Summary
Background
There is little information on country trends in the complete distributions of children's anthropometric status, which are needed to assess all levels of mild to severe undernutrition. We aimed to estimate trends in the distributions of children's anthropometric status and assess progress towards the Millennium Development Goal 1 (MDG 1) target of halving the prevalence of weight-for-age Z score (WAZ) below −2 between 1990 and 2015 or reaching a prevalence of 2·3% or lower.
Methods
We collated population-representative data on height-for-age Z score (HAZ) and WAZ calculated with the 2006 WHO child growth standards. Our data sources were health and nutrition surveys, summary statistics from the WHO Global Database on Child Growth and Malnutrition, and summary statistics from reports of other national and international agencies. We used a Bayesian hierarchical mixture model to estimate Z-score distributions. We quantified the uncertainty of our estimates, assessed their validity, compared their performance to alternative models, and assessed sensitivity to key modelling choices.
Findings
In developing countries, mean HAZ improved from −1·86 (95% uncertainty interval −2·01 to −1·72) in 1985 to −1·16 (–1·29 to −1·04) in 2011; mean WAZ improved from −1·31 (–1·41 to −1·20) to −0·84 (–0·93 to −0·74). Over this period, prevalences of moderate-and-severe stunting declined from 47·2% (44·0 to 50·3) to 29·9% (27·1 to 32·9) and underweight from 30·1% (26·7 to 33·3) to 19·4% (16·5 to 22·2). The largest absolute improvements were in Asia and the largest relative reductions in prevalence in southern and tropical Latin America. Anthropometric status worsened in sub-Saharan Africa until the late 1990s and improved thereafter. In 2011, 314 (296 to 331) million children younger than 5 years were mildly, moderately, or severely stunted and 258 (240 to 274) million were mildly, moderately, or severely underweight. Developing countries as a whole have less than a 5% chance of meeting the MDG 1 target; but 61 of these 141 countries have a 50–100% chance.
Interpretation
Macroeconomic shocks, structural adjustment, and trade policy reforms in the 1980s and 1990s might have been responsible for worsening child nutritional status in sub-Saharan Africa. Further progress in the improvement of children's growth and nutrition needs equitable economic growth and investment in pro-poor food and primary care programmes, especially relevant in the context of the global economic crisis.
Funding
The Bill & Melinda Gates Foundation and the UK Medical Research Council.
Introduction
Restricted growth as a result of infections and inadequate nutrition, measured by anthropometric status, is an important cause of morbidity and mortality in infants and children.1–3 The proportion of children younger than 5 years who are underweight is also an indicator for the Millennium Development Goal 1 (MDG 1).
There have been estimates of stunting, underweight, and wasting prevalence by country at a single point in time2 and trends in prevalence by region,4–7 but trends by country have not been quantified. Further, previous analyses did not incorporate non-linear trends, which might happen in periods of economic growth or contraction or because of new interventions—eg, those resulting from the MDGs. Previous analyses did not assess the complete distributions of anthropometric indicators, even though the hazardous effects of undernutrition happen along a continuum of mild, moderate, and severe undernutrition.2,8 Without data on distributions, we also cannot assess whether changes in prevalence are due to a shift in the whole distribution—eg, as a result of overall economic and nutritional improvements—or because of interventions targeting high-risk groups.
Country-level information on trends is needed for analysis of progress towards MDG 1, and for priority setting, planning, and policy and programme evaluation; for example, those related to the Scaling-Up Nutrition initiative. We aimed to estimate trends in the complete distributions of anthropometric indicators of child nutrition by country and to assess countries' progress towards MDG 1.
Methods
Study design
We estimated trends, and their uncertainties, between 1985 and 2011 in the distributions of height-for-age and weight-for-age Z scores (HAZ and WAZ) for children younger than 5 years in 141 developing countries. We organised the countries into seven regions (appendix p 14) on the basis of the reporting regions of the Global Burden of Diseases, Injuries, and Risk Factors 2010 study.9 We calculated Z scores with the 2006 WHO child-growth standards, which are based on a multicountry study of child growth potential.10
We do not report weight-for-height Z scores because, although some chronic wasting exists, weight for height is commonly affected by acute economic, environmental, and political factors. These short-term changes are of particular programmatic interest but are empirically indistinguishable from variations due to study design and implementation problems that are smoothed out in trend analysis. Possibly for this reason, previous regional analyses reported trends in stunting and underweight, but reported wasting for a single year.4–7
Our analysis comprised four steps: identifying data sources, and accessing and extracting data; converting data that were based on the 1977 US Centers for Disease Control and Prevention National Center for Health Statistics (NCHS)/WHO reference population to 2006 WHO standards; applying a statistical model to estimate trends in Z-score distributions and their uncertainties; and assessing the external predictive validity of the estimates and their sensitivity to key modelling choices.
The distributions we estimated in the third step provide coherent estimates of mean HAZ or WAZ, and of the prevalence of children whose HAZ or WAZ is below −1, −2, or −3 (ie, more than 1, 2, or 3 SDs below the WHO standards' median); these thresholds are commonly used to define mild, moderate, and severe stunting or underweight.
Data sources
We designed our data search and access strategy to obtain as many population-based sources as possible while ensuring representativeness, quality, and comparability of measurements. Estimating the complete distributions without overly restrictive assumptions requires as many sources as possible to provide individual records that characterise distributions. The details of our data search and access are provided in the appendix (pp 1–3). In brief, our data sources were health examination, nutrition, and household surveys with anonymised individual records available through national and international agencies and through survey databases; summary statistics, including mean and prevalences below specific thresholds, from the WHO Global Database on Child Growth and Malnutrition;11 and summary statistics not in the WHO database, extracted from reports of national and international agencies. Inclusion criteria are listed in the appendix (pp 1–3).
