Abstract
Depression and posttraumatic stress disorder (PTSD) are common after trauma, but it remains unclear what factors determine which disorder a trauma survivor will develop. A prospective longitudinal study of 222 assault survivors assessed candidate predictors derived from cognitive models of depression and PTSD at 2 weeks posttrauma (N = 222), and depression and PTSD symptom severities (N = 183, 82%) and diagnoses at 6 months (N = 205, 92%). Structural equation modeling showed that the depression and PTSD models predicted both depression and PTSD symptom severity, but that the disorder-specific models predicted the respective outcome best (43% for depression, 59% for PTSD symptom severity). Maintaining cognitive variables (hopelessness and self-devaluative thoughts in depression; cognitive responses to intrusive memories and persistent dissociation in PTSD) showed the clearest specific relationships with outcome. Model-derived variables predicted depression and PTSD diagnoses at 6 months over and above what could be predicted from initial diagnoses. Results support the role of cognitive factors in the development of depression and PTSD after trauma, and provide preliminary evidence for some specificity in maintaining cognitive mechanisms.
Keywords: cognitive models, cognitive specificity, posttraumatic stress disorder, depression, structural equation model
Depression (Kilpatrick & Acierno, 2003) and posttraumatic stress disorder (PTSD; e.g., Brewin, Andrews, Rose, & Kirk, 1999; Resnick, Kilpatrick, Dansky, Saunders, & Best, 1993) may both develop in response to traumatic events. Although trauma survivors may only develop one of these disorders, comorbidity is common. There is some overlap in symptom patterns, for example, emotional numbing or sleep disturbance occur in both depression and PTSD, suggesting a degree of shared underlying psychopathology (for a review see Brady, Killeen, Brewerton, & Lucerini, 2000). Nevertheless, there are disorder-specific symptoms, such as suicidal ideation in depression and reexperiencing symptoms in PTSD, and previous research has indeed suggested that depression and PTSD following trauma are correlated but independent outcomes (Blanchard, Buckley, Hickling, & Taylor, 1998; Grant, Beck, Marques, Palyo, & Clapp, 2008). This raises the question of what factors predict whether a trauma survivor will develop depression or PTSD. Cognitive models may be helpful in answering this question because they suggest cognitive specificity, that is, they posit that each disorder is characterized by disorder-specific beliefs and cognitive biases (e.g., Beck, 1967; Beck, Emery, & Greenberg, 1985; Clark, 1999; Riskind & Alloy, 2006).
Cognitive Models of Anxiety and Depression
The basic precept of cognitive models of anxiety and depression (Beck, 1967; Beck, Emery, & Greenberg, 1985; Clark, 1999) is that a person's response to a situation depends on how this person interprets, or appraises, its meaning. The models acknowledge that stressors play a role in the onset of anxiety and depression, but emphasize individual differences in cognitive vulnerability in response to stress. The vulnerability comprises both the way the stressful event is processed and its idiosyncratic meaning for the person's view of the self, the world, and the future. Cognitive models further include factors that are thought to maintain the disorder, namely behaviors and cognitive strategies that maintain a perception of threat in anxiety disorders (see Clark, 1999), and cognitive reactions that worsen or maintain the negative mood (Beck, 1967; Teasdale & Barnard, 1993).
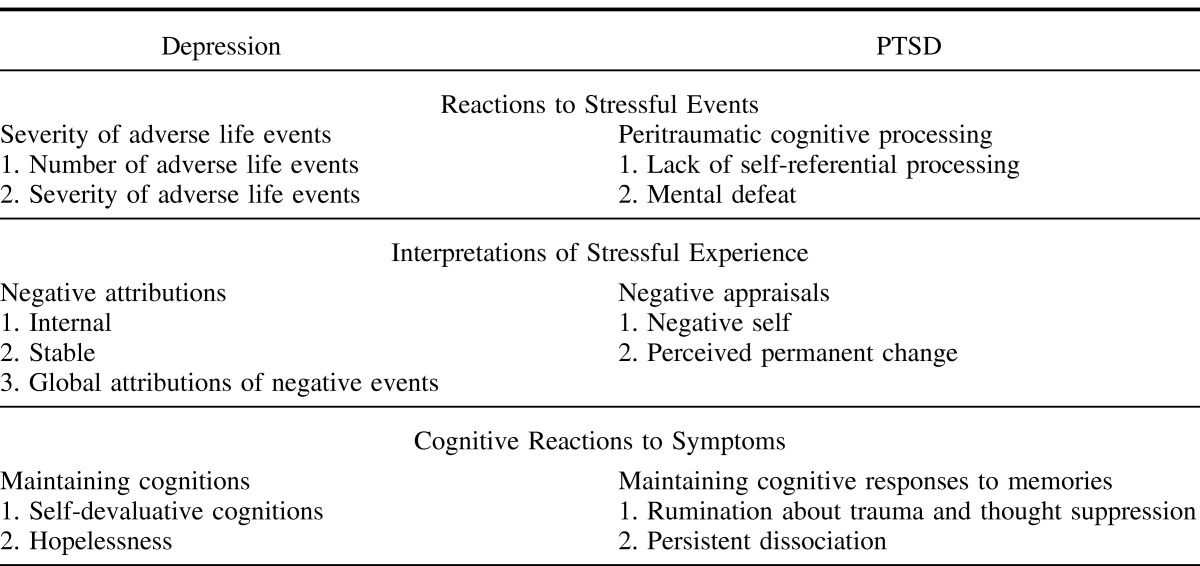
There is empirical support for the role of cognitive factors in the prediction of both depression and PTSD from cross-sectional studies (for reviews see Brewin, Andrews, & Valentine, 2000; and Ozer, Best, Lipsey, & Weiss, 2003), and prospective studies (e.g., Bryant & Guthrie, 2005, 2007; Dunmore, Clark, & Ehlers, 2001; Ehring, Ehlers, & Glucksman, 2008; Halligan, Michael, Clark, & Ehlers, 2003; Kleim, Ehlers, & Glucksman, 2007; Mayou, Bryant, & Ehlers, 2001; O'Donnell, Creamer, & Pattison, 2004; O'Donnell, Elliott, Wolfgang, & Creamer, 2007). Few studies to date have tested the power of cognitive models in the differential prediction of anxiety versus depression (Ehring, Ehlers, & Glucksmanet, 2006, 2008; Mayou et al., 2001; O'Donnell et al., 2004), and if they did, focused mainly on individual predictors (e.g., Mayou et al., 2001). Hankin, Abramson, and Haeffel (2004) showed that cognitive vulnerability for depression interacted with negative events to predict future depression, but not anxiety. Ehring et al. (2006, 2008) found that predictors derived from disorder-specific models predicted depressive, phobic, and PTSD symptoms best. Thus, there is preliminary evidence that cognitive models may be helpful in accounting for who is vulnerable to developing depression or PTSD following a traumatic event. However, previous studies did not test the pathways between the different components of the models and symptom outcome. The present study tested the structural validity of two disorder-specific cognitive models, and their ability to predict chronic depression and PTSD following assault. The main predictors under consideration are summarized in Table 1 and are described below.
