Abstract
Objective
The “Heidelberg Model of Music Therapy for Chronic Tinnitus” is a manualized short term treatment (nine 50-minutes sessions of individualized therapy on five consecutive days). It has proven to be efficient in reducing tinnitus symptoms in the short run. Now the long-term impact of the treatment after up to 5.4 years should be explored.
Materials and methods
206 patients who had attended the neuro-music therapy were addressed in a structured follow-up questionnaire survey. 107 complete questionnaires entered analysis. Follow-up time was 2.65 (SD 1.1) years.
Results
76% of the patients achieved a reliable reduction in their tinnitus scores, the overall tinnitus distress as measured by the Mini-TQ diminished from 11.9 (SD = 4.9) to 7.4 (SD = 5.2) points, 87% of the patients were satisfied by the way they were treated during therapy, and 71% of the patients did not undergo any further treatment after. Evaluation of therapeutic elements displays, that only music therapy specific interventions were rated helpful by the patients. Tinnitus related factors (such as tinnitus pitch or loudness, time since onset) did not influence therapy outcome but female gender, positive therapeutic relationship, and higher initial Mini-TQ scores became apparent as factors predicting better chances for greater therapy success.
Discussion
The “Heidelberg Model of Music Therapy for Chronic Tinnitus” seems to be effective in the long run. The outcome effect size of d’ = 0.89, can be accounted for as “large” effect and falls into the upper range value compared to established treatments.
Keywords: Music Therapy, tinnitus, long-term outcome, tinnitus questionnaire, odds ratio, logistic regression
Introduction
Tinnitus, the enduring perception of ringing or buzzing sounds without an external source, is one of the most common symptoms in ENT medicine [1]. In western countries about 5 - 15 % of the population suffer from tinnitus [2].
Three factors leading to tinnitus perception are prominent in discussion [3]: 1. changes in the sensory input (e.g. hearing loss increases annoyance [4]), 2. psychological strains and their underlying neurophysiological network [5] and 3. changes in the neural activity in the brain. Since there is no integrative knowledge about the underlying mechanisms generating tinnitus [6], different tinnitus models based on different aspects of these factors are under discussion. The “gain control” model [7] assumes that peripheral sensory deprivation due to cochlear damages increases neuronal activity in the central auditory system in order to adapt neural sensitivity to the reduced sensory inputs. This central gain could over amplify “neural noise” thus ultimately causing the percept of tinnitus. According to the “noise cancellation” model [8], tinnitus is related to dysfunctional feedback connections from limbic regions to auditory brain areas interacting at the thalamic level. Normally, the limbic system may indentify and inhibit an irrelevant sensory signal and thus prevent it from reaching auditory cortex. In cases in which this limbic regulation is compromised, the ‘noise-cancellation’ mechanism breaks down and the tinnitus signal is relayed to the auditory cortex where it enters into consciousness.
Tinnitus research has evolved remarkably in the last years suggesting a variety of promising treatment options [9-12]. To our knowledge, only cognitive-behavioural therapy (CBT) and tinnitus retraining therapy (TRT) have been evaluated in long-term studies covering more than 12 months so far. CBT is short in duration (several weeks to months) but nevertheless has long lasting effects [11] up to 15 years after treatment [13-16]. In more time consuming therapy approaches (duration up to 18 months) such as the TRT [12] the global improvement in tinnitus scores accrues over a longer period only but then it seems to be a stable and clinically significant therapy [17-20].
Irrespective of the type of therapy, treatment outcome seems to stabilize over time, though the prognosis of the therapeutic outcome remains individualized. Prominent moderating variables turn out to be initial tinnitus symptoms and possible co-morbidities (esp. psychological strains / psychiatric diseases and otological risk factors, mostly hearing impairment and hyperacusis). Therapies with an in-patient setting appear to be the best option in severe, multimorbid cases [21] while outpatient treatments are sufficient for patients with lower tinnitus related distress [22,23]. Furthermore, therapeutic concepts incorporating both training techniques aiming at a neuronal reorganisation accompanied by procedures to solidify the results on an emotional level should secure the most sufficient and long lasting reduction of tinnitus symptoms.
In 2004 a novel treatment option, referred to as "Heidelberg Model of Music Therapy", was first offered. This neuro-music therapy for chronic tinnitus strives for an integration of strategies to manage the psychological state and possibly restore the assumed underlying neurophysiological reorganisation in both the lemniscal and extralemniscal auditory pathways [24]. For this purpose, complementary music- and psychotherapeutic interventions and techniques are structured into modules. This makes up a manualized short term music therapeutic treatment concept (see section ‘materials and methods’ for detailed description of this music therapy manual). Results from several clinical trials [25-27] demonstrate that this integrative music therapy approach has proven to be an efficient means to reduce tinnitus distress. About 80% of the patients accomplish a reliable decrease of tinnitus distress as measured by the Tinnitus Questionnaire [28]. In the short run, this effect was independent of tinnitus characteristics or otological co-symptoms and remained unchanged at a follow-up after six months [29].
Since it is of utmost importance that therapy results are not just short-lived but enduring, it seems reasonable to investigate the long-term impact of the treatment option according to the “Heidelberg Model of Music Therapy for Chronic Tinnitus”. By means of a questionnaire survey, we wanted to assess especially the sustainable efficiency. Of further interest was to explore factors possibly moderating the chance for therapy success or failure. Such potential predictors include patient characteristics (i.e. demographic factors such as age or gender); factors related to tinnitus (e.g. otological characteristics, tinnitus history) and music therapy related factors (e.g. role of music therapy specific interventions, patient-therapist relationship).
Materials and methods
Subjects
The neuro-music therapy according to the “Heidelberg Model of Music Therapy for Chronic Tinnitus” was announced by press releases (newspapers and magazines, radio and TV) and offered to patients at the outpatient department of the ENT-clinic of the university hospital Heidelberg as well as to patients of ENT-doctors in own practice nationwide.
All patients attending the neuro-music therapy at the German Center for Music Therapy Research during the period October 2004 to June 2009 were eligible for this survey. Patients taking part in evaluative clinical trials were excluded due to the extra amount of assistance and additional measurement procedures typical for clinical trials.
At time of admission for therapy, all patients suffered from chronic tinnitus which had lasted for at least six months. The “Heidelberg Model” is eligible for patients who do not have any psychiatric disorder, are of the minimum age of 18 years and have hearing loss in pure tone audiometry no greater than 50 dB HL up to the frequency region of their estimated tinnitus pitch (if necessary patients have to be provided with hearing aids).
All subjects gave written informed consent in accordance with the Declaration of Helsinki. The survey was in accordance with the requirements of the local institutional review board.
Design
Overall 206 patients who had received music therapy in the regular care were addressed in August 2010.
A detailed questionnaire (see survey questionnaire) was sent to them by electronic (n = 156) or surface (n = 50) mail. Nine questionnaires were undeliverable (n = 7 via e-mail, n = 2 via post), five patients declined to answer and three postponed their return due to an ongoing alternative treatment. Of the remaining n = 189 patients, n = 107 returned their questionnaires resulting in a response rate of 56.6%.
