Abstract
Aims
To assess the vision-related quality of life of corneal transplant recipients using the National Eye Institute Visual Function Questionnaire-25 (NEI VFQ-25), and to identify the socio-demographic factors that associate with patients' self-assessment of perceived visual function.
Methods
Thirty patients who received corneal transplants were included in this prospective observational, cross-sectional study. Socio-demographic and clinical data, including age, sex, systemic health status, employment status, visual acuity, reason of corneal transplantation, laterality of corneal graft, and follow-up period were collected. NEI VFQ-25 was scored using Rasch analysis. Subgroup analyses were also performed.
Results
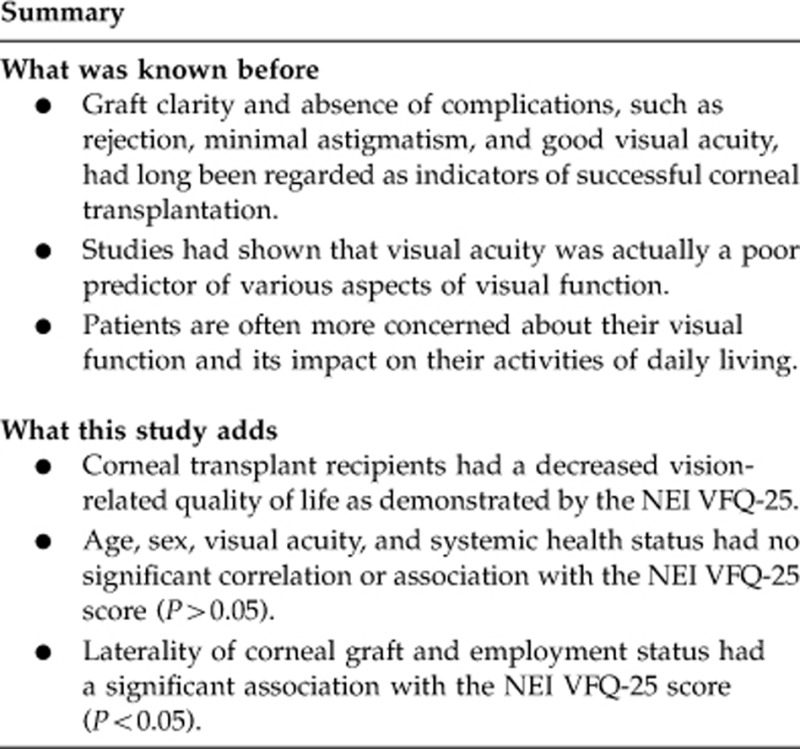
Age, sex, visual acuity, and health status had no significant correlation or association with the Rasch-transformed score. Patients who received bilateral corneal grafts were significantly less able socioemotionally than those with unilateral graft. Patients who became unemployed or retired after transplantation were also significantly less able in both visual functioning and socioemotional status.
Conclusion
Corneal transplant recipients had a decreased vision-related quality of life as demonstrated by the NEI VFQ-25. Apart from anatomical success and visual acuity, ophthalmologists should also consider other aspects of visual outcome. In particular, those who received bilateral grafts require more attention. Employment programmes should be part of corneal transplantation rehabilitation planning.
Keywords: corneal transplant, quality of life, visual function
Introduction
Corneal transplant is a vision-saving procedure and is the most common type of human transplant surgery.1 A surgeon's definition of successful corneal transplantation is often based on the postoperative anatomical outcome and visual acuity. However, these criteria do not necessarily correlate with the patient's performance of daily activities.2, 3, 4, 5 A patient's perception may be completely different. It has been shown that disparities exist between ophthalmologists and their patients in estimating the benefit of treatment. The reason is clinical examinations do not evaluate patients' subjective perception of their own diseases.6 The patients' expectations may not be met, and they may still experience poor functional outcome despite successful corneal transplantion.7
To understand the patients' situation and need, it is also important to evaluate their vision-related quality of life in addition to standard clinical variables. A number of self-reported questionnaires had been designed to address this issue, one of which is the National Eye Institute Visual Function Questionnaire-25 (NEI VFQ-25). The NEI VFQ-25 is a questionnaire that was developed to evaluate the vision-related quality of life of patients with ocular diseases, and to test the psychometric properties of diseases that cause vision loss.8 It has been widely used to study the quality of life in patients with various ocular diseases, including cataract,9 glaucoma,10 age-related macular degeneration,11 diabetic retinopathy,12 central or branch retinal vein occlusion,13, 14 retinal detachment,15 and Graves' ophthalmopathy.16
This study aimed to assess the vision-related quality of life in corneal transplant recipients using the NEI VFQ-25. It also aimed to identify the socio-demographic factors that associate with the patients' self-assessment of perceived visual function.
