Abstract
Objective
To explore and synthesize the literature on phenomena associated with sick leave among patients with Medically Unexplained Physical Symptoms (MUPS).
Design
A systematic review of the literature was undertaken in three phases: (1) a search of the following databases: Medline, Embase, Psych Info, Cochrane Collaboration Library, Digital Dissertations, DiVA, SweMed +, NORART, and ISI Web of Science, (2) selection of studies based on pre-specified inclusion criteria was undertaken, extracting study design and results, (3) quality assessment was undertaken independently by two reviewers. Due to heterogeneity in study designs, populations, interventions, and outcome measures, a mixed research synthesis approach was used. Results were assessed in a pragmatic and descriptive way; textual and numerical data were extracted from the included studies, and classified into patient- and doctor-related factors.
Results
Sixteen studies were included. With regard to patients, an association was found between sick leave and psychiatric comorbidity as well as total symptom burden. With regard to doctors, knowledge of the patient, sympathy, and trust appeared to increase the probability of the patient being sick-listed. None of the interventions in the educational programmes aiming to improve doctors’ management of MUPS patients succeeded in lowering sick leave.
Implications
Despite MUPS being a leading cause of sickness absence, the review identified only a small number of studies concerning phenomena associated with sick leave. The authors did not identify any studies regarding the impact of the working conditions on sick leave among MUPS patients. This is an important area for further studies.
Key Words: General practice, medically unexplained symptoms, Norway, review, sick leave, somatoform disorder
Phenomena associated with sick leave among patients with Medically Unexplained Physical Symptoms are related to patients as well as doctors.
In patients, sick leave was related to psychiatric comorbidity and to the total symptom burden.
With regard to doctors, knowledge of the patient, sympathy, and trust seemed to influence probability of the patient being sick-listed.
Medical educational programmes were not found to change sickness certification rates in this group of patients.
Introduction
Medically Unexplained Physical Symptoms (MUPS) is an increasingly used term for symptoms where no clear or consistent organic pathology can be demonstrated [1]. Due to the lack of consensus regarding definition [2], research on MUPS-related phenomena is challenging. Other related terms are Bodily Distress Disorder [3], Functional Somatic Syndromes [4], and Subjective Health Complaints [5]. Still, the group of patients is both common (15–19% of consultations in general practice, [1]) and highly recognizable to general practitioners (GPs). In practice, patients will usually present complex problems like digestive problems, widespread muscular pain, or asthenia, often in combination.
Traditionally, medical training has focused on understanding and treatment of single symptoms with corresponding findings leading to a specific diagnosis. However, in general practice many patients present several non-specific complaints without corresponding clinical signs or findings. For many clinicians, the notion of MUPS has improved the understanding of the patients’ complaints. It has been suggested that MUPS may be caused by a common mechanism with different expressions [6]. Such mechanisms may be explained by the Biopsychosocial Model [7] or the Cognitive Activation Theory of Stress [8].
Nearly half of all sickness absence in Norway is given a musculoskeletal diagnosis, and 20% a psychiatric diagnosis [7,9,10]. As these diagnoses in primary care most often are non-specific and not well defined, researchers have suggested MUPS to represent a leading cause for sick leave [9,11,12]. The doctor will often put a diagnosis of musculoskeletal or mental disorder on complaints based on the patient's presentation of the symptoms [13,14]. Accordingly, many patients on sick leave for musculoskeletal or mental reasons suffer from conditions which can be categorized as MUPS.
Comorbidity occurs frequently in patients with MUPS [15]. Some 31% of patients sick-listed with a diagnosis of low back pain also had a psychiatric disease [16] and 20–50% of patients with irritable bowel disease also had a diagnosis of fibromyalgia [17].
The impact of MUPS symptoms on work disability varies from patient to patient. Some continue to work as usual, while others become sick listed for apparently comparable symptom burdens [9]. The transition from normal self-limiting complaints to disabling symptoms is not well known. In this review we wanted to explore and synthesize the literature on sick leave among MUPS patients, focusing on phenomena associated with sick leave.
