Abstract
Headache is a common complaint that makes up for approximately 25% of any neurologists outpatient practice. Yet, it is often underdiagnosed and undertreated. Ninety percent of headaches seen in practice are due to a primary headache disorder where there are no confirmatory tests, and neuroimaging studies, if done, are normal. In this situation, a good headache history allows the physician to recognize a pattern that in turn leads to the correct diagnosis. A comprehensive history needs time, interest, focus and establishment of rapport with the patient. When to ask what question to elicit which information, is an art that is acquired by practice and improves with experience. This review discusses the art of history-taking in headache patients across different settings. The nuances of headache history-taking are discussed in detail, particularly the questions related to the time, severity, location and frequency of the headache syndrome in general and the episode in particular. An emphasis is made on the recognition of red flags that help in the identification of secondary headaches.
Keywords: Headache, history-taking, migraine
Introduction
Headache is one of the most common of medical complaints with numerous underlying causes and many patterns of presentation. “Headache” cuts across different specialities, occurs in all age groups and in both acute and chronic settings. As different headaches have different treatment, it is imperative to try and first establish a working diagnosis whenever you examine patients who present with headache.
The ideal way to approach a headache patient would be to divide all headaches into two groups: Primary and Secondary, as has been done in The International Headache Society Classification of Headache Disorders (ICHD 2 – 2004).[1] Primary headaches are those headaches where there is no cause identifiable on examination or investigation and where diagnosis is made by recognizing a pattern, e.g. migraine, cluster headache, tension-type headache. Secondary headaches are those headaches where there is a definite underlying cause identifiable on examination or investigation, e.g. brain tumors, meningitis, sub-arachnoid hemorrhage. Ninety percent of headaches seen in practice are primary headaches, and less than 10% are secondary headaches.[2] Primary headaches, although more common, are not life threatening. Secondary headaches are worrisome because they can lead to serious complications. The severity of pain does not indicate whether the headache is of the primary or secondary variety. One of the biggest challenges, therefore, when faced with a headache patient, is to separate the benign primary from the serious secondary. Rarely, secondary headache disorders can mimic a primary headache or may co-exist along with a primary headache.
With imaging and other investigations being noncontributory to the diagnosis of primary headaches, pattern recognition is the key to specific diagnosis. A good history is an invaluable tool to help establish the pattern. Clinicians differentiate between primary and secondary headaches but do not differentiate between the different primary headaches. History is important even with secondary headaches, but here you have the additional support of an appropriate test that will confirm your suspected provisional diagnosis. This review aims to discuss the way to go about taking a comprehensive history in a headache patient across different settings and is based on the author's experience of having seen headache patients through a tertiary headache clinic over the last 15 years. Details of individual diagnostic entities, examination findings, investigative modalities and treatment options are beyond the scope of this article. If it seems too exhaustive, it is meant to be so, because in the modern era of imaging, history taking in headache patients is gradually becoming a forgotten Art. “Choose something common and you will find not much is known about it! And so it is with ‘Headache’!”[3]
Headache History Taking: The Art
Headache history taking is an Art that needs to be perfected by constant practice. You have to ask the right questions in a manner that will elicit information which will lead you to the right diagnosis. Headache patients are in pain, are often depressed and sometimes frustrated because so many earlier treatments have failed. When you evaluate such a patient, you therefore need to first establish a rapport and then ask the right questions based on the right suspicions. You need to improvise as you go along, based on the information obtained and this has to be done in the right sequence. If you have taken a good history, then based on the temporal profile and associated features you should have a provisional differential working diagnosis even before you examine the patient or plan your investigation.
Unfortunately, because of inadequate training in medical school and because headaches are mostly chronic and recurrent in nature, clinicians often lack interest and get frustrated seeing headache patients. As a result, they do not know what to look for, ask only a few questions, accept the patient's self-diagnosis and wrongly conclude that the headache is due to sinus infection or refractive error or stress. We need to train ourselves in the art of history-taking and learn further from experience.
Headache treatment often fails because of a routine hurried history taken without interest. Time is one of the essential prerequisites. You need to understand the patient's misery and be empathetic. Most patients have been through many hasty and failed, disappointing consultations following which the headache has not improved and where they have not been told why the head pains. It has been rightly said that “Patients respond to physicians who respond”.
