Abstract
There is a debate among medical education experts on the application of dissection or prosection for learning anatomy. However, the literature reveals that the majority of published articles are in favor of dissection. In this article, we present a case of an abdominal aortic aneurysm (AAA) with intracardiac thrombus in a cadaver on routine dissection. We will discuss possible explanations for such finding and provide some insight into how this finding can support the significance of the cadaver-based teaching of anatomy of the medical students. Initially, the abdomen was dissected and exposed to study the abdominal structures in an anatomy class and later the thoracic region was dissected and all the clinical abnormalities were examined and documented. Autopsy of the clot was obtained for histopathology analysis. The intracardiac thrombus was present in the right atrium characterized by its projection into the superior vena cava, inferior vena cava, and the right ventricle. The AAA was extensive and inferior to the renal arteries constricting the entire inferior vena cava. Moreover, associated findings included presence of numerous collaterals in the thoracic region near the superior vena cava; histological examination of the clot showed extensive population of leukocytes. There were enlarged mediastinal lymph nodes. Our cadaver showed an excellent model for integrating between clinical anatomy and pathology by triggering medical students to think of normal and abnormal structures: often called “thinking outside the box.” Such an effort might help them in developing their thought processes and future medical careers.
Keywords: medical education, dissection, student-centered learning, intracardiac thrombus
There is a debate among medical education experts on the application of dissection or prosection for learning clinical anatomy.1 This debate intensified when some universities (e.g., Peninsula Medical School in the United Kingdom) introduced the teaching of anatomy without the use of cadavers while others taught anatomy only through short courses using prosected cadavers.2 Many of the universities that abandoned dissection came back to teaching anatomy through dissection.3 The reasons for this include: (1) inadequate student understanding of the anatomical arrangement of the human body that became apparent in the clinical years and (2) the mini lectures accompanying prosected cadaver examination short-changed student-centered enquiry and exploration with many students choosing dissection courses as an elective.3 Rizzolo and Stewart3 further argue that dissection allows for integration of imaging and physical diagnosis as well as sets the bases for clinical skills of “observation/history taking to discover facts; interpretation of findings to develop a differential diagnosis; and development/execution of a management plan.” Dissection experience also teaches students that there can be variability of blood vessels, muscles, sutures, etc., which provides a valuable experience for future diagnostic practice.4
Most schools, including ours,5 teach gross anatomy in a clinically relevant fashion, sometimes focusing on the clinical utility of anatomy.6 We have found that cadaver dissection correlates well with the problem-based learning (PBL) method of teaching that is currently adopted by our institution. We have found that the dissection laboratory offers many opportunities for integrating many of the basic medical science subjects as well as with clinical sciences, which is also the aim of the PBL modules. For example, we reported previously on another cadaver with persistent bilateral sciatic artery,7 which was identified by the students as an abnormal finding, but in fact they developed a new concept early in their medical career that abnormalities are related to malfunctioning developmental programs.
In this article we demonstrate how one cadaver being dissected at Alfaisal University resulted in a better understanding of vascular histology by encountering an abdominal aneurysm and the clotting cascade by encountering an intracardiac thrombus that extended into the pulmonary trunk as well as superior and inferior venae cavae. This finding reinforced the understanding of what governs the clotting cascade that was being taught in the physiology and molecular medicine courses and, thus, setting the stage for the students' pathology course to be taken in the following year.
Method
Our cadavers were obtained from Germany. The cadavers were maintained at 10°C and kept moist with water containing 4% of formaldehyde. The anterior abdominal wall was dissected in the typical manner and exposed for studying the abdominal structures. Later the thoracic region was dissected as well and all the clinical abnormalities encountered were examined and documented. Autopsy of the thrombus found was obtained for histopathology analysis with paraffin embedding, sectioning, staining with hematoxylin and eosin, and then examined microscopically.