Table 1. Cognitive Models: Indicators Representing the Latent Variables.
Depression Model
Predictors of depression were derived from cognitive conceptualizations of the disorder (for a review see Ingram, Miranda, & Segal, 1998; see also Abramson et al., 1999; Abramson, Metalsky, & Alloy, 1989; Abramson, Seligman, & Teasdale, 1978; Beck, Rush, Shaw, & Emery, 1979). According to these vulnerability stress models, depressogenic cognitive patterns are activated when vulnerable individuals encounter adverse life events or when their mood deteriorates (see Kessler, 1997, for a review; Reilly-Harrington, Alloy, Fresco, & Whitehouse, 1999). A well-established cognitive vulnerability factor for developing depression in response to life events is a pessimistic explanatory style, comprising internal, stable, and global negative attributions (Abramson et al., 1978). People with a pessimistic explanatory style are thought to be likely to make negative inferences about the causes, consequences and self-implications of negative life events they encounter, hence increasing the likelihood of developing hopelessness, a proximal cause of depression (Abramson et al., 1989). A sense of hopelessness (Abramson et al., 1989) and a tendency to engage in self-devaluative cognitions (Ingram et al., 1998) have been proposed as maintaining cognitive processes in depression.
PTSD Model
Cognitive models of PTSD focus on people's responses during and after the trauma. Problematic information processing during the trauma (peritraumatic cognitive processing, e.g., Brewin, Dalgleish, & Joseph, 1996; Ehlers & Clark, 2000) and negative appraisals of the trauma and its consequences (Ehlers & Clark, 2000; Foa & Riggs, 1993; Resick & Schnicke, 1993) play a central role in these models. Although appraisals of external threat are taken into account (e.g., “The world is a dangerous place,” “I am going to be assaulted again”), there is an emphasis on negative appraisals about the self. These include appraisals of the trauma such as “I am inadequate” as well as appraisals of one's responses to the trauma such as “My reactions since the trauma mean I am going crazy” (Ehlers & Steil, 1995; Foa & Riggs, 1993). Appraisals of being permanently changed for the worse are particularly predictive of persistent PTSD (Dunmore, Clark, & Ehlers, 1999, 2001; Ehlers, Maercker, & Boos, 2000). Some forms of problematic peritraumatic cognitive processing are thought to contribute to such appraisals, namely a lack of self-referential processing, which is thought to lead to poor integration of the trauma memory with other experiences of the self in the autobiographical memory base (Ehlers & Clark, 2000), and mental defeat, a perceived loss of all psychological autonomy (Dunmore et al., 1999, 2001; Ehlers et al., 2000). Cognitive models of PTSD further suggest that PTSD is maintained because the negative appraisals of the trauma and its consequences motivate a series of maintaining cognitive processes, (Ehlers & Clark, 2000). Among these, cognitive responses to intrusive memories (rumination and thought suppression; Ehlers, Mayou, & Bryant, 1998; Ehlers & Steil, 1995) and persistent dissociation (Halligan et al., 2003; Murray, Ehlers, & Mayou, 2002) have found to be predictive of chronic PTSD.
Overlaps and Differences Between Depression and PTSD Models
Some of the factors proposed in cognitive models of depression and PTSD share similarities. For example, some of the negative self-related appraisals (e.g., “I am inadequate”) highlighted in PTSD models are likely to correlate with negative internal attributions of negative events (e.g., “When bad things happen, I think it is my fault”) emphasized in depression models. Others (e.g., “My reactions to the event show that I am going crazy”) may be more specific to PTSD. Similarly, maintaining cognitive processes may show some overlap, but also specificity. For example, hopelessness may be more predictive of depression, and persistent dissociation more predictive of PTSD. Taken together, the above models suggest cognitive pathways to the development of depression or PTSD following trauma.
Aims and Hypotheses
Assault survivors frequently report symptoms of reexperiencing, avoidance of reminders of the assault, and other common PTSD symptoms, but also symptoms of depression (Foa & Riggs, 1995). The present study used structural equation modeling techniques to investigate whether and how variables derived from two cognitive models of depression and PTSD contribute to the prediction of depressive and PTSD symptoms following assault. Both models included three latent variables. The first latent variable characterizes reactions to stressful events. As the depression literature highlights the cumulative effects of different stressors, the depression model included participants' reactions to severe stressors including the assault. As theories of PTSD highlight cognitive processing during the traumatic event, cognitive processing during the assault was included in the PTSD model. The second latent variable characterizes the individuals' interpretation of stressful events, namely negative attributions of stressful events in the depression model, and negative appraisals of the trauma in the PTSD model. The third latent variable characterizes maintaining cognitive responses to symptoms, and included hopelessness and self-devaluative thoughts in response to depressive symptoms in the depression model; and rumination, thought suppression and persistent dissociation in response to intrusive trauma memories in PTSD.
It was hypothesized that (a) model-based assumptions about relationships between cognitive variables assessed at 2 weeks and symptom severity at 6 months after trauma would be in accord with the data structure, (b) model variables predict a significant amount of variance in depression and PTSD symptom severity at 6 months postassault. Finally, we tested to what extent (c) cognitive models predict diagnoses of depression and PTSD at 6 months, and whether they predict over and above initial diagnoses.
Method
Participants
Participants were recruited from assault survivors treated for their injuries at the Emergency Department of a large urban teaching hospital between July 2003 to December 2004. Participants had to have experienced an assault meeting DSM–IV criterion A, and to understand and speak English fluently enough to be able to answer interview questions and fill in questionnaires. Participants with current psychosis and substance dependence, and those who could not remember the event (e.g., due to a head injury or alcohol black-out) were excluded.
A total of 1,063 assault survivors who attended the Emergency Department during the recruitment period was contacted, of whom 389 did not fulfill inclusion criteria and 197 declined to take part. Another 255 were initially interested, but failed to schedule or attend the research session within the designated time period; 222 participants consented to participate in a research session at 2 weeks after the assault and filled in questionnaires.
At 6 months postassault, 205 participants (92% of the initial sample) completed a telephone interview assessing their diagnoses of depression and/or PTSD, and 183 (82%) completed symptom questionnaires. Our main analyses are based on data from these 183 participants. Table 2 presents demographic and clinical sample characteristics. Participants were mainly physically assaulted, with an average of two assailants involved, M (SD) = 2.43 (2.84), and an average assault duration of 8 min, M (SD) = 7.83 (8.69). In about half of the cases, the attacker had a weapon, n = 85, 45.6%.
Table 2. Structural Equation Modeling Sample: Demographic and Clinical Characteristics (N = 183).
Of the 205 participants who completed the phone interview at 6 months, 34 (17%) met diagnostic criteria for major depression, and 49 (24%) met PTSD criteria. There was substantial comorbidity in that 47% of those with PTSD at 6 months also had major depression, and 68% of those with major depression also had PTSD. At 2 weeks, 45 (20% of 222 participants) met criteria for major depression, and 37 (17%) met diagnostic criteria for acute stress disorder (ASD).