Design, material, and method
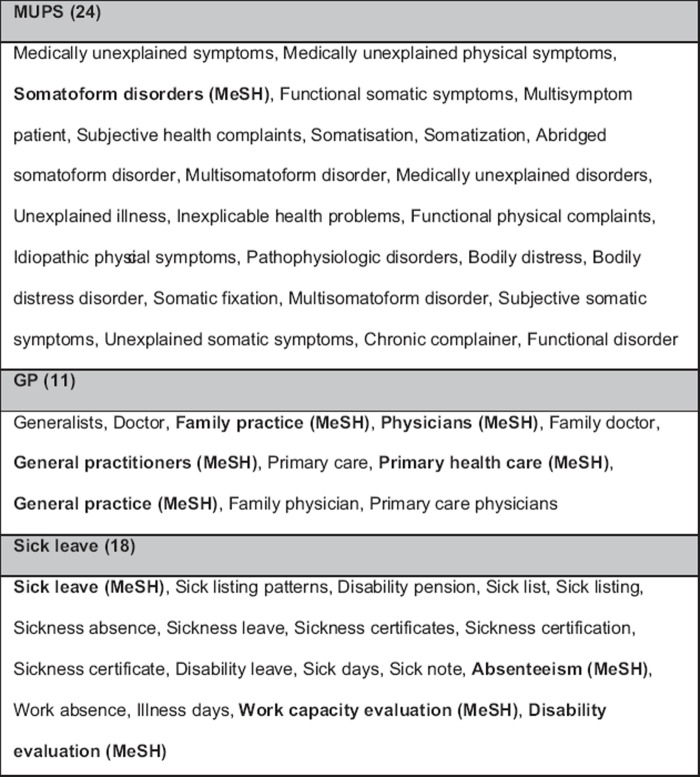
A systematic review of the literature was conducted to gather, critically evaluate, and synthesize studies dealing with phenomena associated with sick leave among MUPS patients in primary care. Such associations could include any element influencing the process of sick leave in terms of the individual MUPS patient. Due to the nature of the topic, studies with quantitative and qualitative designs were included. The study comprised three steps. Step 1 involved a systematic search of the literature based on a combination of keywords (see Figure 1). Step 2 involved screening of literature titles and abstracts using specific pre-specified inclusion criteria described in the following. Step 3 involved classifying the internal validity of the included studies using established and valid tools, which was undertaken by the same reviewers independently.
Figure 1.
List of keywords used in the search-string.
Due to the heterogeneity in study designs, populations, interventions, and outcome measures, a mixed research synthesis approach was used. Results were assessed in a pragmatic and descriptive way, with textual and numerical data extracted from the studies included.
Step 1: Search of studies
The following electronic databases were searched from their inception date until 17 June 2010: Medline, Embase, Psych Info, Cochrane Collaboration Library, Digital Dissertations, DiVA, SweMed +, NORART, and ISI Web of Science. Each database was searched using a combination of keywords for MUPS and related overarching terms (Figure 1), primary care setting, and sickness certification by the first author in cooperation with an academic librarian. An auto-alert was created in OVID (Medline, Psyc Info, and Embase) to identify studies published in the period from 17 June 2010 to 31 December 2010. Finally, in March 2012 we searched in all databases once more for potentially new publications in the period after 1 January 2011, which revealed one additional study for inclusion [18].
Inclusion criteria were studies of adults (>18 years) with MUPS or a related term, in a primary care setting, with work incapacity or sick leave as an outcome, and published in English, German, French, or any Scandinavian language. Studies of specified syndromes and single symptom diagnosis, such as fibromyalgia and low back pain were excluded.
Step 2: Selection of studies
Titles and abstracts were screened, and articles fulfilling the criteria were obtained in full text and assessed again for eligibility. Any discrepancy in the results was negotiated until unified consensus was reached upon inclusion.
Step 3: Assessment of study quality and risk of bias in the studies included
Two appraisal tools were chosen to classify the internal validity and quality of the included studies. Quantitative studies were assessed with a framework presented by Hayden et al. [19]. Assessment of the internal validity of studies was based on six potential sources of bias: (1) study participation, (2) study attrition, (3) exposure measurement, (4) confounding measurement and account, (5) outcome measurement, and (6) analysis. The framework outlined by Malterud was used to assess the qualitative studies [20]. The internal validity and quality of the included studies were assessed independently by AAA and ELW who met to discuss the final internal validity scores. Differences were negotiated until a consensus was reached. The methodological study quality was classified as strong (S), medium (M), or low (L) according to a modified version of Hayden's framework [19].
Results
Study characteristics
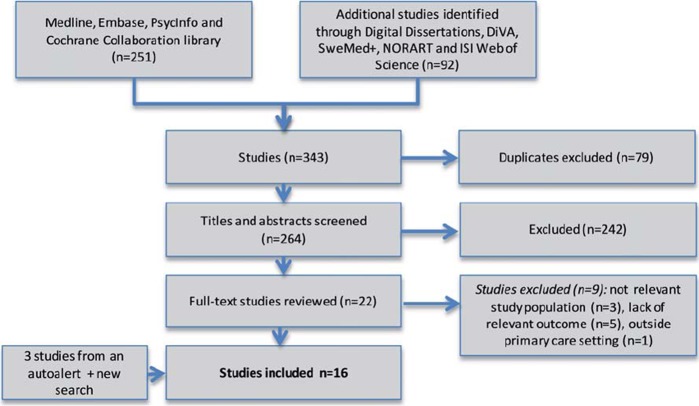
The initial search identified 264 studies, of which 16 studies fulfilled the inclusion criteria (Figure 2). Study designs included three qualitative studies [14,21,22], four randomized controlled studies (RCTs) [23–26], and nine cross-sectional observational studies [18,27–34] (see Tables I and II). Overall the RCTs together included 1229 patients and 85 GPs.
Figure 2.
Identification of studies.
Table I.
