Abstract
Objective:
A prospective prevalence study of primary headache disorders in school going children (8–18 years) in Srinagar district of Kashmir valley was conducted.
Materials and Methods:
The study population comprised of a randomized sample of 5000 school going children in the age group of 8–18 years from various educational institutions of Srinagar city. A self-administered pretested questionnaire was filled by the participants and the diagnosis established by following the International Headache Society criteria (IHS) 2004.
Results:
The overall prevalence of primary headache disorders was found to be 664/1000. The prevalence of tension-type headache and migraine was found to be 50.99% and 26.98%, respectively. The prevalence revealed an upward trend with increasing age with preponderance for female sex.
Keywords: Children, headache, India, Kashmir, prevalence
Introduction
Headache is one of the most frequent complaints evaluated by internists and neurologists in the office practice.[1] Primary headaches are unaccompanied by any structural, metabolic or any other lesion in the body in general and brain in particular, whereas secondary headaches are caused by exogenous disorders.[2] Common forms of primary headache disorders as per population prevalence include tension-type headache (TTH) (69%) and migraine (16%).[3]
Migraine is a ubiquitous familial disorder characterized by periodic, often unilateral, pulsatile headache, which begins in childhood, adolescence or early adult life and recurs with diminishing frequency during advancing years. Migraine with aura (classic or neurologic migraine) is ushered in by an evident disturbance of nervous function, most often visual, followed in a few minutes by hemicranial or in about 1/3rd of the cases, by bilateral headache, nausea and sometimes vomiting, all of which last for 4–72 h. Migraine without aura (common migraine) is characterized by a sudden onset of hemicranial or less often by global headache with or without nausea and vomiting, which then follows the same temporal pattern as the migraine with aura. Photophobia and phonophobia accompany both types of migraine.[2] Migraine and TTH have been considered distinct entities by the International Headache Society.[4]
The only hospital-based, cross-sectional study about the profile of various headache disorders in Kashmir valley revealed preponderance of TTH over migraine. However, majority of the patients in this study were adults and therefore is not representative of headache disorders in childhood.[5] The present study is a maiden endeavor to assess the magnitude of various headache disorders among school going children in Kashmir valley of north India.
Materials and Methods
Eligible subjects included students between 8 and 18 years of age from various schools falling within the jurisdiction of the Srinagar Municipal Corporation. A randomized sample of 5000 school going children from various public schools of Srinagar city was included in the study. In order to include a representative sample of school children, one class from every grade (grade 2–12) was randomly selected from each of the schools of Srinagar city. The randomization was performed with the help of the available list of classes/schools with the state education department and random numbers generated by a computer.
The questionnaire was formulated on the basis of the International Headache Society criteria for the diagnosis of headache disorders, and included questions pertaining to issues such as duration, onset, type, severity, frequency and associated features like aura, nausea, vomiting, tinnitus, parasthesias, visual obscurations and, lastly, any aggravating or relieving factors. Participants who reported less than three episodes of headache in life time, headache of less than 2 h of duration and those who did not remember description of their headache were excluded from the study to remove the recall bias. Moreover, individuals with headache secondary to sinusitis, brain tumors or due to any other systemic disorders too were excluded from the study. In order to validate the questionnaire, a pilot study was carried out in which a random sample of 254 school going children, stratified for age and sex, were interviewed and examined by a resident doctor. The concerned head teacher distributed the questionnaires, which were filled up at home by the students or their parents/guardians. The questionnaire was provided to every student, but only those who gave consent for participation in the study were included. The consent was obtained from parents as well as from school authorities to participate in the study. Fifteen percent of the students did not return the questionnaire and were excluded from the study. The questionnaire was interpreted in local vernacular wherever deemed necessary. The diagnosis of various headache disorders was established by adopting the International Headache Society criteria (2004).[4] The study was conducted by a team of residents. Subsequently, the diagnosis was affirmed by the neurologist after detailed history and relevant examination. The stress was assessed by the DASS21 scale.[6]
The study protocol was approved by the institutional review and ethical committee.
Results
For data analysis, Student's t-test, Chi-square test and Fishers exact test were used, with a P value of <0.05 being considered to be statistically significant.