Measures of Psychological Outcomes
PTSD symptom severity
Severity of PTSD was assessed with the Posttraumatic Diagnostic Scale (PDS; Foa, Cashman, Jaycox, & Perry, 1997), a widely used standardized and validated self-report measure of PTSD symptom severity. The PDS asks participants to rate how much they were bothered by each of the 17 PTSD symptoms specified in DSM–IV ranging from 0 (never) to 3 (5 times per week or more/very severely). Internal consistency in this sample was α = .93.
Depression symptom severity
Severity of depression was assessed with the Beck Depression Inventory (BDI; Beck & Steer, 1987), a widely used and validated standardized questionnaire measure of depression. Respondents are asked to decide between four different response choices reflecting different degrees of symptom severity (representing scores of 0 to 3). Internal consistency in this sample was α = .94.
Structured clinical interviews
Current and past major depression and ASD/PTSD diagnoses were established with the Structured Clinical Interview for DSM–IV (SCID; First, Spitzer, Gibbon, & Williams, 1996) and the Acute Stress Disorder Interview (Bryant & Harvey, 2000). A trained clinical psychologist (BK) conducted all interviews at 2 weeks postassault under the supervision of the senior author (AE). At 6 months, the SCID modules were administered over the telephone by the same interviewer. Cases were selected randomly for interrater reliability ratings, which were high (κ = 1 for depression, κ = .82 for PTSD, κ = .97 for ASD; based on 56 interviews, two raters who were each uninformed as to the other rater's diagnoses).
Assessment of Predictors
Depression Model
Severity of adverse life events
The severity of adverse life events was assessed with an adapted version of the Trauma History Interview (Kubany et al., 2000). Participants were asked whether they had experienced any from a list of 11 highly stressful events (e.g., an earlier assault, a motor vehicle accident, natural disaster, warfare). The first index of the severity of adverse life events was the number of adverse events reported. The second index comprised the mean score of the distress of adverse events felt at the time of the events, rated on a scale from 0 (not stressful) to 100 (extremely distressing).
Negative attributions
The Depressive Attributions Questionnaire measures depressogenic attributions (internal, stable, global) of negative events (Kleim, Gonzalo, & Ehlers, 2011). Participants rated to what extent they agreed with 11 statements on a scale from 0 (not at all) to 4 (very strongly), indexing internal (α = .77), stable (α = .88), and global attributions (α = .83). The subscales correlate significantly with the respective subscales of the Attributional Style Questionnaire.
Maintaining cognitions
A short form (four items) of Beck's Hopelessness Scale (Beck & Steer, 1988) compiled by Williams (2003) was used to assess participants' hopelessness, that is, their expectations about their future (α = .83). Self-devaluative cognitions were assessed with the self-devaluation subscale of the Depressed States Checklist (DSQ; Teasdale & Cox, 2001). Participants are asked to describe how they felt when their mood started to deteriorate during the preceding month by rating 28 adjectives on a scale from 0 (not at all) to 4 (extremely). Half of the adjectives imply self-devaluation (e.g., unacceptable, rejected, unwanted, worthless). The mean score of responses to the 14 self-devaluative descriptors (α = .96) was used in this study.
PTSD Model
Peritraumatic cognitive processing
The 8-item self-referential processing scale from the Cognitive Processing Questionnaire (Halligan et al., 2003) was used to assess the extent to which participants processed the assault as happening to themselves and linked it with other autobiographical information related to the self. Participants rated on a scale from 0 (not at all) to 4 (very strongly) how much each statement applied to them during the assault until help arrived. The scale has been shown to be reliable and to predict PTSD in previous studies (Ehring et al., 2006, 2008; Halligan et al., 2003). Internal consistency in this sample was α = .89.
Mental defeat was assessed with the 11-item Mental Defeat Scale (MD; Dunmore et al., 1999, 2001). Participants rated on a scale from 0 (not at all) to 4 (very strongly) to what extent each statement about perceived loss of psychological autonomy applied to them at any moment during the assault until help arrived. The scale has been shown to have good reliability and predictive validity in previous studies (Dunmore et al., 1999, 2001). Internal consistency in this sample was α = .90.
Negative appraisals
Negative thoughts about the self, and perceived permanent change were measured with the Posttraumatic Cognitions Inventory (PTCI; Foa, Ehlers, Clark, Tolin, & Orsillo, 1999). Participants are asked to rate negative thoughts about the trauma on a scale from 1 (totally agree) to 7 (totally disagree). The scale has been shown to be reliable and to distinguish between trauma survivors with and without PTSD (Foa et al., 1999). A mean score was calculated separately for the 17 relevant items for the negative self scale (e.g., “I am inadequate,” excluding permanent change, α = .91), and for the 4 items representing perceived permanent change (e.g., “I have permanently changed for the worse,” α = .77).
Maintaining cognitive responses to memories
The sum of the respective subscales of the Response to Intrusions Questionnaire (RIQ) was used to measure thought suppression (six items), and rumination (six items). Participants rated on a scale from 0 (not at all) to 4 (very strongly) how much each statement applied to them. The scale had adequate reliability and predictive validity in a range of studies (Clohessy & Ehlers, 1999; Ehring et al., 2006, 2008; Murray et al., 2002). Internal consistency in this sample was α = .86.
The State Dissociation Questionnaire (SDQ; Murray et al., 2002) was used to measure persistent dissociation after the traumatic event. This measure has been shown to predict PTSD after motor vehicle accidents and assault, to have good reliability (α ≥ .80), and correlate with other measures of dissociation (Halligan et al., 2003; Murray et al., 2002). The questionnaire asks participants to rate how often they had each of a list of nine dissociative experiences during the last week. Internal consistency in this sample was α = .95.
Procedure
The study was approved by the local ethics committee. A few days after their admission at the Emergency Department, assault survivors received information about the study by mail and were invited to participate in a research session at 2 weeks after the assault. The invitation letter was followed by a telephone call where further information about the study was given. Upon arrival at the session, participants had the opportunity to ask further questions, gave written informed consent, and completed questionnaires and diagnostic interviews. At 6 months, participants filled in symptom severity questionnaires. Participants were reimbursed £50 ($97) for their time and travel expenses.
Data Analysis
Data were analyzed with structural equation modeling (SEM; AMOS, Version 7.0., Arbuckle, 2006). The maximum likelihood (ML) method of estimation evaluated the plausibility of the hypothetical depression and PTSD models. Both models were theory-derived, without post hoc model modifications, and comprised three latent independent variables summarized in Table 1. Both outcomes were modeled in one structural equation model for each set of predictors, and were allowed to correlate with each other using correlated error terms (see Kline, 1998). Split-half scales were created by splitting items at random and used to operationalize latent measures of outcome (Cronbach's alpha for split half scales: BDI: α = .90, .90, PDS: α = .93, .92).
