Abstract
Purpose
To demonstrate the results of the ray tracing-type aberrometer in measuring spherical aberration (SA) in pseudophakic eyes with monofocal intraocular lens (IOL), aspheric monofocal IOL, or aspheric diffractive multifocal IOL.
Methods
Total, corneal, and internal SA were measured using iTrace at a 6-mm pupil size in 27 eyes of 27 patients implanted with a monofocal spherical IOL (group 1: Natural, SN60AT), 30 eyes of 30 patients implanted with a monofocal aspheric IOL (group 2: IQ, SN60WF), and 30 eyes of 30 patients implanted with a multifocal aspheric IOL (group 3: ReSTOR, SN6AD1) at 3 months after cataract surgery. We compared the internal SAs of these IOLs in pupil sizes of 3, 4, 5, and 6 mm.
Results
There were no demographic statistically significant differences among the groups. The internal SA of group 1 had a positive value. The internal SA of group 2 was −0.175±0.135 μm in 5-mm pupils and −0.227±0.253 μm in 6-mm pupils. The internal SA of group 3 was −0.072±0.128 μm in 5-mm pupils and −0.173±0.231 μm in 6-mm pupils.
Conclusion
Measuring internal SA with iTrace yields relatively accurate results in all types of IOLs with adequate pupil sizes.
Keywords: spherical aberration, aberrometer, aspheric IOL, multifocal IOL, ray tracing
Introduction
Cataract surgery involves the extraction of an opaque lens, which leads to improved visual performance. Developing interest about the impact of cataract surgery on visual acuity, function, and quality of life has led to the acceleration of the development and refinement of the intraocular lens (IOL).1
The modification of IOL asphericity has been a key focus of IOL development, as adjusting the asphericity of the IOL to corneal spherical aberration (SA) can result in a decrease of total aberration.2, 3, 4, 5, 6 Aberration is the phenomenon by which an image becomes distorted when the lens cannot completely concentrate incoming rays of light into a single focus. Without compensation of positive corneal SA, the rays of light will fail to focus onto a single spot of the retina and will result in a distortion of the image and compromise of contrast sensitivity. Although previously designed IOLs did not pay much attention to correcting higher order aberration, aspheric IOLs were designed with an aspheric surface that induced negative SA that may compensate for corneal SA to improve visual quality.
The development of the multifocal IOL has been generating increasing interest, as they can provide reasonable vision at both near and distance. The Acrysof ReSTOR (Alcon, Inc., Fort Worth, TX, USA), a type of diffractive multifocal IOL, has central apodized diffractive zones and many studies have revealed its usefulness for improving visual performance.7, 8, 9 To maximize visual outcome after multifocal IOL implantation, minimizing refractive error is critical and, in some cases, additional surgical procedure are required to reduce remaining refractive error.2, 3, 10, 11, 12 To optimize surgical outcomes, wavefront-guided refractive surgery has also been considered. To maximize visual acuity after refractive error surgery, surgeons attempt to not only correct remaining refractive error but also to minimize ocular aberration.
A previous report showed that implantation of monofocal IOLs did not interfere with accurate measurements of ocular aberration using a Hartmann–Shack aberrometer.13 However, when the input beam passes through a diffractive multifocal IOL, it is divided into two focus points and previous studies have shown that using the Hartmann–Shack technique to measure ocular aberration after implantation of diffractive multifocal IOLs had unreliable accuracy.14, 15 The wavefront of a diffractive multifocal IOL is very complex due to the large number of Fresnel edges that are part of the design. However, as the central 2 mm is usually free of these Fresnel edges, the input beam should arrive at the retina in the same way as would occur in a monofocal IOL. The unreliability of the measurements occurs only when the light arrives at the Hartmann–Shack sensor, which has a resolution unable to resolve the very high orders of aberration present in the wavefront of a multifocal IOL.
