Abstract
Although less common than adult fractures, fractures of the pediatric maxillofacial skeleton present unique challenges. Different considerations including variations of anatomy including tooth buds, dental variations, as well as considerations for future growth must be addressed. When traditional techniques to treat adult fractures are applied for securing intermaxillary fixation (IMF) such as arch bars, difficulty arises because the primary teeth are shorter and conventional arch bar techniques may slip off intra or postoperatively. We present a technique to achieve both IMF as well as interdental stability using a Risdon cable. Although this technique is not new, we present it as our preferred method for treating pediatric fractures of the facial skeleton where IMF must be accomplished.
Keywords: pediatric, maxillofacial, trauma
Fractures in the pediatric and mixed dentition phases of development present unique surgical challenges. Not only are there different anatomical considerations, there are also different physiological factors that affect wound healing, fracture stability, and growth of the facial bones. Although less common than adult fractures, pediatric facial fractures are occasionally encountered. The same surgical approaches and techniques that are used for adults are often inappropriate or cumbersome.
Pediatric mandibular fractures comprise the most frequent type of pediatric maxillofacial fracture presentation (55%) followed by orbital (30%) and dentoalveolar fractures (23%).1 However, it is believed that there is a significant underreporting of dentoalveolar injury in the literature, as these are often managed in a dental office. The most common dentoalveolar injury mechanism is related to organized recreational events, while maxillofacial fractures are most commonly related to motor vehicle accidents. Other mechanisms include falls and interpersonal violence.2,3 Males are twice as likely to be encountered. Maxillary incisors are the most common teeth involved in dental trauma, followed by maxillary lateral incisors.2 Traumatized teeth are treated by replantation and/or repositioning followed by splinting using a semirigid splint typically done with modern dental composite materials. Maxillofacial fractures are treated by first reestablishing the existing occlusion as necessary followed by open reduction internal fixation if necessary.
In patients with adult dentition, the use of arch bar wiring historically has been the default for establishing maxillomandibular fixation (MMF) due to familiarity and ease of use. The deciduous dentition, however, is characterized by short, bulbous crowns making conventional arch bar application and retention difficult. The arch bar and teeth have similar height resulting in the individual circumdental wires slipping off when either MMF is applied intraoperatively or in the recovery room during emergence from anesthesia. An “arch bar” in the form of a Risdon cable provides a useful alternative.4
Technique
Indications for this procedure include patients in primary and mixed dentition that require either a device to stabilize the teeth or to provide an arch bar for MMF. This method was employed originally when arch bars were unavailable.5 It was first described by using a thick 1-mm diameter wire that was twisted around the last molar tooth of the mandible. The ends were then twisted following the contour of the mandible at the cervical margin of the teeth to the midline. This was accomplished bilaterally. The two twisted ends were then twisted together in the symphyseal region to form a substitute arch bar. Ligature wires (35 mm long) were then passed to secure the individual teeth to the bar. This was also done on the maxilla to allow MMF. The technique was originally credited to E. Fulton Risdon, Canada's first plastic surgeon, and thus bears his name (Fig. 1).
Figure 1.
E. Fulton Risdon.
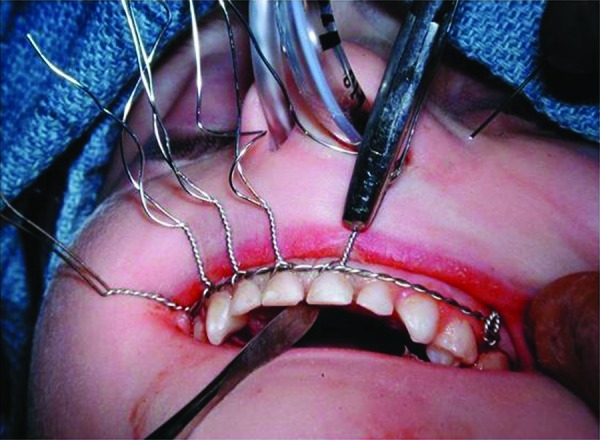
Modifications to this procedure include using 24-gauge stainless steel wire that is passed from the last molar as originally described (Fig. 2). The wire is then twisted from one side of the dental arch to the other (Fig. 3). Ideally, circumdental ligatures are passed to secure the individual teeth as the cable is being twisted (Fig. 4). This will allow for secure fastening of the cable and ligature complex. Finally, when the wires composing the Risdon cable have reached the contralateral molar tooth, it is then secured and the final circumdental ligature is placed. The circumdental wires are cut and twisted in a traditional fashion that will allow loops for securing elastics or wiring to establish MMF or guiding functions (Fig. 5). If elastics are used for MMF, it is most unusual for the Risdon wiring to pull off or otherwise fail as the elastics “give.” Aside from establishing MMF, this procedure may also be used for splinting avulsed or luxated teeth, and may be supplemented with autopolymerizing resin for stability (Fig. 6). Following application of the Risdon cable, open reduction internal fixation may then be performed with the patient in MMF (Fig. 7).
Figure 2.