Statistical analysis
When individual-level data were accessible, we calculated Z scores with the WHO standards. Some data, especially from older sources, were available to us only as summary statistics in relation to the NCHS reference. To use a consistent reference population, we converted these summary statistics from the NCHS reference to the WHO standards as described in the appendix (p 4).
We aimed to estimate the complete distributions of HAZ and WAZ, which would then allow us to calculate any summary statistic. After calculating Z scores based on sex-specific growth standards, we pooled data from boys and girls because they tracked closely (appendix p 86) and because some sources did not separate data by sex. We did all analyses separately for HAZ and WAZ.
Many country-years had no data or no nationally representative data. Further, some sources reported one or more summary statistics but did not provide individual-level records. We applied a statistical model to estimate Z-score distributions by country and year with a combination of individual-level and summarised data. We used a Bayesian hierarchical mixture model, which is ideal for analysing distributions.12–15 We describe the model in the appendix (pp 6–9) and summarise it below.
The model uses a mixture (ie, a weighted-average) of multiple normal (bell shaped) densities to characterise the full Z-score distributions, and can characterise distributions that are not normal. We used a mixture of five normal distributions in our main analysis (in the appendix [pp 6–11, 53] we provide the reasons for and the sensitivity of results to this choice). The mixture model used individual-level data, when available, to fully inform distributions. Summary statistics also provided information on the distribution, especially when multiple summary statistics were available.
Z-score distributions and their trends for countries were nested in regional and global levels and trends. Estimates for each country-year were informed by data from that country-year itself, if available, and by data from other years in the same country and in other countries, especially those in the same region with data in similar periods. The hierarchical model borrows information to a greater degree where data are non-existent or weakly informative (ie, have large uncertainty), and a lesser degree in data-rich countries and regions.
We modelled trends over time as a linear trend plus a smooth non-linear trend, at the country, regional, and global levels. We also used time-varying country-level covariates to inform the estimates. The covariates were maternal education,16 national income (natural logarithm of per-person gross domestic product in inflation-adjusted international dollars), urbanisation (proportion of population that lived in urban areas), and an aggregate metric of access to basic health care.17 To reduce the effect of interannual fluctuations, we used a weighted average of gross domestic product and urbanisation over the past 5 years, with progressively smaller weights in the more distant past. We assessed how covariates affected our estimates and whether they improved the estimates, as described in the appendix (pp 10, 11, 47, 48, 53).
Nationally representative sources have errors larger than their sampling error, illustrated by the differences between two nationally representative surveys in the same or adjacent years (appendix pp 90–231), due to factors related to study design (eg, absence of a reliable recent sample frame) or implementation (eg, errors in measuring weight, height, and age). To account for this, our model included a non-sampling error term for national data, estimated empirically. Further, subnational data can have additional variation because of subgroup variability. Our model included an added variance component for subnational data, also estimated empirically. This additional variance allowed us to include subnational data but for them to have less effect on estimates than national data.
Some studies did not cover the full 0–59 month age range: of the 125 such studies, 55 (44%) covered an age range of at least 4·5 years, 14 (11%) 4·0–4·5 years, and another 43 (34%) 3·0–4·0 years. Because WAZ and HAZ distributions change with age,18 such sources have an additional error, which we accounted for by an additional variance component in our model.
The uncertainties of our estimates included uncertainty due to sampling uncertainty in each data source; uncertainty associated with non-sampling error of national data; additional uncertainty associated with subnational data and with sources that did not cover 0–59 months; uncertainty due to converting from NCHS reference to WHO standards; and uncertainty due to making estimates by country and year when data were missing altogether or when only summary statistics (vs individual-level data) were available.
We fitted the Bayesian model with a Markov chain Monte Carlo algorithm, as detailed in the appendix (pp 6–9), and obtained 5000 samples from the parameters' posterior, in turn used to obtain 5000 posterior Z-score distributions for each country-year. We used the distributions to calculate 5000 means and prevalences. All reported uncertainty intervals represent the 2·5–97·5th percentiles of these 5000 draws. We calculated distributions for regions and the world as population-weighted averages of the constituent country estimates.
We estimated changes in mean or prevalence as a linear trend (absolute for mean and proportional for prevalence) over the 26 years of analysis and reported as change per decade; we also made separate trend estimates for the pre-2000 and post-2000 years because 2000 marks the adoption of the MDGs and an increase in development assistance for health. We report the posterior probability (PP) that an estimated increase or decrease represents a truly increasing or decreasing trend. We calculated the PP that countries and regions would meet the MDG 1 target of halving the prevalence of WAZ below −2 between 1990 and 2015 or reaching a prevalence of 2·3% or lower, as we would expect in a well nourished population, if the post-2000 linear trends continue.
We assessed the external predictive validity of our estimates, including comparison with alternative models, and assessed their sensitivity to key modelling choices, as we detail in the appendix (pp 10, 11, 47–53).
Role of the funding sources
The sponsors of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The Writing and Global Analysis Group had access to all data sources. The corresponding author is responsible for the content of the report and had final responsibility for the decision to submit for publication.
Results
Our final dataset for HAZ and WAZ included 628 country-years, comprising anthropometric measurements of more than 7·7 million children (figure 1; appendix pp 15–46), providing an average of 4·5 years of data per country or territory. Data availability ranged from 1·1 years per country in Oceania to 6·8 in south Asia. 543 (86%) of these 628 country-years were nationally representative (appendix p 87). 126 of 141 countries, with greater than 99% of the total population, had at least one data source; of these, 111 had at least two. Each country in south Asia and sub-Saharan Africa had at least one data source.
Figure 1.