Included studies: Patient-related phenomena associated with sick leave.
| First author, year, country [reference] | Aim | Study design | Patient-related phenomena | Quality of paper |
| Harris, 2009, Boston, US [30] | A comparison of somatizing and non-somatizing patients regarding disability and role impairment, and determination of the independent contribution of somatization to this | Cross-sectional observational study with self-report questionnaires (n =467) | Somatizers reported more often psychiatric comorbidity (60% vs. 14%) and somatic co morbidity (39% vs 30%) than non-somatizers, and also more often reported work limitations (OR 3.2) | S |
| Muller, 2008, South Africa [34] | To evaluate the prevalence of depressive and anxiety disorders in patients with multisomatoform disorder, and to compare demographic and clinical outcomes in those with and without comorbidity | Cross-sectional observational study with structured diagnostic interview (n =51), 90% females. Among outcomes were disability and reported sick-days | 4 or more psychiatric comorbid disorders were associated with significantly higher levels of overall disability, p =0. 041 | M |
| Hoedemann, 2009, Netherlands [32] | To assess the prevalence of MUPS in sick-listed employees and its associations with depressive or anxiety disorders, health anxiety, distress, and functional impairment | Cross-sectional observational study (n =489) | A prevalence of 15.1% severe MUPS, i.e. >15 symptoms on PHQ-15, which was associated with 4–6 times more psychiatric comorbidity and impairment | S |
| Gureje, 1997, Australia – WHO, 14 countries [29] | To determine the frequency and correlates of somatization in primary care settings in 14 countries | Cross-sectional study with a stratified sample (n =5438). Correlates: gender, age, physical health and disability | Somatization is common across cultures and it is associated with older age, less education, worse self-reported health, psychiatric comorbidity, and more occupational disability (more than >1 day self-reported last month) | M |
| Gullbrandsen, Norway, 1998 [28] | To describe the prevalence of self-perceived work disability in general practice and the level of psychosocial problems among work-disabled patients. | Cross-sectional observational study (n =1058). Self-reporting questionnaire | Study identified 7 not work-related psychosocial problems of which 6 were 2–3 times more likely to occur among the work-disabled patients, indicating a correlation between greater self-reported work disability with increasing number of psychosocial problems | S |
| Hoedemann, 2010, Netherlands [31] | To compare patients with high levels of somatic symptom severity (HLSS) vs. lower levels. Outcomes: duration of sick leave, return to work and disability | Cross-sectional observational study with the same population as in reference [32] | Patients with HLSS had longer duration of sick leave (median 78 days longer) and remained more often disabled. Health anxiety and older age were associations for sick-leave duration among HLSS patients | S |
| Kroenke, US, 2002 [33] | To validate a 15-item questionnaire on mental and somatic symptoms and its association with functional status, disability days, and health-care utilization | Cross-sectional observational study (n =6000). Outcomes included functional status (SF-20), self-reported sick days and clinic visit | Greater levels of somatization severity were associated with a stepwise increase in disability days | S |
| Al-Windi, 2005, Sweden [27] | To examine the impact of different symptoms on health-care utilization | Cross-sectional observational study (n =1055). 7 symptoms groups: depression, tension, GI, musculoskeletal, metabolism, cardiopulmonary, and head | A linear correlation between numbers of symptom categories and days of sick leave | M |
| Thorslund, 2007, Sweden [25] | To determine the effect of solution-focused group therapy on RTW among MUPS1 patients on long-term sick leave | RCT (n =30). Sick-listed for 1–5 months. Randomized to solution focus group therapy or waiting list (control) | The intervention group returned to work at a significantly higher rate and worked more days, and this difference increased at 3-month follow-up | M |
| Roelen, 2010, [18], Netherlands | To estimate prevalence of Subjective Health Complaints (SHC), and see if either number or type of complaints were related to sickness absence | Cross-sectional observational study (n =409). Self-reported questionnaire, linked to number of sickness absence episodes in 2003–2004 | Prevalence of SHC: 78%. Positive relation between number of SHC and number of sickness absence episodes | S |
Note: 1Redefined as MUPS in this study: Diagnoses fell into two categories, D4 (depression, anxiety, stress-syndrome, and adjustment reactions) and D12 (musculoskeletal illnesses and fibromyalgia).
Table II.
Included studies: GP-related phenomena associated with sick leave.
| First author, year, country [reference] | Aim | Study design | GP-related phenomena | Quality of paper |
| Schilte, 2001, Netherlands [24] | To evaluate a disclosure intervention among somatizing patients. Sick leave was one outcome | RCT (n =161). 9 other GP offices served as an extra control-group | The intervention did not reduce the sick leave but seemed to impact negatively | S |
| Larisch, 2005, Germany [26] | To evaluate the cost effects of specialized psychosocial training of GPs working with somatizing patients. Sick leave was an indirect cost | RCT (n =20 GPs/73 patients in the intervention group versus 17 GPs/54 patients in the control group) | No significant difference in costs related to sick leave days. | S |
| Rosendal, 2007, Denmark [23] | To evaluate the effect of an educational programme (TERM) where one outcome was disability days | RCT (n =43 GPs, 911 somatizing patients) | Disability days decreased by 1.7 days in the control group and increased by 1.0 day in the intervention group, but the results were not significant (p =0.212) | S |
| Ringsberg, 2006, Sweden [21] | To elucidate GPs’ perception of MUS patients, focusing on stressing situations, emotional reactions, and coping strategies | Focus-group discussion, 5 groups, total of 27 GPs. Tape-recording, verbatim typewritten, phenomenographic approach | GPs issued a sickness certificate when they felt “stuck” and felt they needed a “breathing space” from the patient | S |
| Woivalin, 2004, Sweden [22] | To explore GPs’ perceptions and ways of managing patients with MUS | The same focus groups as Ringsberg (ref [21]) | Findings of a pathological test, even subtle, eased the assessment of sick-listing the patient. They were aware of medicalization when accepting psychosocial problems as cause for sick leave as they needed to label the symptoms as a disease | M |
| Nilsen, Norway, 2011 [14] | To explore GPs’ considerations in decision-making regarding sick-listing of patients suffering from subjective health complaints | Focus-group discussion, 9 groups, total of 48 GPs. Tape-recording, verbatim typewritten, systematic text condensation | Factors described to ease assessment of sick leave: finding of an objective sign, seeing a clear purpose of sickness certificate, an established good therapeutic relationship based on prior knowledge, trust and sympathy | S |
One study was published in German [26], the remainder in English. All continents were represented, with a North European majority. Three of the RCTs described interventions to improve GPs’ management of MUPS patients [23,24,26], whereas one RCT described an intervention intended to support coping for MUPS patients [25].