The iTrace (Tracey Technology, Houston, TX, USA), one of the ray tracing-type aberrometers, measures aberrations using a position sensitive detector to measure the displacement of a laser beam reflected from the retina. In the Tracey aberrometer, the problem is reversed: the incidence beams scatter when they pass through the multifocal IOL, but the detection of the retinal image is affected less. We formed a hypothesis that the ray tracing-type aberrometers may provide a more reliable SA in pseudophakic eyes than Hartmann–Shack type.
In this study, we compared intraocular SA measured using the iTrace system, a ray tracing-type aberrometer, with various pupil size to theoretical SA values of monofocal spherical, monofocal aspheric, and multifocal aspheric IOLs as provided by their manufacturers.
Patients and methods
Patients underwent cataract surgery between January 2007 and August 2010. All procedures were performed by one surgeon (TK). Eligible patients for this study included patients between the ages of 40 and 75 who underwent operation for senile cataract and IOL implantation. Exclusion criteria included having any other ocular disease that could decrease visual acuity and quality of vision (eg, uveitis, glaucoma, any corneal opacity, and any macular disease), any previous ocular surgery, abnormal fundus finding, posterior capsule rupture during surgery, IOL decentration >0.5 mm,16 corneal astigmatism >2.0D, and best-corrected visual acuity (BCVA) under 20/25 postoperatively. This study included 27 eyes of 27 patients implanted with a monofocal spherical IOL (SN60AT; Alcon, Inc.; group 1), 30 eyes of 30 patients implanted with a monofocal aspheric IOL (SN60WF; Alcon, Inc.; group 2), and 30 eyes of 30 patients implanted with a multifocal aspheric IOL (Acrysof ReSTOR, SN6AD1; Alcon, Inc.; group 3). When a patient had operations performed on both eyes, one eye was randomly selected to avoid correlation effect in statistical analysis. This study was approved by the Institutional Review Board of Yonsei University Medical Center, Seoul, Korea. All study procedures were performed in accordance with the Declaration of Helsinki.
Three months after the cataract procedure, all patients were checked for uncorrected visual acuity, BCVA, intraocular pressure, and refractive error. Aberrations of all patients were measured by iTrace (software version 4.1.0) at pupil sizes >6 mm under pharmacological dilation with Mydrin-P (Santen Pharmaceutical, Osaka, Japan). The iTrace displays ocular aberrations, including entire, corneal, and intraocular measures, in root mean square values automatically. Among various aberration values, we analysed intraocular SAs of each eye at pupil sizes of 3, 4, 5, and 6 mm. The wavefronts measured in the 6-mm pupils were scaled down to pupil sizes of 3, 4, and 5 mm using the Tracey software. The iTrace automatically rejects abnormal value points and in this study, we only used data showing <10 rejected points as to optimize the reliability of the results.
Statistical analyses were performed using SPSS for Windows (Version 13.0; LEAD Technology, Inc., Chicago, IL, USA). One-way analysis of variance was used to compare differences between baseline characteristics. In group 1, the connection between internal SA and the IOL diopter was analysed by correlation analysis. One-sample t-tests were used to compare actual aberrations and expected values in groups 2 and 3. Probability values <0.05 were considered statistically significant.
