Abstract
Objective:
The objective of this investigation was to determine the prevalence of migraine and headache symptoms in a national sample of US office employees. Also, we explored the association of headache symptoms with indoor environmental parameters of the work place.
Background:
Sick building syndrome (SBS), which includes headache, is a common global phenomenon, but the underlying environmental cause is uncertain.
Materials and Methods:
We used data from the 1994–1998 US Environmental Protection Agency's (EPA) Building Assessment and Survey Evaluation, a cross-sectional study of workers employed in 100 public and private office buildings across 25 states. The study used a self-administered questionnaire to assess headache frequency and prevalence of self-reported physician-diagnosed (SRPD) migraine. Indoor environmental parameters (IEP) were collected per EPA protocol from each building over a 1-week period and included carbon dioxide, carbon monoxide, temperature, relative humidity, particulate matter, volatile organic compound, illuminance, and sound level. The standards of American Society of Heating, Refrigerating and Air Conditioning Engineers were used to categorize IEP as either within- or out-of-comfort range for human dwelling. These limits delineate whether a parameter value is safe for human dwelling. Out-of-comfort range IEPs are associated with SBS and other human diseases. SRPD migraine and headache frequency were the primary outcome measures of the study. Multivariate logistic regression analyses were employed for the purpose of assessing the association between the outcome variable and IEPs.
Results:
Of the 4326 participants, 66% were females and 60% were between 30 and 49 years. Headache frequency during the last 4 weeks was as follows: None in 31%, 1–3 days in 38%, 1–3 days per week in 18%, and every or almost every workday in 8%. Females had higher SRPD migraine prevalence compared to males (27% vs. 11%, P<0.001) and were more likely to report any headache in the last month compared to males (75% vs. 53%, P<0.001). Odds of SRPD migraine were higher (P<0.05) for those exposed to IEP out-of-comfort range, and odds of exposure to out-of-comfort range IEPs were higher in groups who reported higher headache frequencies.
Conclusions:
Migraine diagnosis and elevated headache frequency are associated with an uncomfortable indoor environment. Periodic assessments and adjustments of IEP may have a beneficial impact on employees who are vulnerable to SBS.
Keywords: EPA BASE study, headache, indoor environmental parameter, migraine, sick building syndrome
Introduction
Subsequent to the oil crisis in 1970s, the rise of fuel prices heightened the importance of energy conservation. In order to conserve energy, attempts were made to make buildings airtight. As a result, many building types, especially offices, hotels, public and educational buildings, became totally dependent on artificial heating, ventilation and air-conditioning (HVAC) systems. Indoor environmental quality (IEQ) of artificially ventilated buildings tends to be problematic due to the continuous use of HVAC systems.[1] Additionally, improper operation and maintenance of HVAC systems results in contaminants and gases being circulated from one part of the system to another. IEQ is a measure of various indoor environmental parameters (IEPs) that include illuminance, temperature, sound level, relative humidity (RH), and presence of pollutants [such as volatile organic compound (VOC), particulate matter of less than or equal to 10 μm (PM 10)] and gases (such as carbon monoxide and carbon dioxide).[2]
During the last three decades, investigators have reported a high prevalence of symptoms that are associated with poor IEQ among the occupants of artificially ventilated office buildings.[1,3,4] These complaints are often referred to as “sick building syndrome” (SBS), a term the United States Environmental Protection Agency (EPA)[5] uses to describe situations in which building occupants experience acute health effects that appear to be linked to time spent in a building, but no specific illness or cause can be identified. SBS has been characterized by headache, fatigue, dizziness, symptoms of irritation in eyes, nose, throat, lower airways, and/or skin, and non-specific hyper reactivity.[6] Considering that Americans spend nearly 90% of their time indoors and nearly 25% of the US residents are affected by poor IEQ either at the workplace or at home, EPA ranks poor IEQ as one of the severe national environmental threats.[7] Although extensive resources have been devoted to the investigation of IEQ problems over the last three decades, the etiology of SBS still remains elusive.