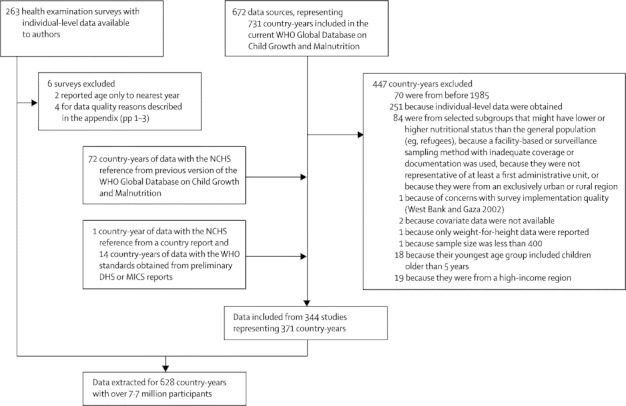
Flowchart of data sources, access, and inclusion
NCHS=US Centres for Disease Control and Prevention National Center for Health Statistics. DHS=Demographic and Health Survey. MICS=Multiple Indicator Cluster Survey.
When all 141 developing countries in our analysis were taken together, children's anthropometric status improved between 1985 and 2011 but did not reach optimum nutritional status as envisioned by the WHO growth standards (figure 2). In 1985, global (ie, all countries in our analysis) mean HAZ was −1·86 (95% uncertainty interval −2·01 to −1·72) and WAZ was −1·31 (–1·41 to −1·20; figure 3), representing a world where children were on average near the moderate stunting threshold (Z score of −2); these values improved to a mean HAZ of −1·16 (–1·29 to −1·04) and a mean WAZ of −0·84 (–0·93 to −0·74) in 2011. Over this period, prevalences of moderate-and-severe stunting declined from 47·2% (44·0 to 50·3) to 29·9% (27·1 to 32·9) and underweight from 30·1% (26·7 to 33·3) to 19·4% (16·5 to 22·2; PPs of being true decreases >0·999).
Figure 2.
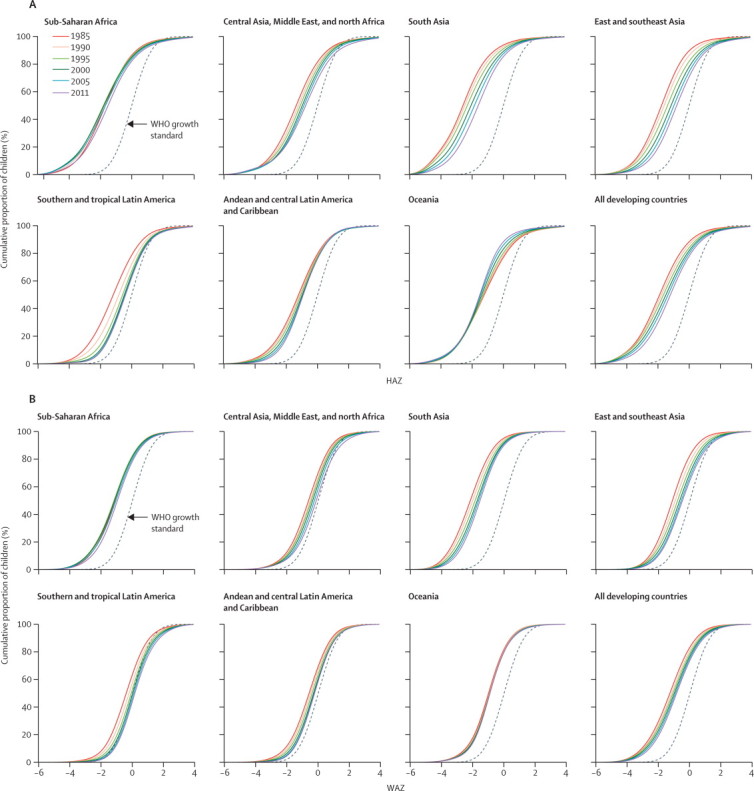
Trends in the cumulative distribution functions for HAZ (A) and WAZ (B) by region
Each curve shows the cumulative proportion of children (y-axis) that lies below a given HAZ or WAZ level (x-axis). Therefore, the lower the curve, the better the nutritional status of the region. All distributions are compared with the WHO standards. We present the trends by country in the appendix (pp 90–231). HAZ=height-for-age Z score. WAZ=weight-for-age Z score.
Figure 3.
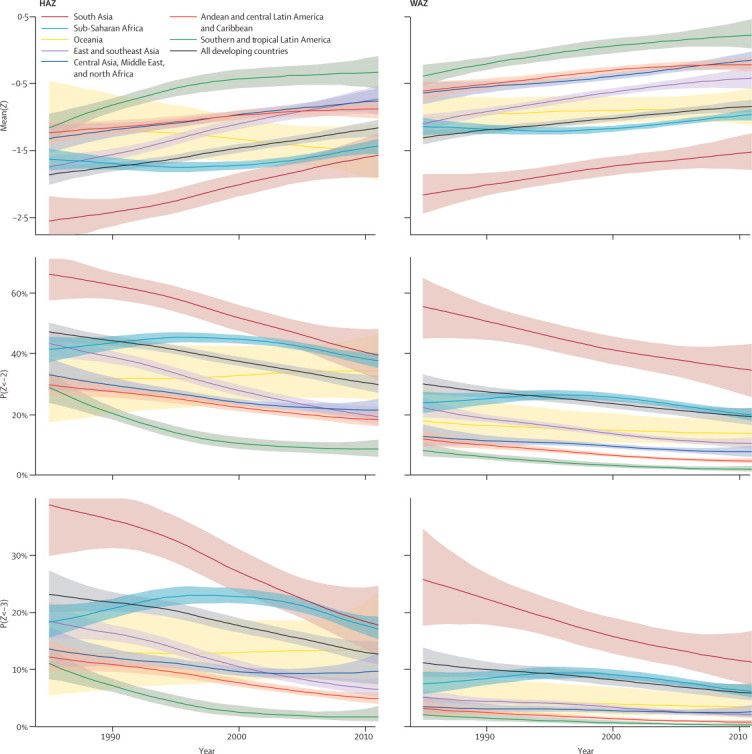
Trends in HAZ and WAZ means and prevalences by region between 1985 and 2011
Shaded regions show the uncertainty interval. We present the trends by country in the appendix (pp 90–231). Prevalence of children with Z scores below −2 includes all children below this cutoff, including those with Z scores below −3. HAZ=height-for-age Z score. WAZ=weight-for-age Z score.