Materials and methods
The authors obtained prior approval of the study protocol from the Survey and Behavioural Research Ethics Sub-Committee, Faculty of Medicine, The Chinese University of Hong Kong, and the Ethics Committee of Kowloon West Cluster, Hospital Authority, Hong Kong. The study was conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from all recruited patients.
Patient selection
This is a prospective, observational, cross-sectional study. Corneal transplant recipients scheduled for consultation sessions were recruited. Inclusion criteria were 18 years old or above, recipients of corneal graft, minimum 1 year of follow-up after corneal transplantation, absence of other systemic or ocular diseases that could potentially affect vision, and the patient being able to understand and being willing to give informed consent to the study. Eligible patients were asked to participate in a 10-min questionnaire survey. The first 30 consecutive patients to complete the questionnaire were included in the study. All patients were ethnic Chinese.
Socio-demographic and clinical data collection
Socio-demographic data, including age, sex, systemic health status, and employment status before and after corneal transplant operation were collected. Clinical data, including visual acuity, reason of corneal transplantation, laterality of corneal graft, and follow-up period were also collected.
For practical reasons, the visual acuity included in this study was based on Snellen chart with roman numerals. In our population, among people aged 55 years or above, 33.3% of men and 55.1% of women had no schooling or had only attained pre-primary education.17 This lack of formal education was attributed by the unavailability of schools before and after the Second World War and the relative poverty during that period.18 Hence, Snellen chart with roman numerals had to be adopted because of the inability of many patients to recognize the alphabets on the ETDRS chart.
Questionnaire on vision-related quality of life
The Chinese version of the NEI VFQ-25 was used to assess the vision-related quality of life in recruited subjects. The Chinese version had been validated with its reliability established.18 It consists of a general health rating question, and addresses a number of vision-related subscales, including general vision, difficulty with near and distance activities, limitations with peripheral and colour vision, ocular pain, social functioning, role limitations, dependency, and mental health. Subjects were asked to rate the level of severity of their difficulties in daily activities.
Statistical analysis
The NEI VFQ-25 was scored using Rasch analysis, transforming the raw questionnaire data, which were composed of nominal numeric values, into a continuous scale. This enabled valid parametric statistical analysis of the questionnaire's output. The data were analysed based on the Long-form Visual Functioning Scale25 (LFVFS25) and the Long-form Socioemotional Scale25 (LFSES25).19 Correlation between age and the score was assessed using Pearson's correlation. Association between sex and the score was analysed using Student's t-test. In addition, patients were divided into two groups based on visual acuity, namely those with Snellen vision worse than 20/400 or those better than 20/400. The value of 20/400 was chosen as this is the definition of legal blindness based on World Health Organization criteria.20 The difference in the scores obtained by these two groups of subjects was assessed. Patients were also divided into two groups according to their systemic health status. The scores of patients with vs without systemic diseases were compared. Likewise, the scores reported by patients who received unilateral vs bilateral corneal grafts were compared. The difference in the scores for employment status was also determined.
The data were entered onto a Microsoft Excel spreadsheet (Microsoft, Redmond, WA, USA) for compilation. Conversion to Rasch scores was performed by using specially designed Excel spreadsheets.19 Subsequent analysis was performed using the Statistical Package for the Social Sciences version 10.0 for Windows software (SPSS, Inc., Chicago, IL, USA). Continuous data were expressed in mean±SD. A P-value of <0.05 was considered to be statistically significant.