As with other medical conditions, for headaches also, the first history is usually the best history. Delegating “headache” history taking to a junior physician or nurse assistant and then reconfirming the facts does not help establish rapport and so too is the method of making the patients answer a number of “yes/no” questions on a computer screen. The ambience in which the history is taken also helps. It should ideally be an undisturbed environment with no unexpected intrusions, no disturbing phone calls. Correct focus helps convince the patient and relatives that the doctor is interested and then the patient is willing to volunteer information easily. We need to sometimes literally tease out the headache history in order to avoid misdiagnosis, particularly when there is some overlap, as happens between migraine, cluster headache, sinus-related headache and tension-type headache.
Ideally, the patient should be allowed to speak first, the spouse and relatives can pitch in later to reconfirm the facts or add additional details. It is generally thought that children are not good historians, but all children above the age of 5 years, in our experience, can give their own history. You can ask the questions in a set sequence and ask the patient to provide brief to-the-point answers. When you ask the questions, you are essentially looking for clues – some straight-forward, some subtle. The other way of eliciting a headache history is to ask the patient “Tell me all about your headaches” and then to start asking relevant questions once the patient has finished. “Listen to the Patient quite often he is telling you the Diagnosis!”[4]
Once you are done with questioning the patient, the spouse and relatives can be encouraged to speak and they could also tell you about the medications taken earlier, the investigations done so far, failed treatments, alternative treatments tried out, the extent of disability and the impact of the headache on the patient's life-style. Accompanying persons can often give useful information about other medical illnesses, including depression, drug allergies and other fears. The history should also help you ascertain if the patient has a secondary headache and if so who should ideally treat and if need be he/she should be referred appropriately. The questions that you will ask will differ according to the diagnosis you suspect.
A good and complete history should always be based on sound knowledge of the various underlying conditions that can present with headache. Besides knowing the different causes, you should also know when to suspect which condition. If you do not know what you are looking for, you are not going to find it. “What the mind does not know the eyes are not going to see!”
Under the list of causes, you have to remember not only the neurological conditions but also conditions in the overlap specialities, the systemic causes and psychiatric conditions. It should be the aim of every physician who sees headache patients to try and devise for himself a flow chart or algorithm that will help rule out or confirm a serious underlying secondary cause and diagnose specifically the benign primary headache. One should know what to look for on examination and what test to order in which patient. It is always helpful to make the right diagnosis and treat specifically rather than use painkillers and tranquilizers while being unsure about the underlying cause. If you do not spend time on taking a proper history and just order a battery of tests, this is more like “fishing” for a diagnosis rather than proceeding in a targeted manner. You will only end up feeling safe that there is no serious underlying cause, but you will still not know how to treat the patient. After a standard set of questions, more specific questions can be generated depending on the patient's answers and your suspicions. And, finally, at the end, you need to ask three blanket questions in all headache patients.
“Is there anything that you wish to tell me which you think I have not asked you?”
“Why the consultation now?”
“What is your expectation from this consultation?”
The Standard Headache History
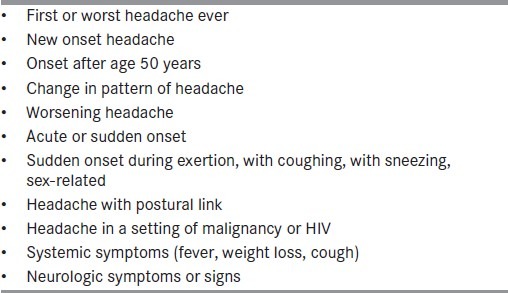
Routine history taking begins with a set of standard questions that will elicit basic information and, depending on the acuity of onset, the age of the patient and whether he/she presents to you in the office/consulting room or emergency department/casualty, you will need to elicit additional history. In every headache patient, our worry and the patients fear is that no serious life-threatening cause should be overlooked. It is therefore important to keep in mind the “red flags” and ask the right questions to be able to decide whether the patient could be having a serious secondary headache warranting further investigation. Any new onset headache or anything that is atypical for a particular type of primary headache should get you worried about the presence of a secondary headache and warrant imaging. “Red flags” that should caution you to be careful and investigate further are listed in Table 1.[5]
Table 1.
Headache “Red flags”[5]
The questions can flow in the following preset fashion:
Since how long have you been having headaches?
This will tell us about the onset and the duration of the headache. It is useful to divide this into two phases: (i) an immediate phase of increased frequency or severity for which the patient has now come for consultation and (ii) an earlier phase of lesser frequency or severity. This will help determine if this is definitely a NEW onset headache or something that has been there since before and has worsened now. You are sometimes surprised by patients who half-way through the history tell you, “Oh, I have always had these normal headaches since childhood!” This could mean an earlier mild migraine that has been there and that has now worsened. New onset headaches should always be taken seriously. The longer the time for which the headaches have been present, the greater the likelihood of the headache being a primary headache. If there is an acute onset, severe, first and worst headache, the common possibilities are sub-arachnoid hemorrhage, vascular dissection, cerebral venous thrombosis, reversible cerebral vasoconstriction syndrome, acute hypertensive crisis or a primary thunderclap headache. Rarely pituitary apoplexy, colloid cyst, sphenoid sinusitis or spontaneous intracranial hypotension may present with acute onset headache.