Music therapy treatment outline
The neuro-music therapy according to the Heidelberg Model for tinnitus is a manualized short term music therapeutic treatment lasting for nine consecutive 50-minutes sessions of individualized therapy. Therapy takes place on five consecutive days (from Monday to Friday) with two therapy sessions per day. The therapy is carried out by a team of two trained therapists (with academic degree, at least B.A.), usually one music therapist and one psychotherapist. The interventions are structured into the following modules:
Module 1: Counseling
All patients receive a comprehensive individualised personal instruction in order to establish a cognitive model of tinnitus. Patients are informed about the underlying neuroscientific principles of the music therapy. Possible physical diseases and current medications are examined. In case of doubt a physician is consulted. As the specific modules used in therapy are based on the patients’ individual tinnitus sound, their ‘tinnitus-equivalent’, has to be set up. For patients who describe their tinnitus as tonal, tinnitus frequency is matched by a sinus wave generator (Mair & Rohner OEG ©: Arbitrary Waveform Generator WG 810) which is able to generate arbitrary wave shapes with maximum clock frequency of 10MHz. In the tinnitus therapy we used the sinusoidal wave shape [30] only. For patients with noise-like tinnitus, the program “noise estimator” which generates noises of diverse bandwidth (up to 10.000 Hz) and pitch (up to 22.050 Hz) designed by © Dr.rer.med. Christoph M. Krick, Neurocenter of the Saarland University Clinic, was used to match the subjective tinnitus.
Module 2: Resonance Training
The Resonance Training is intended both to increase blood circulation of the entire head, especially in tinnitus related brain regions, and to innervate auditory pathway via somatosensory stimulation. The patients learn a vocal exercise stimulating the cranio-cervical resonating cavities. The supposed cranial activation can easily be inspected by palpating trigger points [31].
Module 3:Neuroauditive Cortex Training
The Neuroauditive Cortex Training uses tone sequences performed live by a trained music therapist on a piano which have to be vocally imitated by the patient. A systematic and targeted training of inaccurately intonated musical sounds enables the patients to exert influence on their auditory processes since they learn to actively filter out irrelevant information and to concentrate on relevant acoustic stimuli. In addition to an increased auditory attention control this training aims at a neuronal reorganization of the auditory cortex.
In chronic tinnitus characteristic auditory cortical reorganizations are traceable, which seem to be frequency specific [32,33]. Frequency discrimination training may interrupt the cortical representations that are generating tinnitus [34,35]. One possible explanation might be that the musical training leads to a suppression of neural activity by lateral inhibition of the auditory cortex [36]. Experimental data indicate that it is more efficient to train at normal hearing frequencies rather than in the region of hearing loss or tinnitus frequency [9,35]. We therefore propose that it is possible to alter the internal tinnitus spectrum by means of the Neuroauditive Cortex Training, which represents a specific perceptual training within in the normal hearing frequencies. Furthermore it is very important, to ensure the training regime is intrinsically motivating. Active music therapy guarantees the lasting co-operation of the patients.
Module 4:Tinnitus Reconditioning
The Tinnitus Reconditioning offers coping mechanisms related to stress control along with a sound based habituation procedure. 1. Relaxation training: A well known and effective relaxation exercise, the music therapeutic relaxation training according to Bolay/Selle [37] was adapted to the needs of the tinnitus therapy. By means of music as calming background stimulus, the balance between the activity of the sympathetic and the parasympathetic branches of the autonomic nervous system shall be restored. The attention is diverted from the tinnitus and physical recreation is supported. Additionally the patients imagine a positive autobiographic episode (e.g. reminiscence of a holiday experience) which serves as anchor stimulus: every time the patients call up this ‘well-being-imagination’, the bodily and mental relaxation should be triggered. 2. Habituation training: During the relaxation exercise, the tinnitus sound will be integrated intermittently into the background music. The volume is adapted to the individual hearing level compensating for a potential hearing deficit. For this purpose, before the training session starts, the patients have to set the background music to a convenient level such that they can easily listen to the music while still being able to follow verbal instructions from the therapist. 3. Stress management (Tinnitus Map): Subsequently the patients have to set up a ‘tinnitus-map’. This map identifies situations aggravating or intensifying the tinnitus. These aversive situations can be imagined during the relaxation. The patients thus learn to decouple tinnitus and aversive associations (Table 1).
Table 1.
Manual outline of the “Heidelberg Model of Music Therapy for Chronic Tinnitus”
| Module | Technique | Proposed working factor |
|---|---|---|
| Counseling | Neuroscientifically founded individualised personal instruction on tinnitus aetiopathology | NW: Counselling, facilitation of therapy motivation |
|
|
||
| Compilation of a tinnitus-sound equivalent by means of a sine-wave generator and conversion to the heptatonic scale | SW: Externalisation of the tinnitus, musical conversion | |
|
| ||
| Resonance Training | vocal exercises, i.e. intonation of the individual tinnitus sound and stimulation of craniocervical resonating cavities.→ stimulation of cranio-cervical resonating cavities | SW: Regain confidence in the own hearing; active masking of the tinnitus sound; increase of blood circulation, corrective stimulation of the auditory pathway by means of somatosensory innervations |
|
| ||
| Neuroauditive Cortex Training | Audition of unknown, standardized atonal music sequences | SW: Attention diversion, increase of discriminative abilities, enhancement of auditive skills |
|
|
||
| Detailed training of intonation and listening capacity in the range of the transposed tinnitus frequency by means of an intonation exercise of erroneous intervals in the range of the tinnitus frequency | SW: Neuronal reorganisation of the tonotopic representation in the auditory cortex | |
|
| ||
| Tinnitus Reconditioning | Musically based training in relaxation and self-control and creation of a ”well-being image“ as anchor for physiological relaxation | SW: Physical relaxation and regulation of physiological processes |
|
|
||
| Compilation of tinnitus evoking / attenuating factors and situations (temporal tinnitus map) | NW: Identification of unspecific factors SW: sensitization for connections between stress factors/well-being and tinnitus | |
|
|
||
| Systematic desensitization in order to decouple tinnitus from psychophysiological reaction patterns | SW: Subliminal training of auditory filtering; self-efficient steering of physical reactions on tinnitus perception | |
SW = Specific Working factor (proposed to be specific for the music therapy concept); NW = non-specific working factor (general factors).
Survey questionnaire data
Main measurements correspond to the German Clinical Practice Guideline [38].
Socio-demographic and otological data
Socio-demographic (gender, age, highest level of education, current occupation) and otological data from the intake interview were used. Otological data comprised: initial onset-time of tinnitus, tinnitus core frequency at intake in kHz, tinnitus minimum masking level [dB (SD)], subjective loudness on a scale 1-100, sound quality of the tinnitus (sinusoidal / narrow-band noise, broad-band noise), location of the tinnitus sounds (left/right ear, both ears, inside head), possible fluctuations of the tinnitus, previous therapies concerning especially sound stimulation devices (hearing aids / noiser, masker, tinnitus instrument).
Long-term therapy outcome
Tinnitus severity and individual tinnitus related distress were assessed by the German version of the Tinnitus Questionnaire (TQ, [28] in its abbreviated form, the “Mini-TQ” [39]). The most relevant twelve items of the German Version of the Tinnitus Questionnaire which have proven to be most sensitive to change constitute the Mini-TQ. Seven items concern intrusiveness and emotional distress, three cover cognitive distress, and one item captures sleep disturbance and negative effects on social relationships respectively. The Mini-TQ has no subscales due to the small number of items but the total score has good psychometric properties (reliability rtt = .89, internal consistency Cronbachs alpha = .90; validity: Pearson correlations between TQ and Mini-TQ: r = .93). Each item has to be answered on a three point-scale (the response alternatives for each item are true = 2 points, partly true = 1 point, and not true = 0 points). The final score results from the sum of all items and has a range from 0 to 24. The calculation of the quartiles leads to four clinical categories (0-7 points: light distress; 8-12 points: moderately distressed, 13-18 points: severely distressed, 19-24 points: most severely distressed).
