was due to undetected congenital glaucoma or central nervous system involvement. Ocular changes frequently associated with congenital glaucoma include corneal oedema, enlarged cornea, optic disc cupping, and increased intraocular pressure. The first reports of glaucoma in relation to Rubinstein–Taybi syndrome were described in the literature in the 1970s.6, 7 A case of unilateral glaucoma associated with the condition was described in which a trabeculotomy was performed with normalisation of intraocular pressure.8 However, visual outcome was not reported. The association with glaucoma and other findings that may be confused with glaucoma was reviewed in 614 patients with Rubinstein–Taybi syndrome.9 In eight individuals with Rubinstein–Taybi syndrome, glaucoma was described without mention of other eye abnormalities. Other ocular findings associated with or mistaken for glaucoma may also be seen in the absence of elevated intraocular pressure. Corneal lesions described in Rubinstein–Taybi syndrome may be confused with the corneal clouding seen in glaucoma. However, the corneal lesions seen in this condition are more localised and clearly demarcated in contrast to the diffuse glaucomatous-induced corneal oedema. Cases of Rubinstein–Taybi syndrome with optic nerve coloboma, excavation of the papilla or large cup–disc ratios were reported without the presence of glaucoma.9 These changes may be mistaken for glaucoma in the absence of a recorded measurement of intraocular pressure. The incidence of glaucoma was probably overestimated in this study as the measurement of elevated intraocular pressure to verify the diagnosis of glaucoma was not recorded.
A case report of bilateral congenital glaucoma associated with the condition has been described.10An 8-month-old girl with the typical features was described with clear corneas and increased horizontal and vertical corneal diameters. In this case intraocular pressure measurement was elevated in both eyes. The iridocorneal angle was abnormal and there was optic disc pallor with a cup–disc ratio of 0.6. Ten months after trabeculotomy, intraocular pressure was within normal limits without topical or systemic treatment and the appearance of the optic nerve head had improved. A series of ocular features of 24 patients with Rubinstein–Taybi syndrome was reported.11 Only one of these patients had congenital glaucoma with bilateral buphthalmos. However, intraocular pressure was only recorded in four patients and of these none had elevated intraocular pressure. The appearance of the optic discs was reported as excavated or pale in 10 of the 24 patients. This report highlights the importance of measuring intraocular pressure in infantile glaucoma as it is a preventable cause of blindness.
The authors declare no conflict of interest.
References
- Rubinstein JH, Taybi H. Broad thumbs and toes and facial abnormalities. Am J Disease Child. 1963;105:588–608. doi: 10.1001/archpedi.1963.02080040590010. [DOI] [PubMed] [Google Scholar]
- Petriji F, Giles RH, Dauwerse HG, Saris JJ, Hennekam RC, Masuno M, et al. Rubinstein-Taybi syndrome caused by mutations in the transcriptional co-activator CBP. Nature. 1995;376:348–351. doi: 10.1038/376348a0. [DOI] [PubMed] [Google Scholar]
- Roelfsema JH, White SF, Ariyurek Y, Bartholdi D, Niedrist D, Papadia F, et al. Genetic heterogeneity in Rubinstein-Taybi syndrome: mutations in both the CBP and EP300 genes cause disease. Am J Hum Genet. 2005;76:572–580. doi: 10.1086/429130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartholdhi D, Roelfsema JH, Papadia F, Breuning MH, Niedrist D, Hennekam RC, et al. Genetic heterogeneity in Rubinstein-Taybi syndrome: delineation of the phenotype of the first patients carrying mutations in EP300. J Med Genet. 2007;44:327–333. doi: 10.1136/jmg.2006.046698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hennekam RCM. Rubinstein Taybi syndrome. Eur J Hum Genet. 2006;14:981–985. doi: 10.1038/sj.ejhg.5201594. [DOI] [PubMed] [Google Scholar]
- Shaffer RN, Weiss DT. Congenital and Paediatric Glaucomas. The CV Mosby Co: Saint Louis; 1970. pp. 57–58. [Google Scholar]
- Weiss DI.Glaucoma and systemic diseaseIn: Duane T (ed.).Clinical Ophthalmology Vol 5Chap 4.Harper and Row Publishers: Hagerstown; 19783–4. [Google Scholar]
- Bardelli AM, Lasorella G, Barberi L, Vanni M. Ocular manifestations in Kniest syndrome, Smith-Lemli-Opitz syndrome, Hallermann-Streiff-Francois syndrome, Rubinstein-Taybi syndrome and median cleft face syndrome. Ophthal Paediatr Genetics. 1985;6:103–107. [PubMed] [Google Scholar]
- Brei TJ, Burke MJ, Rubinstein JH. Glaucoma and findings simulating glaucoma in the Rubinstein-Taybi syndrome. J Paediatr Ophthalmol Strabismus. 1995;32:248–252. doi: 10.3928/0191-3913-19950701-12. [DOI] [PubMed] [Google Scholar]
- Quaranta L, Quaranta CA. Congenital glaucoma associated with Rubinstein Taybi syndrome. Acta Ophthalmologica Scandinavica. 1998;76:112–113. doi: 10.1034/j.1600-0420.1998.760122.x. [DOI] [PubMed] [Google Scholar]
- Van Genderen MM, Kinds GF, Riemslag FCC, Hennekam RCM. Ocular features in Rubinstein-Taybi syndrome: investigation of 24 patients and review of the literature. Br J Ophthalmol. 2000;84:1177–1184. doi: 10.1136/bjo.84.10.1177. [DOI] [PMC free article] [PubMed] [Google Scholar]