Investigators of SBS have noticed that headaches represent the single most common symptom in almost all indoor environmental studies,[8] but there is a paucity of research on the association between headache symptoms and IEPs. Among the few studies that have examined headache symptoms and IEQ, one study reported that increasing air temperature above 73.4°F with RH above 50% increased the intensity of headache among a small group of female office workers.[9] In another study, the effect of air temperature on the occupants’ headache was also reported to be significant.[10] Headache symptoms were found to be less frequent and of lower intensity among the occupants when a personalized ventilation system supplied outdoor air at 68°F, while the most intense symptoms occurred with mixing ventilation.[11] Other studies have revealed partial correlation between symptoms of headaches, dizziness, heavy headedness, tiredness, difficulties in concentrating among occupants with unpleasant odor, and high CO2 concentrations.[10,12] Within the wide spectrum of studies trying to identify the association of SBS symptoms with IEPs, no study has investigated the epidemiology of headache symptoms among occupants as it relates to the indoor environmental parameters of their work place. Therefore, the purpose of this study was to determine the prevalence of migraine and headache symptoms in a national sample of US office workers. Also, we explored the association of headache symptoms of these workers with IEPs of their work places.
Materials and Methods
Materials
This was a multi-center cross-sectional study of office workers (N=4326) employed in 100 randomly selected large office buildings across 25 states in the US. The study used the data collected by EPA for the Building Assessment Survey and Evaluation (BASE) study during 1994–1998. Data and samples were collected in each of 100 “large” office buildings with a minimum of 50 employees in “metropolitan” cities using a standard protocol over a 1-week period during either the summer or winter season.[13] IEP data were collected from each building over a period of 1 week; data of occupants’ health symptoms were also collected during the same week.
The BASE study confidentially collected occupant information, including gender, age, and health symptoms using a self-administered questionnaire. Data on the prevalence of headache symptoms were collected using a 4-point Likert-type scale that assessed the frequency of headaches in the last 4 weeks as follows: None, 1–3 days, 1–3 days per week, and every or almost every workday. Data on self-reported physician-diagnosed (SRPD) migraine were also collected by asking the participants if a physician had ever diagnosed them with migraine. The responses were in “yes” or “no” format.
Methods
At each office building, the IEPs were measured at three indoor locations that were randomly selected. Real-time data on illuminance, sound level, indoor temperature, RH, carbon monoxide (CO), and carbon dioxide (CO2) were collected as 5-minute averages. For the purpose of analyses, this study has used the data collected over a nominal 9-hour period from 8:00 am to 5:00 pm, assuming it to be normal daytime working hours. Two types of monitoring locations were established in each of the study buildings: Fixed and mobile. There were four fixed and five mobile indoor monitoring locations in each of the buildings. In addition, there was one outdoor fixed monitoring location. While integrated, continuous, and real-time time monitoring was conducted at the fixed locations, real-time measurements were collected at the mobile locations. An average for the 7-day period was computed to represent a constant value of the parameter during the office hours in each building as that is the time when workers are exposed to IEPs. VOC canister samples were collected and analyzed by gas chromatograph-mass spectrometry using standardized method.[14] PM 10 particles was collected on filters, and their mass was computed by measuring the difference in filter weights before and after sampling and dividing it by the sample volume.[14]
Over the last several years, large-scale measurements of indoor pollutants have been made during investigations of suspected sick buildings. However, there are no well-established limits yet for the exposure to internal pollutants in non-industrial buildings such as offices or homes. The limits set by institutions such as National Institute for Occupational Safety and Health (NIOSH) and American Society of Heating, Refrigerating and Air Conditioning Engineers (ASHRAE) are targeted for industrial environments.[1] For this study, ASHRAE's standards were used to categorize IEPs of the buildings as within- or out-of-comfort range for human dwelling. These limits delineate whether a parameter value is safe for human dwelling. Out-of-comfort range IEPs are associated with SBS and other human diseases. RH of 30–60% and temperatures of 69°F–75°F were considered within range. For all other parameters, the values above the sample mean for all the buildings were considered to be out of range and the values below the sample mean were considered to be within range.