Where in the head does it pain and how does it radiate?
This will tell us about the location and the pattern of radiation. It could be unilateral to begin with and then become generalized, which is what would be seen with a migraine headache, or it could be holocranial, generalized as with tension-type headache or it could start periorbitally as with cluster headache. Migraine headaches are usually in the temporal region, over the vertex, in the occipital region and often radiate to the neck on the same side as the pain. They often alternate sides but can rarely remain side-locked. Side-locked headaches warrant investigation to rule out an underlying structural cause. Cluster headache is classically side-locked and is mostly periorbital to start with and may then spread to becoming hemicranial. Because of an overlapping nerve supply, periorbital headaches can have many causes.
Patients with headache who also complain of neck, shoulder or arm pain should be investigated to rule out cervicogenic headache, although 75% of migraine patients can have associated neck pain.[6] Due to an overlapping nerve supply and referral and convergence patterns, pain can also be referred to distant locations. Supratentorial structures are innervated by the ophthalmic division of the fifth cranial nerve and the posterior fossa structures are supplied by C2 and C3. Therefore, pain from the upper cervical spine or posterior fossa can be referred anteriorly to the front of the head.
Facial pain has many underlying causes, of which trigeminal neuralgia is the most common. When a patient presents with facial pain, you need to consider the neuralgias, facial pain syndromes involving the cranial nerves, the trigemino-autonomic cephalgias (TACs), rhinologic conditions, dental disorders, temporomandibular problems and idiopathic facial pain. In addition to the questions listed, it is very important to ask for cutaneous triggers for the facial pain as with trigeminal neuralgia
How often does the head pain?
This will tell you about the frequency and whether it is a monthly, weekly or daily headache. If it is a daily or near-daily headache, is it only once a day or more than once per day. Ask if it was less earlier and more frequent now, if the pain comes on at any particular time of the day, if it has a diurnal variation, if it is more at night than in the day, if it wakes up the patient from sleep or if it is present on awakening. Some headaches that are more likely to present with headache at night are hypnic headache syndrome, cluster headache, SUNCT syndrome or exploding head syndrome. With headache present on awakening in the morning, one has to suspect obstructive sleep apnea, poorly controlled hypertension, raised intracranial pressure or migraine. Ask for any fixed seasonal pattern, whether it comes on only during certain times of the year, with periods of spontaneous remission as with cluster headache, or whether there is a cyclic pattern as with cyclic migraine. A progressively worsening frequency or a headache that is unresponsive to treatment indicates a secondary cause.
How long does each attack last? Is it short-lasting or long-lasting?
It is important to ascertain if it is a short-lasting headache or long-lasting headache. An arbitrary duration of 4 hours is considered as the cut-off between short-lasting and long-lasting headache. The trigemino-autonomic cephalgias (TACs) such as cluster headache and chronic paroxysmal hemicrania (CPH) are examples of short-lasting headaches that usually last for under 4 hours. Primary stabbing headaches are very brief and can last from 10 secs to a minute. Likewise, trigeminal neuralgia attacks are lightening stabs of pain that are of also very brief duration, usually a few seconds, as are headaches due to the SUNCT syndrome, which is another example of a TAC. Migraine headaches on the other hand are of longer duration and last anywhere from 4 to 72 h.
How severe is the pain?
This will tell us about the severity. S everity of the pain can be subjectively gauged on the verbal rating scale from 0 to 10, where 0 refers to no pain and 10 is the worst pain. Cluster headache and moderate to severe migraine are usually described as a 9/10 or 10/10 severity pain as compared with tension-type headache, which is usually a 3–5/10 severity pain. It is necessary to emphasise here that severity of the head pain does not tell us whether we are dealing with a primary or secondary headache. The pain of migraine or cluster headache can be just as severe and disabling as that due to a sub-arachnoid hemorrhage.
What type of pain is it? What is the Nature of the pain?
Although not always a useful pointer, most headaches that are pulsatile or throbbing or hammering in nature are usually due to migraine. The other strikingly different short-lasting pains are the ice pick pains. Tension-type headache is a dull featureless pain with no accompaniments. Ask if the headache builds up gradually as with migraine or does it peak rapidly as with the TACs.