In the observational studies, sick leave was registered by patients’ self-report or based on recordings. One author was contacted for further information to clarify the relationship between self-reported work disability and actually sick leave [28]. Two studies reported on the same study population, but were included due to different outcomes [31,32].The internal validity of the papers was strong (n =11), medium (n =5), and low (n =0). All three qualitative studies applied focus groups [14,21,22].
The results are presented as two levels of associations: those related to the patient (n =10) and those related to the sick listing GP (n =6). The studies are summarized in Table I and Table II.
Patient-related associations
Psychiatric comorbidity seems to be a common feature of MUPS patients, which increases the risk of sick leave. Six studies identified depression and anxiety disorders as being associated with the ability to work for this group of patients [24,26,30–32,34]. Three of these studies reported psychiatric comorbidity ranging from 21% to 60% [24,26,30]. Levels of depression and anxiety (29% and 53%) were found in addition to MUPS symptoms in one study [34]. Also Hoedeman's studies reported an over-representation of psychiatric comorbidity among the work-disabled MUPS patients [31,32].
In addition to somatic symptoms, significantly more health-affecting psychosocial problems were reported among patients perceiving themselves as work-disabled by at least 50% [28]. A linear correlation between an increasing number of symptoms and sick leave days was reported in five studies, suggesting that MUPS patients with the most heavy symptom load also present most impaired work function [18,27,29,31,33]. One RCT reported a group therapy intervention with MUPS patients. The intervention group returned to work at a significantly higher rate and worked more days, indirectly suggesting that impaired coping may be a catalyst for persistent sick leave [25].
General practitioner-related associations
The included qualitative studies demonstrated that a positive therapeutic alliance based on prior knowledge, trust, and sympathy for the patient [14], supplemented with a broad insight into patients’ private and working conditions [14, 22], could ease the doctors’ decision to grant sick leave. Seeing a clear purpose of the sick leave or seeing the patient as more “vulnerable” and in need of a “time-out” [14] were also reported as phenomena that could be associated with the doctors’ motivation to prescribe sick leave.
Analysis of the qualitative studies disclosed that even the GPs’ personal needs could be associated with the decision to sick-list MUPS patients. If they felt “stuck” with the patient, sick leave could be granted so that the GP could gain a breathing space [21]. Also being short of time in the consultation setting could make the GPs give in to patients’ demand for sick leave [14]. The studies suggested that the lack of objective signs, pathological [22] as well as functional [14], made decisions more difficult. Identifying an objective sign, even subtle, was said to ease the process towards sick-listing.
Three RCTs explored the outcome of different treatment strategies for MUPS patients, but none of them reduced sick leave [23,24,26]. One study provided three home visits by specially trained “disclosure doctors” to see if disclosures of emotionally important events in the patient's life could improve subjective health and reduce sick leave in MUPS patients [24]. A second study used a specific training programme for GPs to enhance their psychosocial competence [26], and a third study provided an extensive educational programme designed to improve the diagnosing and treatment of patients with functional disorders [23].
Discussion
In this systematic review we report and summarize phenomena associated with sick leave among MUPS patients. On the patient level, we found an association between sick leave and psychiatric comorbidity as well as total symptom burden. For the doctors, knowledge about the patient, sympathy, and trust seem to increase the probability for the patient to be sick-listed. None of the interventions in the educational programmes aiming to improve doctors’ management of MUPS patients lowered sick-leave rates.
The association between sick leave and psychiatric comorbidity in MUPS patients is not necessarily a causal relationship, but may be bi-directional. In a longitudinal study, Hotopf et al. demonstrated that patients with a predominantly mental disorder were likely to develop several physical symptoms over the years, while three or more initially predominant physical symptoms were equally predictive of the onset of a psychiatric disorder some years later [35]. The probability of psychiatric comorbidity increases proportionally with numbers of symptoms in MUPS patients [1,36], corresponding with our finding that the most severely burdened MUPS patients are also the most work limited. About 50–70% of patients with a diagnosable psychiatric disorder initially present with somatic symptoms to their GP [37], which may obscure the underlying psychiatric distress leading to undetected and untreated psychiatric disease. Conversely, it has been reported that identification of psychiatric illness may be higher if physical symptoms are unexplained rather than explained [38].