Assessment of tinnitus symptoms by the Mini-TQ was performed three times: 1) at admission, 2) immediately after therapy at discharge and 3) after a period of up to 5.4 years succeeding therapy (follow-up – FU).
Follow-up questionnaire
At the time of the follow-up survey, a structured questionnaire was administered. This questionnaire is based on items from the Structural Tinnitus Interview [40], items recommended by the Tinnitus Research Initiative [41] and items specific for the music therapy approach. Main topics were subjective tinnitus characteristics (at time of therapy and currently), therapy satisfaction, subjective therapy outcome, therapy evaluation and subsequent treatment attempts (see Table 2).
Table 2.
contents of the follow-up-questionnaire
| Tinnitus characteristics |
| Please describe the tinnitus you wanted to be treated by music therapy (tonal/noisiform) |
| If you still perceive any tinnitus: Where do you perceive your tinnitus? (right side / left side / both sides / inside the head / elsewhere) |
| If you still perceive any tinnitus: Please rate the intrusiveness of your current tinnitus (0 = not intrusive/100 extremely intrusive) |
| Therapy satisfaction |
| Therapeutic relationship: Please rate your satisfaction concerning the therapist-patient relationship (5-point scale: very dissatisfied – very satisfied) |
| Therapy satisfaction: Please rate your satisfaction concerning the treatment (5-point scale: very dissatisfied – very satisfied) |
| Subjective therapy outcome |
| Was your tinnitus percept changed by the music therapy? (worsened/unaffected/improved) |
| How did the tinnitus change since therapy? (no tinnitus any more / periods without tinnitus / tinnitus present all time) |
| Therapy evaluation |
| Which elements from therapy did you consider helpful? (each element: yes/no: Resonance Training / Neuroauditive Cortex Training / Tinnitus Reconditioning / Counseling / therapeutic conversation / none) |
| Which elements from therapy do you still perform in your daily life? (each element: yes/no: resonance training/ tinnitus-reconditioning / others / none) |
| Subsequent treatment attempts |
| Which of the following therapies did you undertake since music therapy (each element: yes/no: none / TRT / psychotherapy / inpatient therapy / pharmacological therapy / physiotherapy / hearing aids / sound generator / acupuncture / others) |
| Do you currently use hearing aids (none / one ear / both ears / I own a hearing aid but it is not in use) |
Statistical analysis
Statistical analysis of the data was performed using parametrical and non-parametrical tests in SPSS 19 (SPSS Inc. Headquarters, 233 S. Wacker Drive, 11th floor, Chicago, Illinois 60606). Level of significance was p < .05, adjusted for multiple testing by the Bonferroni method if necessary.
Socio-demographic and otological data
Discrete variables are presented as frequencies and percentages, for continuous variables means and standard deviation are reported. Group differences (responders vs. non-responders) were analyzed using the chi-square test (discrete variables) or by unpaired t-test (continuous variables).
Mini-TQ
The continuous variable Mini-TQ scores was analyzed using univariate analysis of variance (ANOVA) for repeated measures procedures (three assessments: admission, discharge and follow-up) and student’s t-test for dependent samples (post-hoc analysis admission – discharge; admission – follow-up and discharge – follow-up).
In addition Cohen's d’ effect size [42] was calculated to measure the magnitude of the treatment effect.
Apart from the statistical significance, it is important to estimate the clinical impact of therapy outcome. Therefore, individual changes were assessed according to the concept of “clinical significance” [43]. This method allows for calculating a “reliable change index”, i.e. whether the change in questionnaire scores is unlikely to be due to simple measurement unreliability. The formula for criterion level is: RC = 1.96/2*√2*SE (With SE = standard error of the Mini-TQ (SE=SD*√(1- rtt) and SD = 5.3 = standard deviation of the norming sample and rtt = 0.89 [18]). Based on this formula, the RC for the Mini-TQ is estimated to 1.8 score points. Any patient who has scores differing for more than 1.8 points between two measurement points has achieved a clinically relevant change – either a reliable amelioration (reduction by more than 1.8 points) or a reliable deterioration (increase by more than 1.8 points). All patients having scores differing between -1.8 and +1.8 points have not achieved a reliable change in the Mini-TQ.
Data of the four clinical categories are presented as percentages, group differences are calculated by nonparametric statistics (Wilcoxon test).
Follow-up questionnaire
Discrete variables are presented as frequencies and percentages, for continuous variables means and standard deviation are reported.
Group differences between patients attending music therapy only and patients attempting at least one further therapy are presented as frequencies and percentages, the continuous variable Mini-TQ scores was analyzed using univariate analysis of variance (ANOVA) for repeated measures procedures (three assessments: admission, discharge and follow-up).
Factors possibly influencing enduring therapy success
In order to predict parameters possibly influencing therapy outcome, a logistic regression model was calculated using “therapy success” (reliable change in the TQ yes/no) as binary dependent variable and the following variables as independent variables: demographic factors (gender, age), therapy related factors (therapy satisfaction, music therapy only vs. subsequent treatment attempts after music therapy) and tinnitus related factors (initial tinnitus severity in the Mini-TQ), sound quality of the treated tinnitus, frequency, time since onset of tinnitus. We calculated both the regression coefficients and odds ratio. The odds ratio is used to assess the chance (here: therapy success i.e. reliable change) of a particular outcome if a certain factor (or exposure) is present.
Results
Patients
On average the follow-up time was M = 2.65 years (SD = 1.1 years, range: 1.1 – 5.4 years). The detailed otological and psychometric data at admission for all patients who were addressed in the follow-up survey can be seen in Table 3.
Table 3.
Socio-demographic data and Tinnitus-Characteristics
| Variable | Numbers |
|---|---|
| N [all (female)] | 107 (39) |
| Age in years [mean (SD)] | 54.3 (12.4) |
| highest level of education [general school / intermediate school / grammar school / university / others] | 11.2% / 35.7% / 3.1% / 49.0% / 1.0% |
| Occupation [working / homemaker / vocational training / retirement / unemployed / untrained] | 55.9% / 2.7% / 3.5% / 15.1% / 6.2% / 2.7% |
| Initial onset – time in years [mean (SD); Min-Max, Median] | 7.3 (8.3); min 1. max 44. med 4.0 |
| Tinnitus frequency [kHz (SD)] | 6.1 ± 2.5 |
| Tinnitus minimum masking level [dB (SD)] | 52.2 (21.3) |
| Subjective loudness [scale 1-100] | 55.8 (46.6) |
| Sound quality of the tinnitus [sinusoidal / NB / BB] | 56.9% / 24.5% / 18.6% |
| Subjective tinnitus sensation [pure tone / noise] | 80.4% / 19.6% |
| Tinnitus location: N [LE / BE / RE / inside head] | 54.1% / 55.4% / 16.2% / 5.4% |
| Tinnitus changes over time [present all time / sometimes not audible] | 77.3% / 22.7% |
| Sound stimulation devices [Hearing aids / sound generators(noiser, masker, tinnitus instrument)] | 14.1% / 7.8% |
There were no significant differences of demographic variables and tinnitus related problems between those patients who returned the questionnaires and those who did not answer with the exception of age: respondents (M = 51.8 yrs), were significantly older than deniers (M = 47.2 yrs) (t(187) = -2.27, p = .024). Immediate treatment outcome at discharge was identical in both groups (ANOVA interaction time x group: F (1, 187) = .01, p = .921) indicating that the respondents are representative for the sample. From now on, only data by respondents will be reported.
Therapy outcome
In order to measure and to quantify therapy success, Mini-TQ-scores obtained at three different measurement times (admission, discharge and follow-up) were compared by means of parametric (overall TQ-score) and non-parametric (individual changes) statistics.