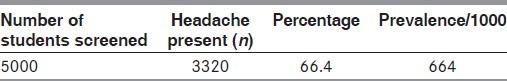
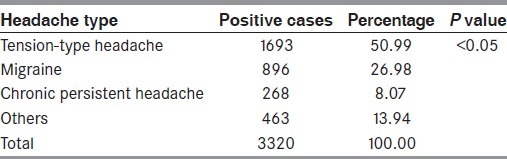
The student population consisted of 5000 subjects, which included 2727 (54.54%) females and 2273 (45.46%) males. The students fulfilling IHS criteria numbered 3320 (66.4%) [Table 1].
Table 1.
Prevalence of primary headache disorders in school children
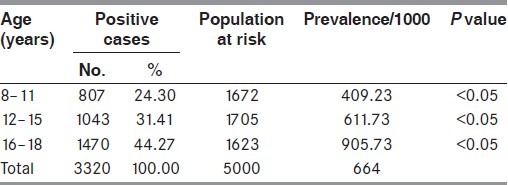
The prevalence of primary headache disorders was more common in female sex (65.15%) as compared with male gender (35.85%), which was statistically significant (P value <0.05) [Table 2] The study revealed an increasing trend in prevalence of primary headache disorders with an increase in age [Table 3].
Table 2.
Gender-specific prevalence of primary headache disorders in school children
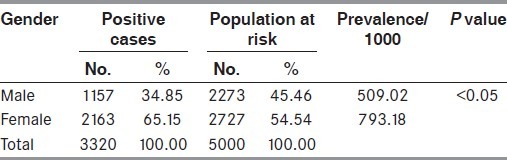
Table 3.
Age-specific prevalence of primary headache disorders in school children
Moreover, the prevalence of primary headache disorders differed according to schooling status of the students. An increase in the prevalence of primary headache disorders was observed among students belonging to government-run educational institutions (882.01/1000) as compared with their counterparts belonging to privately run educational institutions (510.23/10000) [Table 4]. TTH (50.99%) was the most common headache syndrome, followed by migraine (26.98%) [Table 5]. Throbbing quality headache was noticed in 46.05% of the patients, followed by continuous headache in 13.19% and pressing quality in 18.01% cases.
Table 4.
Headache prevalence in relation to schooling status
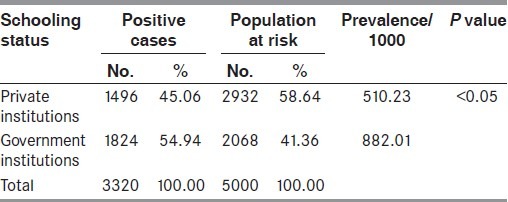
Table 5.
Prevalence of headache subtypes in school children
Furthermore, a positive family history of headache was elicited in 66.18% of migraneurs as compared with 35% in the tension-type group, the difference being statistically significant (P value <0.05).
Other noteworthy findings in the present study included: (i) aura was associated with 35.49% of the students with migranous headache, (ii) average frequency, duration and age of onset of first episode of headache was 2.6 episodes/month, 6.3 h and 9.2 years, respectively, (iii) stress that included mental stress, sleep deprivation, physical exertion, watching TV for long hours, etc. was the most common trigger factor for all primary headache disorders in general and more so for migraine (85.06%) than TTH (43.08%), (iv) majority of the patients received analgesics (77.5%) to relieve their headache and (v) the primary headache disorders contributed to 34.61% of the total school days lost in a calendar year.
Discussion
Headache in the pediatric population is underdiagnosed and undertreated, despite a high prevalence of headache disorders in children and adolescents.[7] Headaches, although not uncommon during childhood, tend to increase in frequency during adolescence.