Nevertheless, MUPS should not be regarded as a psychiatric disorder in disguise. Only 20% of patients with a single MUPS are diagnosed with current psychological illness [39]. The majority of patients with MUPS do not have psychiatric comorbidity [40], and neither somatized mental distress nor somatization disorders adequately account for most patients seen with MUPS in primary care [1]. Burton dismiss the notion that MUPS are expressions of a simple somatization process (particularly the somatization of mental distress), or are due to a somatization disorder that can be defined primarily in terms of numbers of symptoms.
This does not mean, however, that psychological factors are without significance in this group. Harris et al. found that patients with somatization had substantially greater functional disability and role impairment than non-somatizing patients, even after adjusting the results for psychiatric and medical comorbidity [30]. Also Barsky et al. describe how somatizing independently influences medical care utilization and annual costs after adjusting for both psychiatric and medical comorbidity [41].
It is a consistent finding in previous research that the higher the number of pain sites, the more severe are the associated physical, psychological, and social problems [42]. This association remains across different societies and cultures [40] and appears to be established during childhood and adolescence [43]. This reflects the finding of the current review that increasing symptom burdens increases the work limitation.
The current literature on the association between objective findings and sick-listing is scarce and conflicting. Normen et al. found that complaints judged to be non-somatic enhance the risk of sickness certification [44], while the participating GPs in a recent Norwegian focus-group study indicated a higher level in terms of reluctance to grant sick-listing when lacking objective proof of disability [14]. GPs’ personal needs like gaining a break from the patient or the limited time per patient at the encounter also seemed to influence sick listing. Furthermore, Linton et al. reported that doctors with high levels of fear avoidance had a higher risk of believing sick leave to be a good treatment for patients with back pain than doctors with a low level of fear avoidance [45].
GPs have often known their patients for years and have established a close relationship with them. In previous studies, GPs have reported the maintenance of their relationship with their patient as more important than challenging cognitions about illness and work in relation to sick-leave negotiations [46–48]. The process of sick-listing is complex in many ways and the GP's dual role as gatekeeper and health care provider is perceived as conflicting on several levels [49].
In some studies, the researchers have suggested more training in the sick-listing process [50,51]. This could potentially improve understanding of the MUPS patients and then result in better treatment and reduced sick leave. However, none of the included studies in this review showed any effect on different educational programmes for GPs, which is in line with most interventions on health care providers treating back pain patients [52].
Strengths and limitations
A systematic search strategy was employed in the current review with few language restrictions. Cooperation with an academic librarian enhanced the quality of the search. There were no serious disagreements in the inclusion and appraisal processes, and the minor discussions that took place were not recorded.
Nine of the included studies were cross-sectional studies, which cannot imply causality, and no longitudinal studies were found. Qualitative studies could be missing from our search since indexing of qualitative research in medical databases seems to have a potential for improvement [53]. The number of relevant studies was surprisingly low, which in itself is an interesting finding.
The main limitation of the present review is that the designs, patient populations, and outcome measures differ across included studies. This heterogeneity made the synthesis of results challenging. However, there is general agreement that including qualitative studies in systematic reviews is legitimate and potentially has advantages [54]. There are different ways to integrate both quantitative and qualitative studies in a systematic review [55,56]. The qualitative studies included were too limited for conduction of a formal synthesis or meta-ethnography.
Including specific syndrome diagnoses such as fibromyalgia, low back pain, or chronic fatigue syndrome in our search strategy would have increased the number of studies identified. In this study, however, we specifically wanted to include studies where the overarching label of MUPS or comparable terms had been applied. An extension to syndrome diagnoses would have increased the heterogeneity of the included studies even more and one would question whether all patients studied could be regarded as a common group of patients.
The inconsistency in terms used on the patient group is challenging and a potential bias of this study. It might for example be objected that somatoform disorders are something other than MUPS. Based on our thorough assessment of the included studies, we consider all included studies to be related to comparative patient groups characterized by physical symptoms without objective markers of disease. MUPS, MUS, and SHC are broad descriptive terms, whereas Multisomatoform Disorders are based on numbers of symptoms, and even somatizing has several definitions [57,58]. Some will claim that somatizing represents a single psychiatric diagnosis while others use MUPS and somatizing synonymously [22]. In the European Working Group on MUPS [59], as in several of the included studies [23,24, 29–33], MUPS is used synonymously with somatization. We chose the MUPS term because we found it descriptive without indicating any reasons for the symptoms, still emphasizing that “unexplained” is not the same as “unexplainable”. Through lack of a general agreement on a descriptive term for these patients, we made pragmatic choices for our search strategy as presented in Figure 1.
No studies described workplace-related associations between MUPS and sick leave. From a clinical point of view, we experienced that MUPS, psychosocial context, and working conditions together contribute to the sickness certification process. We believe that the lack of studies focusing on the impact of the workplace in the process of sick-listing MUPS patients and the limited literature on GP-related associations should encourage future research. The present study has also revealed a need for a more unified definition of this patient group.