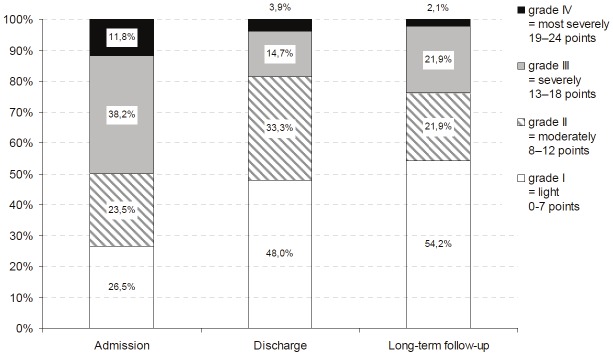
According to the concept of “clinical significance”, 71% of the patients achieved a reliable reduction in their tinnitus scores from admission to discharge, and this proportion of significant improvement increased to 76% at longterm follow-up. Figure 1 depicts individual changes of all patients accordingly.
Figure 1.
Jacobson-Plot of TQ-Scores. The graph depicts individual TQ-scores of each patient at admission and follow-up. All data outside the area between the two diagonal lines in the middle belong to patients with reliable changes, i.e. changes succeed 1.8 points. Scores above the line indicate a reliable deterioration, scores below the lines indicate a reliable bettering, and scores between the lines indicate no reliable change.
The overall tinnitus distress as measured by the Mini-TQ score (see Table 4) diminished from admission to discharge and even improved further until long-term follow-up (ANOVA: F(2, 105) = 39.87, p = .000; post hoc t-tests: admission – discharge t(105) = 13.49; p = .000; admission – follow-up t(105) = 6.18; p = .000, discharge – follow-up t(105) = .14; p = .888). This change corresponds to an effect size of d’ = 0.80 from admission to discharge and to an effect size of d’ = 0.89 from admission to follow-up.
Table 4.
Mini-TQ raw scores (all subjects)
| Admission | Discharge | Long term follow-up | Relative Change Adm – Disc. | Relative Change Adm / FU | ||
|---|---|---|---|---|---|---|
| Value | Respondents (n=107) | 11.9 ± 4.9 | 8.0 ± 4.8 | 7.4 ± 5.2 | 33% | 38% |
| Deniers (n=79) | 11.7 ± 4.5 | 8.0 ± 4.3 | 32% | |||
| ANOVA | ANOVA Main effect time | F[1, 363] = 49.03; p = .000 | ||||
| Main effect “therapy group” | F[1, 363] = 3.98; p = .685 | |||||
| Interaction “time x therapy group” | F[1,363] = 0.08; p = .773 | |||||
As the time elapsed since therapy could be influential on therapy outcome, a correlation between ‘follow-up time [years]’ and ‘change in tinnitus distress [TQ-scores]’ was calculated but revealed no significant connection (r(105)= .15, p = .136) (Figure 3).
Figure 3.
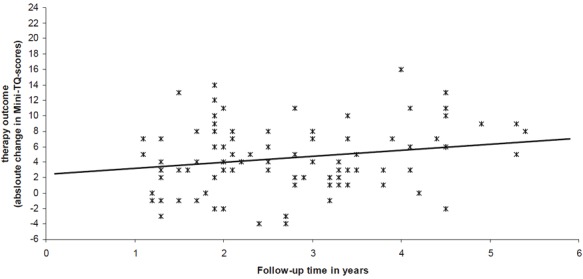
Scatter plot therapy outcome versus elapsed time. Correlation of therapy outcome (change in absolute Mini-TQ scores) versus elapsed time (years since end of therapy).
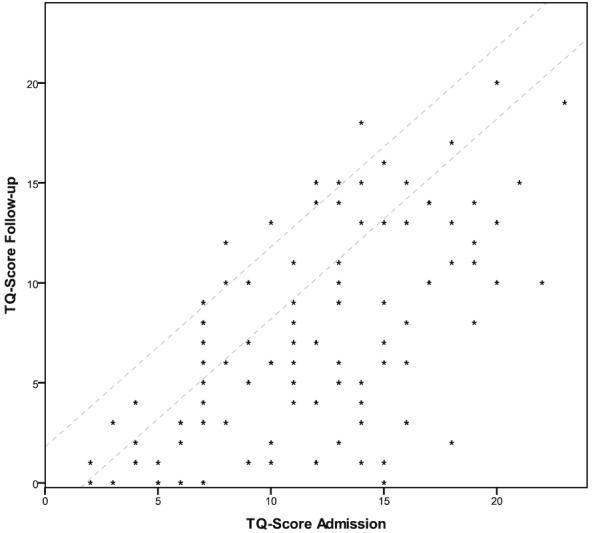
The Mini-TQ allows for the calculation of clinical categories. The distribution of the patients according to the four clinical grades of the TQ is given in Figure 2. The Wilcoxon test reveals a significant shift on the distribution in the four groups from admission to discharge such as the number of slightly distressed patients rose up and the number of severely/ most severely affected patients declined (Z = 6,55, p = .000). This pattern remained stable from discharge to long-term follow-up (Z = .04, p = .967).
Figure 2.
clinical categories of patients according to the Mini-TQ severity grades. Distribution of the patients in the four clinical categories of the Mini-TQ at the different times of data collection.
At follow-up, 71% of the patients said that they still heard their tinnitus all day long, 21% experienced periods without tinnitus and 8% indicated not to perceive their tinnitus any longer.
Therapy satisfaction
Overall, 87% of the patients were “very satisfied” or “satisfied” by the way they were treated during therapy (positive therapist-patient relationship; rating on a fivepoint scale: 4 or 5; M = 4.7, SD = 0.8). 48% were “very satisfied” or “satisfied” with therapy outcome in the long run (rating on a five-point scale: 4 or 5; M = 4.3, SD = 0.4), 42% were undetermined (rating on a five-point scale: 3) and 10% were dissatisfied (rating on a fivepoint scale: 1 or 2; M = 1.5, SD = 0.5). Most prominent were the wish for “more intensive after-care” (84% of the dissatisfied patients) and longer duration or higher number of therapy intervals (37%).
Evaluation of therapeutic elements
As most beneficial the patients specified the therapy elements “Resonance Training” (66% positive feedback), relaxation/reconditioning (61%) and “Neuroauditive Cortex Training” (56%). Pure counselling was not rated as important (only 6% positive feedback). 11% of the patients did not rate any intervention as useful.
Almost three-quarters (73%) of the patients declared to apply one or more of the techniques they had learned during therapy in their daily life: 56% stated to use techniques from “Tinnitus Reconditioning” in order to regulate their physiological state (“relaxation”), 28% said to perform the “Resonance Training” and 13% marked to use other therapy related mechanisms.
Treatment attempts following music therapy
After the music therapy, 71% of the patients did not undergo any further treatment, 12% undertook one further therapy and 15% attempted more than one treatment. The distribution of these subsequent therapies was: physical therapy (41%), sound devices (masker / noisier: 28%), psychotherapy (24%), acupuncture (21%), residential treatment (17%), pharmacological therapy (17%), tinnitus retraining therapy (14%), hearing aids (8%) and others (7%).
A detailed analysis of the two subgroups (music therapy only vs. further treatment) revealed significant group differences (Table 5). Overall both groups did benefit from the therapy (ANOVA main effect group p = .372, main effect time p = .000) though the course of TQ-score changes differed between the two subgroups (significant interaction time x therapy group (p = .043). The two groups did not differ in any moderating variable assessed in the survey (all p > .100) (Figure 3).
Table 5.
