Abstract
Mandible fractures commonly occur in patients who have sustained blunt facial trauma, and the subcondylar region is the most frequently fractured due to its intrinsic biomechanical weakness. The maxillary artery lies in close relation to the medial cortex of the subcondyle and is vulnerable to injury by the sharp edges of the fracture fragments during the initial trauma or during operative fracture reduction. Maxillary artery injuries and subcondylar fractures may be an underdiagnosed phenomenon. Yet, this is of clinical significance as the maxillary artery caliber is usually of significant caliber and may lead to substantial hemorrhage. Surgical access to the artery for hemostasis is challenging and is further compounded by small surgical incisions usually undertaken for fracture fixation, obscuring of the artery by the overlying fracture fragments, and vessel retraction following its transection. In cases where maxillary artery injury is suspected, an open surgical approach may be favored over an endoscopic one. The authors illustrate a case in which brisk hemorrhage from the maxillary artery encountered during a preauricular approach to fixation of the mandible subcondyle was successfully controlled with temporary pressure on the external carotid artery through a neck incision and direct ligation of the lacerated maxillary artery. The authors then discuss diagnosis and treatment of such maxillary artery injuries and propose a novel diagnostic and treatment algorithm.
Keywords: subcondylar fractures, maxillary artery injury, maxillary artery pseudoaneurysm, mandible artery hemorrhage in mandible fractures
Mandible fractures are a common occurrence in patients who have sustained blunt facial trauma. The commonest unilateral fracture of the mandible involves the subcondylar region, while the most common bilateral fractures occur at the condylar heads. Previous epidemiological studies have shown that fractures in and around the condylar region to be the most frequent. The shape of the mandible neck predisposes to intrinsic biomechanical weakness and makes this area particularly vulnerable to breaking.1 The maxillary artery lies in close relation to the medial cortex at the subcondylar portion of the mandible2 and is at risk of injury during the initial trauma or subsequent surgery. The maxillary artery is the largest terminal branch of the external carotid artery and hemorrhage often does not respond to digital pressure. In addition, its deep lie and the small incisions normally used for exposing the fractured subcondyle compound the difficulty in securing hemostasis. In difficult cases, ligation of the external carotid artery may be necessary. The authors describe a patient where maxillary artery hemorrhage encountered during subcondylar fracture surgery was successfully managed with direct surgical ligation.
Case Report
A 16-year-old Caucasian adolescent was the driver of a car that collided with a tree. He presented one day later with progressive bilateral facial pain and swelling. Examination noted an anterior open bite and bilateral preauricular swelling, worse on the left than the right (Fig. 1). Computed tomographic (CT) scans of the face showed bilateral mandible subcondylar fractures associated with a minimally displaced symphyseal fracture (Fig. 2). Two days after the accident, it was observed that the swelling on the left side had increased noticeably; this was attributed to fracture hematoma. The patient underwent an elective operative reduction and internal fixation of the mandible fractures the following day. A lower buccal sulcus approach was used for exposure of the symphyseal fracture, and rigid fixation was achieved with a six-hole 2.0-mm locking titanium plate (Matrix Mandible, Synthes, West Chester, PA). The right subcondyle fracture was fixed through a preauricular approach with a five-hole 1.5-mm plate.
Figure 1.

Preoperative photograph of the patient showing left-sided mandible swelling more than right.