What factors can precipitate or worsen the headache. Are there any triggering or relieving factors?
This will tell you if there are any trigger factors – environmental, dietary, hormonal. Because a common disorder like migraine is influenced by so many trigger factors that vary across regions and cultures, it is essential to be aware of these when taking the history.
Ask if there is any link with the menstrual cycle which would suggest the possibility of migraine, a seasonal link suggestive of cluster headache or if movement or activity worsens the headache. Relieving factors are also important. If there is any increase or reduction with lying down, or postural worsening, it should suggest an alteration in cerebrospinal fluid dynamics.
Are there any accompaniments to the head pain?
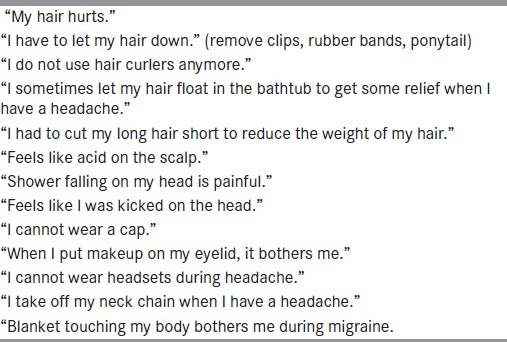
Vomiting can be a feature of migraine or an intracranial disorder, but hypersensitivity phenomena such as photophobia, phonophobia or osmophobia are often seen only with migraine. These can rarely be present with subarachnoid hemorrhage or meningitis. Autonomic features such as lacrimation or rhinorrhea are usually seen with the TACs. Ask if the eye becomes small (ptosis) or if the eye becomes red or swollen. These are features of Horner's syndrome and indicate the possibility of TACs. Pulsating, throbbing temporal vessels are seen with migraine. A tender painful superficial temporal artery can occur with giant cell arteritis. Syncope in a headache patient can be seen with migraine or more rarely with a colloid cyst of the third ventricle. When a nonpainful stimulus can induce pain over the scalp region, it is termed cutaneous allodynia and is seen in many migraine patients and some cluster headache patients. The manifestations of allodynia are listed in Table 2.
Table 2.
Cutaneous allodynia: The manifestations[13]
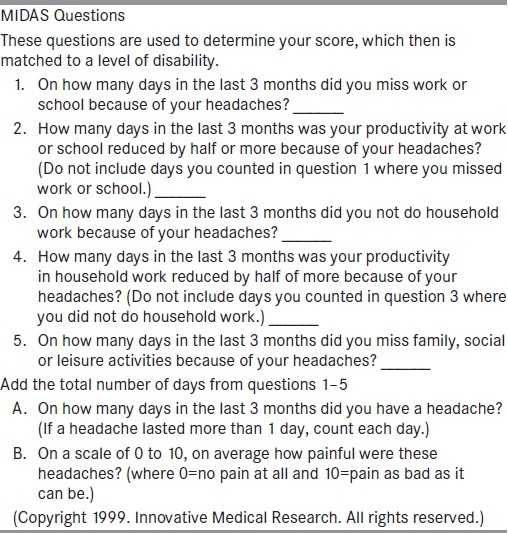
Ask for associated neurological complaints such as seizures, syncope, double vision, etc. Ask about behavior during the attack. Irritability and confusion with the headache should suggest migraine and restlessness or pacing up and down is more with cluster headache. Ask for disability or limitation of activities during the headache, which usually happens with migraine. The extent of disability can be gauged using instruments[7] such as MIDAS or HIT-6. The items on these Instruments of Disability Assessment are featured in Table 3.
Table 3.
MIDAS score[7]
Ask for any visual or sensory aura?
Ask for auras that may preceed or accompany the head pain of migraine. Visual auras are the most common. Auras occur in succession, and the same patient may have a visual aura, followed sequentially by sensory paresthesiae or speech difficulty. Conditions that can mimic a migraine aura include strokes, TIAs, seizure disorders, tumors, venous thrombosis, arteriovenous malformations and carotid dissections. The onset, progression and duration of the symptoms help to differentiate between a migraine aura and a TIA or a seizure. Difficulty in making a distinction between these entities occurs when the aura is not followed by a headache. A gradual onset and progression over a few minutes is characteristic of a migraine aura as compared with a sudden onset in a TIA or a seizure. The classical duration of a migraine aura is 20–30 minutes as compared with a significantly shorter duration for a seizure and a longer one for a TIA.
Ask if there is just one type or more than one type of headache?