Results
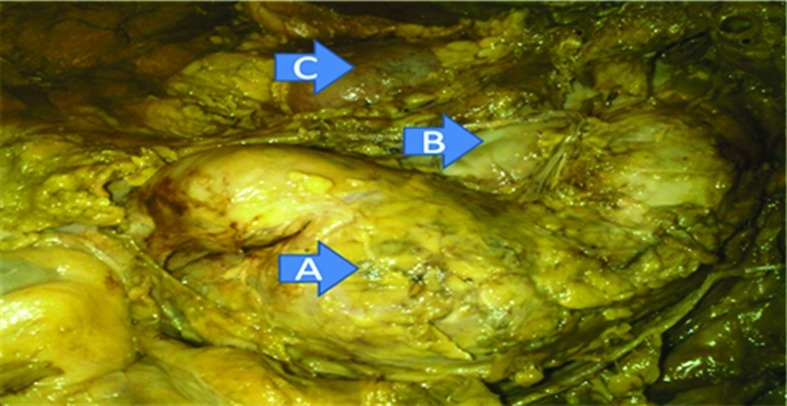
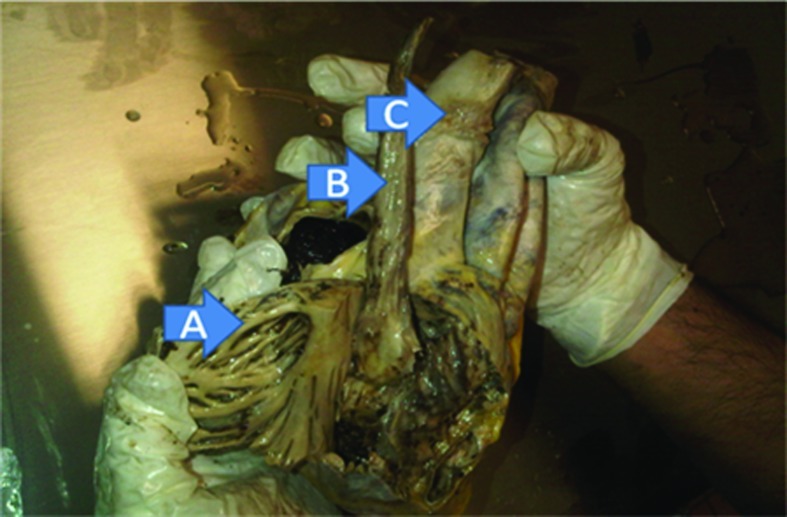
In the abdominal area, an extensive abdominal aortic aneurysm (AAA), inferior to the renal arteries was observed. This was associated with compression of the inferior vena cava (Fig. 1). Moreover, in the thoracic region, the heart was enlarged and numerous collateral veins were seen in the thoracic region, along with enlarged mediastinal lymph nodes. Dissection of the heart revealed a large mass in the right atrium arising from the inter-atrial wall with projections into the superior vena cava, inferior vena cava, and the right ventricle extending into the pulmonary arteries (Figs. 2 and 3). The histopathological analysis demonstrated that this was a well-established thrombus that showed large accumulations of leukocytes (Fig. 4), predominantly neutrophils, and lower numbers of macrophages.
Figure 1.
(A) Gross appearance of abdominal aortic aneurysm (AAA) inferior to the renal arteries. (B) The aneurysm is compressing on the anterior side of the inferior vena cava which may cause stagnation of blood flow. (C) Right kidney.
Figure 2.
(A) exposed right atrium and appearance of the musculi pectinati. (B) Gross appearance of the blood clot lateral to the superior vena cava (C).
Figure 3.