The present epidemiological study regarding prevalence of primary headache disorders in school going children in Kashmir valley is a maiden endeavor from this part of the world. Prevalence of primary headache disorders in school going children in the literature varies from 27.2% to 72.90% in males and 76% to 98% in females.[8] Our study revealed a prevalence of primary headache disorders in female sex to the tune of 65.15% and that in males as 34.85%. This finding is statistically significant and consistent with other data reported in the literature.[8]
An upward trend in the prevalence of primary headache disorders with increase in age was observed, which again is in agreement with the results of other researchers.[8–11]
Various studies revealed a higher prevalence of primary headache disorders in children studying in government schools as compared with their counterparts studying in private schools.[12,13] The results of the present study are in tandem with those of other researchers, showing a higher prevalence of headache in children studying in government and socially underprivileged schools than those studying in privately run educational institutions. This may be attributed to lack of access to adequate medicare facilities to children studying in government-run educational institutions as majority of these children belong to the lower socioeconomic strata.
Our study revealed TTH as the most common primary headache disorder (50.99%), followed by migranous headache. TTH was the most common headache type observed by other researchers as well.[9,12,14–16]
Nausea was the most common associated feature (46.32%), followed by phonophobia (23.11%) and vomiting (23.10%), respectively, and, again, the results are comparable with other researchers.[17–20]
Average duration of primary headache disorders was 6.3 h and mean age of onset and number of episodes/month was 9.2 years and 2.6 episodes/month, respectively. The results are in conformity with the available literature.[8,9,21] A positive family history of headache disorders was obtained in 66.18% of the migraneurs as compared with 35% in the TTH group, which was consistent with other studies.[12,14,21]
Stress (73.40%) was the most common factor, followed by fasting/missed meals and sleep deprivation. Menstruation as a trigger factor was reported by 32.27% of the cases. Majority of our observations are comparable to the available literature.[5,9,14,21,22] 77.5% of the children with headache used analgesics followed by sleep, rest, scalp massage and application of cold substances to the scalp to relieve their headache with mixed results.
Moreover, the study revealed that children on an average lost 3.6 school days due to primary headache disorders in a calendar year, which is lower, although statistically insignificant, in comparison with the available literature, showing a mean of 2.8 school days lost in a calendar year.[10]
Conclusion
The study revealed an overall prevalence of primary headache disorders among school going children to the tune of 664/1000 population with an upward trend with increase in age. Gender-specific prevalence rates revealed a statistically significant higher prevalence of primary headache disorders in the female sex. Among all the primary headache disorders, TTH was the most common headache disorder, followed by migrainous headache, and stress was the most common trigger for all headache disorders.
Furthermore, studies are required in the future to find out precipitating factors for primary headache disorders to avoid its adverse impact on the quality of life as well as unnecessary use of medications to alleviate headache.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
References
- 1.Raieli V, Raimondo D, Cammalleri R, Camarda R. Migraine headaches in adolescents: A student population-based study in Monreale. Cephalgia. 1995;15:4–12. doi: 10.1046/j.1468-2982.1995.1501005.x. [DOI] [PubMed] [Google Scholar]
- 2.Goadsby PJ, Raskin NH. Headache. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, Loscalzo J, editors. Harrison's Principles of Internal Medicine. 17th ed. McGraw-Hill Companies, United States of America, Inc; 2008. pp. 95–107. [Google Scholar]