This implies distinctive types of headache and not headache of different levels of severity. Migraine and cluster headache can coexist, cluster headache can be associated with trigeminal neuralgia (cluster–tic syndrome) or migraine patients may have acute sinusitis. Two types of headache can coexist and need to be treated separately. Therefore, it is important to recognize different headaches when they coexist. When there is more than one type of headache, it helps to have the details of each type of headache.
Ask if the headache is precipitated or significantly worsened by the Valsalva manouvre’? Ask if there is worsening with sexual intercourse? Ask if there is postural worsening?
Worsening with Valsalva manoeuvre or with coughing or laughing or sneezing suggests a need to rule out a posterior fossa or cranio-verteberal junctional anomaly such as a Chiari I malformation. If a secondary cause is ruled out, then one can diagnose a primary cough headache. When a headache worsens on exertion, one must keep in mind the possibility of cardiac cephalalgia, phaeochromocytoma, dissection or primary exertional headache. If a headache begins or worsens with sexual activity, suspect a sub-arachnoid hemorrhage or dissection or primary sexual headache. There are some headaches such as those due to spontaneous intracranial hypotension or postlumbar puncture that can worsen with change to the erect posture. Headaches due to raised intracranial pressure can worsen in the supine position. Ask for aggravation of the headache with physical activity as in migraine.
Ask about the personal history, habits and occupation?
Ask for details of personal habits that may worsen headaches. Consumption of alcohol can aggravate cluster headache during the active phase. Ask about excess caffeine consumption, such as with too much coffee or tea or caffeinated beverages. Ask about sleep pattern and sleep disturbances.
Ask for a family history of headaches?
Asking about a history of similar headaches in other family members may elicit “No” for an answer. Asking about “any” headache at all will tell you about the presence of headaches in other members of the family.
Ask about the impact of the headache on the patient's lifestyle?
This will tell you how disabling the headaches are and this will also help build a rapport. There are instruments such as MIDAS and HIT 6, but these will need monitoring of the headache using a headache diary.
Ask about medication overuse?
It is well established that overuse of/self-medication with analgesics containing caffeine and codeine, combination analgesics, ergotamine or triptans can result in chronic headache.[8] Always remember to ask about the specific acute headache medication consumed, the number of tablets and number of days for which they have taken it. Some medications taken for other conditions can have headache as a side-effect, for e.g. the combined oral contraceptive or phosphodiesterase inhibitors can worsen migraine headache. Coronary vasodilators can be associated with severe headaches. A careful drug history is important. Many cardiovascular dilatory drugs such as the nitrates, antiarrhythmics, some of the agents for erectile dysfunction can cause headache as a side-effect.
Ask about the interictal status?
This will tell you the interictal state of health. It is important to know if there is a background headache or if the headache comes in recurrent attacks that are trigger-linked.
Ask about investigations that have been done so far? And the treatment that has been taken so far?
While taking the history, one has to also plan for investigations based on the differential diagnosis and the tests that have already been done. If a patient tells you that he has had a recent scan done that is normal, it will reassure you and also tell you that you are dealing with a primary headache. Asking about the previous treatments will tell you about failed treatments and will help you plan the further line of treatment.
Ask if there is anything else that the patient wants to tell you? Ask if there are any other complaints or medical problems?
This query will bring out other medical illness that may be related or unrelated, for e.g. asthma, polycystic ovarian syndrome, hypothyroidism, hyperprolactinemia, previous head or neck trauma, drug allergies, history of hypertension and history of medications for other conditions. Some headache medications may be contraindicated with other medical conditions, e.g. betablockers in bronchial asthma. Ask for history of fever and weight loss, which should indicate a systemic infection or malignancy. A history of galactorrhea in a headache patient will warrant ruling out of a hyperprolactinemia secondary to a pituitary adenoma. Malarial fevers or viral fevers can sometimes be followed by intense headache. Ask the right questions to rule out immunocompromised states like HIV that can lead to opportunistic infections. Rarely, neurosarcoidosis or Lyme disease can present with headache. Ask to check if there is an occupational history that can aggravate headaches.
Specific settings needing additional history
Beyond the standard history, headache history-taking should NOT follow the same set pattern in all patients. You need to adapt and modify based on the setting and the suspected diagnosis. If the patient presents to the Emergency Department with a sudden onset headache, you may need to take a quick history and you may sometimes need to order tests. You may sometimes need to start treatment even before you diagnose. History taking in an emergency department is therefore different from history taking in an office setting; history in a child with headache will differ from the elderly patient beyond 50 years who presents with headache, where different causes will need to be suspected.