Results
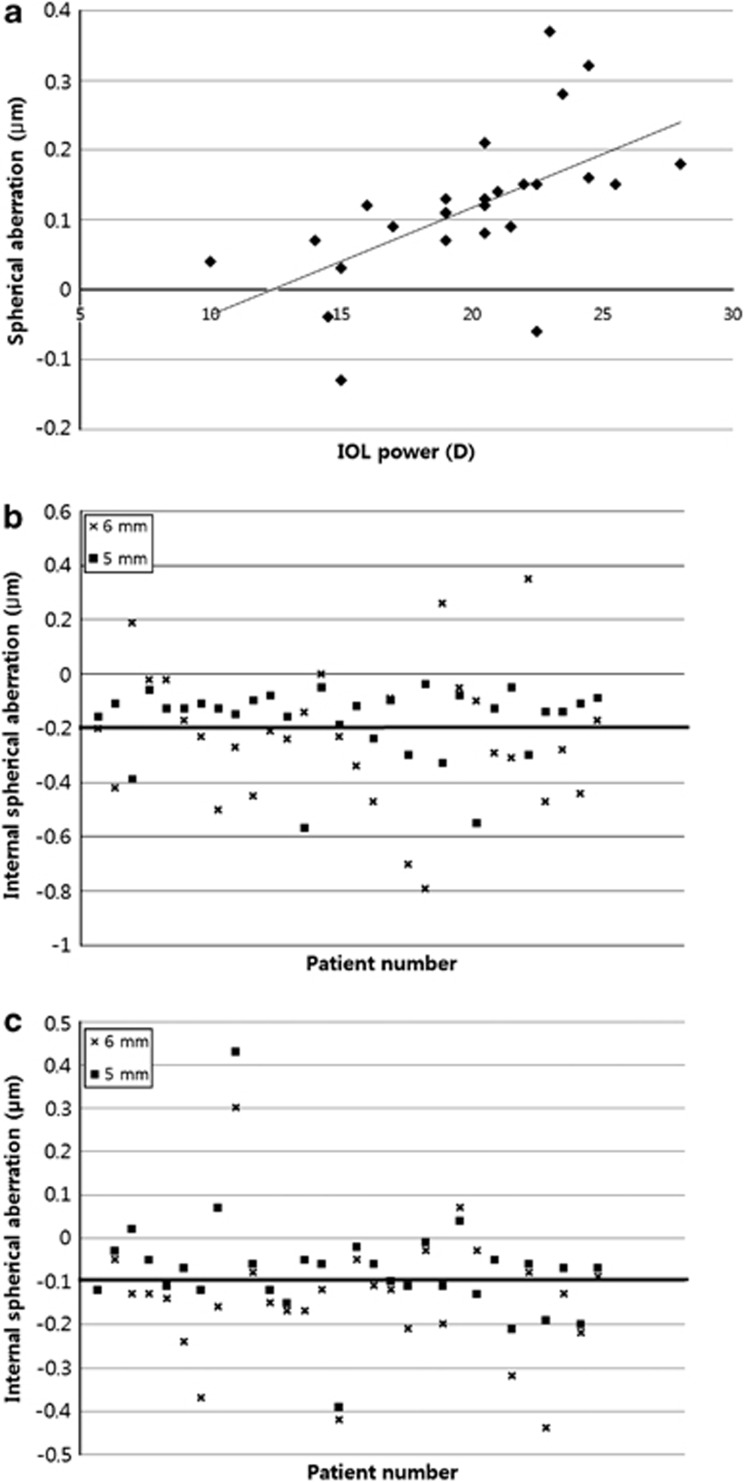
There was no statistically significant difference in baseline characteristics between the three groups (Table 1). In patients with a 6-mm pupil size, the average internal SA in patients with a monofocal spherical IOL (group 1) was 0.121±0.182 μm. As pupil size decreased, the internal SA of the IOL for group 1 was diminished (Table 2). Because there was no reference value for SA of AcrySof Natural IOL, the one-sample t-test could not be applied. However, many studies have shown that AcrySof Natural IOL has a slightly positive aberration, with a SA that increases in a diopter-dependent manner.17, 18, 19, 20 In this study, the internal SA of group 1 had a positive value. Correlation analyses showed diopter-dependent increases in SA at pupil sizes of 5 and 4 mm (5 mm: P=0.001 and 4 mm: P=0.009; Table 2 and Figure 1a).