Data analysis
Data from the study were analyzed using SPSS 17.0. Data analysis included descriptive statistics with a report of the appropriate frequencies, means, and standard deviations to describe the responses to the questionnaire items as well as the demographic and background characteristics of the respondents. Binary logistic regression analyses were employed to compute the association between the outcome (headache) and selected environmental exposures.
Results
Of the 4326 participants, 66% were females and 60% were between 30 and 49 years of age [Table 1]. Headache frequency reported by the study participants in the past 4 weeks was: None in 31%, 1–3 days in 38%, 1–3 days per week in 18%, and every or almost every workday in 8%.
Table 1.
Selected characteristics of study participants
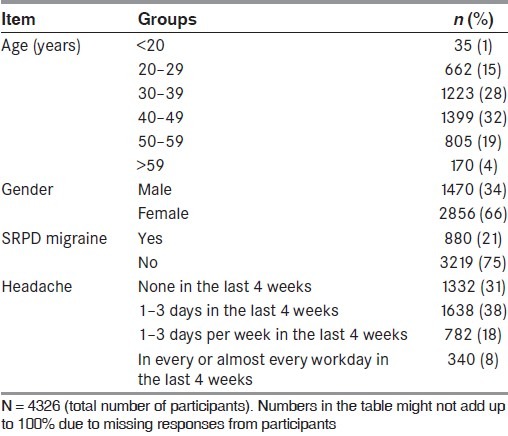
Twenty-one percent of participants had SRPD migraine. Females had higher SRPD migraine prevalence than males [27% vs. 11%; odds ratio (OR) 3.16, 95% confidence interval (CI) 2.61–3.82, P<0.001]. Participants were categorized into two groups based on having or not having any headache in the last 4 weeks. Sixty-three percent of the participants reported having any headache in the past 4 weeks. Females were more likely to report any headache in the last 4 weeks compared to males (75% vs. 53%; OR 2.71, 95% CI 2.37–3.11, P<0.001). The prevalence of SRPD migraine was 7% in the group that reported no headaches, 21% in the group that reported 1–3 headache days in the last 4 weeks, 35% in the group that reported 1–3 headache days per week in the last 4 weeks, and 51% in the group that reported headaches every or almost every workday in the last 4 weeks.
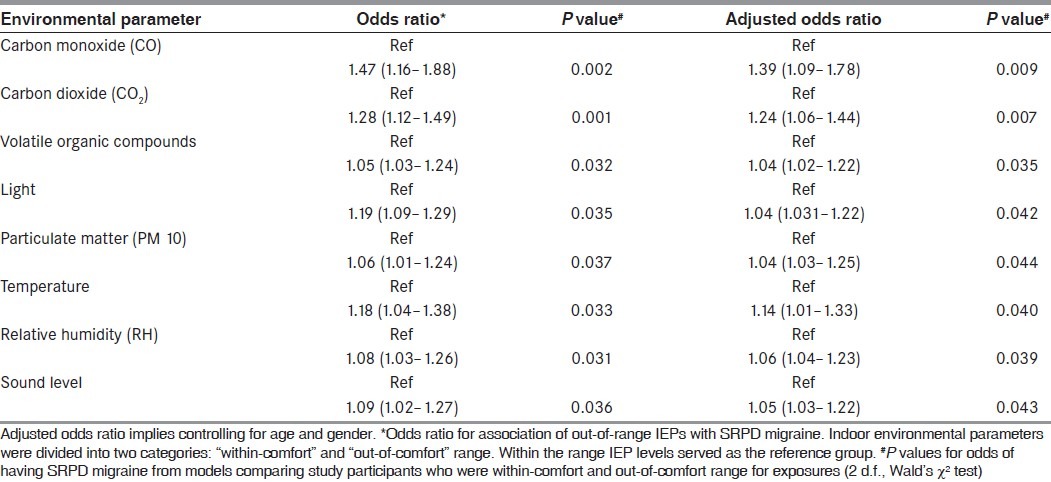
IEPs’ exposures were categorized into two groups: Within-comfort range and out-of-comfort range for human dwelling. Multivariate logistic regression showed odds of SRPD migraine to be higher (P<0.05) for those exposed to IEPs out-of-comfort range [Table 2]. The odds for having SRPD migraine were highest for those individuals who were exposed to out-of-comfort range carbon monoxide (OR 1.47, 95% CI=1.16–1.88, P=0.002) and carbon dioxide (OR 1.28, 95% CI=1.12–1.49, P=0.001). The odds for having SRPD migraine were almost similar for those individuals who were exposed to out-of-comfort range light (OR 