For evaluation of model fit, four fit indices were considered (Bollen, 1989; Kline, 1998): normed chi-square, χ2/degree of freedom ratio (CMIN/DF; values smaller than 2.0, 3.0, or 5.0 have been recommended as indicating good model fit in the literature), comparative fit index (CFI; > .90 indicates good fit), normed fit index (NFI; > .90 indicates good fit), and root mean square error of approximation (RMSEA; < .10 indicates good fit). Moreover, coefficients of determination (amount of variance; R2), which indicate how well the models explained PTSD and depression severity; as well as the direct, indirect, and total effects of the model variables were of interest. A direct influence is the influence a variable has on another variable in a direct linkage; an indirect effect consists of all paths from one variable to another that are mediated by at least one additional variable; and the total effect is the sum of the direct and indirect effects. Kline (1998) outlined a rough guide for interpreting standardized path coefficients, with coefficients of less than .10 small effect, .30 medium effect, and .50 or greater large effect. In addition, logistic regression analyses predicting depression and PTSD diagnoses at 6 months were performed with SPSS 15.0.
Results
Prediction of Depression and PTSD Symptom Severities by Cognitive Models
Table 3 presents zero-order correlations between the predictors from the depression and PTSD models, assessed at 2 weeks, and psychological outcomes at 6 months (full scale scores). Correlations between the predictors at 2 weeks and symptom severities at 6 months were substantial. The predictors also correlated with each other, with the exception of nonsignificant associations between severity of stressful life events and internal and stable attributions and hopelessness. Depression and PTSD symptom severity scores were significantly correlated, r = .77, p < .001, in line with the high comorbidity observed in the current sample. Predictors from both models correlated with both outcomes.
Table 3. Zero-Order Correlations Between Predictors From Depression and PTSD Models, Assessed at 2 Weeks, and Psychological Outcomes at 6 Months (Correlations With Model-Specific Outcomes in Bold).
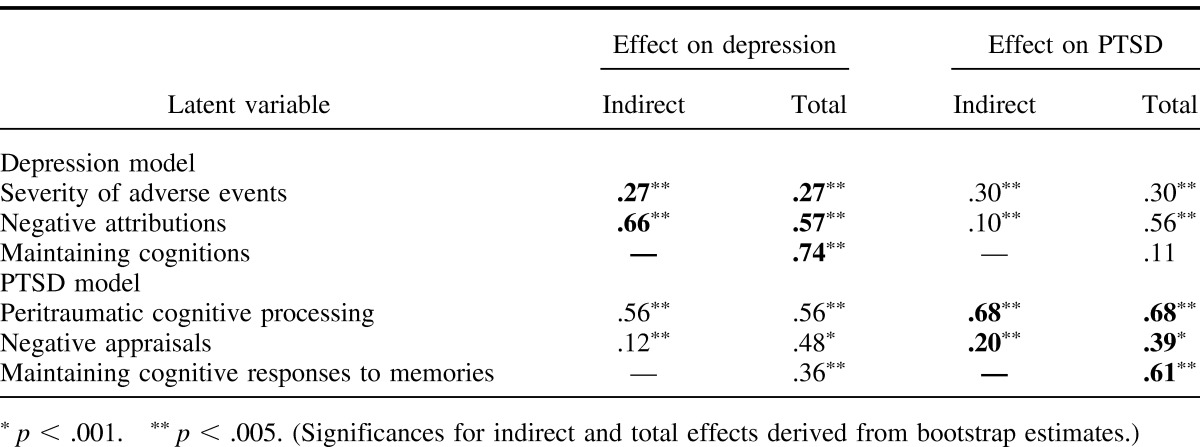
Figures 1 and 2 present the full structural equation models for the depression and PTSD models. All loadings of the depression model (arrows from latent to manifest variables) ranged from β = .72 to .95, with one exception of a low factor loading between adverse event distress and severity of adverse events, β = .34. Loadings for the PTSD model were all acceptable and ranged from β = .72 to .99. Indirect effects and the total proportion of variance explained by each latent variable are summarized in Table 4.
Figure 1. Prediction of psychological outcomes at 6 months with predictors from depression model assessed at 2 weeks (model-specific psychopathology outcome shaded in gray). Rectangles represent observed variables (questionnaires scores) and ovals represent latent variables. Single-headed arrows represent hypothesized causal effects. In the interest of clarity, all double-headed errors representing correlations among symptom outcome variables, as well as error terms associated with the observed (indicator) variables, have been excluded from the figures. Results of the standardized maximum likelihood estimates are presented; error variables and disturbances are not displayed; a correlation between error terms of PTSD and depression was also modeled, but is not displayed. For indirect effects see Table 4. All path coefficients, except those in brackets, were significant. Severity of adverse events = number and distress of adverse life events (Trauma History Interview); Negative attributions = internal/global/stable attributions of negative events (Depressive Attributions Questionnaire); Maintaining Cognitions = hopelessness (Hopelessness Questionnaire); self-devaluative cognitions (Depressed States Questionnaire); PTSD = PTSD severity, split-half scales (Posttraumatic Stress Diagnostic Scale); Depression = depression severity, split-half scales (Beck Depression Inventory).
Figure 2. Prediction of psychological outcomes at 6 months with predictors from the PTSD model assessed at 2 weeks (model-specific psychopathology outcome shaded in gray). Results of the standardized maximum likelihood estimates are presented; error variables and disturbances are not displayed; a correlation between error terms of PTSD and depression was also modeled, but is not displayed. All path coefficients, except those in brackets, were significant. For indirect effects see Table 4. Peritraumatic cognitive processing = lack of self-referential processing (Cognitive Processing Questionnaire); mental defeat (Mental Defeat Questionnaire); Negative Appraisals = negative cognitions about self/permanent change (Posttraumatic Cognitions Inventory); Maintaining cognitive responses to memories = rumination about the trauma and thought suppression (Responses to Intrusion Questionnaire), persistent dissociation (State Dissociation Questionnaire); PTSD = PTSD severity, split-half scales (Posttraumatic Stress Diagnostic Scale); Depression = depression severity, split-half scales (Beck Depression Inventory).
Table 4. Standardized Indirect and Total Effects of Latent Variables at 2 Weeks on Depression and PTSD Symptom Severities at 6 Months (N = 183) (Effects on Model-Specific Outcomes in Bold).
Depression Model
Figure 1 displays the proposed relations between the three latent variables in the depression model assessed at 2 weeks and the two outcome variables at 6 months (depression and PTSD severity). This model accounted well for the observed relationships in the data, χ2 = 48.14, df = 36, p = .085, CMIN/DF = 1.34, CFI = .992; NFI = .969; RMSEA = .039. The coefficients of determination showed that the depression model accounted for 43% of variance of depression severity, and 32% of PTSD symptom severity.
Table 4 shows that the severity of adverse life events indirectly predicted depression severity, β = .27, via the other cognitive variables. Internal, stable, and global attributions of negative events did not directly predict depression, β = −.09, but nevertheless had a strong total effect on depression severity, β = .57, via maintaining cognitions. Maintaining cognitions (self-devaluation and hopelessness) had a strong predictive effect on depression, β = .74, and had a smaller direct influence on PTSD, β = 11.
In order to rule out a possible spurious inflation of associations between cognitive predictors and depression severity, we repeated the analysis with a modified BDI outcome variable, excluding the 5 BDI items with cognitive content. Results were very similar (overall model fit: χ2 = 50.78, df = 36, p = .052; explained depression severity: 41%).