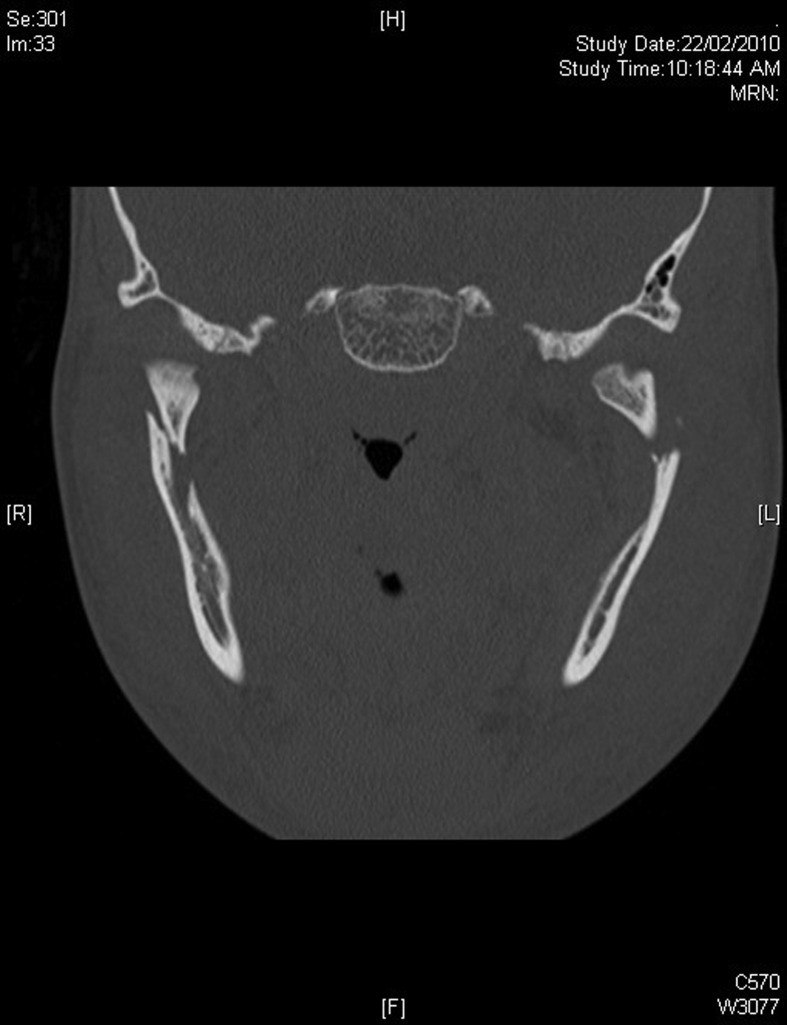
Figure 2.
Coronal view of computed tomographic (CT) scan of the patient showing bilateral mandible subcondylar fractures.
During surgical exposure of the left subcondyle (exposed via a preauricular approach), brisk hemorrhage was encountered that did not stop with direct pressure. The vascular service was consulted and the left external carotid artery was exposed through a neck incision. A silicone vascular loop served as a sling for control of bleeding. Following this, the preauricular wound was again explored and a longitudinal laceration of the maxillary artery was seen. It was probable that this laceration was in contact with the sharp edges of the mandible fracture. The maxillary artery was subsequently surgically ligated and the fracture fixation proceeded uneventfully. A CT arteriogram of the external carotid artery performed on the first postoperative day confirmed the ligation of the maxillary artery (Fig. 3). Distal reconstitution of the arterial flow was observed, and no false aneurysm was seen.