1.19, 95% CI=1.01–1.29, P=0.035) and temperature (OR 1.18, 95% CI=1.04–1.38, P=0.03). Analyses adjusted for gender and age did not significantly alter the odds for having SRPD migraine based on exposure to out-of-comfort range IEPs. Gender was a significant predictor for migraine, but age was not. An interaction between age and gender was significant for IEPs and SRPD migraine.
Table 2.
Logistic regression analysis for association of SRPD migraine with indoor environmental parameters
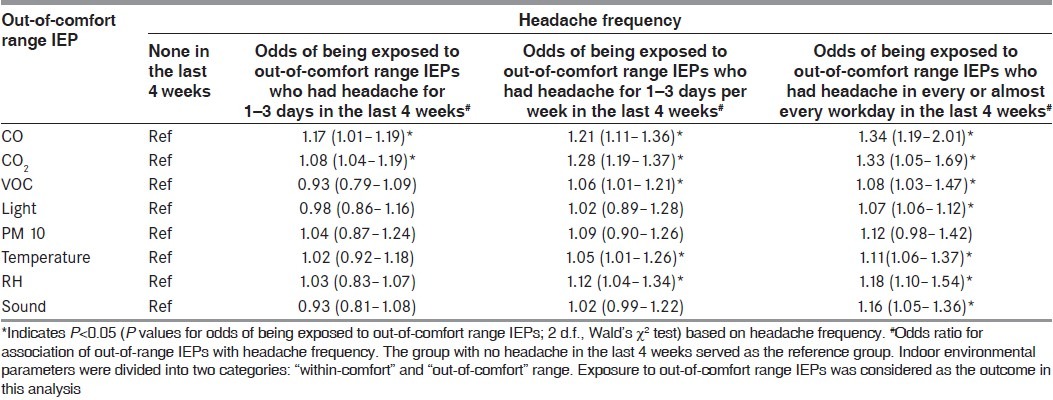
A logistic regression was also conducted to assess the odds of exposure to out-of-comfort range IEPs in different groups of study participants based on their headache frequencies in the last 4 weeks as compared to the group of individuals who reported no headaches in the past 4 weeks. Odds of exposure to out-of-comfort range IEPs were higher in groups that reported higher headache frequencies [Table 3]. As compared to individuals with no headaches, the odds of reporting exposure to out-of-comfort range carbon monoxide was high for individuals with 1–3 days of headache in the last 4 weeks (OR=1.17, 95% CI=1.01–1.19), higher for individuals with headache for 1–3 days per week in the last 4 weeks (OR=1.21, 95% CI=1.11–1.36), and highest for those individuals who had headaches in every or almost every workday in the last 4 weeks (OR=1.34, 95% CI=1.19–2.01). Similarly, as compared to individuals with no headaches, the odds of reporting exposure to out-of-comfort range carbon dioxide was high for individuals with 1–3 days of headache in the last 4 weeks (OR=1.08, 95% CI=1.04–1.19), higher for individuals with headache for 1–3 days per week in the last 4 weeks (OR=1.28, 95% CI=1.19–1.37), and highest for those individuals who had headaches every or almost every workday in the last 4 weeks (OR=1.33, 95% CI=1.05–1.69). Odds of exposure to out-of-comfort levels of VOC, temperature, and RH were significantly higher (P<0.05) in individuals who reported headache frequency of more than or equal to 1–3 days per week in the last 4 weeks, as compared to individuals who reported no headaches or headaches for 1–3 days in the last 4 weeks. Analysis with models that considered males only and females only was conducted. The associations held true for female only models, but were lost for male only models.