It will be beyond the scope of this review to discuss each condition that can present with headache, but the conditions to be considered in different settings are grouped in a tabular form, and this should help you ask the right questions in the right setting.
Thunderclap headache
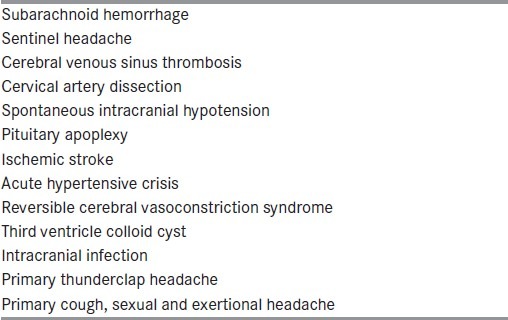
Thunderclap headache (TCH) refers to a sudden, severe headache that attains peak intensity at onset itself. TCH is defined in ICHD-21 as a severe headache reaching maximal intensity within seconds to a minute. The rapidity of onset and the severity are the characteristic features of TCH. The conditions that can present with TCH range from benign to life-threatening, and are listed in Table 4.[9]
Table 4.
Causes of thunderclap headache[9]
Chronic daily headache
Chronic daily headache or CDH is the umbrella term used to describe patients who present with headache on more than 15 days/month for more than 3 months. CDH is divided into two groups: Primary and secondary CDH. Secondary causes of CDH should always be ruled out before diagnosing primary CDH. The causes of CDH have been listed in Table 5.
Table 5.
Chronic daily headache (CDH): The causes[9]
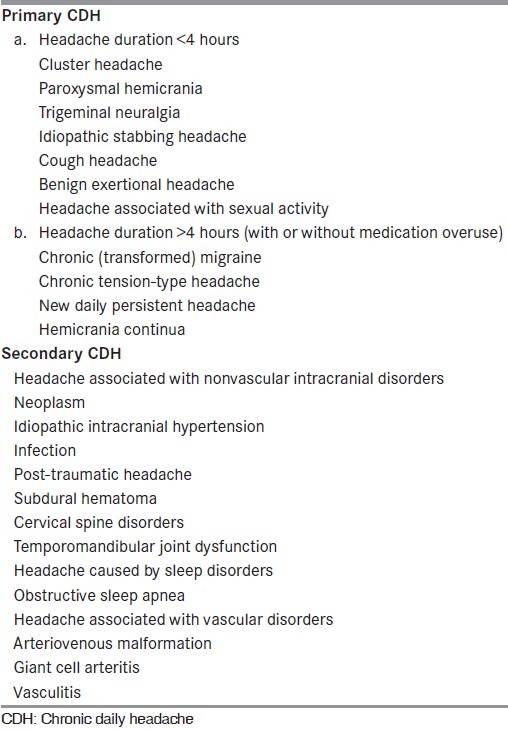
The number of headache days, the duration of the headache, the number of days on which the headache fulfills the criteria for migraine, the response to ergots or triptans and the presence of medication overuse have all to be enquired about in order to make the diagnosis of chronic migraine.[10]
New onset headache
When there has been no history of headaches in the past and the headache occurs on a daily basis for more than 3 months, it would be labeled as NDPH[11] or New Daily Persistent Headache, but only after making sure that other secondary conditions have been ruled out. The causes that need to be ruled out before diagnosing NDPH will be covered in a separate article.
Indomethacin responsive headaches
Because there are some conditions that respond exquisitely to Indometacin, you need to be able to suspect and identify these headaches. CPH and Hemicrania Continua are exquisitely responsive to Indomethacin. Some of the other conditions that are responsive to Indomethacin are Valsalva-induced headaches, primary cough headache and primary stabbing headache.