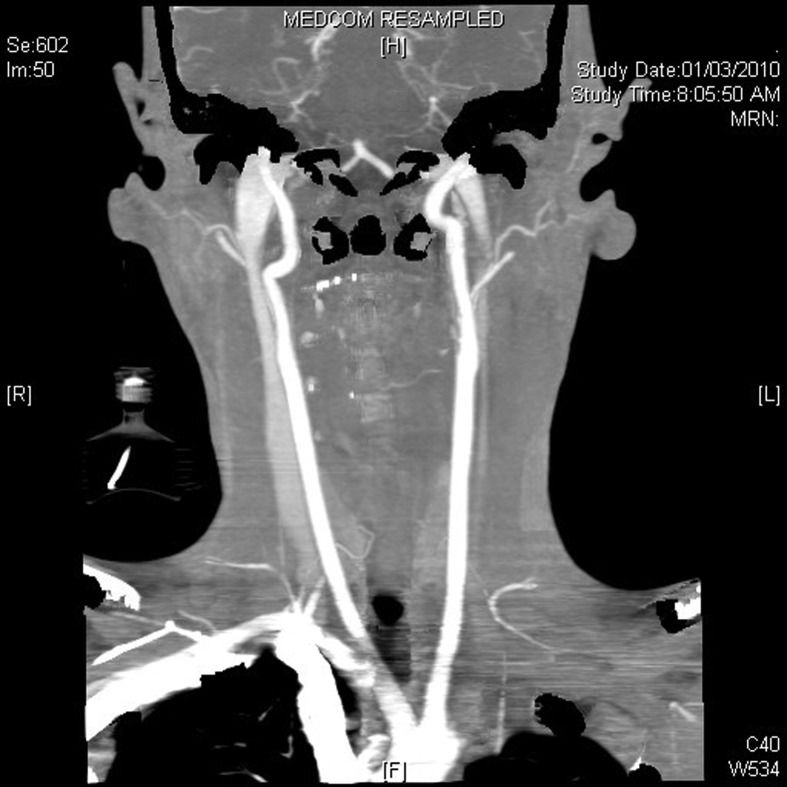
Figure 3.
Computed tomographic (CT) arteriogram of the external carotid system done 24 hours after the surgery confirming successful ligation of the maxillary artery.
The patient was discharged on the second postoperative day and had a favorable postoperative dental occlusion when reviewed in the clinic at 6 months.
Discussion
Mandible fractures occur in males and are most often caused by interpersonal altercations.3 Most fractures occur in the 25- to 34-year-old age group. In children, the mandible is the site of injury in ~40% of pediatric facial trauma cases and is most commonly the result of motor vehicle accidents.4 Previous epidemiological studies have shown the approximate distribution by anatomical region to be condylar (36%), body (21%), angle (20%), symphysis (14%), alveolar ridge (3%), ramus (3%), and coronoid (2%).2
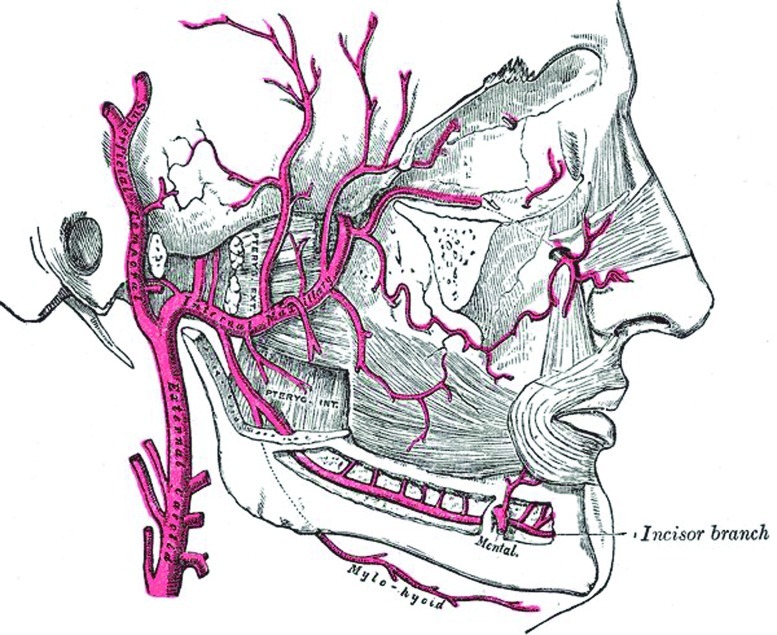
The maxillary artery is divided into three portions based on its relationship to the lateral pterygoid muscle: (1) the mandibular portion (posterior to lower border of lateral pterygoid muscle); (2) the pterygoid portion (deep or superficial to the lateral pterygoid muscle); and (3) the pterygopalatine portion (within the pterygopalatine fossa). The anatomy of the maxillary portion of the maxillary artery has only recently been studied. Based on dissection of cadaveric specimens, Orbay et al5 found that the mean distance of the artery to the medial border of the subcondylar portion of the mandible was 6.8 mm, while the mean distance of the maxillary artery to the tragal pointer was 16.2 mm in the horizontal plane and 21.4 mm in the vertical plane. In this study, significant intra- and interindividual variations were noted. Given the close relation of the first portion of the artery and mandible, it is not surprising that lacerations to the artery may occur here (Fig. 4). A possible mechanism of injury involves a lateral force causing medial displacement of fracture fragments. The maxillary artery, being buttressed medially by soft tissues, remains relatively immobile and is hence lacerated by sharp edges of the fracture fragments. Even if the artery was not injured during the initial trauma, its proximity to the fracture edges puts it in constant danger of being lacerated by subsequent motion of the fractured bone ends. Given the knowledge of the close anatomical relationship of the artery and the mandible, maxillary artery injuries and subsequent hemorrhage are quite possibly underappreciated and underdiagnosed. Such occurrences can be often dismissed as “fracture hematoma” and may lead to a delay in diagnosis and treatment, and may unexpectedly present with torrential bleeding during surgery for the subcondylar fracture.