Results
Patient demographics and clinical status
Thirty patients were recruited for the study. The average age was 60±15 years (range, 24–83). The male to female ratio was 15 : 15. Twenty-two had unilateral whereas eight had bilateral corneal grafts. The mean duration of follow-up since receiving the corneal graft was 10.4±6.7 years (range, 1–22). The visual acuity is better than 20/400 in 70% and worse than 20/400 in 30%. Further breakdown of patient demographics is summarized in Table 1.
Table 1. Patient demographics of the study group.
| Features | Count |
|---|---|
| No. of patients | 30 |
| Mean age±SD (years) | 60±15 (range, 24–83) |
| Male : female ratio | 15 : 15 |
| Male: mean age ±SD (years) | 60±14 (range, 30–80) |
| Female: mean age ±SD (years) | 59±17 (range, 24–83) |
| Systemic health status | |
| With systemic diseases | 15 (50%) |
| Without systemic diseases | 15 (50%) |
| Unilateral : bilateral corneal grafts | 22 : 8 |
| Mean duration since transplantation (years) | 10.4±6.7 (range, 1–22) |
| 1–5 | 8 (26.7%) |
| 6–10 | 8 (26.7%) |
| 11–15 | 5 (16.7%) |
| >15 | 9 (30%) |
| Employment status | |
| Unchanged after transplantation | 17 (56.7%) |
| Became unemployed or retired after transplantation | 13 (43.3%) |
Percentages may not total up to 100 due to effect of rounding off.
Vision-related quality-of-life assessment
Table 2 shows the Rasch-transformed scores of the NEI VFQ-25 based on LFVFS25 and LFSES25. Using Rasch-transformed scores, age, sex, visual acuity, and systemic health status had no significant correlation or association with the scores obtained (P>0.05). On the other hand, laterality of corneal graft had a significant association with the score on the LFSES25. Patients who received bilateral corneal grafts were significantly less able socioemotionally when compared with those who had unilateral corneal graft (P<0.05). In addition, employment status also had a significant association with the scores on both the LFVFS25 and the LFSES25. For both visual functioning and socioemotional status, patients whose employment status remained unchanged after corneal transplantation were significantly more able when compared with those who became unemployed or retired after their operations (P<0.05).
Table 2. The mean National Eye Institute Visual Function Questionnaire-25 (NEI VFQ-25) Rasch-transformed scores.
| LFVFS25 items | Rasch-transformed score | LFSES25 items | Rasch-transformed score |
|---|---|---|---|
| Eyesight | 0.00±3.87 | See how people react to things | −0.25±2.38 |
| Read ordinary print in newspapers | −0.48±2.83 | Visiting with people in their homes, or at parties, or in restaurants | 0.00±2.38 |
| See well close-up | −1.37±2.41 | Accomplish less | 0.84±2.26 |
| Find something on a crowded shelf | −0.29±2.35 | Limited | −0.30±2.29 |
| Read street signs or the names of stores | −0.28±2.66 | Stay home most of the time | 0.35±2.03 |
| Going down steps, stairs, or curbs in dim light or at night | −0.91±2.61 | Frustrated | −1.88±1.74 |
| Notice objects off to the side while walking | −0.45±2.41 | Much less control | −0.55±2.14 |
| Rely too much on what other people tell | −0.36±1.84 | ||
| Need a lot of help | 0.03±1.99 | ||
| Do things that will embarrass | 0.15±1.94 |
Abbreviations: LFVFS25, Long-form Visual Functioning Scale25; LFSES25, Long-form Socioemotional Scale25.
Data are presented as mean±SD.
Table 3 illustrates further analysis of the LFVFS25 and LFSES25 Rasch-transformed scores based on laterality of the corneal graft and employment status. When compared with those with unilateral corneal graft, patients who received bilateral corneal grafts were less able in all but the ‘frustrated' item. The difference was significant in the ‘see how people react to things', ‘accomplish less', and ‘limited' items on the LFSES25 (P<0.05).