Initiating the cable by ligating the first molar tooth.
Figure 3.

Securing the cable to the opposing first molar tooth.
Figure 4.
Interdental wiring for stabilization of cable and individual teeth.
Figure 5.

Final wiring of both the maxilla and mandible.
Figure 6.

Stabilization of both cable and teeth using autopolymerizing resin.
Figure 7.
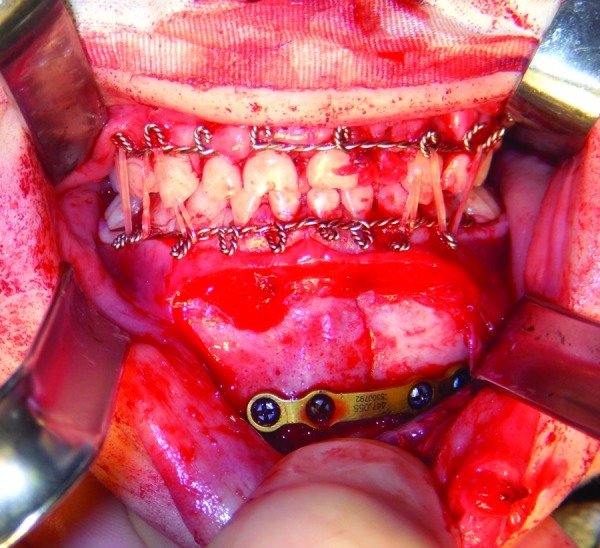
Open reduction internal fixation completed with intermaxillary fixation accomplished using rubber bands and Risdon cables.
Discussion
Risdon cables provide a sturdy yet thin construct that is well adapted to primary teeth, allowing the placement of elastics or wires to be used intra- or postoperatively. Young patients have high osteogenic potential and great potential for remodeling, which allows nonsurgical management to be successful in younger patients with conservative approaches. This becomes especially useful in the management of pediatric dislocated condylar fractures where open surgery has yet to show advantages.6 Adequate occlusal function and guidance may reduce the need for secondary procedures as the facial complex matures. Most concerning is the need for subsequent orthognathic surgery from asymmetry resulting from condylar fracture.7 By using a reliable means of stabilizing both occlusion and dentition using the Risdon cable technique we have had excellent results in managing both maxillofacial fractures as well as dental trauma.
References
- 1.Posnick J C Wells M Pron G E Pediatric facial fractures: evolving patterns of treatment J Oral Maxillofac Surg 1993518836–844., discussion 844–845 [DOI] [PubMed] [Google Scholar]
- 2.Bruns T, Perinpanayagam H. Dental trauma that require fixation in a children's hospital. Dent Traumatol. 2008;24(1):59–64. doi: 10.1111/j.1600-9657.2006.00508.x. [DOI] [PubMed] [Google Scholar]
- 3.Ferreira P C, Amarante J M, Silva A C, Pereira J M, Cardoso M A, Rodrigues J M. Etiology and patterns of pediatric mandibular fractures in Portugal: a retrospective study of 10 years. J Craniofac Surg. 2004;15(3):384–391. doi: 10.1097/00001665-200405000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Risdon F. The treatment of fractures of the jaws. Can Med Assoc J. 1929;20:260–262. [PMC free article] [PubMed] [Google Scholar]
- 5.Rowe N L, Killey H C. Baltimore: Williams and Wilkins; 1968. Fractures of the Facial Skeleton. 2 ed. [Google Scholar]
- 6.Deleyiannis F W, Vecchione L, Martin B, Jiang S, Sotereanos G. Open reduction internal fixation of dislocated condylar fractures in children: long term clinical and radiologic outcomes. Ann Plast Surg. 2006;57(5):495–501. doi: 10.1097/01.sap.0000226943.79337.bf. [DOI] [PubMed] [Google Scholar]
- 7.Schweinfurth J M, Koltai P J. Pediatric mandibular fractures. Facial Plast Surg. 1998;14(1):31–44. doi: 10.1055/s-0028-1085300. [DOI] [PubMed] [Google Scholar]