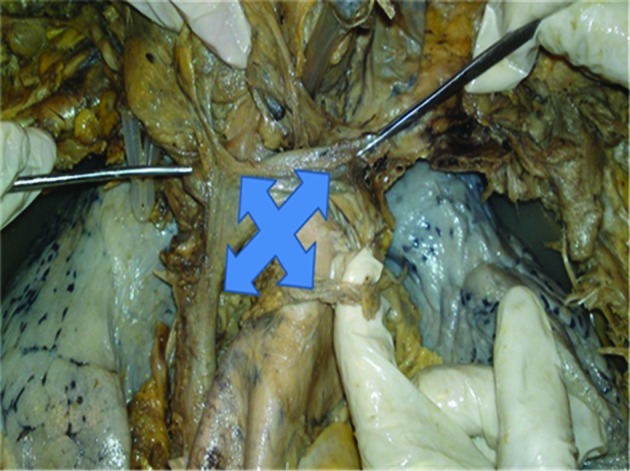
Appearance of extensive collaterals in the thorax near the superior vena cava as alternative mean for conducting blood to areas suffering less blood flow.
Figure 4.
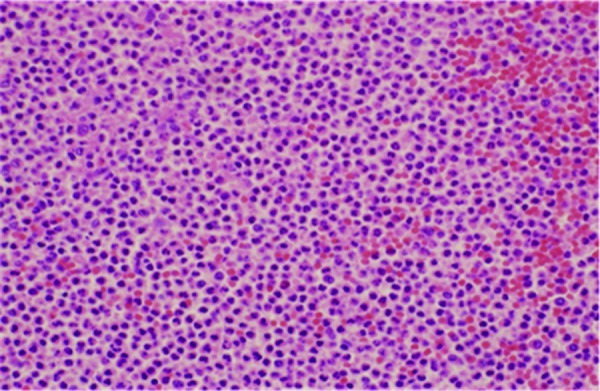
Section of the clot showed extensive infiltration of neutrophils indicating inflammation.
Associated findings included absence of left kidney, a large shunt from the femoral vein to the subclavian vein, an endovascular stent extending to the abdominal aorta, and discoloration of the right side of the body with prominent appearance of capillaries on the top of the skull.
Discussion
This cadaver offered multiple opportunities for students to integrate various basic medical sciences. Obvious problems included AAA, a femoral-subclavian venous shunt, enlarged heart, intracardiac thrombus, enlarged mediastinal lymph nodes, and supernumerary thoracic veins.
The presence of an abdominal aneurysm reinforced knowledge on the histological composition of arteries and how deficiencies in the protein fibrous network can result in localized ballooning in response to arterial pressure, thus, reinforcing physiological concepts such as how cardiac output, vascular resistance, and vascular compliance are related to blood pressure.
The presence of an intracardiac thrombus within the right atrium extending into the venae cavae and via the right ventricle into the pulmonary trunk offered multiple opportunities to integrate knowledge. The presence of numerous leukocytes suggests that this occurred relatively slowly antemortem; possibly in response to an infection. Most intracardiac thrombi found at necropsy are present in the left ventricle followed by right ventricle, then right atrium and least common in the left atrium.8 The European Cooperative Study on the clinical significance on right cardiac thrombi categorized the most common as being mobile and serpentine in shape and likely due to mobilization of a deep vein thrombus (DVT) and a less common nonmobile and nonserpentine thrombus.9 The presence of a femoral-subclavian vein shunt suggests the possibility that the thrombus found in this cadaver may be a dislodged DVT that secondarily became attached to the interatrial wall in the right ventricle. The large number of leukocytes in the clot is suggestive of an inflammatory problem in the vicinity of the clot.
The observations of the thrombus focused students' attention on blood clotting mechanisms, which were covered in their molecular medicine and physiology courses. How deep vein blood stasis promotes blood clotting and the role of turbulence in promoting clotting remained interesting question. Further, the observation of an intracardiac thrombus emphasized the importance of the roles of protein S, protein C, and factor V in limiting the extent of clotting and suggesting there may be some problem with limiting the clotting cascade. Reinforcing the integration of information was that the students during this time were also engaged in a PBL module based on a case report10 on a patient heterozygous for Factor V Leiden and G20210A prothrombin genotypes.