Table 3. The National Eye Institute Visual Function Questionnaire-25 (NEI VFQ-25) Rasch-transformed scores analysed based on laterality of corneal graft and employment status.
| Items | Unilateral corneal graft (n=22) | Bilateral corneal grafts (n=8) | P-value | Unemployed or retired after operation (n=13) | Employment status unchanged (n=17) | P-value |
|---|---|---|---|---|---|---|
| LFVFS25 | ||||||
| Eyesight | −0.10 | 0.26 | 0.86 | 1.74 | −1.34 | 0.02 |
| Read ordinary print in newspapers | −0.88 | 1.01 | 0.07 | 1.08 | −1.64 | 0.02 |
| See well close-up | −1.86 | −0.01 | 0.08 | −1.07 | −1.60 | 0.57 |
| Find something on a crowded shelf | −0.64 | 0.67 | 0.27 | 0.64 | −1.00 | 0.07 |
| Read street signs or the names of stores | −0.61 | 0.62 | 0.24 | 0.93 | −1.21 | 0.03 |
| Going down steps, stairs, or curbs in dim light or at night | −1.57 | 0.91 | 0.03 | −0.66 | −1.11 | 0.65 |
| Notice objects off to the side while walking | −1.10 | 1.35 | 0.05 | 0.44 | −1.12 | 0.09 |
| LFSES25 | ||||||
| See how people react to things | −1.01 | 1.84 | 0.02 | 0.03 | −0.47 | 0.58 |
| Visiting with people in their homes, or at parties, or in restaurants | −0.47 | 1.46 | 0.08 | 1.12 | −0.91 | 0.02 |
| Accomplish less | −1.20 | 0.14 | 0.05 | −0.04 | −1.46 | 0.08 |
| Limited | −0.73 | 0.86 | 0.04 | 0.90 | −1.22 | 0.01 |
| Stay home most of the time | 0.09 | 1.27 | 0.31 | 1.67 | −0.87 | 0.00 |
| Frustrated | −1.85 | −1.98 | 0.83 | −1.16 | −2.47 | 0.12 |
| Much less control | −1.01 | 0.76 | 0.08 | 0.41 | −1.58 | 0.02 |
| Rely too much on what other people tell | −0.53 | 0.06 | 0.50 | 0.63 | −1.20 | 0.02 |
| Need a lot of help | −0.15 | 0.40 | 0.54 | 1.23 | −0.83 | 0.02 |
| Do things that will embarrass | −0.08 | 0.59 | 0.45 | 1.73 | −0.98 | 0.00 |
Abbreviations: LFVFS25, Long-form Visual Functioning Scale25; LFSES25, Long-form Socioemotional Scale25.
Patients whose employment status remained unchanged after corneal transplantation were more able in all items than those who became unemployed or retired. The difference was significant in the ‘eyesight', ‘read ordinary print in newspapers' and ‘read street signs or the names of stores' items on the LFVFS25 (P<0.05), and in the ‘visiting with people in their homes, or at parties, or in restaurants', ‘limited', ‘stay home most of the time', ‘much less control', ‘rely too much on what other people tell', ‘need a lot of help', and ‘do things that will embarrass' items on the LFSES25 (P<0.05).
Discussion
Graft clarity and absence of complications, such as rejection, minimal astigmatism, and good visual acuity, had long been regarded as indicators of successful corneal transplantation. However, patients are often more concerned about their visual function and its impact on their activities of daily living. It was until the 1980s when ophthalmologists started to agree that measuring visual acuity alone may not adequately reflect visual function from the patients' perspective.21 Studies had shown that visual acuity was actually a poor predictor of various aspects of visual function.22, 23, 24, 25, 26, 27, 28, 29 Other important aspects of visual function included contrast sensitivity30, 31, 32 or simply reading performance.33
Because of this increase in interest in vision-related quality of life as an outcome measure, a number of questionnaires had been designed. The Medical Outcomes Study Short Form-36 (SF-36)34 is a multi-purpose medical health survey containing 36 questions. The questionnaire is easy to use and is considered reliable. However, there is a weak correlation between all SF-36 domains and visual acuity or visual field impairment.35 The VF-14 is a reliable and valid measure of functional impairment caused by cataract,2 yet visual field defect and colour vision were excluded.