Figure 4.
Illustration showing anatomy of maxillary artery and hemimandible.
There have been few isolated reports of maxillary artery pseudoaneurysms associated with such fractures.6,7 In all except the first case, presentation of the pseudoaneurysm occurred weeks to months following the initial trauma. Similarly, maxillary artery pseudoaneurysms have been reported following mandibular subcondylar osteotomies.8
It is important to distinguish between a fracture hematoma and maxillary artery pseudoaneurysm preoperatively as there are important surgical consequences. Pseudoaneurysms continue to expand even after 48 hours from the time of the initial injury, unlike typical fracture hematomas, which stabilize in size. When a pseudoaneurysm is suspected, a preoperative angiogram will be useful in diagnosis, as well as determining the surgical approach. In these patients, a limited-access endoscopic approach may be detrimental as compared with the conventional open approach. Early access to the vascular service can be obtained so that hemostasis can be achieved promptly should torrential hemorrhage be encountered.
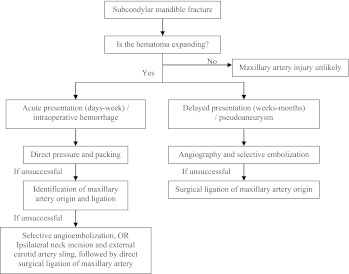
Treatment of maxillary artery hemorrhage can be challenging and depends on the timing of its presentation. In the acute setting, treatment by means of pressure packing and topical hemostatic agents can be attempted, but with the maxillary artery being of significant caliber, hemorrhage is often difficult to control in this manner. Surgical ligation of the origin of the maxillary artery is the preferred method of hemostasis but can be technically difficult initially, as the preauricular incision offers limited access to the vessel. The difficulty is compounded by the presence of fracture fragments superficial to the artery, hence obscuring the view. Furthermore, the vessel ends may retract in cases of complete transaction thus making access even more difficult. An ipsilateral neck incision allows rapid access to the external carotid artery. Ligation of the external carotid artery or its distal branches may be considered but remains a controversial maneuver.5 A rich network of collateral arterial anastomoses exists with the contralateral external carotid artery branches, the ipsilateral internal carotid artery via the ophthalmic artery, the ipsilateral subclavian artery via the costocervical and thyrocervical trunks, and the ipsilateral vertebral artery.9 Consequently, unilateral ligation of the external carotid artery below the level of the lingual and facial arteries leads to only a partial (40%) decrease in the maxillary artery blood flow.10 In this case, a postoperative external carotid artery angiogram performed confirmed the proximal ligation of the maxillary artery. Distally, the flow of the artery was reconstituted by collateral supply and supports the anatomical observations by Takeuchi et al.9
Intuitively, ligation of the origin of the maxillary artery is likely to minimize collateral flow reconstitution and result in more effective hemostasis. A silicone vascular sling can be used to temporarily occlude the proximal external carotid artery, which can usually be achieved in minutes; before isolating the maxillary artery at its origin for direct surgical ligation. In doing so, proximal ligation of the external carotid artery can be avoided, yet ensuring effective hemostasis. In a surgical service where selective angiographic embolization is available, this alternative treatment modality can be used to great effect, particularly in the delayed setting, where healed mandible fragments make surgical access to the maxillary fracture much more difficult. The authors propose the following algorithm in the treatment of suspected maxillary artery injury in a subcondylar mandible fracture (Fig. 5).