Acknowledgement
The authors would like to thank medical librarians Regina Küfner Lein and Hilde Strøm for search advice, Lillebeth Larun (PT,PhD) for methodological advice, and Brona Fullen (PT, PhD) for linguistic advice.
Declaration of interest
The authors report no conflict of interest. The authors alone are responsible for the content and writing of the paper.
Source of funding
Fund for research in general practice, Norwegian Medical Association.
References
- 1.Burton C. Beyond somatisation: A review of the understanding and treatment of medically unexplained physical symptoms (MUPS) Br J Gen Pract. 2003;53:231–9. [PMC free article] [PubMed] [Google Scholar]
- 2.Creed F, Guthrie E, Fink P, Henningsen P, Rief W, Sharpe M, et al. Is there a better term than “medically unexplained symptoms”? J Psychosom Res. 2010;68:5–8. doi: 10.1016/j.jpsychores.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 3.Fink P, Schroder A. One single diagnosis, bodily distress syndrome, succeeded to capture 10 diagnostic categories of functional somatic syndromes and somatoform disorders. J Psychosom Res. 2010;68:415–26. doi: 10.1016/j.jpsychores.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 4.Barsky AJ, Borus JF. Functional somatic syndromes. Ann Intern Med. 1999;130:910–21. doi: 10.7326/0003-4819-130-11-199906010-00016. [DOI] [PubMed] [Google Scholar]
- 5.Eriksen HR, Ursin H. Sensitization and subjective health complaints. Scand J Psychology. 2002;43:189–96. doi: 10.1111/1467-9450.00286. [DOI] [PubMed] [Google Scholar]
- 6.Bruusgaard D, Natvig B. [Unclear conditions – common mechanisms?] Tidsskr Nor Laegeforen. 2009;129:1481–3. doi: 10.4045/tidsskr.08.0667. [DOI] [PubMed] [Google Scholar]
- 7.Wadell G. Preventing incapacity in people with musculoskeletal disorders. Br Med Bull. 2006:77–8. doi: 10.1093/bmb/ldl008. [DOI] [PubMed] [Google Scholar]
- 8.Ursin H, Eriksen HR. Cognitive activation theory of stress (CATS) Neurosci Biobehav Rev. 2010;34:877–81. doi: 10.1016/j.neubiorev.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 9.Ihlebaek C, Brage S, Eriksen HR. Health complaints and sickness absence in Norway, 1996–2003. Occup Med–Oxford. 2007;57:43–9. doi: 10.1093/occmed/kql107. [DOI] [PubMed] [Google Scholar]
- 10.Brage S, Kann I. Fastlegers sykemeldingspraksis I: Variasjoner [General practitioners’ sickness certification practices] RTV-rapport 2006/04. available from http://www.nav.no/For siden/_attachment/1073745851?=true&_ts=10cd428e448, (in Norwegian) [Google Scholar]
- 11.Bakker IM, Terluin B, van Marwijk HWJ, van der Windt DAWM, Rijmen F, van Mechelen W, et al. A cluster-randomised trial evaluating an intervention for patients with stress-related mental disorders and sick leave in primary care. PLoS Clinical Trials. 2007 doi: 10.1371/journal.pctr.0020026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wahlström R, Alexanderson K. Physicians’ sick-listing practices: Sickness absence – causes, consequences and physicians’ certification practice. A systematic literature review by the Swedish Council on Technology asessment in Health Care. Scand J Prim Health Care. 2004;32((Suppl 63)):6–11. [Google Scholar]
- 13.Engblom M, Nilsson G, Arrelöv B, Löfgren A, Skånér Y, Lindholm C, et al. Frequency and severity of problems that general practitioners experience regarding sickness certification. Scand J Prim Health Care. 2011;29:227–33. doi: 10.3109/02813432.2011.628235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nilsen S, Werner EL, Maeland S, Eriksen HR, Magnussen LH. Considerations made by the general practitioner when dealing with sick-listing of patients suffering from subjective and composite health complaints. Scand J Prim Health Care. 2011;29:7–12. doi: 10.3109/02813432.2010.514191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kato K, Sullivan PF, Evengard B, Pedersen NL. A population-based twin study of functional somatic syndromes. Psychol Med. 2009;39:497–505. doi: 10.1017/S0033291708003784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reme SE, Tangen T, Moe T, Eriksen HR. Prevalence of psychiatric disorders in sick listed chronic low back pain patients. Eur J Pain. 2011;15:1075–80. doi: 10.1016/j.ejpain.2011.04.012. [DOI] [PubMed] [Google Scholar]
- 17.Spiller R, Aziz Q, Creed F, Emmanuel A, Houghton L, Hungin P, et al. Guidelines on the irritable bowel syndrome: Mechanisms and practical management. Gut. 2007;56:1770–98. doi: 10.1136/gut.2007.119446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roelen CA, Koopmans PC, Groothoff JW. Subjective health complaints in relation to sickness absence. Work: J Prevention, Assessment & Rehabilitation. 2010;37:15–21. doi: 10.3233/WOR-2010-1052. [DOI] [PubMed] [Google Scholar]