The NEI VFQ-25 is easy to use, fully validated, and is considered reliable.35 It has been translated into many languages and was applied to patients with various ocular diseases. The original English version of the NEI VFQ-25 consists of 1 general health rating question and 11 vision-related domains, namely general vision, ocular pain, near vision, distance vision, social functioning, mental health, role difficulties, dependency, driving difficulties, colour vision, and peripheral vision. The validated Chinese version of the questionnaire omitted the driving subscale as almost all Chinese participants did not drive. Going out to watch movies, plays or sporting events also had a high non-response rate; these had been replaced with another question regarding difficulty when watching and enjoying television programmes. The five-level general health rating was also substituted with the 0–10 rating scale in the appendix.18
Corneal transplant recipients had a decreased vision-related quality of life as demonstrated by the NEI VFQ-25. Studies had shown that depression was common among adults with visual impairment.36, 37 This is of particular relevance to corneal graft recipients. Although most patients with cataract or age-related macular degeneration are the elderly, many corneal graft recipients are young, fit adults who require corneal transplantation for indications, such as trauma, keratitis, or keratoconus.
Depression has adverse effects on a person's work performance,38 interpersonal relationship,39 and general health.40 Depression could also influence a patient's self-perception of the burden of eye disease and treatment effectiveness.41 It is therefore important to identify corneal graft recipients who are at risk of developing depression given the availability of effective treatment for the condition. The NEI VFQ-25 can act as a useful tool to screen for such patients. Once they are identified, strategies that target at teaching them to cope with vision loss can be implemented to reduce the impact on their daily functioning. In addition, corneal graft recipients should receive proper preoperative counselling so that they can formulate a realistic expectation of the outcome following corneal transplantation.
Systemic diseases and comorbidities may affect the NEI VFQ-25 score.14 The subjects in our study were divided into two groups based on their systemic health status. The first group consisted of patients with no systemic diseases and the second group patients with any systemic diseases. Each group consisted of 15 patients. Reported systemic diseases in the study group included hypertension, diabetes mellitus, heart disease, chronic obstructive airway disease, gout, epilepsy, and cervical spondylosis. There was no significant difference between the scores obtained by the two groups (P>0.05). Furthermore, to reduce the effect of co-existing ocular diseases on the NEI VFQ-25 score, we had excluded patients with other ocular diseases from our study. These supported the analysis that corneal transplant recipients had a decreased vision-related quality of life.
When compared with those with unilateral corneal grafts, patients who received bilateral corneal grafts were found to be less able in their socioemotional status as indicated by their Rasch-transformed scores on the LFSES25. This suggested that more attention should be put on patients who received bilateral corneal grafts to ensure they could maintain as good a socioemotional quality of life as possible. Patients with bilateral corneal grafts may need more time to adapt to their change. This pointed to their need for enhanced preoperative counselling and postoperative rehabilitation programmes.
Employment status also had an impact on the NEI VFQ-25 score. Patients who became unemployed or retired after corneal transplantation were significantly less able in many items on both the LFVFS25 and the LFSES25. We believe the relationship between employment status and vision-related quality of life is bidirectional. In other words, patients who remained employed after their operations had a better quality of life, and patients who had a better vision-related quality of life were more readily available for employment. We propose implementation of employment programmes as part of the rehabilitation planning for corneal transplant recipients.
With advances in skills and the availability of better instruments, surgical success in performing corneal transplantation is increasing. In the same time, vision-related quality of life of corneal graft recipients deserves more attention from ophthalmologists as it provides a more complete picture of patient satisfaction and daily performance. Ophthalmologists should provide proper preoperative counselling to candidates of corneal transplantation. This allows them to formulate a more realistic prediction of their postoperative outcome so as to raise their vision-related quality of life. A multidisciplinary approach should be adopted. Apart from doctors, a rehabilitation team involving social workers and psychologists would be of value as they could assist patients in various activities of daily living by arranging jobs and providing psychological and social support.