Table 3.
Logistic regression analysis for odds of exposure to out.of.comfort range IEP in groups based on headache frequency
Discussion
In this study, we found the prevalence of SRPD migraine to be similar to that reported in population-based surveys of persons of similar age.[15] However, considering the fact that many persons with migraine never seek medical attention and are therefore undiagnosed, it is difficult to compare the prevalence rates of our study with those of population-based surveys. Our finding that migraine is associated with indoor environmental parameter abnormalities in people working in mechanically ventilated environment is corroborated by an earlier study, which found the association with migraine to be higher than in naturally ventilated buildings, particularly when the mold and dust content was high.[16] In addition, the literature also supports the association of headache with CO and particulate exposure.[17–19] Our findings that a migraine diagnosis is more common in those exposed at work to out-of-comfort range light and sound has been reported, but usually in the context of these parameters serving as a trigger in susceptible individuals.[20,21] The impact of temperature and RH on migraine has been found to be negligible, but these data are from studies of the weather rather than the indoor environment.[22,23]
The finding that the odds of exposure to out-of-comfort range IEP increased with increasing headache frequency is novel and suggests a possible association. The etiology is uncertain, but it has been hypothesized that chemical irritants in the environment entering through the body through the respiratory system directly trigger peripheral nerve receptors. When the impulse is relayed to the central nervous system, it is redirected to another location, leading to the release of inflammatory neuropeptides at this distant site. This process is referred to as neurogenic switching and has been implicated as a potential mechanism of the SBS–migraine association.[24]
The strengths of the study include the large number of sites and their geographic diversity, as well as the broad spectrum of IEPs we selected. There are, however, several limitations of this study. The information on migraine prevalence comes from self reports, and we do not have information on whether physicians based the diagnosis on International Headache Society (IHS) criteria. In addition, it is not clear whether the diagnosis of migraine was established before or after starting of employment. Fixed site monitoring in each building may not fully reflect variation in exposure between individuals. Also, individual data on potential confounders such as socioeconomic status, race, medication use, and co-morbid conditions were not available. A variety of confounders that could relate to headache were not considered in the analysis as the original database did not have detailed elicitation of this information from participants. This may have limited our abilities to capture the true odds of having headaches in an environment that would be considered out of human comfort zones. However, higher odds of health symptoms have also been reported by several investigators who have analyzed this database for other health problems.[25,26] Lastly, associations between IEPs decrease our ability to attribute the observed associations to individual parameters.