Despite this improvement, in 2011, 314 (296 to 331) million children younger than 5 years had HAZ below −1. Just greater than half of these children (170 [154 to 186] million) had HAZ below −2. 258 (240 to 274) million children had WAZ below −1, less than half (110 [94 to 126] million) of whom had WAZ below −2. 37% of all children with mild-to-severe stunting and 46% with mild-to-severe underweight lived in south Asia (figure 4). Sub-Saharan Africa had the second largest number, a position that had belonged to east and southeast Asia in 1985.
Figure 4.
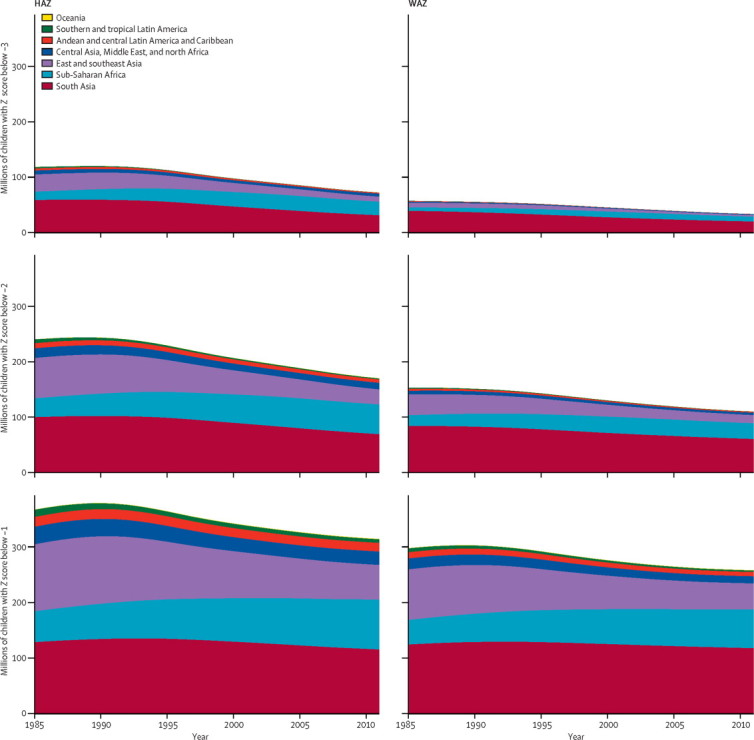
Number of children in the mild to severe parts of the HAZ and WAZ distributions, by region
The number of children with Z scores below −1 includes all children below this cutoff, including those with Z scores below −2 and −3. Similarly, the number of children with Z scores below −2 includes all children below this cutoff, including those with Z scores below −3. HAZ=height-for-age Z score. WAZ=weight-for-age Z score.
Sub-Saharan Africa experienced a period of increasing undernutrition until the late 1990s, when anthropometric status began to improve (panel 1). With large uncertainty, HAZ might have worsened slightly and WAZ might have improved only slightly in Oceania. Height for age and weight for age improved in all other regions. The largest improvements were in south Asia and east and southeast Asia (figure 2), with mean HAZ increasing by about 0·4 per decade and mean WAZ by about 0·25 per decade (PPs >0·99). Although Asia outperformed other regions in absolute gains, southern and tropical Latin America not only started with the best nutritional status but also had the largest relative decline in prevalences, with 39–44% declines per decade in moderate-and-severe stunting and underweight; the reductions in the severe tail were even larger.
Panel 1. Children's nutrition: a tale of three continents (and four countries).
In 1985, Burkina Faso, Brazil, China, and Ghana had mean height-for-age Z scores (HAZ) ranging from −1·34 to −1·67 and prevalences of moderate-and-severe stunting that ranged from 34% to 40%, with China faring slightly worse than the other three countries (appendix pp 88–89). Over the subsequent 26 years, they had very different trajectories in children's nutritional status and growth. Brazilian and Chinese children experienced large improvements throughout the period such that, by 2011, mean HAZ had reached −0·33 to −0·42 and the prevalence of moderate-and-severe stunting was 9–13% (figure appendix 1, appendix pp 90–231). By contrast with these success stories, nutritional status of children in Burkina Faso worsened for over a decade before improving slowly after the late 1990s. As a result, children's nutritional status in 2011 was only slightly better than it had been 26 years earlier, and was much worse than those of children in Brazil and China. These three countries exemplify the experiences of their respective regions, and the regionalisation of child undernutrition. Yet some countries like Ghana, one of Africa's best governed nations with strong commitment to agriculture and nutrition, defied the negative trends of the late 1980s and 1990s in sub-Saharan Africa and achieved steady, although slow, improvements.
Even in these countries with moderately rich data it is hard to identify the precise contributions of specific determinants of trends, perhaps because children's growth is multifaceted and affected by a complex, dynamic, and interactive array of social, environmental, nutritional, and health-care determinants.19,20 The existing evidence collectively suggests that improving children's anthropometric status requires enhancing nutrition, the living environment, and health care for the poor through equitable economic development, maternal education, and pro-poor agriculture, food, and health-care policies and programmes.
As a result of these trends, the regions' HAZ and WAZ distributions were reordered between 1985 and 2011. South Asia had the single worst nutritional status in 1985. By 2011, its HAZ distribution was similar to those of sub-Saharan Africa and Oceania, which had experienced periods of deterioration or stagnation (figures 2, 3). South Asia's WAZ did not catch up with other regions, but the difference with sub-Saharan Africa became smaller. At the other extreme, southern and tropical Latin America maintained its position as the best-nourished developing region, and increased its advantage compared with the Andean and central Latin America and Caribbean region and the central Asia, Middle East, and north Africa region. Improvements in southern and tropical Latin America slowed down after 2000, especially for mean. East and southeast Asia's strong performance led to its HAZ surpassing those of the central Asia, Middle East, and north Africa region and the Andean and central Latin America and Caribbean region.