Acknowledgments
The NEI VFQ-25 was developed by RAND and sponsored by the National Eye Institute, the USA. The Chinese version was translated and validated by Drs CWS Chan, D Wong, CLK Lam, S McGhee, and WW Lai, The University of Hong Kong. The Hong Kong Cornea Concern Association assisted in conducting the study. Professor JSY Chor, School of Public Health and Primary Care, The Chinese University of Hong Kong, provided suggestions on the study design. Drs KM Hui, TW Leung, and CH Kwong, Department of Ophthalmology, Caritas Medical Centre, Hong Kong, helped recruit patients for the study.
The authors declare no conflict of interest.
References
- Waldock A, Cook SD. Corneal transplantation: how successful are we. Br J Ophthalmol. 2000;84:813–815. doi: 10.1136/bjo.84.8.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg EP, Tielsch JM, Schein OD, Javitt JC, Sharkey P, Cassard SD, et al. The VF-14. An index of functional impairment in patients with cataract. Arch Ophthalmol. 1994;112:630–638. doi: 10.1001/archopht.1994.01090170074026. [DOI] [PubMed] [Google Scholar]
- Williams KA, Ash JK, Pararajasegaram P, Harris S, Coster DJ. Long-term outcome after corneal transplantation. Visual result and patient perception of success. Ophthalmology. 1991;98:651–657. doi: 10.1016/s0161-6420(91)32238-3. [DOI] [PubMed] [Google Scholar]
- Musch DC, Farjo AA, Meyer RF, Waldo MN, Janz NK. Assessment of health-related quality of life after corneal transplantation. Am J Ophthalmol. 1997;124:1–8. doi: 10.1016/s0002-9394(14)71636-8. [DOI] [PubMed] [Google Scholar]
- Sharma S, Brown GC, Brown MM, Shah GK, Snow K, Brown H, et al. Converting visual acuity to utilities. Can J Ophthalmol. 2000;35:267–272. doi: 10.1016/s0008-4182(00)80077-0. [DOI] [PubMed] [Google Scholar]
- Stein JD. Disparities between ophthalmologists and their patients in estimating quality of life. Curr Opin Ophthalmol. 2004;15:238–243. doi: 10.1097/01.icu.0000120712.35941.ad. [DOI] [PubMed] [Google Scholar]
- Mendes F, Schaumberg DA, Navon S. Assessment of Visual Function after Corneal Transplantation: The Quality of Life and Psychometric Assessment after Corneal Transplantation (Q-PACT) Study. Am J Ophth. 2003;135:785–793. doi: 10.1016/s0002-9394(02)02278-x. [DOI] [PubMed] [Google Scholar]
- Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD. Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2001;119:1050–1058. doi: 10.1001/archopht.119.7.1050. [DOI] [PubMed] [Google Scholar]
- Espindle D, Crawford B, Maxwell A, Rajagopalan K, Barnes R, Harris B, et al. Quality-of-life improvements in cataract patients with bilateral blue light-filtering intraocular lenses: clinical trial. J Cataract Refract Surg. 2005;31:1952–1959. doi: 10.1016/j.jcrs.2005.03.060. [DOI] [PubMed] [Google Scholar]
- McKean-Cowdin R, Wang Y, Wu J, Azen SP, Varma R, Los Angeles Latino Eye Study Group Impact of visual field loss on health-related quality of life in glaucoma: the Los Angeles Latino Eye Study. Ophthalmology. 2008;115:941–948. doi: 10.1016/j.ophtha.2007.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lotery A, Xu X, Zlatava G, Loftus J. Burden of illness, visual impairment and health resource utilisation of patients with neovascular age-related macular degeneration: results from the UK cohort of a five-country cross-sectional study. Br J Ophthalmol. 2007;91:1303–1307. doi: 10.1136/bjo.2007.116939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein R, Moss SE, Klein BE, Gutierrez P, Mangione CM. The NEI-VFQ-25 in people with long-term type 1 diabetes mellitus: the Wisconsin Epidemiologic Study of Diabetic Retinopathy. Arch Ophthalmol. 2001;119:733–740. doi: 10.1001/archopht.119.5.733. [DOI] [PubMed] [Google Scholar]