Comparison of Mini-TQ raw scores for the subgroups of patients “music therapy only” vs. “further therapy”
| Admission | Discharge | Long term follow-up | Relative Change Adm – Disc | Relative Change Adm / FU | Relative Change Disc / FU | ||
|---|---|---|---|---|---|---|---|
| Value | Music Therapy only (N=76) | 11.8 ± 5.2 | 8.0 ± 5.0 | 6.7 ± 5.1 | 32.1% | 42.9% | 15.8% |
| Further Treatment (N=31) | 12.2 ± 4.3 | 7.9 ± 4.3 | 8.8 ± 5.2 | 35.1% | 27.7% | -11.4% | |
| ANOVA | Main effect “time” | F[2, 210] = 56.85; p = .000 | |||||
| Main effect “therapy group” | F[1, 105] = 0.81; p = .372 | ||||||
| Interaction “time x therapy group” | F[2, 210] = 3.20; p = .043 | ||||||
Factors possibly influencing enduring therapy success
Therapy and tinnitus related factors as well as demographic data were entered into a logistic regression model. Therapy success was defined as reliable change in the Mini-TQ (i.e. more than 1.8 points amelioration from admission to follow-up). The aim was to define possible factors associated with tinnitus which may contribute to a correct classification of patients with longstanding therapy success.
The logistic regression analysis (Table 6) revealed for the demographic factors, that female patients had a fivefold higher chance to benefit from the therapy than male patients (OR: 5.22, p = .021, 95% CI [1.28, 21.21]). Age did not affect therapy outcome.
Table 6.
logistic regression and Odds Ratios predicting therapy outcome (binary variable: therapy success = reliable change in Mini-TQ yes/no)
| Regr. coeff. B | Standard Error | Wald | df | Sig. | OR | 95% CI EXP(B) | ||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| lower | upper | |||||||
| Demographic factors | ||||||||
| Female gender | 1.652 | .716 | 5.332 | 1 | .021 | 5.22 | 1.28 | 21.21 |
| Age (year of birth) | .013 | .026 | .266 | 1 | .606 | 1.01 | 0.96 | 1.07 |
| Therapy related factors | ||||||||
| Therapeutic relationship | .773 | .388 | 3.960 | 1 | .047 | 2.17 | 1.01 | 4.64 |
| Therapy outcome satisfaction | .408 | .322 | 1.610 | 1 | .204 | 1.50 | 0.80 | 2.83 |
| Music therapy only | 1.278 | .623 | 4.203 | 1 | .040 | 3.59 | 1.06 | 12.18 |
| Tinnitus related factors | ||||||||
| Initial tinnitus severity | .663 | .352 | 3.556 | 1 | .059 | 1.94 | 0.97 | 3.86 |
| Mini-TQ | ||||||||
| Frequency | .000 | .000 | .448 | 1 | .503 | 1.00 | 1.000 | 1.00 |
| Minimal Masking Level | -.011 | .019 | .336 | 1 | .562 | .989 | .952 | 1.027 |
| Time since onset of tinnitus | .014 | .037 | .144 | 1 | .704 | 1.01 | 0.94 | 1.09 |
| Sound quality of the tinnitus | .064 | .789 | .006 | 1 | .936 | 1.07 | 0.23 | 5.00 |
In the field of the therapy related factors, a positive therapeutic relationship led to a twofold higher chance of positive therapy outcome (OR: 2.17, p = .047, 95% CI [1.01, 4.64]) whereas the subjective overall treatment satisfaction did not predict the objective therapy success (OR: 1.50, p = .204, 95% CI [0.80, 2.83]). Patients who undertook no further therapy had a 3.6 times higher chance for long lasting tinnitus relief (OR: 3.59, p = .040, 95% CI [1.06, 12.18]).
Tinnitus related factors played a minor role: Neither tinnitus frequency nor the time since the initial onset of tinnitus nor the subjective sound quality of the treated tinnitus had any impact (all OR near 1.0, p > .5), only the initial tinnitus severity predicted by trend a twofold higher chance for tinnitus relief (OR: 1.94, p = .059, 95% CI [0.97, 3.86]).
Discussion
Tinnitus is a very common symptom, yet difficult to treat. Therefore there is an urge for a short term therapy with preferably minimal effort but long lasting effect. The proposed therapy concept “Heidelberg Model of Music Therapy for Chronic Tinnitus” seems to be a potential completion of the therapy spectrum. This model of music therapy previously has proven to be a very efficient treatment option in chronic tinnitus immediately after therapy and shortly afterwards (six months follow-up) [13]. The present survey could find evidence for long term therapy impact up to 5.4 years after end of therapy.
Therapy outcome
The improvement in tinnitus distress achieved during therapy remained stable until follow-up and the corresponding effect size of d’ = 0.89 from admission to follow-up was substantial compared to therapeutic effects found in other studies (Table 7).
Table 7.
Effect sizes of long-term trials on tinnitus treatment
| Author | Therapy Type | Evaluation | FU-Time | N | ES |
|---|---|---|---|---|---|
| Folmer et al. 2000 | CBT | TSI | 22 months | 190 | 0.46 |
| Andersson et al. 2002 | CBT | TRQ | 4,9 years | 146 | No Baseline data |
| Goebel et al. 2006 | CBT | TQ | 15 years | 244 | 0.46 |
| Henry et al. 2006 | TRT | THI | 18 months | 53 | 1.56 |
| Caffier et al. 2006 | TRT | TQ | 24 months | 40 | 0.91 |
| Baracca et al. 2007 | TRT | VAS | 18 months | 51 | No validated outcome measure |
| Forti et al. 2009 | TRT | THI | 18 months | 45 | No data available |
Therapy Type: CBT = Cognitive Behavioral Therapy, TRT = Tinnitus Retraining Therapy; Evaluation (outcome measurement): TSI = Tinnitus Severity Index (Meikle et al. 1995), TRQ = Tinnitus Reaction Questionnaire (Wilson et al. 1991), TQ = Tinnitus Questionnaire (Goebel & Hiller, 1998), THI = Tinnitus Handicap Inventory (Newman et al. 1996); FU = Follow-up time; N = Number of participants, ES = effect size according to Cohen’s d’.
Though most patients still perceive their tinnitus – either constantly or intermittently – about three-quarters of the patients accomplished a reliable decrease of Mini-TQ scores from admission to follow-up as revealed by the scores in the “Tinnitus Questionnaire” (TQ, [17]).
In order to set the results in the context of existing therapies, the outcome of the Heidelberg model should be compared to other studies evaluating long-term impact of tinnitus treatments. For this purpose, effect sizes for long-term trials on CBT and TRT were calculated. Unfortunately it was impossible to obtain reliable data. For three out of seven trials no effect size could be computed due to missing or insufficient data. The remaining trials report enough data to calculate effect sizes but since the authors used a wide range of tinnitus outcome measurements (TQ [28], THI [44], TSI [45]) incorporating each a different notion on tinnitus symptoms, the results are rather incommensurable – a problem common to tinnitus research ([46,47]).
Unaccounted for these flaws, an effect size of d’ = 0.89 as achieved by the Heidelberg Model, can be accounted for as “large” effect and falls into the upper range value compared to established treatments.
Therapy satisfaction
The ratings of therapy satisfaction revealed a rather high level of satisfaction, especially due to a positive working alliance. Therapeutic relationship is a common factor in all psychotherapeutic settings and contributes to up to 30 percent of improvement in psychotherapy [48]. Thus it is not surprising that those patients, who did state a good relationship, had a higher chance of lower Mini-TQ scores in the long run.