PTSD Model
The PTSD model (see Figure 2) showed good fit with the data, χ2 = 44.0, df = 27, p = .021, CMIN/DF = 1.63., CFI = .990; NFI = .974; RMSEA = .053. The coefficients of determination indicated that the PTSD model explained 59% versus 47% of the variance in PTSD and depression severity, respectively. Peritraumatic cognitive processing indirectly predicted PTSD severity, β = .68, mediated by the other cognitive variables (see Table 4). Negative appraisals directly predicted PTSD at trend level, β = .19 p = .087, and had a strong total effect on PTSD severity, β = .39, which was largely mediated by maintaining cognitive responses to memories (rumination, thought suppression, and persistent dissociation), which had a strong predictive effect on PTSD, β = .61. Negative appraisals also had a strong effect on depression, β = .48. Finally, maintaining cognitive responses to memories had a stronger effect on PTSD than on depression, β = .61 versus β = .36.
Prediction of Diagnoses at 6 Months
Logistic regressions tested whether the depression and PTSD model predicted the respective diagnosis over and above initial diagnoses. The depression model variables predicted depression at 6 months over and above what was predicted by a diagnosis of depression at 2 weeks, χ2 (7, 160) = 19.05, p < .001; step 1 (diagnosis of major depression at 2 weeks), χ2 (1, 160) = 13.54, p < .001, Nagelkerke R2 = .134, sensitivity 43%; step 2 (including variables from depression model), χ2 (8, 160) = 32.59, p < .001, Nagelkerke R2 = .305, sensitivity 75%. Similarly, for PTSD, variables derived from the PTSD model predicted PTSD at 6 months over and above ASD diagnosis at 2 weeks, χ2 (6, 176) = 41.48, p < .001; step 1 (diagnosis of ASD at 2 weeks), χ2 (1, 176) = 31.30, p < .001, Nagelkerke R2 = .252, sensitivity 50%; step 2 (including variables from PTSD model), χ2 (7, 176) = 72.78, p < .001, Nagelkerke R2 = .523, sensitivity 74%.
As previous research has shown that adverse life events may play a larger role in the recurrence of depression than in first episodes of depression (Kessler, 1997), we tested the predictive power of the depression model separately for participants with and without a history of major depression. Of the participants who met criteria for major depression at either 2 weeks or 6 months after the assault, 65% reported a history of depression, and 35% had the first depressive episode. The depression model predicted recurrent depression well, χ2 (7, 147) = 43.82, p < .001, Nagelkerke R2 = .405, sensitivity 80%. It marginally predicted new onset of depression after the assault, χ2 (7, 133) = 13.85, p = .054, Nagelkerke R2 = .190, sensitivity 63%.
Discussion
The study used a prospective longitudinal design to investigate cognitive pathways to development and maintenance of depression and PTSD after a traumatic event. As predicted, depression and PTSD symptom severity at 6 months after injury in an assault could be predicted from candidate predictors at 2 weeks that were derived from cognitive models of depression and PTSD. The depression and PTSD models provided good fit with the data and explained a substantial proportion of the variance of the respective symptom severity at 6 months, 43% for depressive and 59% for PTSD symptoms. The model-derived variables also predicted depression and PTSD diagnoses at 6 months, and were shown to predict over and above initial depression/ASD diagnoses, respectively. Taken together, the results supported the role of early cognitive responses in the prediction of chronic posttrauma symptoms. For both depression and PTSD, cognitive variables showed large effects in predicting psychological outcome, and enhanced the predictive accuracy over and above initial symptoms.
Overall, PTSD was better predicted in this study than depression. One possible reason is that all symptoms were measured in response to a traumatic event. The depression model may be more powerful in predicting depression after traumatic events involving loss (Kendler, Hettema, Butera, Gardner, & Prescott, 2003). Furthermore, several months elapsed between the assessment of the cognitive variables and assessment of outcome. As depression tends to follow a fluctuating course, modest long-term prediction is to be expected (Kessler, Zhao, Blazer, & Swartz, 1997). In contrast, although there is natural recovery in PTSD, symptoms tend to become chronic after a few months (Rothbaum, Foa, Riggs, Murdock, & Walsh, 1992).
Although the models used in the present investigation explained a substantial proportion of the variance of chronic posttrauma symptoms, some previous studies have reported even better prediction of depression and PTSD by cognitive models (e.g., depression: Hankin, Abramson, & Haeffel, 2004; PTSD: Halligan et al., 2003, but see Ford, Ayers, & Bradley, 2010). One explanation for the somewhat smaller effect size in the prediction of depression in the current study may be that the cognitive vulnerability-stress model does not apply universally to all forms of depression. Different subtypes of depression may require unique conceptualizations of factors involved in onset and maintenance of the disorder. A study by Lewinsohn, Allen, Seeley, and Gotlib (1999), for instance, demonstrated that first episodes of depression were predicted by different constructs than were recurrent episodes of depression. In line with previous research showing clearer evidence for the role of adverse life events in predicting recurrent depression than in the first onset of depression (Kessler, 1997), this study found greater predictive power for the depression model in predicting recurrent depression than the first episode of depression after the assault. Furthermore, it is possible that the prediction of depression may have been improved by including further predictors such as rumination about sad mood (Nolen-Hoeksema, 2000; Smith & Alloy, 2009). Similarly, with respect to the prediction of PTSD, other studies (Ehring et al., 2006, 2008; Halligan et al., 2003) included a larger set of predictors derived from Ehlers and Clark's (2000) model and included characteristics of trauma memories, which are central to the model and may have added power to the differential prediction.
The present results provided evidence for an overlap of mechanisms in depression and PTSD, and some evidence for specificity. Each model predicted both disorders reasonably well. Nevertheless, the depression model predicted depression best (43% explained variance for depression vs. 32% for PTSD), and the PTSD model explained PTSD best (59% vs. 47% for depression). In the depression model, internal, global, and stable attributions of negative events predicted depression, but also PTSD well. This is consistent with earlier findings showing that trauma survivors with PTSD have similar attributional styles as depressed people (Wenninger & Ehlers, 1998) and the role of self-blame in PTSD (Foa et al., 1999). In contrast, cognitive responses to sad mood that are thought to maintain depression (self-devaluation and hopelessness) were specific in that they were more predictive of depression than of PTSD. The pattern for the PTSD model was similar in that negative appraisals about the self were not specific and explained depression even somewhat better than PTSD, but responses to trauma memories (rumination, thought suppression, and persistent dissociation), the proposed maintaining variables, explained PTSD better than depression.
Thus, this study found the best evidence for specificity for the latent variables representing maintaining cognitive responses. It has been suggested that people with PTSD use cognitive processes such as thought suppression and rumination about the trauma to reduce their sense of current threat, but maintain the problem by preventing change in trauma memory and appraisals, and may lead to paradoxical increases in symptoms (Ehlers & Clark, 2000; Ehlers & Steil, 1995). In depression, hopelessness is thought to mediate the course of depression by hampering the person's ability to generate adaptive beliefs and solutions to problems (Beck, 1967). The effects of attributions and appraisals on outcomes were mediated by maintaining cognitions in both the depression and PTSD models. These results are in line with a recent analogue trauma study (Regambal & Alden, 2008). Maintaining factors may be more important in predicting long-term psychopathology than factors that explain the onset of initial symptoms, such as distress, fear, or cognitive processing during adverse events (Ehlers & Clark, 2000; Ehlers & Steil, 1995).