- Deramo VA, Cox TA, Syed AB, Lee PP, Fekrat S. Vision-related quality of life in people with central retinal vein occlusion using the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2003;121:1297–1302. doi: 10.1001/archopht.121.9.1297. [DOI] [PubMed] [Google Scholar]
- Awdeh RM, Elsing SH, Deramo VA, Stinnett S, Lee PP, Fekrat S. Vision-related quality of life in persons with unilateral branch retinal vein occlusion using the 25-item National Eye Institute Visual Function Questionnaire. Br J Ophthalmol. 2010;94:319–323. doi: 10.1136/bjo.2007.135913. [DOI] [PubMed] [Google Scholar]
- Okamoto F, Okamoto Y, Hiraoka T, Oshika T. Vision-related quality of life and visual function after retinal detachment surgery. Am J Ophthalmol. 2008;146:85–90. doi: 10.1016/j.ajo.2008.02.011. [DOI] [PubMed] [Google Scholar]
- Bradley EA, Sloan JA, Novotny PJ, Garrity JA, Woog JJ, West SK. Evaluation of the National Eye Institute Visual Function Questionnaire in Graves' ophthalmopathy. Ophthalmology. 2006;113:1450–1454. doi: 10.1016/j.ophtha.2006.02.060. [DOI] [PubMed] [Google Scholar]
- Census and Statistics Department, The Government of the Hong Kong Special Administrative Region. Hong Kong 2006 Population By-census Main Report 2006. Volume I. The Government Logistics Department, The Government of the Hong Kong Special Administrative Region: Hong Kong.
- Chan CWS, Wong D, Lam CLK, McGhee S, Lai WW. Development of a Chinese version of the National Eye Institute Visual Function Questionnaire (CHI-VFQ-25) as a tool to study patients with eye diseases in Hong Kong. Br J Ophthalmol. 2009;93:1431–1936. doi: 10.1136/bjo.2009.158428. [DOI] [PubMed] [Google Scholar]
- Pesudovs K, Gothwal VK, Wright T, Lamoureux EL. Remediating serious flaws in the National Eye Institute Visual Function Questionnaire. J Cataract Refract Surg. 2010;36:718–732. doi: 10.1016/j.jcrs.2009.11.019. [DOI] [PubMed] [Google Scholar]
- World Health Organization Statistical Classification of Diseases and Related Health Problems10th revised edn. World Health Organization: Geneva; 1992 [Google Scholar]
- Massof RW, Rubin GS. Visual function assessment questionnaires. Surv Ophthalmol. 2001;45:531–548. doi: 10.1016/s0039-6257(01)00194-1. [DOI] [PubMed] [Google Scholar]
- Hess RF, Woo G. Vision through cataracts. Invest Ophthalmol Vis Sci. 1978;17:428–435. [PubMed] [Google Scholar]
- Paulsson L-E, Sjöstrand J. Contrast sensitivity in the presence of a glare light. Theoretical concepts and preliminary clinical studies. Invest Ophthalmol Vis Sci. 1980;19:401–406. [PubMed] [Google Scholar]
- Marron JA, Bailey IL. Visual factors and orientation-mobility performance. Am J Optom Physiol Opt. 1982;59:413–426. doi: 10.1097/00006324-198205000-00009. [DOI] [PubMed] [Google Scholar]
- Owsley C, Sloane ME. Contrast sensitivity, acuity, and the perception of ‘real-world' targets. Br J Ophthalmol. 1987;71:791–796. doi: 10.1136/bjo.71.10.791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lennerstrand G, Carl-Otto A. Contrast sensitivity in macular degeneration and the relation to subjective visual impairment. Acta Ophthalmol. 1989;67:225–233. doi: 10.1111/j.1755-3768.1989.tb01863.x. [DOI] [PubMed] [Google Scholar]