- 19.Hayden JA, Cote P, Bombardier C. Evaluation of the quality of prognosis studies in systematic reviews. Ann Intern Med. 2006;144:427–37. doi: 10.7326/0003-4819-144-6-200603210-00010. [DOI] [PubMed] [Google Scholar]
- 20.Malterud K. Qualitative research: Standards, challenges, and guidelines. Lancet. 2001;358:483–8. doi: 10.1016/S0140-6736(01)05627-6. [DOI] [PubMed] [Google Scholar]
- 21.Ringsberg KC, Krantz G. Coping with patients with medically unexplained symptoms: Work-related strategies of physicians in primary health care. J Health Psychol. 2006;11:107–16. doi: 10.1177/1359105306058853. [DOI] [PubMed] [Google Scholar]
- 22.Woivalin T, Krantz G, Mantyranta T, Ringsberg KC. Medically unexplained symptoms: Perceptions of physicians in primary health care. Fam Pract. 2004;21:199–203. doi: 10.1093/fampra/cmh217. [DOI] [PubMed] [Google Scholar]
- 23.Rosendal M, Olesen F, Fink P, Toft T, Sokolowski I, Bro F. A randomized controlled trial of brief training in the assessment and treatment of somatization in primary care: Effects on patient outcome. Gen Hosp Psychiatry. 2007;29:364–73. doi: 10.1016/j.genhosppsych.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 24.Schilte AF, Portegijs PJ, Blankenstein AH, van Der Horst HE, Latour MB, van Eijk JT, et al. Randomised controlled trial of disclosure of emotionally important events in somatisation in primary care. BMJ. 2001;323:86. doi: 10.1136/bmj.323.7304.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thorslund KW. Solution-focused group therapy for patients on long-term sick leave: A comparative outcome study. J Fam Psychother. 2007:11–24. [Google Scholar]
- 26.Larisch A, Fisch V, Fritzsche K. Cost-effectiveness of psychosocial interventions for somatising patients by the general practitioner [in German] J Psychosom Res. 2004;57:507–14. doi: 10.1016/j.jpsychores.2004.04.372. [DOI] [PubMed] [Google Scholar]
- 27.Al-Windi A. The influence of complaint symptoms on health care utilisation, medicine use, and sickness absence: A comparison between retrospective and prospective utilisation. J Psychosom Res. 2005;59:139–46. doi: 10.1016/j.jpsychores.2005.02.012. [DOI] [PubMed] [Google Scholar]
- 28.Gulbrandsen P, Hjortdahl P, Fugelli P. Work disability and health-affecting psychosocial problems among patients in general practice. Scand J Soc Med. 1998;26:96–100. doi: 10.1177/14034948980260020801. [DOI] [PubMed] [Google Scholar]
- 29.Gureje O, Simon GE, Ustun TB, Goldberg DP. Somatization in cross-cultural perspective: A World Health Organization study in primary care. Am J Psychiatry. 1997;154:989–95. doi: 10.1176/ajp.154.7.989. [DOI] [PubMed] [Google Scholar]
- 30.Harris AM, Orav EJ, Bates DW, Barsky AJ. Somatization increases disability independent of comorbidity. J Gen Intern Med. 2009;24:155–61. doi: 10.1007/s11606-008-0845-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoedeman R, Blankenstein AH, Krol B, Koopmans PC, Groothoff JW. The contribution of high levels of somatic symptom severity to sickness absence duration, disability and discharge. J Occup Rehabil. 2010;20:264–73. doi: 10.1007/s10926-010-9239-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hoedeman R, Krol B, Blankenstein N, Koopmans PC, Groothoff JW. Severe MUPS in a sick-listed population: A cross-sectional study on prevalence, recognition, psychiatric co-morbidity and impairment. BMC Public Health. 2009;9:440. doi: 10.1186/1471-2458-9-440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kroenke K, Spitzer RL, Williams JBW. The PHQ-15: Validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64:258–66. doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Muller JE, Wentzel I, Nel DG, Stein DJ. Depression and anxiety in multisomatoform disorder: Prevalence and clinical predictors in primary care. S Afr Med J. 2008;98:473–6. [PubMed] [Google Scholar]
- 35.Hotopf M, Mayou R, Wadsworth M, Wessely S. Temporal relationships between physical symptoms and psychiatric disorder: Results from a national birth cohort. Br J Psychiatry. 1998;173:255–61. doi: 10.1192/bjp.173.3.255. [DOI] [PubMed] [Google Scholar]
- 36.Wessely S, Chalder T, Hirsch S, Wallace P, Wright D. Psychological symptoms, somatic symptoms, and psychiatric disorder in chronic fatigue and chronic fatigue syndrome: A prospective study in the primary care setting. Am J Psychiatry. 1996;153:1050–9. doi: 10.1176/ajp.153.8.1050. [DOI] [PubMed] [Google Scholar]
- 37.Barsky AJ, Borus JF. Somatization and medicalization in the era of managed care. JAMA. 1995;274:1931–4. [PubMed] [Google Scholar]
- 38.Kisely S, Goldberg D, Simon G. A comparison between somatic symptoms with and without clear organic cause: Results of an international study. Psychol Med. 1997;27:1011–19. doi: 10.1017/s0033291797005485. [DOI] [PubMed] [Google Scholar]