The study had several limitations. First, the number of variables included in the structural equation models was limited due to restrictions in sample size. It would be desirable for future studies to include additional cognitive variables, such as characteristics of trauma memories as risk factors for PTSD (e.g., Brewin et al., 1996; Ehlers & Clark, 2000; Foa & Riggs, 1993), or rumination about sad mood for depression (e.g., Smith & Alloy, 2009). Larger samples sizes would allow the investigation of more comprehensive models. Second, numbers of trauma survivors within the disorder categories were too small (and comorbidity too high) to examine subgroups of “pure” disorders, which would allow for a sophisticated investigation into the diagnostic specificity of the models. Third, the results were obtained in a sample of assault survivors, and a cross-validation of the structural models in survivors of other traumatic events would be helpful to test whether the results generalize to other populations.
Despite these limitations, the present study had a number of strengths. To our knowledge, it is one of the first studies to test the relationships and predictive power of factors derived from cognitive models of depression and PTSD simultaneously with a prospective design. Cognitive variables measured at two weeks postassault predicted depression and PTSD symptoms at 6 months posttrauma. The study provided evidence for some specific and some common mechanisms in predicting these disorders with cognitive models. Maintaining cognitive processes such as hopelessness and self-devaluation in depression and rumination about the trauma and effortful suppression of trauma memories in PTSD were strong predictors, and showed the clearest evidence for disorder specificity among the variables under investigation. Clinically, this suggests that such maintaining processes are promising targets for treatment. Cognitive–behavioral treatments that target these maintaining cognitive processes in a structured way (for reviews see Ehlers & Clark, 2008; Hollon, Stewart, & Strunk, 2006) are effective and acceptable to patients (Bisson et al., 2007; Butler, Chapman, Forman, & Beck, 2006; Gloaguen, Cottraux, Cucherat, & Blackburn, 1998). The present data provide additional support for their underlying treatment rationale. Cognitive models may also inform screening efforts after trauma in increasing the prognostic validity screening instruments. In the present sample, cognitive variables predicted over and above initial diagnoses and increased sensitivity of the prediction substantially. Identification of trauma survivors at risk for the development of depression or PTSD may thus be further improved by focusing on such model-derived cognitive features (see also O'Donnell et al., 2008). Given that the majority of trauma survivors with posttrauma psychopathology are not treated (Zatzick, 2003), the possibility of identifying survivors at risk, and the prospect of offering those with particular cognitive profiles specific prevention or intervention programs appears promising.
Acknowledgments
Birgit Kleim is currently at the University of Zurich, Department of Clinical Psychology and Psychotherapy, Zurich, Switzerland. Anke Ehlers is now based at Oxford University, Department of Experimental Psychology, Oxford, UK.
The study was funded by the Psychiatry Research Trust and the Wellcome Trust (Grant 069777). We thank Thomas Ehring, Silke Frank, Anke Weidmann, Johanna Hissbach, Jennifer Baumeister, and Stephanie Spengler, as well as the staff of King's College Hospital's Accident and Emergency Department for their help.
References
- Abramson L. Y., Alloy L. B., Hogan M. E., Whitehouse W. G., Donovan P., Rose D. T., . . . Raniere D. (1999). Cognitive vulnerability to depression: Theory and evidence. Journal of Cognitive Psychotherapy: An International Quarterly, 13, 5–20. [Google Scholar]
- Abramson L. Y., Metalsky G. I., & Alloy L. B. (1989). Hopelessness depression: A theory-based subtype of depression. Psychological Review, 96, 358–372. doi:10.1037/0033-295X.96.2.358 [Google Scholar]
- Abramson L. Y., Seligman M. E. P., & Teasdale J. D. (1978). Learned helplessness in humans: Critique and reformulation. Journal of Abnormal Psychology, 87, 49–74. doi:10.1037/0021-843X.87.1.49 [PubMed] [Google Scholar]
- Arbuckle J. L. (2006). Amos (Version 7.0) [Computer Program]. Chicago, IL: SPSS. [Google Scholar]
- Beck A. T. (1967). Depression: Clinical, experimental and theoretical aspects. New York, NY: Harper & Row. [Google Scholar]
- Beck A. T., Emery G., & Greenberg R. L. (1985). Anxiety disorders and phobias: A cognitive perspective. New York, NY: Basic Books. [Google Scholar]
- Beck A. T., Rush A. J., Shaw B. F., & Emery G. (1979). Cognitive therapy of depression. New York, NY: Guilford Press. [Google Scholar]
- Beck A. T., & Steer R. A. (1987). Beck depression inventory: Manual. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Beck A. T., & Steer R. A. (1988). Manual for the beck hopelessness scale. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Bisson J. I., Ehlers A., Matthews R., Pilling S., Richards D., & Turner S. (2007). Psychological treatments for chronic posttraumatic stress disorder. Systematic review and meta-analysis. British Journal of Psychiatry, 190, 97–104. doi:10.1192/bjp.bp.106.021402 [DOI] [PubMed] [Google Scholar]
- Blanchard E. B., Buckley T. C., Hickling E. J., & Taylor A. E. (1998). Posttraumatic stress disorder and comorbid major depression: Is the correlation an illusion? Journal of Anxiety Disorders, 12, 21–37. doi:10.1016/S0887-6185(97)00047-9 [DOI] [PubMed] [Google Scholar]
- Bollen K. A. (1989). Structural equations with latent variables. New York, NY: Wiley. [Google Scholar]
- Brady K. T., Killeen T. K., Brewerton T., & Lucerini S. (2000). Comorbidity of psychiatric disorders and posttraumatic stress disorder. Journal of Clinical Psychiatry, 61, 22–32. [PubMed] [Google Scholar]
- Brewin C. R., Andrews B., Rose S., & Kirk M. (1999). Acute stress disorder and posttraumatic stress disorder in victims of violent crime. American Journal of Psychiatry, 156, 360–366. [DOI] [PubMed] [Google Scholar]
- Brewin C. R., Andrews B., & Valentine J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68, 748–766. doi:10.1037/0022-006X.68.5.748 [DOI] [PubMed] [Google Scholar]
- Brewin C. R., Dalgleish T., & Joseph S. (1996). A dual representation theory of posttraumatic stress disorder. Psychological Review, 103, 670–686. doi:10.1037/0033-295X.103.4.670 [DOI] [PubMed] [Google Scholar]