The most undernourished country-years were in Bangladesh in the 1980s, when mean HAZ was as low as −2·7 and WAZ as low as −2·4; nearly three-quarters of children had HAZ below −2; more than a third were severely stunted; and about two-thirds were underweight (appendix pp 88, 89). Although children's anthropometric status improved in most countries (appendix pp 90–231, 233–239), height for age and weight for age remained very low in some places in 2011: children in Burundi, Yemen, Timor-Leste, Niger, and Afghanistan had HAZ means below or close to the −2 cutoff for moderate stunting (figure appendix 1). About half of children in these countries were moderately or severely stunted. Mean WAZ was −1·5 or less in Timor-Leste, Bangladesh, Niger, India, and Nepal, with one-third or more of children moderately or severely underweight (figure appendix 2). At the other extreme, children in Chile, Jamaica, and Kuwait had HAZ distributions indistinguishable from a well-nourished population in 2011, with means between 0·01 and 0·04. Similarly, 25 countries, mostly in the Latin America and Caribbean region and the central Asia, Middle East, and north Africa region, had WAZ means that surpassed the WHO standards, with the highest WAZ mean and lowest underweight prevalence in Chile.
HAZ probably deteriorated in 17 countries between 1985 and 2011, nearly all in sub-Saharan Africa and Oceania (appendix pp 230–239); most had large uncertainties, but the PPs for the observed deteriorations were 0·90 in Côte d'Ivoire and Niger. The largest improvement in children's height was in China, followed by smaller improvements in six other Asian countries, Brazil, and Tunisia; in these countries mean HAZ increased by 0·35–0·51 per decade, all with PPs of 0·99 or greater. WAZ improvements varied less across countries, ranging from possible worsening in Somalia, Burkina Faso, Central African Republic, Zimbabwe, Côte d'Ivoire, and Madagascar to improvements of 0·25 or greater per decade in Brazil and some countries in Asia and Middle East, all with PPs of 0·98 or greater. Mirroring these, underweight prevalences declined by a third or more per decade in 21 countries, nearly halving each decade in Brazil.
In most countries, changes in moderate-and-severe stunting or underweight prevalences between 1985 and 2011 were statistically indistinguishable from those we expected had the whole HAZ and WAZ distribution shifted by as much as its median (appendix p 232). In other words, reductions in prevalence were generally because of overall improvements in population nutrition versus interventions targeting children at high risk. In some countries, especially in the Latin America and Caribbean region, however, prevalence declined more than expected from the improvement in the population median—ie, an inequality-reducing change in the distribution.
Despite improvements, the probability that developing countries as a whole will meet the MDG 1 target is less than 0·05 if post-2000 trends continue. The probability ranged from virtually zero in sub-Saharan Africa to close to 1 in the two Latin America and Caribbean regions. 27 countries in the Latin America and Caribbean region, the central Asia, Middle East, and north Africa region, and east and southeast Asia have probabilities of 0·80 or greater, with probability close to 1·0 in Chile, Brazil, Mexico, and China. Another 34 countries had probabilities between 0·50 and 0·80, leaving 80 countries with less than a 50% chance of reaching this target (figure 5). Only six countries in sub-Saharan Africa had probabilities of 0·50 or greater, with the highest chances of success in Ghana and Angola.
Figure 5.
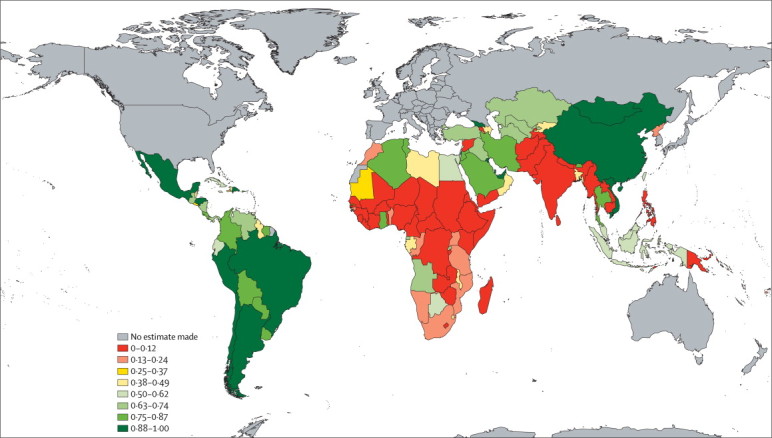
Posterior probability of meeting the MDG 1 target
Defined here as halving the prevalence of WAZ below −2 between 1990 and 2015 or reaching a prevalence 2·3% or lower if post-2000 trend continues. WAZ=weight-for-age Z score.
Discussion
Our findings show that, on average, children's anthropometric status has improved in developing countries over the past 26 years, but there were major differences across regions and countries in trends and in present nutritional status. There were impressive improvements in Asia and the Latin America and Caribbean region, contrasting with periods of stagnation or worsening in Oceania and sub-Saharan Africa. This deterioration had not been noted in previous analyses that used linear trends (panel 2).4–7 In a positive development, nutritional status improved in sub-Saharan Africa in more recent years, and the pace of improvement accelerated in south Asia. Despite these positive trends, children in some countries in sub-Saharan Africa and south Asia remain alarmingly undernourished whereas in the Latin America and Caribbean region; central Asia, Middle East, and north Africa; and increasingly east Asia, children are largely fulfilling their growth potential. Improvements in southern and tropical Latin America slowed down after 2000, especially for mean, perhaps because some countries approached a state of having almost no undernutrition, with improvements only in the small remaining tail of the distribution. Unless there are unprecedented improvements in child nutrition in the next few years, more than half of developing countries have less than a 50% chance of meeting the MDG 1 target.