Table 1. Baseline characteristics of study participants.
| Natural (SN60AT) | Acrysof IQ (SN60WF) | Acrysof ReSTOR IOL (SN6AD1) | P-value | |
|---|---|---|---|---|
| Age (mean±SD) | 59.48±10.99 | 63.54±7.51 | 61.30±5.72 | 0.227 |
| Sex (M:F) | 10:17 | 11:19 | 15:15 | 0.496 |
| Laterality (right:left) | 12:15 | 15:15 | 15:15 | 0.891 |
| Axial length (mm, mean±SD) | 23.91±1.72 | 23.65±1.16 | 23.91±1.72 | 0.205 |
| Preoperative spherical equivalent (D, mean±SD) | −0.15±2.29 | −0.82±3.60 | 0.00±2.79 | 0.590 |
Abbreviations: F, female; IOL, intraocular lens; M, male; SD, standard deviation.
Table 2. Internal spherical aberration of groups 1, 2, and 3 as measured by iTrace according to pupil size (group 1: correlation analysis with implanted IOL diopter; group 2 and 3: one-sample t-test with theoretical SA).
|
Group 1 |
Group 2 |
Group 3 |
||||
|---|---|---|---|---|---|---|
| Measured value (μm, mean±SD) | P-value | Measured value (μm, mean±SD) | P-value | Measured value (μm, mean±SD) | P-value | |
| 6 mm | 0.121±0.182 | 0.629 | −0.227±0.253 | 0.566 | −0.173±0.231 | 0.094 |
| 5 mm | 0.116±0.105 | 0.001 | −0.175±0.135 | 0.316 | −0.072±0.128 | 0.242 |
| 4 mm | 0.026±0.076 | 0.009 | −0.068±0.047 | <0.001 | −0.032±0.086 | <0.001 |
| 3 mm | −0.006±0.039 | 0.088 | −0.041±0.057 | <0.001 | −0.017±0.029 | <0.001 |
Abbreviations: IOL, intraocular lens; SA, spherical aberration; SD, standard deviation.
Figure 1.
(a) Internal SA of group 1 at 5-mm pupil size, according to IOL power. (b) Internal SA of group 2 at 6- and 5-mm pupil size (highlighted line: −0.2 μm, designed value of IQ). (c) Internal SA of group 3 at 6- and 5-mm pupil size (highlighted line: −0.1 μm, designed value of ReSTOR).
The internal SA of patients with a monofocal aspheric IOL (group 2) was −0.227±0.253 μm in 6-mm pupils, −0.175±0.135 μm in 5-mm pupils, −0.068±0.047 μm in 4-mm pupils, and −0.041±0.057 μm in 3-mm pupils. The theoretical SA value provided by the manufacturer of the AcrySof IQ IOL was −0.2 μm. One sample t-test showed that the measured SA correlated with the expected SA in 6- and 5-mm pupils, but this correlation did not hold for smaller pupils (6 mm: P=0.566, 5 mm: P=0.316, and 4 and 3 mm: P<0.001; Table 2 and Figure 1b).
The internal SA of patients with a multifocal aspheric IOL (group 3) was −0.173±0.231 μm in 6-mm pupils, −0.072±0.128 μm in 5-mm pupils, −0.032±0.086 μm in 4-mm pupils, and −0.017±0.029 μm in 3-mm pupils. The theoretical SA value provided by the manufacturer of the ReSTOR IOL was −0.1 μm. Similar to group 2, 6- and 5-mm pupils showed measured SAs that correlated well with the expected SAs, but this correlation did not hold for smaller pupils in the one-sample t-test (6 mm: P=0.094, 5 mm: P=0.242, and 4 and 3 mm: P<0.001; Table 2 and Figure 1c).
Discussion
The internal SA of patients with the AcrySof Natural monofocal spherical IOL was positive in value and showed a diopter-dependent increase in pupil sizes of 4 and 5 mm. In patients with a monofocal or multifocal aspheric IOL, the internal SA measured by iTrace, a ray tracing aberrometer, was similar to the manufacturer's designated SA in conditions of 5- and 6-mm pupil size.