- Bryant R. A., & Guthrie R. M. (2005). Maladaptive appraisals as a risk factor for posttraumatic stress: A study of trainee firefighters. Psychological Science, 16, 749–752. doi:10.1111/j.1467-9280.2005.01608.x [DOI] [PubMed] [Google Scholar]
- Bryant R. A., & Guthrie R. M. (2007). Maladaptive self-appraisals before trauma exposure predict posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 75, 5, 812–815. doi:10.1037/0022-006X.75.5.812 [DOI] [PubMed] [Google Scholar]
- Bryant R. A., & Harvey A. G. (2000). Acute stress disorder: A handbook of theory, assessment, and treatment. Washington, DC: American Psychological Association. doi:10.1037/10346-000 [Google Scholar]
- Butler A. C., Chapman J. E., Forman E. M., & Beck A. T. (2006). The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clinical Psychology Review, 2006, 26, 1, 17–31. doi:10.1016/j.cpr.2005.07.003 [DOI] [PubMed] [Google Scholar]
- Clark D. M. (1999). Anxiety disorders: Why they persist and how to treat them. Behaviour Research and Therapy, 37, S5–S27. [DOI] [PubMed] [Google Scholar]
- Clohessy S., & Ehlers A. (1999). PTSD symptoms, response to intrusive memories and coping in ambulance service workers. British Journal of Clinical Psychology, 38, 251–265. doi:10.1348/014466599162836 [DOI] [PubMed] [Google Scholar]
- Dunmore E., Clark D. M., & Ehlers A. (1999). Cognitive factors involved in the onset and maintenance of posttraumatic stress disorder (PTSD) after physical or sexual assault. Behaviour Research and Therapy, 37, 809–829. doi:10.1016/S0005-7967(98)00181-8 [DOI] [PubMed] [Google Scholar]
- Dunmore E., Clark D. M., & Ehlers A. (2001). A prospective investigation of the role of cognitive factors in persistent posttraumatic stress disorder (PTSD) after physical or sexual assault. Behaviour Research and Therapy, 39, 1063–1084. doi:10.1016/S0005-7967(00)00088-7 [DOI] [PubMed] [Google Scholar]
- Ehlers A., & Clark D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38, 319–345. doi:10.1016/S0005-7967(99)00123-0 [DOI] [PubMed] [Google Scholar]
- Ehlers A., & Clark D. M. (2008). Posttraumatic stress disorder: The development of effective psychological treatments. Nordic Journal of Psychiatry, 47, 11–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers A., Maercker A., & Boos A. (2000). PTSD following political imprisonment: The role of mental defeat, alienation, and permanent change. Journal of Abnormal Psychology, 109, 45–55. doi:10.1037/0021-843X.109.1.45 [PubMed] [Google Scholar]
- Ehlers A., Mayou R. A., & Bryant B. (1998). Psychological predictors of chronic PTSD after motor vehicle accidents. Journal of Abnormal Psychology, 107, 508–519. doi:10.1037/0021-843X.107.3.508 [DOI] [PubMed] [Google Scholar]
- Ehlers A., & Steil R. (1995). Maintenance of intrusive memories in posttraumatic stress disorder: A cognitive approach. Behavioural and Cognitive Psychotherapy, 23, 217–249. doi:10.1017/S135246580001585X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehring T., Ehlers A., & Glucksman E. (2006). Contribution of cognitive factors to the prediction of posttraumatic stress disorder, phobia and depression after motor vehicle accidents. Behaviour Research and Therapy, 44, 1699–1716. doi:10.1016/j.brat.2005.11.013 [DOI] [PubMed] [Google Scholar]
- Ehring T., Ehlers A., & Glucksman E. (2008). Do cognitive models help in predicting the severity of posttraumatic stress disorder, phobia and depression after motor vehicle accidents? A prospective longitudinal study. Journal of Consulting and Clinical Psychology, 76, 219–230. doi:10.1037/0022-006X.76.2.219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M. B., Spitzer R. L., Gibbon M., & Williams J. B. W. (1996). Structured clinical interview for DSM-IV axis I disorders. Washington, DC: American Psychiatric Press. [Google Scholar]
- Foa E. B., Cashman L., Jaycox L., & Perry K. (1997). The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment, 9, 445–451. doi:10.1037/1040-3590.9.4.445 [Google Scholar]
- Foa E. B., Ehlers A., Clark D. M., Tolin D. F., & Orsillo S. M. (1999). The Posttraumatic Cognitions Inventory (PTCI): Development and validation. Psychological Assessment, 11, 303–314. doi:10.1037/1040-3590.11.3.303 [Google Scholar]
- Foa E. B., & Riggs D. S. (1993). Posttraumatic stress disorder in rape victims. In Oldham J. M., Riba M. B., & Tasman A. (Eds.), Annual review of psychiatry (pp. 273–303). Washington, DC: American Psychiatric Association. [Google Scholar]
- Foa E. B., & Riggs D. S. (1995). Post-traumatic stress disorder following assault: Theoretical considerations and empirical findings. Current Directions in Psychological Science, 4, 61–65. doi:10.1111/1467-8721.ep10771786 [Google Scholar]
- Ford E., Ayers S., & Bradley R. (2010). Exploration of a cognitive model to predict posttraumatic stress symptoms following childbirth. Journal of Anxiety Disorders, 24, 3, 353–359. doi:10.1016/j.janxdis.2010.01.008 [DOI] [PubMed] [Google Scholar]
- Gloaguen V., Cottraux J., Cucherat M., & Blackburn I. M. (1998). A meta-analysis of the effects of cognitive therapy in depressed patients. Journal of Affective Disorders, 49, 59–72. doi:10.1016/S0165-0327(97)00199-7 [DOI] [PubMed] [Google Scholar]
- Grant D. M., Beck G., Marques L., Palyo S. A., & Clapp J. D. (2008). The structure of distress following trauma: Posttraumatic stress disorder, major depression, and generalized anxiety disorder. Journal of Abnormal Psychology, 117, 662–672. doi:10.1037/a0012591 [DOI] [PubMed] [Google Scholar]
- Halligan S. L., Michael T., Clark D. M., & Ehlers A. (2003). Posttraumatic stress disorder following assault: The role of cognitive processing, trauma memory, and appraisals. Journal of Consulting and Clinical Psychology, 71, 419–431. doi:10.1037/0022-006X.71.3.419 [DOI] [PubMed] [Google Scholar]
- Hankin B. L., Abramson L. Y., & Haeffel G. J. (2004). Cognitive vulnerability-stress theories of depression: Examining affective specificity in the prediction of depression versus anxiety in three prospective studies. Cognitive Therapy and Research, 28, 309–345. doi:10.1023/B:COTR.0000031805.60529.0d [Google Scholar]
- Hollon S. D., Stewart M. O., & Strunk D. (2006). Enduring effects for cognitive behavior therapy in the treatment of depression and anxiety. Annual Review of Psychology, 57, 285–315. doi:10.1146/annurev.psych.57.102904.190044 [DOI] [PubMed] [Google Scholar]
- Ingram R. E., Miranda J., & Segal Z. V. (1998). Cognitive vulnerability to depression. New York, NY: Guilford Press. [Google Scholar]