Panel 2. Research in context.
Systematic review
We searched PubMed for studies published between Jan 1, 1990, and April 11, 2012, with combinations of the keywords “underweight” or “stunting”, and “trends”. We limited our search to publications about low-income and middle-income countries or global analyses. Many such comparisons are in reports of international organisations, which we also identified and accessed. Previous studies reported stunting, underweight, and wasting prevalence by country at a single point in time and linear trends in prevalence by region.2,4–7 The Millennium Development Goals (MDGs) Report21 regularly reports progress towards MDG 1 at regional level, and UNICEF tracks country progress. At least one other study also attempted to assess global progress towards MDG 1.22
Interpretation
Our study adds to the international comparisons of childhood undernutrition and progress towards the MDGs. We estimated trends in distributions of height-for-age and weight-for-age Z scores, which allowed the estimation of means as well as mild, moderate, and severe stunting, and underweight prevalences. We identified that on average children's anthropometric status improved in developing countries but there were major differences across regions and countries in trends and in present nutritional status. The largest improvements were in Asia and the Latin America and Caribbean region but there were periods of stagnation or worsening in Oceania and sub-Saharan Africa. We also estimated the probability that countries and regions would meet the MDG 1 target if their post-2000 trends continue, and noted that more than half of developing countries have less than a 50% chance of meeting the target.
Our estimated global stunting and underweight prevalences for recent years are similar to those based on regional models, especially when the uncertainty intervals are considered.2,6,7 The differences become larger around 2000 and in regions where trends were non-linear, because the previous analyses used a linear model and hence did not detect the peaking of undernutrition in the late 1990s in sub-Saharan Africa or the recent slowdown of improvements in southern and tropical Latin America. The uncertainty interval around our underweight prevalence estimate for 2006 covered the 22% estimate for 2003–09 by UNICEF, but our estimate for severe underweight was lower (6·7% [5·6–7·9%] vs 9%), possibly because we used data and methods that estimated the full distribution. We had previously estimated the prevalences of severe stunting and underweight with restrictive assumptions about distributions without estimating the full distribution;2 this led to estimates of severe stunting and wasting in 2005 that were less than half of those in our present analysis.
Our assessment of progress towards the MDG 1 target differs from that of Svedberg,22 who concluded that “the progress towards the MDG at the global level is on track owing to the large decline in China”. This work did not do a systematic global analysis of trends and analysed data from a small number of countries selected based on their total population, even though the global trend is affected most by the countries with the largest number of underweight children. It is not possible to directly compare our estimates of country progress towards MDG 1 with those from UNICEF because of differences in reference population and reporting.23 Both analyses identified the Latin America and Caribbean region and east and southeast Asia as regions with the best progress, but our estimated probability of 0·70 means that the latter cannot afford for progress to slow, making its classification as “on track” somewhat fragile. Broadly, our probabilistic assessment of progress towards MDG 1 was consistent with UNICEF's categorical assignment for many countries. Differences nonetheless arose in some countries (eg, in Armenia, Benin, Cambodia, Liberia, North Korea, and Tanzania), which are considered “on track” by UNICEF but had probabilities of 0·25 or less in our estimates or in Botswana, Egypt, and Iraq, which UNICEF judges to have “insufficient progress” but had probabilities of 0·57–0·74 in our analysis.
The strengths of our study include analysis of trends by country; the large amount of data accessed and our rigorous inclusion and exclusion criteria; incorporating non-linear trends; accounting for study representativeness such that our estimates used all available data but tracked data from nationally representative studies that covered children younger than 5 years more closely; and systematic estimation and reporting of uncertainty. Although many of these strengths are shared with previous systematic analyses in global health, we estimated trends in the full population distributions, which we used to estimate means as well as prevalences of mild to severe undernutrition without restrictive assumptions. Our Bayesian model also allowed us to the quantify progress towards MDG 1 as a probability, which is consistent with the inherent uncertainty in assessing such progress.
The main limitation of our study is that many country-years remained without data or only had data on parts of the distribution, which increased the uncertainty of our estimates. At the same time, the proportion of countries with data, with time-series data, and with nationally representative data was larger than for other major global risk factors.24,25 Importantly, many countries in sub-Saharan Africa had repeated surveys that showed a deteriorating trend for the first half of our analysis period. Conversion from the (older) NCHS reference to the (newer) WHO standards allowed the use of all data sources but was associated with increased uncertainty.
Children's growth is adversely affected by infection and suboptimal nutrition.1 Hence, food insufficiency, poor water and sanitation, and restricted access to high-quality primary care, all associated with household and community poverty, lead to poor growth outcomes.3 However, interventions such as complementary feeding and diarrhoea case management can mitigate undernutrition.26 We noted that, with few exceptions, the reductions in stunting and underweight prevalences were due to shifts in the whole distribution. This finding suggests a role for broader socioeconomic, agriculture and food, environmental, and health-care determinants in the recorded trends versus targeted programmes, perhaps because the coverage of nutrition-specific interventions generally remain low.6,27 The relative importance of various macro forces is uncertain but a few lessons have emerged from previous research. First, growth in national income seems to have a positive effect on child nutrition but might be insufficient on its own, perhaps because improving nutritional status requires equitable income distribution and investments in healthcare, agriculture, and programmes that improve access to food.28–32 Second, macroeconomic shocks, structural adjustment, and trade policy reforms have been implicated in worsening nutritional status in sub-Saharan Africa in the 1980s and 1990s.33,34 These policies neither expanded agricultural productivity nor reduced poverty, rather they led to lower spending on agriculture and health care.34–37 Their adverse effects on nutrition were largest in poorer households, especially in rural regions, mediated through lower household earnings or assets and reduced food subsidies and health-care use.33,34 By contrast, programmes that improved income, nutrition, and health care for poor people generally also improved growth outcomes, especially in children from families with a lower socioeconomic status.38–40 This all seems to suggest that child nutrition is best improved through equitable economic growth, investment in infrastructures, technologies, and policies that improve agricultural productivity and earnings of smallholder farmers,36 and pro-poor primary care and food programmes. Focusing on these determinants and their effects on nutrition is particularly relevant in the context of the worldwide economic crisis and rising food prices, which might increase inequalities and erode or limit investments in nutrition and health care.