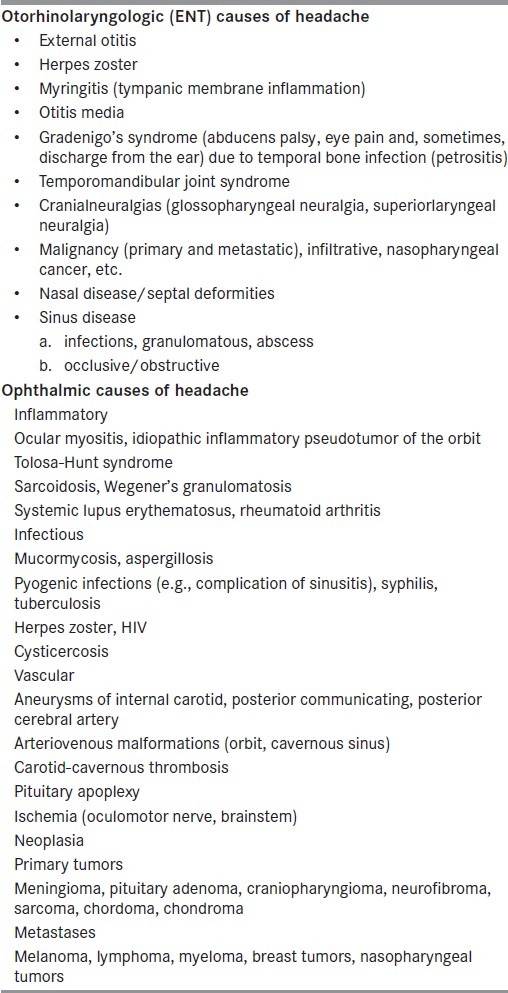
Headaches originating in overlap specialities
There are many causes of headaches in areas with overlapping nerve supply and which are often in the realm of overlapping specialties such as Oto-rhinolaryngology and Ophthalmology. These headaches need to be referred to the right specialists. When you suspect a sinus infection, ask for history of purulent discharge, fever and tenderness over the sinuses. Ophthalmic conditions can be present with headache. Subacute angle closure glaucoma is often deceptive and one has to suspect the entity in the right setting and be alert on examination and refer appropriately. Some important Otorhinolaryngologic and Ophthalmic causes of headache are listed in Table 6.
Table 6.
Otorhinolaryngologic and ophthalmic causes of headache[14]
Headache in children
There are some headache conditions such as abdominal migraine and cyclic vomiting syndrome that are seen more often in children. Always ask for history of recurrent abdominal pain and recurrent intractable attacks of severe vomiting. Migraine headaches in children are of shorter duration, bifrontal in location, may not have all the accompaniments as seen in adults and are characteristically relieved by sleep. Ask about food habits in children – excessive chocolates, cheese, caffeinated drinks and monosodium glutamate containing fast food items are well known to worsen headaches. Even very young children can present with migraine.
Headaches in the elderly
There are also some conditions seen that you need to suspect in the elderly and ask the right questions. Comorbid conditions and medication for other illnesses can cause headaches in the elderly. Secondary headache disorders such as giant cell arteritis, neoplasms, metabolic abnormalities and glaucoma are some conditions to be considered in the elderly.
Specific entities needing additional history
ICHD2 (2004) has specific criteria that need to be fulfilled for the different headache conditions. It is worthwhile remembering the criteria for the common primary headache conditions that one comes across in practice, viz. migraine, cluster headache and tension-type headache. These common conditions and the additional questions that one must ask are discussed below.
Migraine
The diagnosis of migraine needs recognition of the pattern of recurrent trigger-linked episodes of headache with accompaniments such as nausea, vomiting, photophobia and phonophobia. Migraine attacks usually follow a sequence of a prodrome, aura, headache and postdrome. Ask the right questions to establish the sequence or to make a phasic diagnosis of migraine. The premonitory symptoms of difficulty in concentration, feeling low and tired, neck pain, yawning, food cravings and other hypothalamic disturbances can sometimes give a clue to the diagnosis of migraine. You therefore have to ask questions to elicit and establish these characteristic features. There may or may not be a visual or sensory aura. When you suspect migraine with aura, you have to ask additional questions about the aura – the type of aura, the duration, the sequence. If an aura is present, you have to always differentiate between a seizure disorder and a transient ischemic episode. A useful question to ask in order not to miss migraine with aura would be, “Do you have a visual defect or any other neurological problem before or along with the headache? Ask about the prodrome after the headache. Ask if the patient feels tired or drained or fatigued.
There are many features in migraine patients that are not covered by the IHS criteria.[12] Migraine headache is not always unilateral, not always throbbing and can present without nausea, vomiting, photophobia or phonophobia when it is called “Probable Migraine”. You should therefore not be surprised to see migraine presenting in an atypical incomplete manner that is not always described in textbooks.
In women, migraine more often starts at menarche, can worsen around the periods, in pregnancy, with contraceptive use, with use of hormones to treat infertility or polycystic ovarian disease and around menopause with hormone replacement therapy. Migraine decreases during the second and third trimester of pregnancy. There may be a positive family history. Migraine can less commonly present with onset at a later age when you have to make sure that you are not dealing with a late-life migraine accompaniment or a secondary headache.