Figure 5.
Diagnostic and treatment algorithm for suspected maxillary injury in cases of subcondylar mandible fractures.
Conclusion
Mandible fractures most commonly occur at the subcondylar region due to its intrinsic biomechanical weakness. Anatomical studies have demonstrated its close relationship with the maxillary artery and it is possible that such injuries are underappreciated and underdiagnosed. A high index of suspicion of maxillary artery injury in patients with subcondylar fractures allows the surgeon to treat them expediently and effectively. In such cases, an open approach to the fracture may be favored over an endoscopic one, and various possible methods of securing hemostasis are discussed in the article.
Acknowledgment
Competing interests: None declared
Funding: None
Ethical approval: Not required
References
- 1.Garza J R. New York: Thieme; 2002. Mandibular fractures; pp. 769–781. [Google Scholar]
- 2.Dingman R O, Natvig P. Philadelphia: WB Saunders; 1964. Surgery of Facial Fractures. [Google Scholar]
- 3.Lamphier J Ziccardi V Ruvo A Janel M Complications of mandibular fractures in an urban teaching center J Oral Maxillofac Surg 2003617745–749., discussion 749–750 [DOI] [PubMed] [Google Scholar]
- 4.Schweinfurth J M, Koltai P J. Pediatric mandibular fractures. Facial Plast Surg. 1998;14(1):31–44. doi: 10.1055/s-0028-1085300. [DOI] [PubMed] [Google Scholar]
- 5.Orbay H, Kerem M, Unlü R E, Cömert A, Tüccar E, Sensöz O. Maxillary artery: anatomical landmarks and relationship with the mandibular subcondyle. Plast Reconstr Surg. 2007;120(7):1865–1870. doi: 10.1097/01.prs.0000287137.72674.3c. [DOI] [PubMed] [Google Scholar]
- 6.Bozkurt M, Kapi E, Karakol P, Yorgancilar E. Sudden rupture of the internal maxillary artery causing pseudoaneurysm (mandibular part) secondary to subcondylar mandible fracture. J Craniofac Surg. 2009;20(5):1430–1432. doi: 10.1097/SCS.0b013e3181aee442. [DOI] [PubMed] [Google Scholar]
- 7.Görgü M, Aslan G, Tuncel A, Erdoğan A. Massive expanding hematoma: a late complication of a mandibular fracture. J Oral Maxillofac Surg. 2000;58(11):1300–1302. doi: 10.1053/joms.2000.16635. [DOI] [PubMed] [Google Scholar]
- 8.Elton V J, Turnbull I W, Foster M E. An overview of the management of pseudoaneurysm of the maxillary artery: a report of a case following mandibular subcondylar osteotomy. J Craniomaxillofac Surg. 2007;35(1):52–56. doi: 10.1016/j.jcms.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 9.Takeuchi Y, Numata T, Konno A, Suzuki H, Hino T, Kaneko T. Hemodynamic changes in the head and neck after ligation of the unilateral carotid arteries: a study using color Doppler imaging. Ann Otol Rhinol Laryngol. 1994;103(1):41–45. doi: 10.1177/000348949410300107. [DOI] [PubMed] [Google Scholar]
- 10.Rosenberg I, Austin J C, Wright P G, King R E. The effect of experimental ligation of the external carotid artery and its major branches on haemorrhage from the maxillary artery. Int J Oral Surg. 1982;11(4):251–259. doi: 10.1016/s0300-9785(82)80076-8. [DOI] [PubMed] [Google Scholar]