Acknowledgments
Acknowledgments
GAS is a staff member of WHO and is responsible for the views expressed in this publication—they do not necessarily represent the decisions, policy, or views of WHO. The estimates do not represent official statistics from WHO. We thank Ties Boerma, Debbie Bradshaw, Joanne Katz, Colin Mathers, Shelly Sundberg, and Andrew Thorne-Lyman for valuable comments on study design and data sources, and James Hayward for administrative support.
Contributors
ME designed the study concept with input from other authors. GAS, SRF, and AJD collated country data and checked data sources, with contributions from study group members. MMF and CJP developed statistical methods with input from GAS, SRF, and ME. MMF, GAS, SRF, and RAW assessed data and prepared results. ME wrote the first draft of the report and other study group members contributed to subsequent drafts.
Nutrition Impact Model Study Group (Child Growth)
Writing and Global Analysis Group Gretchen A Stevens*, Mariel M Finucane*, Christopher J Paciorek, Seth Flaxman, Richard A White, Abigail Donner, Majid Ezzati. *These authors contributed equally to the research and preparation of the report. Other Members Simon Barquera (Institutó Nacional de Salud Pública, Cuernavaca, México), Zulfiqar Bhutta (Aga Khan University, Karachi, Pakistan), Robert E Black (Johns Hopkins University Bloomberg School of Public Health, Baltimore, MD, USA), Katia Castetbon (Université Paris, Bobigny, France), Farshad Farzadfar (Tehran University of Medical Sciences, Tehran, Iran), Wafaie Fawzi (Harvard School of Public Health, Boston, MA, USA), Young-Ho Khang (University of Ulsan College of Medicine, Seoul, South Korea), Nayu Ikeda (University of Tokyo, Tokyo, Japan), Shahab Khatibzadeh (Harvard School of Public Health, Boston, USA), Guansheng Ma (Chinese Center for Disease Control and Prevention, Beijing, China), Eric Monterubio (Institutó Nacional de Salud Pública, Cuernavaca, México).
Conflicts of interest
We declare that we have no conflicts of interest.
Supplementary Material
Supplementary Material
References
- 1.Scrimshaw NS, SanGiovanni JP. Synergism of nutrition, infection, and immunity: an overview. Am J Clin Nutr. 1997;66:464S–477S. doi: 10.1093/ajcn/66.2.464S. [DOI] [PubMed] [Google Scholar]
- 2.Black RE, Allen LH, Bhutta ZA. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371:243–260. doi: 10.1016/S0140-6736(07)61690-0. [DOI] [PubMed] [Google Scholar]
- 3.UNICEF . Strategy for improved nutrition of children and women in developing countries. UNICEF; New York, NY: 1990. [Google Scholar]
- 4.de Onis M, Frongillo E, Blossner M. Is malnutrition declining? An analysis of changes in levels of child malnutrition since 1980. Bull World Health Organ. 2000;78:1222–1233. [PMC free article] [PubMed] [Google Scholar]
- 5.de Onis M, Blossner M, Borghi E, Frongillo EA, Morris R. Estimates of global prevalence of childhood underweight in 1990 and 2015. JAMA. 2004;291:2600–2606. doi: 10.1001/jama.291.21.2600. [DOI] [PubMed] [Google Scholar]
- 6.Lutter CK, Daelmans BM, de Onis M. Undernutrition, poor feeding practices, and low coverage of key nutrition interventions. Pediatrics. 2011;128:e1418–e1427. doi: 10.1542/peds.2011-1392. [DOI] [PubMed] [Google Scholar]
- 7.de Onis M, Blossner M, Borghi E. Prevalence and trends of stunting among pre-school children, 1990–2020. Public Health Nutr. 2011;15:142–148. doi: 10.1017/S1368980011001315. [DOI] [PubMed] [Google Scholar]
- 8.Pelletier DL, Frongillo EA, Jr, Schroeder DG, Habicht JP. The effects of malnutrition on child mortality in developing countries. Bull World Health Organ. 1995;73:443–448. [PMC free article] [PubMed] [Google Scholar]
- 9.Rajaratnam JK, Marcus JR, Flaxman AD. Neonatal, postneonatal, childhood, and under-5 mortality for 187 countries, 1970–2010: a systematic analysis of progress towards Millennium Development Goal 4. Lancet. 2010;375:1988–2008. doi: 10.1016/S0140-6736(10)60703-9. [DOI] [PubMed] [Google Scholar]
- 10.WHO . WHO child growth standards length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. World Health Organization; Geneva: 2006. [Google Scholar]
- 11.de Onis M, Blossner M. The World Health Organization global database on child growth and malnutrition: methodology and applications. Int J Epidemiol. 2003;32:518–526. doi: 10.1093/ije/dyg099. [DOI] [PubMed] [Google Scholar]
- 12.Frühwirth-Schnatter S. Finite mixture and Markov switching models. Springer; New York, NY: 2006. [Google Scholar]
- 13.Rodriguez A, Dunson DB, Taylor J. Bayesian hierarchically weighted finite mixture models for samples of distributions. Biostatistics. 2009;10:155–171. doi: 10.1093/biostatistics/kxn024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dunson DB. Nonparametric Bayes applications to biostatistics. In: Hjort NL, Holmes C, Müller P, Walker SG, editors. Bayesian nonparametrics. Cambridge University Press; Cambridge: 2010. pp. 223–273. [Google Scholar]
- 15.Tentoni S, Astolfi P, De Pasquale A, Zonta LA. Birthweight by gestational age in preterm babies according to a Gaussian mixture model. BJOG. 2004;111:31–37. doi: 10.1046/j.1471-0528.2003.00006.x. [DOI] [PubMed] [Google Scholar]
- 16.Gakidou E, Cowling K, Lozano R, Murray CJ. Increased educational attainment and its effect on child mortality in 175 countries between 1970 and 2009: a systematic analysis. Lancet. 2010;376:959–974. doi: 10.1016/S0140-6736(10)61257-3. [DOI] [PubMed] [Google Scholar]
- 17.Myerson R, Rosenfeld LC, Lim SS, Murray CJL. Safe pregnancy and delivery: a systematic analysis of trends in the coverage of antenatal and intrapartum care. Global Health Metrics and Evaluation Conference: Controversies, Innovation, Accountability; Seattle, WA, USA; March 14–16, 2011.