- Elliott DB, Hurst MA, Weatherill J. Comparing clinical tests of visual function in cataract with the patient's perceived visual disability. Eye. 1990;4:712–717. doi: 10.1038/eye.1990.100. [DOI] [PubMed] [Google Scholar]
- Elliott DB, Hurst MA. Simple clinical techniques to evaluate visual function in patients with early cataract. Optom Vis Sci. 1990;67:822–825. doi: 10.1097/00006324-199011000-00006. [DOI] [PubMed] [Google Scholar]
- Mangione CM, Phillips RS, Lawrence MG, Seddon JM, Orav EJ, Goldman L. Improved visual function and attenuation of declines in health-related quality of life after cataract extraction. Arch Ophthalmol. 1994;112:1419–1425. doi: 10.1001/archopht.1994.01090230033017. [DOI] [PubMed] [Google Scholar]
- Mannis MJ, Zadnik K, Johnson CA. The effect of penetrating keratoplasty on contrast sensitivity in keratoconus. Arch Ophthalmol. 1984;102:1513–1516. doi: 10.1001/archopht.1984.01040031233025. [DOI] [PubMed] [Google Scholar]
- Mannis MJ, Zadnik K, Johnson CA, Adams C. Contrast sensitivity after penetrating keratoplasty. Arch Ophthalmol. 1987;105:1220–1223. doi: 10.1001/archopht.1987.01060090078032. [DOI] [PubMed] [Google Scholar]
- Rubin GS, Adamsons IA, Stark WJ. Comparison of acuity, contrast sensitivity, and disability glare before and after cataract surgery. Arch Ophthalmol. 1993;111:56–61. doi: 10.1001/archopht.1993.01090010060027. [DOI] [PubMed] [Google Scholar]
- Hazel CA, Petre KL, Armstrong RA, Benson MT, Frost NA. Visual function and subjective quality of life compared in subjects with acquired macular disease. Invest Ophthalmol Vis Sci. 2000;41:1309–1315. [PubMed] [Google Scholar]
- Ware JE, Gandek B. Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. J Clin Epidemiol. 1998;51:903–912. doi: 10.1016/s0895-4356(98)00081-x. [DOI] [PubMed] [Google Scholar]
- Severn P, Fraser S, Finch T, May C. Which quality of life score is best for glaucoma patients and why. BMC Ophthalmol. 2008;8:2. doi: 10.1186/1471-2415-8-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rovner BW, Zisselman PM, Shmuely-Dulitzki Y. Depression and disability in older people with impaired vision: a follow-up study. J Am Geriatr Soc. 1996;44:181–184. doi: 10.1111/j.1532-5415.1996.tb02436.x. [DOI] [PubMed] [Google Scholar]
- Brody BL, Gamst AC, Williams RA, Smith AR, Lau PW, Dolnak D, et al. Depression, visual acuity, comorbidity, and disability associated with age-related macular degeneration Ophthalmology 20011081893–1900.discussion 1900-1901. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Akiskal HS, Ames M, Birnbaum H, Greenberg P, Hirschfeld RM, et al. Prevalence and effects of mood disorders on work performance in a nationally representative sample of U.S. workers. Am J Psychiatry. 2006;163:1561–1568. doi: 10.1176/appi.ajp.163.9.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knobloch LK, Knobloch-Fedders LM. The role of relational uncertainty in depressive symptoms and relationship quality. An actor—partner interdependence model. J Soc Personal Relationships. 2010;27:137–159. [Google Scholar]
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. The Lancet. 2007;370:851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- Owsley C, McGwin G. Depression and the 25-item National Eye Institute Visual Function Questionnaire in older adults. Ophthalmology. 2004;111:2259–2264. doi: 10.1016/j.ophtha.2004.06.026. [DOI] [PubMed] [Google Scholar]