- Kendler K. S., Hettema J. M., Butera F., Gardner C. O., & Prescott C. A. (2003). Life event dimensions of loss, humiliation, entrapment and danger in the prediction of onsets of major depression and generalized anxiety disorder. Archives of General Psychiatry, 60, 789–796. doi:10.1001/archpsyc.60.8.789 [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Zhao S., Blazer D. G., & Swartz M. (1997). Prevalence, correlates, and course of major depression in the national comorbidity survey. Journal of Affective Disorders, 45, 19–30. doi:10.1016/S0165-0327(97)00056-6 [DOI] [PubMed] [Google Scholar]
- Kessler R. C. (1997). The effects of stressful life events on depression. Annual Review of Psychology, 48, 191–214. doi:10.1146/annurev.psych.48.1.191 [DOI] [PubMed] [Google Scholar]
- Kilpatrick D. G., & Acierno R. (2003). Mental health needs of crime victims: Epidemiology and outcomes. Journal of Traumatic Stress, 16, 119–132. doi:10.1023/A:1022891005388 [DOI] [PubMed] [Google Scholar]
- Kleim B., Ehlers A., & Glucksman E. (2007). Early predictors of posttraumatic stress disorder in assault survivors. Psychological Medicine, 37, 1457–1467. doi:10.1017/S0033291707001006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleim B., Gonzalo D., & Ehlers A. (2011). The depressive attributions questionnaire (DAQ): Development of a short self- report measure of depressogenic attributions. Journal of Psychopathology and Behavioral Assessment, 33, 375–385. doi:10.1007/s10862-011-9234-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline R. B. (1998). Principles and practice of structural equation modeling. New York, NY: Guilford Press. [Google Scholar]
- Kubany E. S., Haynes S. N., Leisen M. B., Owens J. A., Kaplan A. S., Watson S. B., & Burns K. (2000). Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment, 12, 210–224. doi:10.1037/1040-3590.12.2.210 [DOI] [PubMed] [Google Scholar]
- Lewinsohn P. M., Allen N. B., Seeley J. R., & Gotlib I. H. (1999). First onset versus recurrence of depression: Differential processes of psychosocial risk. Journal of Abnormal Psychology, 108, 483–489. doi:10.1037/0021-843X.108.3.483 [DOI] [PubMed] [Google Scholar]
- Mayou R. A., Bryant B. M., & Ehlers A. (2001). Prediction of psychological outcomes one year after a motor vehicle accident. American Journal of Psychiatry, 158, 1231–1238. doi:10.1176/appi.ajp.158.8.1231 [DOI] [PubMed] [Google Scholar]
- Murray J., Ehlers A., & Mayou R. A. (2002). Dissociation and posttraumatic stress disorder: Two prospective studies of road traffic accident survivors. British Journal of Psychiatry, 180, 363–368. doi:10.1192/bjp.180.4.363 [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. (2000). The role of rumination in depressive disorders and mixed anxiety/depression symptoms. Journal of Abnormal Psychology, 109, 3, 504–511. doi:10.1037/0021-843X.109.3.504 [PubMed] [Google Scholar]
- O'Donnell M. L., Creamer M., & Pattison P. (2004). Posttraumatic stress disorder and depression following trauma: Understanding comorbidity. American Journal of Psychiatry, 161, 1390–1396. doi:10.1176/appi.ajp.161.8.1390 [DOI] [PubMed] [Google Scholar]
- O'Donnell M. L., Creamer M. C., Parslow R., Elliott P., Holmes A. C., Ellen S., . . . Bryant R. A. (2008). A predictive screening index for posttraumatic stress disorder and depression following traumatic injury. Journal of Consulting and Clinical Psychology, 76, 6, 923–932. doi:10.1037/a0012918 [DOI] [PubMed] [Google Scholar]
- O'Donnell M. L., Elliott P., Wolfgang B. J., & Creamer M. (2007). Posttraumatic appraisals in the development and persistence of posttraumatic stress symptoms. Journal of Traumatic Stress, 20, 173–182. doi:10.1002/jts.20198 [DOI] [PubMed] [Google Scholar]
- Ozer E. J., Best S. R., Lipsey T. L., & Weiss D. S. (2003). Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin, 129, 52–73. doi:10.1037/0033-2909.129.1.52 [DOI] [PubMed] [Google Scholar]
- Regambal M. J., & Alden L. E. (2009). Pathways to intrusive memories in a trauma analogue paradigm: A structural equation model. Depression and Anxiety, 26, 155–166. doi:10.1002/da.20483 [DOI] [PubMed] [Google Scholar]
- Reilly-Harrington N. A., Alloy L. B., Fresco D. M., & Whitehouse W. G. (1999). Cognitive styles and life events interact to predict bipolar and unipolar symptomatology. Journal of Abnormal Psychology, 108, 567–578. doi:10.1037/0021-843X.108.4.567 [DOI] [PubMed] [Google Scholar]
- Resick P. A., & Schnicke M. K. (1993). Cognitive processing therapy for rape victims. Newbury Park, CA: Sage. [DOI] [PubMed] [Google Scholar]
- Resnick H. S., Kilpatrick D. G., Dansky B. S., Saunders B. E., & Best C. L. (1993). Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology, 61, 984–991. doi:10.1037/0022-006X.61.6.984 [DOI] [PubMed] [Google Scholar]
- Riskind J. H., & Alloy L. B. (2006). Cognitive vulnerability to emotional disorders: Theory, design, and methods. In Alloy L. B. & Riskind J. H. (Eds.), Cognitive vulnerability to emotional disorders (pp. 1–29). Mahwah, NJ: Erlbaum. [Google Scholar]
- Rothbaum B. O., Foa E. B., Riggs D. S., Murdock T. B., & Walsh W. (1992). A prospective examination of posttraumatic stress disorder in rape victims. Journal of Traumatic Stress, 5, 455–475. doi:10.1002/jts.2490050309 [Google Scholar]
- Smith J. M., & Alloy L. B. (2009). A roadmap to rumination: A review of the definition, assessment and conceptualization of this multifaceted construct. Clinical Psychology Review, 29, 2, 116–128. doi:10.1016/j.cpr.2008.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teasdale J. D., & Barnard P. J. (1993). Affect, cognition, and change: Re-modelling depressive thought. Hove, UK: Erlbaum. [Google Scholar]
- Teasdale J. D., & Cox S. G. (2001). Dysphoria: Self-devaluative and affective components in recovered depressed patients and never depressed controls. Psychological Medicine, 31, 1311–1316. doi:10.1017/S003329170100424X [DOI] [PubMed] [Google Scholar]
- Wenninger K., & Ehlers A. (1998). Dysfunctional cognitions and adult psychological functioning in child sexual abuse survivors. Journal of Traumatic Stress, 11, 281–300. doi:10.1023/A:1024451103931 [DOI] [PubMed] [Google Scholar]
- Williams J. M. G. (2003). Hopelessness scale: Short form. Unpublished manuscript. [Google Scholar]
- Zatzick D. F. (2003). Posttraumatic stress, functional impairment, and service utilization after injury: A public health approach. Seminars in Clinical Neuropsychiatry, 8, 149–157. doi:10.1016/S1084-3612(03)00017-0 [DOI] [PubMed] [Google Scholar]