Finally, the findings in this cadaver can also be used in the pathology studies, which the students will encounter in their second year. For example, one possible topic can be discussed that how in antiphospholipid syndrome minor alterations in clotting, infection, or other stresses may result in clotting problems.11 Indeed, a clot finding similar to ours has been reported.12
In conclusion, this study clearly shows the benefit of student-directed dissection in learning clinical anatomy. It is recommended that medical schools should continue to use cadaver as one of the teaching modalities in anatomy for its students. The abnormalities of structures can act as trigger. Students get an opportunity to be engaged in the problem-solving exercise.
Acknowledgment
The authors are grateful to Prof. Khaled Al-Kattan for his continuous support to make the dissection laboratory at the Department of Anatomy as one of the student-centered activities at Alfaisal Univesity.
References
- 1.McLachlan J C, Patten D. Anatomy teaching: ghosts of the past, present and future. Med Educ. 2006;40(3):243–253. doi: 10.1111/j.1365-2929.2006.02401.x. [DOI] [PubMed] [Google Scholar]
- 2.McLachlan J C, Bligh J, Bradley P, Searle J. Teaching anatomy without cadavers. Med Educ. 2004;38(4):418–424. doi: 10.1046/j.1365-2923.2004.01795.x. [DOI] [PubMed] [Google Scholar]
- 3.Rizzolo L J, Stewart W B. Should we continue teaching anatomy by dissection when …? Anat Rec B New Anat. 2006;289(6):215–218. doi: 10.1002/ar.b.20117. [DOI] [PubMed] [Google Scholar]
- 4.Korf H W, Wicht H, Snipes R L. et al. The dissection course—necessary and indispensable for teaching anatomy to medical students. Ann Anat. 2008;190(1):16–22. doi: 10.1016/j.aanat.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 5.Cowan M, Arain N N, Assale T S, Assi A H, Albar R A, Ganguly P K. Student-centered integrated anatomy resource sessions at Alfaisal University. Anat Sci Educ. 2010;3(5):272–275. doi: 10.1002/ase.176. [DOI] [PubMed] [Google Scholar]
- 6.Boeckers A, Fassnacht U, Boeckers T M. “Theatrum anatomicum”—a revived teaching facility in gross anatomy. Ann Anat. 2008;190(6):495–501. doi: 10.1016/j.aanat.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 7.Cowan M, Hamweyah K M, Sabbagh M D, Swaid B A, Al Kattan A K, Ganguly P K. Persistent bilateral sciatic artery: report of a rare case. Int J Angiol. 2010;19:e43–e44. doi: 10.1055/s-0031-1278363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Waller B F, Grider L, Rohr T M, McLaughlin T, Taliercio C P, Fetters J. Intracardiac thrombi: frequency, location, etiology, and complications: a morphologic review—part I. Clin Cardiol. 1995;18(8):477–479. doi: 10.1002/clc.4960180811. [DOI] [PubMed] [Google Scholar]
- 9.Thompson C A, Skelton T N. Thromboembolism in the right side of the heart. South Med J. 1999;92(8):826–830. doi: 10.1097/00007611-199908000-00018. [DOI] [PubMed] [Google Scholar]
- 10.Al-Juburi A, Scott M A, Shah H R, Raufman J P. Heterozygosity for factor V Leiden and G20210A prothrombin genotypes in a patient with mesenteric vein thrombosis. Dig Dis Sci. 2002;47(3):601–606. doi: 10.1023/a:1017928421966. [DOI] [PubMed] [Google Scholar]
- 11.Koniari I, Siminelakis S N, Baikoussis N G, Papadopoulos G, Goudevenos J, Apostolakis E. Antiphospholipid syndrome; its implication in cardiovascular diseases: a review. J Cardiothorac Surg. 2010;5:101. doi: 10.1186/1749-8090-5-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Permanyer E, Alegret J M, Muñoz-Guijosa C, Padró J M. Inferior vena cava obstruction by a cardiac mass: unusual presentation of primary antiphospholipid syndrome. Thorac Cardiovasc Surg. 2011;59(3):182–183. doi: 10.1055/s-0030-1250501. [DOI] [PubMed] [Google Scholar]