Whatever the cause, headaches related to office environment may have an impact on productivity. Several studies suggest that poor indoor air quality may affect productivity.[25–27] Effective intervention strategies to reduce prevalence of headache and other symptoms of SBS should follow a systematic approach. Collecting frequent data of IEPs of the office buildings and employing a monitoring system is of prime importance. Based on the IEP data collected, a health risk management plan for the occupants should be designed. Additionally, as work stress appears consistently associated with symptoms,[28] the occupants should be educated through proper health promotion programs. Strategy to increase awareness among the occupants on health and IEQ in general and air pollution and health effects in particular should be instituted as part of the health promotion programs. Lastly, reformation of operation and maintenance program of HVAC systems should be made an integral part of the systematic intervention strategy.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
References
- 1.Rios JL, Boechat JL, Gioda A, dos Santos CY, de Aquino Neto FR, Lapa e Silva JR. Symptoms prevalence among office workers of a sealed versus a non-sealed building: Associations to indoor air quality. Environ Int. 2009;35:1136–41. doi: 10.1016/j.envint.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 2.Wolkoff P, Nøjgaard JK, Franck C, Skov P. The modern office environment desiccates the eyes? Indoor Air. 2006;16:258–65. doi: 10.1111/j.1600-0668.2006.00429.x. [DOI] [PubMed] [Google Scholar]
- 3.Reynolds SJ, Black DW, Borin SS, Breuer G, Burmeister LF, Fuortes LJ, et al. Indoor environmental quality in six commercial office buildings in the midwest United States. Appl Occup Environ Hyg. 2001;16:1065–77. doi: 10.1080/104732201753214170. [DOI] [PubMed] [Google Scholar]
- 4.Zweers T, Preller L, Brunekreef B, Boleij JSM. Health and indoor climate complaints of 7043 office workers in 61 buildings in the Netherlands. Indoor Air. 1992;2:127–36. [Google Scholar]
- 5.United States Environmental Protection Agency. Indoor air facts no. 4: Sick building syndrome. Available from: http://www.epa.gov/iaq/pubs/sbs.html .
- 6.Indoor Air Pollutants: Exposure and Health Effects. Copenhagen: 1983. World Health Organization Regional Office for Europe. [Google Scholar]
- 7.Guieysse B, Hort C, Platel V, Munoz R, Ondarts M, Revah S. Biological treatment of indoor air for VOC removal: Potential and challenges. Biotechnol Adv. 2008;26:398–410. doi: 10.1016/j.biotechadv.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 8.Schwartz BS, Stewart WF, Simon D, Lipton RB. Epidemiology of tension-type headache. JAMA. 1998;279:381–3. doi: 10.1001/jama.279.5.381. [DOI] [PubMed] [Google Scholar]
- 9.Fang L, Wyon DP, Clausen G, Fanger PO. Impact of indoor air temperature and humidity in an office on perceived air quality, SBS symptoms and performance. Indoor Air. 2004;14:74–81. doi: 10.1111/j.1600-0668.2004.00276.x. [DOI] [PubMed] [Google Scholar]
- 10.Norbäck D, Nordström K. Sick building syndrome in relation to air exchange rate, CO(2), room temperature and relative air humidity in university computer classrooms: An experimental study. Int Arch Occup Environ Health. 2008;82:21–30. doi: 10.1007/s00420-008-0301-9. [DOI] [PubMed] [Google Scholar]
- 11.Kaczmarczyk J, Melikov A, Fanger PO. Human response to personalized ventilation and mixing ventilation. Indoor Air. 2004;14:17–29. doi: 10.1111/j.1600-0668.2004.00300.x. [DOI] [PubMed] [Google Scholar]
- 12.Myhrvold AN, Olsen ELauridsen O. Proceedings of Indoor Air ‘96: The 7th International Conference on Indoor Air Quality and Climate. Vol. 4. Nagoya, Japan: 1996. Indoor environment in schools - pupils health and performance in regard to CO2 concentrations; pp. 369–74. [Google Scholar]
- 13.United States Environmental Protection Agency. Building assessment survey and evaluation (BASE) study: Methodology. Available from: http://www.epa.gov/iaq/base/methodology.html .
- 14.United States Environmental Protection Agency. A standardized EPA protocol for characterizing indoor air quality in large office buildings. Available from: http://www.epa.gov/iaq/base/pdfs/2003_base_protocol.pdf .