Evaluation of therapeutic elements
Compared to other treatments with long-term impact evaluation, the “Heidelberg Model of Music Therapy for Chronic Tinnitus” has some distinctive features and follows the notion of “neuropsychotherapy” [49]. According to current etiological findings focusing on neuronal reorganization [50], this treatment aims at a reorganization of the underlying neurophysiologic sources leading to the tinnitus symptoms [51]. The music therapeutic interventions convey an increased ability for attention guidance and a diminished interference by the internal tinnitus distraction. In doing so this therapy is very short in duration: only nine sessions, provided within one week, are sufficient for lasting tinnitus relief. From the patients’ point of view, only the therapy modules which were specific for the music therapy concept – “Resonance Training”, “Neuroauditive Cortex Training”, “Tinnitus Reconditioning” – were rated as helpful and maintained by a majority of patients throughout the follow-up period. Only a marginal proportion of the patients considered general interventions, such as a counseling as helpful. These results justify the higher manpower requirements (two trained therapists) for this model of music therapy compared to conventional psychological or otological treatments.
Treatment attempts succeeding music therapy
About 70% of the patients did not undertake any further therapies after music therapy – an effect especially noteworthy in the realm of tinnitus patients who are known for their frequent healthcare utilization (colloquially called “doctor-hopping”) [52].
Interestingly, performance during the immediate therapy phase of the patients who attended music therapy only and those who attempted at least one further therapy afterwards was statistically undistinguishable. Patients with “music therapy only” had however the greatest impact in the aftermath of the music therapy (amelioration from discharge to follow-up by about 16% in TQ-scores) while the patients with further therapy attempts forfeit their initially equally positive outcome (deterioration by about 11% in TQ-scores from discharge to follow-up). The reasons for this pattern can be but speculation since the two groups did not differ in any moderating variable assessed in the survey (such as age and gender, time since tinnitus onset, time elapsed since therapy, tinnitus pitch, tinnitus loudness, tinnitus localisation, therapist relationship, subjective therapy evaluation) and should be subject for future research.
Factors possibly influencing enduring therapy success
The observed reduction Mini-TQ-scores was mainly independent of tinnitus related factors such as initial tinnitus frequency, minimal masking level, time since onset of tinnitus or sound quality of the tinnitus. Solely a higher initial tinnitus severity increased the chance of greater tinnitus relief, though it is not surprising that tinnitus severity is somehow predictive of reliable change, since a minimum severity/TQ score is needed to make a reliable change possible in the first place.
As far as demographic data are concerned, age did not influence therapy outcome. “Gender” turned out to be a moderating factor. Female patients were generally better off than male patients even if the rather large confidence interval (CI) suggests, that some male patients achieved the largest reduction in TQ scores and some female patients the worst. The current state of research on gender specific treatment outcome in tinnitus is rather weak, but some studies support this somewhat puzzling result. It is known from both general psychotherapy and psychological tinnitus therapy, that women have higher response rates in short term therapy than men [53-55]. Furthermore, men are at a much higher risk to develop tinnitus in the first place [56] and often suffer from more profound hearing loss than age-matched female patients [57]. Consequently it might be more difficult to eliminate the symptoms in male patients.
In the realm of therapy related factors, a good therapeutic relationship doubled the chance for positive therapy outcome. One distinctive feature of music therapy is its comprehensive support leading to this positive relationship.
The numbers of therapies following music therapy was highly influential on therapy outcome. Patients who attended music therapy only had a three times higher change for lasting therapy success – or conversely multiple therapy attempts after the music therapy trebled the risk for outlasting tinnitus distress. Since the two variables are but correlated, there is no causal connection. Possible explanations might be that more heavily distressed patients strive for multiple treatments independent pre se or the higher number of treatments implies a lower chance for therapy impact for example due to a lack of therapy collaboration of those “doctor hoppers”. A detailed analysis of patients attending music therapy only and patients who attempted at least one further therapy reveals that both the initial tinnitus distress and the immediate therapy outcome are identical. Only in the long run the TQ-scores differ. Therefore it seems reasonable to favour hypothesis two.
Generally, the reviewed moderating factors present only a limited view on possible influencing aspects. It is a problem common to follow-up studied to prove a causal relationship between a treatment and long term outcome due to a huge variety of intervening variables [58]. Natural maturation and developmental processes can produce considerable change independently of the therapeutic effects. Furthermore, interfering events such as changes in lifestyle (e.g. relocation, divorce, marriage) or occupational environment (e.g. job change, reduction in working ours) and a generally increased concern for health (e.g. more healthy diets, less noise exposure in leisure and workplace) [13] could influence the progress of tinnitus symptoms. Nevertheless, there is no known significant habituation mechanism in (decompensated) tinnitus due to mere time elapsed [59]. Even if patients are on a waiting list for treatment, the reduction of their symptoms is rather modest [60]. Furthermore, therapy outcome of those patients who attended music therapy only was more prosperous in the long run than of those who tried other treatments after music therapy. Therefore we conclude that - for the most part - the positive effects our patients reported have their proximate cause in the therapy impact.
Limitations of the therapy
One limitation of the music therapy is that it is but suitable for a subgroup of tinnitus sufferers: The musical exercises will only be tolerated if the patients do not present severe hyperacusis and/or hearing loss > 50dB – though hyperacusis and hearing loss are very common symptoms in tinnitus [61]. Although the treatment of tinnitus related psychological distress is part of the music therapy concept, the music therapy is very short in duration and presents a focal therapy and no in depth psychotherapy will be possible. Therefore, patients are not eligible if they suffer from psychiatric co-morbidities (esp. depression or anxiety).
Suggestions for therapy improvements
It is a known factor that malingering and secondary gain are common in chronic diseases which are difficult to diagnose as is a considerable “disease memory” [59]. We therefore conclude that the patients might not be able to differentiate between an actual symptom, their reminiscence and the unconscious wish to retain a mild form of symptom – consequently they do not dare to admit that a symptom has completely vanished since they are in need for the symptom.
Data from neuroimaging would be highly desirable in order to clear up this point. In terms of therapy interventions, more importance should be attached to extinct the “tinnitus memory”. Some approaches are under way, such as including biofeedback mechanisms in the receptive part of music therapy in order to strengthen the objective influence on tinnitus symptoms.
Suggestions for more sophisticated outcome measurements
Outcome measurements were – apart from a validated questionnaire, the Mini-TQ –a variety of single items in order to evaluate treatment outcome in the long run. Results of single item questions have to be taken with a pinch of salt and are only meaningful in the context of a more sophisticated evaluation such as validated questionnaires (here: Mini-TQ). Another possible source of information would be audiometric data. We could assess the audiometric status only once, at admission. Since the patients in our survey came from all over Germany and were not participants of a clinical trial, no personal in-patient contact was possible at followup, therefore no additional data could be obtained. We suggest these lines of measurement for any further trials.
Suggestions for further trials
Future studies should most notably include a control group treated with a conventional therapy such as TRT or CBT in order to rule out common factors and to refine the impact of the “Heidelberg Model” of music therapy.
Conclusion
On the whole, the “Heidelberg Model of Music Therapy for Chronic Tinnitus” appears to be a method with fast onset and possibly long lasting impact for patients with chronic tinnitus. Whether the results from this survey are stable, has to be proven in further more sophisticated research.