TACs
Always ask about accompanying autonomic signs and symptoms in headache patients. Head pain associated with lacrimation, nasal stuffiness, conjunctival injection, facial swelling or Horner's syndrome on the same side as the head pain should alert you to the possibility of cluster headache or one of the TACs. The duration of the attacks in TACs is shorter than in migraine, they are more frequent, you can get more than one attack per day and they are generally side-locked. The TACs will be discussed in detail in another article. In all patients with migraine or cluster headache, ask for overlapping features. Cluster headache patients can present with aura, photophobia, phonophobia, nausea or vomiting and migraine patients can have associated autonomic features. With intractable TACs, ask to rule out obstructive sleep apnea and look for atypical patterns that should raise suspicions of an underlying secondary cause.
Tension-type headache
Tension-type headaches are “featureless headaches” without accompaniments and are not so common in headache patients who decide to consult. They are more common in the general population than in patients seen in the clinic.
Conclusion
Unlike in other areas of medicine where investigative techniques have overtaken the need for detailed history-taking, in the headache field, one still has to perfect the art of history-taking in order to arrive at the right diagnosis. The process of history-taking is time consuming, but it is an art that needs to be perfected by practice. History-taking is all about entertaining the RIGHT suspicions, asking the RIGHT questions in the RIGHT sequence to arrive at the RIGHT diagnosis and initiate the RIGHT treatment within the RIGHT time-frame.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
References
- 1.Headache classification committee, International Headache Society. Classification and diagnostic criteria for headache disorders, cranial neuralgias, and facial pain. Cephalalgia. 2004;24(Suppl 1):1–160. [PubMed] [Google Scholar]
- 2.Rasmussen BK, Jensen R, Schroll M, Olesen J. Epidemiology of headache in a general population – a prevalence study. J Clin Epidemiol. 1991;44:1147–57. doi: 10.1016/0895-4356(91)90147-2. [DOI] [PubMed] [Google Scholar]
- 3.Blau JN, MacGregor EA. Migraine consultations: A triangle of viewpoints. Headache. 1995;35:104–6. doi: 10.1111/j.1526-4610.1995.hed3502104.x. [DOI] [PubMed] [Google Scholar]
- 4.Osler W. Osler's “A Way of Life” and Other Addresses, with Commentary and Annotations. Durham and London: Duke University Press; 2001. [Google Scholar]
- 5.Evans RW. Diagnostic testing for headache. Med Clin North Am. 2001;85:865. doi: 10.1016/s0025-7125(05)70348-5. [DOI] [PubMed] [Google Scholar]
- 6.Kaniecki RG. Migraine and tension-type headache: An assessment of challenges in diagnosis. Neurology. 2002;58(9 Suppl 6):S15–20. doi: 10.1212/wnl.58.9_suppl_6.s15. [DOI] [PubMed] [Google Scholar]
- 7.Bigal ME, Rapoport AM, Lipton RB, Tepper SJ, Sheftell FD. Assessment of migraine disability using the migraine disability assessment (MIDAS) questionnaire: A comparison of chronic migraine with episodic migraine. Headache. 2003;43:336–42. doi: 10.1046/j.1526-4610.2003.03068.x. [DOI] [PubMed] [Google Scholar]
- 8.Mathew NT, Reuveni U, Perez F. Transformed or evolutive migraine. Headache. 1987;27:102–6. doi: 10.1111/j.1526-4610.1987.hed2702102.x. [DOI] [PubMed] [Google Scholar]
- 9.Schwedt TJ, Matharu M, Dodick DW. Thunderclap Headache. Lancet Neurol. 2006;5:621–31. doi: 10.1016/S1474-4422(06)70497-5. [DOI] [PubMed] [Google Scholar]
- 10.Silberstein SD, Lipton RB, Goadsby PJ. Headache in clinical practice. 2d ed. London: Martin Dunitz; 2002. Chronic Daily Headache diagnosis and treatment; p. 129. [Google Scholar]
- 11.Li D, Rozen TD. The clinical characteristics of new daily persistent headache. Cephalalgia. 2002;22:66–9. doi: 10.1046/j.1468-2982.2002.00326.x. [DOI] [PubMed] [Google Scholar]
- 12.Ravishankar K. Optimising primary headache management. J Assoc Physicians India. 2006;54:928–34. [PubMed] [Google Scholar]
- 13.Mathew NT, Kailasam J, Seifert T. Clinical recognition of allodynia in migraine. Neurology. 2004;63:848–52. doi: 10.1212/01.wnl.0000137107.27585.f7. [DOI] [PubMed] [Google Scholar]
- 14.Evans RW, Mathew NT. Handbook of Headache. 2d ed. Philadelphia: Lippincott-Williams and Wilkins; 2005. p. 3. [Google Scholar]