- 15.Lipton RB, Stewart WF, Diamond S, Diamond ML, Reed M. Prevalence and burden of migraine in the United States: Data from the American Migraine Study II. Headache. 2001;41:646–57. doi: 10.1046/j.1526-4610.2001.041007646.x. [DOI] [PubMed] [Google Scholar]
- 16.Vincent D, Annesi I, Festy B, Lambrozo J. Ventilations system, indoor air quality, and health outcomes in Parisian modern office workers. Environ Res. 1997;75:100–12. doi: 10.1006/enrs.1997.3764. [DOI] [PubMed] [Google Scholar]
- 17.Dales RE, Cakmak S, Vidal CB. Air pollution and hospitalization for headache in Chile. Am J Epidemiol. 2009;170:1057–66. doi: 10.1093/aje/kwp217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Szyszkowicz M. Ambient air pollution and daily emergency department visits for headache in Ottawa, Canada. Headache. 2008;48:1076–81. doi: 10.1111/j.1526-4610.2007.01039.x. [DOI] [PubMed] [Google Scholar]
- 19.Szyszkowicz M, Stieb D, Rowe B. Air pollution and daily ED visits for headache in Edmonton, Canada. Am J Emerg Med. 2009;27:391–6. doi: 10.1016/j.ajem.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 20.Kelman L. The triggers or precipitants of the acute migraine attack. Cephalalgia. 2007;27:394–402. doi: 10.1111/j.1468-2982.2007.01303.x. [DOI] [PubMed] [Google Scholar]
- 21.Niemann H, Bonnefoy X, Braubach M, Hecht K, Maschke C, Rodrigues C, et al. Noise-induced annoyance and morbidity results from the pan-European LARES study. Noise Health. 2006;8:63–9. doi: 10.4103/1463-1741.33537. [DOI] [PubMed] [Google Scholar]
- 22.Villeneuve PJ, Szyszkowicz M, Stieb D, Bourque DA. Weather and emergency room visits for migraine headaches in Ottawa, Canada. Headache. 2006;46:64–72. doi: 10.1111/j.1526-4610.2006.00322.x. [DOI] [PubMed] [Google Scholar]
- 23.Zebenholzer K, Rudel E, Frantal S, Brannath W, Schmidt K, Wöber-Bingöl C, et al. Migraine and weather: A prospective diary-based analysis. Cephalalgia. 2011;31:391–400. doi: 10.1177/0333102410385580. [DOI] [PubMed] [Google Scholar]
- 24.Meggs WJ. Neurogenic switching: A hypothesis for a mechanism for shifting the site of inflammation in allergy and chemical sensitivity. Environ Health Perspect. 1995;103:54–6. doi: 10.1289/ehp.9510354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Erdmann CA, Steiner KC, Apte MG. Indoor Carbon Dioxide Concentrations and Sick Building Syndrome Symptoms in the BASE Study Revisited: Analyses of the 100 Building Dataset. Indoor Air. 2002:443–8. Conference Proceedings. [Google Scholar]
- 26.Apte MG, Fisk WJ, Daisey JM. Associations Between Indoor CO2 Concentrations and Sick Building Syndrome Symptoms in US Office Buildings: An Analysis of the 1994-1996 BASE Study Data. Indoor Air. 2000;10:246–57. doi: 10.1034/j.1600-0668.2000.010004246.x. [DOI] [PubMed] [Google Scholar]
- 27.Wyon DP. The effects of indoor air quality on performance and productivity. Indoor Air. 2004;14:92–101. doi: 10.1111/j.1600-0668.2004.00278.x. [DOI] [PubMed] [Google Scholar]
- 28.Marmot AF, Eley J, Stafford M, Stansfeld SA, Warwick E, Marmot MG, et al. Building health: An epidemiological study of “sick building syndrome” in the Whitehall II study. Occup Environ Med. 2006;63:283–9. doi: 10.1136/oem.2005.022889. [DOI] [PMC free article] [PubMed] [Google Scholar]