References
- 1.Heller AJ. Classification and epidemiology of tinnitus. Otolaryngol. Clin North Am. 2003;36:239–248. doi: 10.1016/s0030-6665(02)00160-3. [DOI] [PubMed] [Google Scholar]
- 2.Møller AR, editor. Tinnitus: Diagnosis and treatment. London: Springer; 2010. [Google Scholar]
- 3.Goodey R. Management of Tinnitus – Introduction. In: Møller AR, editor. Tinnitus: Diagnosis and treatment. London: Springer; 2010. pp. 523–252. [Google Scholar]
- 4.Hiller W, Goebel G. When tinnitus loudness and annoyance are discrepant: audiological characteristics and psychological profile. Audiol Neurootol. 2007;12:391–400. doi: 10.1159/000106482. [DOI] [PubMed] [Google Scholar]
- 5.Vanneste S, Plazier M, van der Loo E, van Heyning P de, Congedo M, Ridder D de. The neural correlates of tinnitus-related distress. Neuroimage. 2010;52:470–480. doi: 10.1016/j.neuroimage.2010.04.029. [DOI] [PubMed] [Google Scholar]
- 6.Melcher JR, Knudson IM, Levine RA. Subcallosal brain structure: Correlation with hearing threshold at supra-clinical frequencies (8 kHz), but not with tinnitus. Hearing research. 2012 doi: 10.1016/j.heares.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 7.Noreña AJ. An integrative model of tinnitus based on a central gain controlling neural sensitivity. Neurosci Biobehav Rev. 2011;35:1089–1109. doi: 10.1016/j.neubiorev.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 8.Rauschecker JP, Leaver AM, Mühlau M. Tuning out the noise: limbic-auditory interactions in tinnitus. Neuron. 2010;66:819–826. doi: 10.1016/j.neuron.2010.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoare DJ, Kowalkowski VL, Hall DA. Effects of frequency discrimination training on tinnitus: results from two randomised controlled trials. J Assoc Res Otolaryngol. 2012;13:543–559. doi: 10.1007/s10162-012-0323-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hobson J, Chisholm E, El Refaie A. Sound therapy (masking) in the management of tinnitus in adults. Cochrane Database Syst Rev. 2010:CD006371. doi: 10.1002/14651858.CD006371.pub2. [DOI] [PubMed] [Google Scholar]
- 11.Martinez Devesa P, Waddell A, Perera R, Theodoulou M. Cognitive behavioural therapy for tinnitus. Cochrane Database Syst Rev. 2007:CD005233. doi: 10.1002/14651858.CD005233.pub3. [DOI] [PubMed] [Google Scholar]
- 12.Phillips JS, McFerran D. Tinnitus Retraining Therapy (TRT) for tinnitus. Cochrane Database Syst Rev. 2010:CD007330. doi: 10.1002/14651858.CD007330.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Folmer RL. Long-term reductions in tinnitus severity. BMC Ear Nose Throat Disord. 2002;2:3. doi: 10.1186/1472-6815-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Andersson G, Vretblad P, Larsen HC, Lyttkens L. Longitudinal follow-up of tinnitus complaints. Arch Otolaryngol Head Neck Surg. 2001;127:175–179. doi: 10.1001/archotol.127.2.175. [DOI] [PubMed] [Google Scholar]
- 15.Bessman P, Heider T, Watten VP, Watten RG. The tinnitus intensive therapy habituation program: a 2-year follow-up pilot study on subjective tinnitus. Rehabil Psychol. 2009;54:133–137. doi: 10.1037/a0015660. [DOI] [PubMed] [Google Scholar]
- 16.Goebel G, Kahl M, Arnold W, Fichter M. 15-year prospective follow-up study of behavioral therapy in a large sample of inpatients with chronic tinnitus. Acta Otolaryngol. 2006:70–79. doi: 10.1080/03655230600895267. [DOI] [PubMed] [Google Scholar]
- 17.Henry JA, Schechter MA, Zaugg TL, Griest S, Jastreboff PJ, Vernon JA, Kaelin C, Meikle MB, Lyons KS, Stewart BJ. Clinical trial to compare tinnitus masking and tinnitus retraining therapy. Acta Otolaryngol. 2006:64–69. doi: 10.1080/03655230600895556. [DOI] [PubMed] [Google Scholar]
- 18.Caffier PP, Haupt H, Scherer H, Mazurek B. Outcomes of long-term outpatient tinnitus-coping therapy: psychometric changes and value of tinnitus-control instruments. Ear Hear. 2006;27:619–627. doi: 10.1097/01.aud.0000240504.77861.1a. [DOI] [PubMed] [Google Scholar]
- 19.Baracca GN, Forti S, Crocetti A, Fagnani E, Scotti A, Del Bo L, Ambrosetti U. Results of TRT after eighteen months: our experience. Int J Audiol. 2007;46:217–222. doi: 10.1080/14992020601175945. [DOI] [PubMed] [Google Scholar]
- 20.Forti S, Costanzo S, Crocetti A, Pignataro L, Del Bo L, Ambrosetti U. Are results of tinnitus retraining therapy maintained over time? 18-month follow-up after completion of therapy. Audiol Neurootol. 2009;14:286–289. doi: 10.1159/000212106. [DOI] [PubMed] [Google Scholar]
- 21.Graul J, Klinger R, Greimel KV, Rustenbach S, Nutzinger DO. Differential outcome of a multimodal cognitive-behavioral inpatient treatment for patients with chronic decompensated tinnitus. Int Tinnitus J. 2008;14:73–81. [PubMed] [Google Scholar]
- 22.Pilgramm M, Lebisch H, Pehle W. Das ambulante Tinnitusbewältigungs- und Hyperakusis-training [Outpatient tinnitus management and hyperacusis training] . HNO. 2012;60:545–556. doi: 10.1007/s00106-012-2493-2. [DOI] [PubMed] [Google Scholar]
- 23.Hesser H, Weise C, Westin VZ, Andersson G. A systematic review and meta-analysis of randomized controlled trials of cognitive-behavioral therapy for tinnitus distress. Clin Psychol Rev. 2011;31:545–553. doi: 10.1016/j.cpr.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 24.Møller AR. Neural plasticity in tinnitus. Prog Brain Res. 2006;157:365–372. doi: 10.1016/S0079-6123(06)57022-0. [DOI] [PubMed] [Google Scholar]
- 25.Argstatter H, Krick C, Bolay HV. Musiktherapie bei chronisch-tonalem Tinnitus. Heidelberger Modell evidenzbasierter Musiktherapie. HNO. 2008;56:678–685. doi: 10.1007/s00106-008-1722-1. [DOI] [PubMed] [Google Scholar]
- 26.Argstatter H, Krick C, Plinkert P, Bolay HV. Musiktherapie bei nichttonalem Tinnitus (Tinnitusrauschen). Konzeptentwicklung und Behandlungsevaluation. HNO. 2010;58:1085–1093. doi: 10.1007/s00106-010-2113-y. [DOI] [PubMed] [Google Scholar]
- 27.Nickel AK, Hillecke T, Argstatter H, Bolay HV. Outcome research in music therapy: a step on the long road to an evidence-based treatment. Ann N Y Acad Sci. 2005;1060:283–293. doi: 10.1196/annals.1360.021. [DOI] [PubMed] [Google Scholar]
- 28.Goebel G, Hiller W. Tinnitus-Fragebogen: (TF); ein Instrument zur Erfassung von Belastung und Schweregrad bei Tinnitus; Handanweisung. Göttingen: Hogrefe Verl; 1998. für Psychologie. [Google Scholar]
- 29.Argstatter H. Heidelberger Musiktherapiemanual: chronisch-tonaler Tinnitus. Berlin: Uni-Ed; 2009. [Google Scholar]
- 30.Mair & Rohner OEG. Arbitrary Waveform Gene rator WG820. http://www2.produktinfo.conrad.com/datenblaetter/100000-124999/120056-an-01-en-Signalgenerator_WG_820.pdf. Accessed 24 July 2012 . [Google Scholar]