AcrySof IQ is a monofocal, aspheric, single-piece IOL, which is based on the AcrySof Natural. The difference between the two IOLs is that the posterior surface of the AcrySof IQ has the aspheric design to reduce ocular SA. The IQ has a negative SA of −0.20 μm in a 6-mm pupil. The ReSTOR IOL adopts a similar platform to IQ and has apodized diffractive multifocal character with a negative SA of −0.10 μm in a 6-mm pupil.
The ReSTOR multifocal IOL produces bifocal visual effects by applying different diffractive concentric circles. Nominally, this IOL splits the incoming light, so that disparate wavefronts emerge. In practice, aberration and contrast sensitivity of multifocal lenses are worse than those of monofocal IOLs.4, 21 Because of the splitting of entering light, glare and night halos are frequent in multifocal IOLs.22 We can also deduce that splitting light makes aberrometer analysis more challenging, because such analysis computes reflected rays shot into the eyes by separating beams.
Studies using either the Hartmann–Shack-type aberrometer or automated retinoscopy-type aberrometer to measure SA of multifocal IOL have concluded that caution was needed to translate the value.14, 15 Campbell et al23 used the Hartmann–Shack method to estimate the wavefront measurements in artificial eyes implanted with multifocal IOLs (AMO ZM900, AMO Rezoom NXG1, and AMO 811E (Abbott Medical Optics Inc, Abbott Park, IL, USA)). They discovered a spot-doubling phenomenon, in which two images came from measurements taken with a different centration of the test eye. We tried to measure ocular aberration after implantation of multifocal IOLs with the Hartmann–Shack-type aberrometer. However, we could not analyse aberration due to poor image quality. We believed the spot-doubling phenomenon made the image quality poor, as other studies had previously shown.
In the ray tracing method, the beams of light shooting into the eye are sequentially launched. The input beam is sensed in each position according to the ocular aberration. The software then reproduces the two-dimensional data into three-dimensional results. This aberrometer was already used in several studies.24, 25, 26, 27 Furthermore, some studies reported the comparability and repeatability of ray tracing aberrometers with good results.28, 29, 30, 31, 32 However, no previous study measured the aberration of multifocal IOLs using a ray tracing-type aberrometer. The ray tracing method has relatively less interference because of its sequential shooting. Furthermore, the abnormal value points are rejected automatically in the iTrace aberrometer and are thus not included in calculating aberration (we only used data showing <10 rejected points as to optimize the reliability of the results in this study). Based on the mechanism of the ray tracing-type aberrometer, we expected the iTrace to measure SA aberration more accurately in multifocal IOLs.
Pupil size is also one of the important factors that can influence SA measurement. In patients with smaller pupils, the internal SAs of patients with a monofocal or multifocal aspheric IOL were significantly different than the manufacturer-designated SAs. According to previous studies,33, 34 the difference of total SA between spherical and aspheric IOLs reduces as the pupil size gets smaller.
We measured aberrations with the iTrace at a pupil size of 6 mm, so that 256 (16 × 16) beams entered the 6-mm pupil. In a 5-, 4-, and 3-mm pupil, 182 (about (16 × 5/6)2), 122 (about (16 × 4/6)2), and 74 (about (16 × 3/6)2) beams were used for calculating SA, respectively. We believed that because only small numbers of beams can enter smaller-sized pupils, SA values could not be accurate.
This is the first study of our knowledge to investigate the efficacy of the iTrace, a ray tracing-type aberrometer, for the analysis of internal SA in multifocal IOL implanted eyes. Although the theoretical SA values provided by the manufacturers may not perfectly represent the internal SA values, we believe that these values can be used as the standard values to represent internal SA.
In conclusion, measuring internal SA with iTrace yields relatively accurate results in all types of IOLs with adequate pupil sizes. Accurate tools and sufficiently large pupils are important for reliable measurements of SA.
Acknowledgments
We would like to thank Bradford Sgrignoli DO from Yonsei University Corneal Dystrophy Research Institute for his help with the correction of English in the study. This work was partially supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MEST No. 2009-0066392) and the Converging Research Center Program funded by the Ministry of Education, Science and Technology (2011K000680).