- 3.Olesen J, Tfelt-Hansen P, Michael Welch K, Goadsby PJ, Ramadan NM, et al. The Headaches. 3rd ed. Philadelphia: Lippincott, Williams and Wilkins; 2005. [Google Scholar]
- 4.Headache classification subcommittee of the International Headache Society. Cephalgia. 2004;24(Suppl 1):1–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 5.Shah PA, Nafae A. Clinical profile of headache and cranial neuralgias. J Assoc Physc Ind. 1999;47:1072–5. [PubMed] [Google Scholar]
- 6.Levibond SH, Levibond PF. Manual for the depression anxiety stress scale. 2nd ed. Sydney, Australia: Physiology foundation, University of New South Wales; 1995. [Google Scholar]
- 7.Paul Winner. Overview of pediatric headache. Current treatment options in neurology. Headache. 2004;3:38–54. doi: 10.1007/s11940-004-0005-8. [DOI] [PubMed] [Google Scholar]
- 8.Linet MS, Stewart WF, Celentano DD, Ziegler D, Sprecher M. An epidemiologic study of headache among adolescents and young adults. JAMA. 1989;261:2211–6. [PubMed] [Google Scholar]
- 9.Sillanpaa M, Piekkala P. Prevalence of migraine and other headaches in early puberty. Scand J Prim Health Care. 1984;2:27–32. doi: 10.3109/02813438409017698. [DOI] [PubMed] [Google Scholar]
- 10.Abu-Arefeh I, Russel G. Prevalence of headache and migraine in school children. BMJ. 1994;309:765–9. doi: 10.1136/bmj.309.6957.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mortimer MJ, Kay J, Jaron A. Childhood migraine in general practice, clinical features and characteristics. Cephalalgia. 1992;12:238–43. doi: 10.1046/j.1468-2982.1992.1204238.x. [DOI] [PubMed] [Google Scholar]
- 12.Barea LM, Tannhauser M, Rotta NT. An epidemiologic study of headache among children and adolescents of southern Brazil. Cephalagia. 1996;26:545–9. doi: 10.1046/j.1468-2982.1996.1608545.x. [DOI] [PubMed] [Google Scholar]
- 13.Alfven G. The covariation of common psychosomatic symptoms among children from socio-economically differing residential areas. An epidemiological study. Acta Paediatr. 1993;83:484–7. doi: 10.1111/j.1651-2227.1993.tb12728.x. [DOI] [PubMed] [Google Scholar]
- 14.Bugdayci R, Ozge A, Sasmaz T, Kurt AO, Kaleagasi H, Karakelle A, et al. Prevalence and factors affecting headache in Turkish school children. Pediatr Int. 2005;47:316–22. doi: 10.1111/j.1442-200x.2005.02051.x. [DOI] [PubMed] [Google Scholar]
- 15.Laurrel K, Larsson B, Eeg-Olofsson O. Prevalence of headache in Swedish schoolchildren, with a focus on tension-type headache. Cephalalgia. 2004;24:380–8. doi: 10.1111/j.1468-2982.2004.00681.x. [DOI] [PubMed] [Google Scholar]
- 16.Sillanpaa M. Changes in the prevalence of migraine and other headaches during the first seven school years. Headache. 1983;23:15–9. doi: 10.1111/j.1526-4610.1983.hed2301015.x. [DOI] [PubMed] [Google Scholar]
- 17.Sillanpaa M, Piekkela P, Kero P. Prevalence of headache at preschool age in an unselected child population. Cephalalgia. 1991;11:239–342. doi: 10.1046/j.1468-2982.1991.1105239.x. [DOI] [PubMed] [Google Scholar]
- 18.Viswanathan V, Bridges SJ, Whitehouse W, Newton RW. Childhood headache: Discrete entities or cantinum? Dev Med Child Neurol. 1988;40:544–50. doi: 10.1111/j.1469-8749.1998.tb15413.x. [DOI] [PubMed] [Google Scholar]
- 19.Wöber-Bingöl C, Wöber C, Karwautz A, Vesely C, Wagner-Ennsgraber C, Amminger GP, et al. Diagnosis of headache in childhood and adolescence: A study in 437 patients. Cephalalgia. 1995;15:13–21. doi: 10.1046/j.1468-2982.1995.1501013.x. [DOI] [PubMed] [Google Scholar]
- 20.Seshia SS, Wolstein JR, Adams C, Booth FA, Rggin JD. International headache society criteria and childhood headache. Dev Med Child Neurol. 1994;36:419–28. doi: 10.1111/j.1469-8749.1994.tb11868.x. [DOI] [PubMed] [Google Scholar]
- 21.Zencir M, Ergin H, Sahiner T, Kiliç I, Alkiş E, Ozdel L, et al. Epidemiology and symptomatology of migraine among school children: Denzizil urban area in Turkey. Headache. 2004;44:780–5. doi: 10.1111/j.1526-4610.2004.04145.x. [DOI] [PubMed] [Google Scholar]
- 22.Aromaa M, Rautova P, helenius H, Sillanpaa M. Factors of early life as predictors of headaches in children at school entry. Headache. 1998;38:23–30. doi: 10.1046/j.1526-4610.1998.3801023.x. [DOI] [PubMed] [Google Scholar]