- 18.Victora CG, de Onis M, Hallal PC, Blossner M, Shrimpton R. Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics. 2010;125:E473–E480. doi: 10.1542/peds.2009-1519. [DOI] [PubMed] [Google Scholar]
- 19.von Braun J, Ruel M, Gulati A. Accelerating progress toward reducing child malnutrition in India. International Food Policy Research Institute; Washington, DC: 2008. [Google Scholar]
- 20.Monteiro CA, Benicio MH, Konno SC, Silva AC, Lima AL, Conde WL. Causes for the decline in child under-nutrition in Brazil, 1996–2007. Rev Saude Publica. 2009;43:35–43. doi: 10.1590/s0034-89102009000100005. [DOI] [PubMed] [Google Scholar]
- 21.UN . The millennium development goals report 2011. United Nations; New York, NY: 2011. [Google Scholar]
- 22.Svedberg P. Declining child malnutrition: a reassessment. Int J Epidemiol. 2006;35:1336–1346. doi: 10.1093/ije/dyl157. [DOI] [PubMed] [Google Scholar]
- 23.United Nations Statistics Division . Indicators for monitoring the millennium development goals—definitions, rationale, concepts and sources. United Nations; New York, NY: 2004. [Google Scholar]
- 24.Finucane MM, Stevens GA, Cowan MJ. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet. 2011;377:557–567. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Danaei G, Finucane MM, Lin JK. National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5·4 million participants. Lancet. 2011;377:568–577. doi: 10.1016/S0140-6736(10)62036-3. [DOI] [PubMed] [Google Scholar]
- 26.Bhutta ZA, Ahmed T, Black RE. What works? Interventions for maternal and child undernutrition and survival. Lancet. 2008;371:417–440. doi: 10.1016/S0140-6736(07)61693-6. [DOI] [PubMed] [Google Scholar]
- 27.Bryce J, Coitinho D, Darnton-Hill I, Pelletier D, Pinstrup-Andersen P. Maternal and child undernutrition: effective action at national level. Lancet. 2008;371:510–526. doi: 10.1016/S0140-6736(07)61694-8. [DOI] [PubMed] [Google Scholar]
- 28.Smith LC, Haddad L. How potent is economic growth in reducing undernutrition? What are the pathways of impact? New cross-country evidence. Econ Dev Cult Change. 2002;51:55–76. [Google Scholar]
- 29.Ravallion M. Income effects on undernutrition. Econ Dev Cult Change. 1990;38:489–515. [Google Scholar]
- 30.Anand S, Ravallion M. Human-development in poor countries—on the role of private incomes and public-services. J Econ Perspect. 1993;7:133–150. [Google Scholar]
- 31.Subramanyam MA, Kawachi I, Berkman LF, Subramanian SV. Is economic growth associated with reduction in child undernutrition in India? PLoS Med. 2011;8:e1000424. doi: 10.1371/journal.pmed.1000424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haddad L, Alderman H, Appleton S, Song L, Yohannes Y. Reducing child malnutrition: how far does income growth take us? World Bank Econ Rev. 2003;17:107–131. [Google Scholar]
- 33.Pongou R, Salomon JA, Ezzati M. Health impacts of macroeconomic crises and policies: determinants of variation in childhood malnutrition trends in Cameroon. Int J Epidemiol. 2006;35:648–656. doi: 10.1093/ije/dyl016. [DOI] [PubMed] [Google Scholar]
- 34.Cooper Weil D, Alicbusan A, Wilson J, Reich M, Bradley D. The impact of development policies on health: a review of the literature. World Health Organization; Geneva: 1990. [Google Scholar]
- 35.Sundberg S. Agriculture, poverty and growth in Africa: linkages and policy challenges. CAB Reviews: Perspectives in Agriculture, Veterinary Science, Nutrition and Natural Resources. 2009;4:92. [Google Scholar]
- 36.Sanchez PA, Swaminathan MS. Hunger in Africa: the link between unhealthy people and unhealthy soils. Lancet. 2005;365:442–444. doi: 10.1016/S0140-6736(05)17834-9. [DOI] [PubMed] [Google Scholar]
- 37.World Bank . World Development Report 2008: Agriculture for Development. The World Bank; Washington, DC: 2008. [Google Scholar]
- 38.Rivera JA, Sotres-Alvarez D, Habicht JP, Shamah T, Villalpando S. Impact of the Mexican program for education, health, and nutrition (Progresa) on rates of growth and anemia in infants and young children: a randomized effectiveness study. JAMA. 2004;291:2563–2570. doi: 10.1001/jama.291.21.2563. [DOI] [PubMed] [Google Scholar]
- 39.Fernald LC, Gertler PJ, Neufeld LM. Role of cash in conditional cash transfer programmes for child health, growth, and development: an analysis of Mexico's Oportunidades. Lancet. 2008;371:828–837. doi: 10.1016/S0140-6736(08)60382-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lagarde M, Haines A, Palmer N. Conditional cash transfers for improving uptake of health interventions in low- and middle-income countries: a systematic review. JAMA. 2007;298:1900–1910. doi: 10.1001/jama.298.16.1900. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