The authors declare no conflict of interest.
Footnotes
This study was presented in the annual meeting of American Academy of Ophthalmology, 21–26 Oct 2011, Orlando, FL, USA.
References
- Rocha KM, Chalita MR, Souza CE, Soriano ES, Freitas L, Muccioli C, et al. Postoperative wavefront analysis and contrast sensitivity of a multifocal apodized diffractive IOL (ReSTOR) and three monofocal IOLs. J Refract Surg. 2005;21 (6:S808–S812. doi: 10.3928/1081-597X-20051101-32. [DOI] [PubMed] [Google Scholar]
- Alfonso JF, Fernndez-Vega L, Monts-Mic R, Valcrcel B. Femtosecond laser for residual refractive error correction after refractive lens exchange with multifocal intraocular lens implantation. Am J Ophthalmol. 2008;146 (2:244–250. doi: 10.1016/j.ajo.2008.03.022. [DOI] [PubMed] [Google Scholar]
- Jendritza B, Knorz MC, Morton S. Wavefront-guided excimer laser vision correction after multifocal IOL implantation. J Refract Surg. 2008;24 (3:274–279. doi: 10.3928/1081597X-20080301-09. [DOI] [PubMed] [Google Scholar]
- Zeng M, Liu Y, Liu X, Yuan Z, Luo L, Xia Y, et al. Aberration and contrast sensitivity comparison of aspherical and monofocal and multifocal intraocular lens eyes. Clin Experiment Ophthalmol. 2007;35 (4:355–360. doi: 10.1111/j.1442-9071.2007.01452.x. [DOI] [PubMed] [Google Scholar]
- Montés-Micó R, Ferrer-Blasco T, Cervio A. Analysis of the possible benefits of aspheric intraocular lenses: review of the literature. J Cataract Refract Surg. 2009;35 (1:172–181. doi: 10.1016/j.jcrs.2008.09.017. [DOI] [PubMed] [Google Scholar]
- Luo M, Ji J, Zhao C, Fan X, Pan Y, Lu J. Comparison of contrast sensitivity and wavefront analysis after implantation of AcrySof IQ aspherical intraocular lens. Zhonghua Yan Ke Za Zhi. 2009;45 (3:239–242. [PubMed] [Google Scholar]
- Souza CE, Muccioli C, Soriano ES, Chalita MR, Oliveira F, Freitas L, et al. Visual performance of AcrySof ReSTOR apodized diffractive IOL: a prospective comparative trial. Am J Ophthalmol. 2006;141 (5:827–832. doi: 10.1016/j.ajo.2005.12.031. [DOI] [PubMed] [Google Scholar]
- Vingolo EM, Grenga P, Iacobelli L, Grenga R. Visual acuity and contrast sensitivity: AcrySof ReSTOR apodized diffractive versus AcrySof SA60AT monofocal intraocular lenses. J Cataract Refract Surg. 2007;33 (7:1244–1247. doi: 10.1016/j.jcrs.2007.03.052. [DOI] [PubMed] [Google Scholar]
- Chiam PJ, Chan JH, Aggarwal RK, Kasaby S. ReSTOR intraocular lens implantation in cataract surgery: quality of vision. J Cataract Refract Surg. 2006;32 (9:1459–1463. doi: 10.1016/j.jcrs.2006.04.015. [DOI] [PubMed] [Google Scholar]
- Kuo IC, Reviglio VE. Wavefront-guided refractive surgery after multifocal lens implantation. Curr Opin Ophthalmol. 2009;20 (4:255–259. doi: 10.1097/ICU.0b013e32832c181a. [DOI] [PubMed] [Google Scholar]
- Kuo IC, O'Brien TP, Broman AT, Ghajarnia M, Jabbur NS. Excimer laser surgery for correction of ametropia after cataract surgery. J Cataract Refract Surg. 2005;31 (11:2104–2110. doi: 10.1016/j.jcrs.2005.08.023. [DOI] [PubMed] [Google Scholar]