- 31.Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. Am Fam Physician. 2002;65:653–660. [PubMed] [Google Scholar]
- 32.Mühlnickel W, Elbert T, Taub E, Flor H. Reorganization of auditory cortex in tinnitus. Proc Natl Acad Sci USA. 1998;95:10340–10343. doi: 10.1073/pnas.95.17.10340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eggermont JJ. Cortical tonotopic map reorganization and its implications for treatment of tinnitus. Acta Otolaryngol. 2006:9–12. doi: 10.1080/03655230600895259. [DOI] [PubMed] [Google Scholar]
- 34.Flor H, Hoffmann D, Struve M, Diesch E. Auditory discrimination training for the treatment of tinnitus. Appl Psychophysiol Biofeedback. 2004;29:113–120. doi: 10.1023/b:apbi.0000026637.77671.f4. [DOI] [PubMed] [Google Scholar]
- 35.Herraiz C, Diges I, Cobo P, Aparicio JM, Toledano A. Auditory discrimination training for tinnitus treatment: the effect of different paradigms. Eur Arch Otorhinolaryngol. 2010;267:1067–1074. doi: 10.1007/s00405-009-1182-6. [DOI] [PubMed] [Google Scholar]
- 36.Pantev C, Okamoto H, Teismann H. Music-induced cortical plasticity and lateral inhibition in the human auditory cortex as foundations for tonal tinnitus treatment. Frontiers in systems neuroscience. 2012;6:50. doi: 10.3389/fnsys.2012.00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bolay HV, Selle EW. Entspannungstraining nach musiktherapeutischen Gesichtspunkten, Trainerhandbuch. Schweinfurt: Neues Forum; 1984. [Google Scholar]
- 38.Deutsche Gesellschaft für Hals-Nasen-Ohren-Heilkunde KHeV. Leitlinie "Tinnitus. 2011. http://www.awmf.org/uploads/tx_szleitlinien/017-064l_S1_Tinnitus.pdf. Accessed 15 June 2012. . [Google Scholar]
- 39.Hiller W, Goebel G. Rapid assessment of tinnitus-related psychological distress using the Mini-TQ. Int J Audiol. 2004;43:600–604. doi: 10.1080/14992020400050077. [DOI] [PubMed] [Google Scholar]
- 40.Goebel G, Hiller W. STI: Strukturiertes Tinnitus-Interview. Göttingen [u.a.]: Hogrefe; 2001. [Google Scholar]
- 41.Langguth B. A review of tinnitus symptoms beyond 'ringing in the ears': a call to action. Curr Med Res Opin. 2011;27:1635–1643. doi: 10.1185/03007995.2011.595781. [DOI] [PubMed] [Google Scholar]
- 42.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 43.Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- 44.Newman CW, Jacobson GP, Spitzer JB. Development of the Tinnitus Handicap Inventory. Arch Otolaryngol Head Neck Surg. 1996;122:143–148. doi: 10.1001/archotol.1996.01890140029007. [DOI] [PubMed] [Google Scholar]
- 45.Meikle MB, Griest SE, Stewart BJ, Press LS. Measuring the negative impact of tinnitus: A brief severity index. Abstr MidWinter Res Meet Assoc Res Otolaryngol. 1995:167. [Google Scholar]
- 46.Langguth B, Goodey R, Azevedo A, Bjorne A, Cacace A, Crocetti A et al. Consensus for tinnitus patient assessment and treatment outcome measurement: Tinnitus Research Initiative meeting, Regensburg, July 2006. Prog Brain Res. 2007;166:525–536. doi: 10.1016/S0079-6123(07)66050-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Langguth B, Searchfield GD, Biesinger E, Greimel KV. History and Questionnaires. In: Møller AR, editor. Tinnitus: Diagnosis and treatment. London: Springer; 2010. pp. 387–404. [Google Scholar]
- 48.Ardito RB, Rabellino D. Therapeutic alliance and outcome of psychotherapy: historical excursus, measurements, and prospects for research. Front Psychol. 2011;2:270. doi: 10.3389/fpsyg.2011.00270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Walter H, Berger M, Schnell K. Neuropsychotherapy: conceptual, empirical and neuroethical issues. Eur Arch Psychiatry Clin Neurosci. 2009;259(Suppl 2):S173–82. doi: 10.1007/s00406-009-0058-5. [DOI] [PubMed] [Google Scholar]
- 50.Adjamian P, Sereda M, Hall DA. The mechanisms of tinnitus: perspectives from human functional neuroimaging. Hear Res. 2009;253:15–31. doi: 10.1016/j.heares.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 51.Low YF, Argstatter H, Bolay HV, Strauss DJ. Evaluation of a compact tinnitus therapy by electrophysiological tinnitus decompensation measures. Conf Proc IEEE Eng Med Biol Soc. 2008;2008:5132–5135. doi: 10.1109/IEMBS.2008.4650369. [DOI] [PubMed] [Google Scholar]
- 52.Bleichhardt G, Timmer B, Rief W. Cognitive-behavioural therapy for patients with multiple somatoform symptoms--a randomised controlled trial in tertiary care. J Psychosom Res. 2004;56:449–454. doi: 10.1016/S0022-3999(03)00630-5. [DOI] [PubMed] [Google Scholar]
- 53.Clarkin JF, Levy KN. The Influence of Client Variables on Psychotherapy. In: Bergin AE, Lambert M, Garfield SL, editors. Bergin and Garfield's handbook of psychotherapy and behavior change. pp. 194–226. [Google Scholar]
- 54.El Refaie A, Davis A, Kayan A, Baskill J, Lovell E, Owen V. A questionnaire study of the quality of life and quality of family life of individuals complaining of tinnitus pre- and post-attendance at a tinnitus clinic. Int J Audiol. 2004;43:410–416. doi: 10.1080/14992020400050052. [DOI] [PubMed] [Google Scholar]
- 55.Seydel C, Haupt H, Szczepek AJ, Klapp BF, Mazurek B. Long-term improvement in tinnitus after modified tinnitus retraining therapy enhanced by a variety of psychological approaches. Audiol Neurootol. 2010;15:69–80. doi: 10.1159/000231632. [DOI] [PubMed] [Google Scholar]
- 56.Bartels H, Middel B, Pedersen SS, Staal MJ, Albers FWJ. The distressed (Type D) personality is independently associated with tinnitus: a case-control study. Psychosomatics. 2010;51:29–38. doi: 10.1176/appi.psy.51.1.29. [DOI] [PubMed] [Google Scholar]
- 57.Møller AR. Epidemiology of Tinnitus in Adults. In: Møller AR, editor. Tinnitus: Diagnosis and treatment. London: Springer; 2010. pp. 29–37. [Google Scholar]
- 58.Rossi PH, Lipsey MW, Freeman HE. Evaluation: A systematic approach. 7th ed. Thousand Oaks, London, New Delhi, Sage, 2005, cop; 2004. [Google Scholar]
- 59.Zenner HP, Pfister M, Birbaumer N. Tinnitus sensitization: Sensory and psychophysiological aspects of a new pathway of acquired centralization of chronic tinnitus. Otol Neurotol. 2006;27:1054–1063. doi: 10.1097/01.mao.0000231604.64079.77. [DOI] [PubMed] [Google Scholar]
- 60.Hesser H, Weise C, Rief W, Andersson G. The effect of waiting: A meta-analysis of wait-list control groups in trials for tinnitus distress. J Psychosom Res. 2011;70:378–384. doi: 10.1016/j.jpsychores.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 61.Nelson JJ, Chen K. The relationship of tinnitus, hyperacusis, and hearing loss. Ear Nose Throat J. 2004;83:472–476. [PubMed] [Google Scholar]