- 39.Fink P, Sorensen L, Engberg M, Holm M, Munk-Jorgensen P. Somatization in primary care: Prevalence, health care utilization, and general practitioner recognition. Psychosomatics. 1999;40:330–8. doi: 10.1016/S0033-3182(99)71228-4. [DOI] [PubMed] [Google Scholar]
- 40.Gureje O, Von Korff M, Kola L, Demyttenaere K, He YL, Posada-Villa J, et al. The relation between multiple pains and mental disorders: Results from the World Mental Health Surveys. Pain. 2008;135:82–91. doi: 10.1016/j.pain.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 41.Barsky AJ, Orav EJ, Bates DW. Somatization increases medical utilization and costs independent of psychiatric and medical comorbidity. Arch Gen Psychiatry. 2005;62:903–10. doi: 10.1001/archpsyc.62.8.903. [DOI] [PubMed] [Google Scholar]
- 42.Kamaleri Y, Natvig B, Ihlebaek CM, Bruusgaard D. Localized or widespread musculoskeletal pain: Does it matter? Pain. 2008;138:41–6. doi: 10.1016/j.pain.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 43.Larsson B, Sund AM. Emotional/behavioural, social correlates and one-year predictors of frequent pains among early adolescents: Influences of pain characteristics. Eur J Pain. 2007;11:57–65. doi: 10.1016/j.ejpain.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 44.Norrm n G, Sv rdsudd K, Andersson DK. How primary health care physicians make sick listing decisions: The impact of medical factors and functioning. BMC Fam Pract. 2008:9–3. doi: 10.1186/1471-2296-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Linton SJ, Vlaeyen J, Ostelo R. The back pain beliefs of health care providers: Are we fear-avoidant? J Occup Rehabil. 2002;12:223–32. doi: 10.1023/a:1020218422974. [DOI] [PubMed] [Google Scholar]
- 46.Campbell A, Ogden J. Why do doctors issue sick notes? An experimental questionnaire study in primary care. Fam Pract. 2006;23:125–30. doi: 10.1093/fampra/cmi099. [DOI] [PubMed] [Google Scholar]
- 47.Chew-Graham C, May C. Chronic low back pain in general practice: The challenge of the consultation. Fam Pract. 1999;16:46–9. doi: 10.1093/fampra/16.1.46. [DOI] [PubMed] [Google Scholar]
- 48.Hussey S, Hoddinott P, Wilson P, Dowell J, Barbour R. Sickness certification system in the United Kingdom: Qualitative study of views of general practitioners in Scotland. BMJ. 2004;328:88–91. doi: 10.1136/bmj.37949.656389.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wynne-Jones G, Mallen CD, Main CJ, Dunn KM. What do GPs feel about sickness certification? A systematic search and narrative review. Scand J Prim Health Care. 2010;28:67–75. doi: 10.3109/02813431003696189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wynne-Jones G, Mallen CD, Main CJ, Dunn KM. Sickness certification and the GP: What really happens in practice? Fam Pract. 2010;27:344–50. doi: 10.1093/fampra/cmp096. [DOI] [PubMed] [Google Scholar]
- 51.Roope R, Parker G, Turner S. General practitioners’ use of sickness certificates. Occup Med–Oxford. 2009;59:580–5. doi: 10.1093/occmed/kqp147. [DOI] [PubMed] [Google Scholar]
- 52.Werner EL, Gross DP, Lie SA, Ihlebaek C. Healthcare provider back pain beliefs unaffected by a media campaign. Scand J Prim Health Care. 2008;26:50–6. doi: 10.1080/02813430801905664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dixon-Woods M, Fitzpatrick R, Roberts K. Including qualitative research in systematic reviews: Opportunities and problems. J Eval Clin Pract. 2001;7:125–33. doi: 10.1046/j.1365-2753.2001.00257.x. [DOI] [PubMed] [Google Scholar]
- 54.Thomas J, Harden A, Oakley A, Oliver S, Sutcliffe K, Rees R, et al. Integrating qualitative research with trials in systematic reviews. BMJ. 2004;328:1010–2. doi: 10.1136/bmj.328.7446.1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;10:45. doi: 10.1186/1471-2288-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sandelowski M, Barroso J, Voils CI. Using qualitative metasummary to synthesize qualitative and quantitative descriptive findings. Res Nurs Health. 2007;30:99–111. doi: 10.1002/nur.20176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rosendal M, Fink P, Bro F, Olesen F. Somatization, heartsink patients, or functional somatic symptoms? Towards a clinical useful classification in primary health care. Scand J Prim Health Care. 2005;23:3–10. doi: 10.1080/02813430510015304. [DOI] [PubMed] [Google Scholar]
- 58.Lipowski ZJ. Somatization: The concept and its clinical application. Am J Psychiatry. 1988;145:1358–68. doi: 10.1176/ajp.145.11.1358. [DOI] [PubMed] [Google Scholar]
- 59.Henningsen P, Creed F. Patients with medically unexplained symptoms and somatisation: A challenge for European health care systems. 2009 [Google Scholar]