- Jin GJ, Merkley KH, Crandall AS, Jones YJ. Laser in situ keratomileusis versus lens-based surgery for correcting residual refractive error after cataract surgery. J Cataract Refract Surg. 2008;34 (4:562–569. doi: 10.1016/j.jcrs.2007.11.040. [DOI] [PubMed] [Google Scholar]
- Daz-Doutn F, Benito A, Pujol J, Arjona M, Gell JL, Artal P. Comparison of the retinal image quality with a Hartmann–Shack wavefront sensor and a double-pass instrument. Invest Ophthalmol Vis Sci. 2006;47 (4:1710–1716. doi: 10.1167/iovs.05-1049. [DOI] [PubMed] [Google Scholar]
- Gatinel D. Limited accuracy of Hartmann–Shack wavefront sensing in eyes with diffractive multifocal IOLs. J Cataract Refract Surg. 2008;34 (4:528–529. doi: 10.1016/j.jcrs.2007.11.038. [DOI] [PubMed] [Google Scholar]
- Charman WN, Monts-Mic R, Radhakrishnan H. Problems in the measurement of wavefront aberration for eyes implanted with diffractive bifocal and multifocal intraocular lenses. J Refract Surg. 2008;24 (3:280–286. doi: 10.3928/1081597X-20080301-10. [DOI] [PubMed] [Google Scholar]
- Baumeister M, Bhren J, Kohnen T. Tilt and decentration of spherical and aspheric intraocular lenses: effect on higher-order aberrations. J Cataract Refract Surg. 2009;35 (6:1006–1012. doi: 10.1016/j.jcrs.2009.01.023. [DOI] [PubMed] [Google Scholar]
- Caporossi A, Casprini F, Martone G, Balestrazzi A, Tosi GM, Ciompi L. Contrast sensitivity evaluation of aspheric and spherical intraocular lenses 2 years after implantation. J Refract Surg. 2009;25 (7:578–590. doi: 10.3928/1081597X-20090610-03. [DOI] [PubMed] [Google Scholar]
- Nanavaty MA, Spalton DJ, Boyce J, Saha S, Marshall J. Wavefront aberrations, depth of focus, and contrast sensitivity with aspheric and spherical intraocular lenses: fellow-eye study. J Cataract Refract Surg. 2009;35 (4:663–671. doi: 10.1016/j.jcrs.2008.12.011. [DOI] [PubMed] [Google Scholar]
- Cadarso L, Iglesias A, Ollero A, Pita B, Monts-Mic R. Postoperative optical aberrations in eyes implanted with AcrySof spherical and aspheric intraocular lenses. J Refract Surg. 2008;24 (8:811–816. doi: 10.3928/1081597X-20081001-08. [DOI] [PubMed] [Google Scholar]
- Padmanabhan P, Yoon G, Porter J, Rao SK, Roy J, Choudhury M. Wavefront aberrations in eyes with Acrysof monofocal intraocular lenses. J Refract Surg. 2006;22 (3:237–242. doi: 10.3928/1081-597X-20060301-07. [DOI] [PubMed] [Google Scholar]
- Ortiz D, Ali JL, Bernabu G, Pongo V. Optical performance of monofocal and multifocal intraocular lenses in the human eye. J Cataract Refract Surg. 2008;34 (5:755–762. doi: 10.1016/j.jcrs.2007.12.038. [DOI] [PubMed] [Google Scholar]
- Toto L, Falconio G, Vecchiarino L, Scorcia V, Di Nicola M, Ballone E, et al. Visual performance and biocompatibility of 2 multifocal diffractive IOLs: six-month comparative study. J Cataract Refract Surg. 2007;33 (8:1419–1425. doi: 10.1016/j.jcrs.2007.05.010. [DOI] [PubMed] [Google Scholar]
- Campbell CE. Wavefront measurements of diffractive and refractive multifocal intraocular lenses in an artificial eye. J Refract Surg. 2008;24 (3:308–311. doi: 10.3928/1081597X-20080301-15. [DOI] [PubMed] [Google Scholar]
- Li Y, Choi JA, Kim H, Yu S, Joo C. Changes in ocular wavefront aberrations and retinal image quality with objective accommodation. J Cataract Refract Surg. 2011;37 (5:835–841. doi: 10.1016/j.jcrs.2010.11.031. [DOI] [PubMed] [Google Scholar]
- Santhiago MR, Netto MV, Barreto J, Gomes BA, Schaefer A, Kara N. Wavefront analysis and modulation transfer function of three multifocal intraocular lenses. Indian J Ophthalmol. 2010;58 (2:109–113. doi: 10.4103/0301-4738.60075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nanavaty MA, Spalton DJ, Marshall J. Effect of intraocular lens asphericity on vertical coma aberration. J Cataract Refract Surg. 2010;36 (2:215–221. doi: 10.1016/j.jcrs.2009.08.024. [DOI] [PubMed] [Google Scholar]
- Rozema J, Koppen C, de Groot V, Tassignon M. Influence of neodymium: YAG laser capsulotomy on ocular wavefront aberrations in pseudophakic eyes with hydrophilic and hydrophobic intraocular lenses. J Cataract Refract Surg. 2009;35 (11:1906–1910. doi: 10.1016/j.jcrs.2009.06.033. [DOI] [PubMed] [Google Scholar]
- Bartsch DU, Bessho K, Gomez L, Freeman WR. Comparison of laser ray-tracing and skiascopic ocular wavefront-sensing devices. Eye (Lond) 2008;22 (11:1384–1390. doi: 10.1038/sj.eye.6702901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rozema J, Van Dyck DE, Tassignon M. Clinical comparison of 6 aberrometers. Part 1: Technical specifications. J Cataract Refract Surg. 2005;31 (6:1114–1127. doi: 10.1016/j.jcrs.2004.11.051. [DOI] [PubMed] [Google Scholar]
- Rozema J, Van Dyck DE, Tassignon M. Clinical comparison of 6 aberrometers. Part 2: statistical comparison in a test group. J Cataract Refract Surg. 2006;32 (1:33–44. doi: 10.1016/j.jcrs.2004.11.052. [DOI] [PubMed] [Google Scholar]
- Moreno Barriuso E, Navarro R. Laser ray tracing versus Hartmann–Shack sensor for measuring optical aberrations in the human eye. J Opt Soc Am A Opt Image Sci Vis. 2000;17 (6:974–985. doi: 10.1364/josaa.17.000974. [DOI] [PubMed] [Google Scholar]
- Visser N, Berendschot TT, Verbakel F, Tan AN, de Brabander J, Nuijts RM. Evaluation of the comparability and repeatability of four wavefront aberrometers. Invest Ophthalmol Vis Sci. 2011;52 (3:1302–1311. doi: 10.1167/iovs.10-5841. [DOI] [PubMed] [Google Scholar]
- Awwad ST, Lehmann JD, McCulley JP, Bowman RW. A comparison of higher order aberrations in eyes implanted with AcrySof IQ SN60WF and AcrySof SN60AT intraocular lenses. Eur J Ophthalmol. 2007;17 (3:320–326. doi: 10.1177/112067210701700307. [DOI] [PubMed] [Google Scholar]
- Awwad ST, Warmerdam D, Bowman RW, Dwarakanathan S, Cavanagh HD, McCulley JP. Contrast sensitivity and higher order aberrations in eyes implanted with AcrySof IQ SN60WF and AcrySof SN60AT intraocular lenses. J Refract Surg. 2008;24 (6:619–625. doi: 10.3928/1081597X-20080601-12. [DOI] [PubMed] [Google Scholar]