Abstract
Objective
To analyse the impact of Janani Suraksha Yojana (JSY) on Maternal Mortality Ratio (MMR).
Design
Retrospective analysis of maternal mortality.
Methods
Analysis of all maternal deaths between January 2001 and December 2009.
Results and Discussion
The total number of deliveries has been steadily rising from 1,685 in 2001 to 3,957 in 2009. The MMR doubled from 1,500/100,000 live births in 2001 to 3,000/100,000 live births in 2006, then declined to 2,464/100,000 live births in 2009. Implementation of the various maternity benefit schemes has had no significant impact on the profile of dying mothers—admission-to-death interval. Deaths due to anemia and eclampsia have significantly increased (P < 0.05), whereas due to sepsis (P < 0.001) and hemorrhage (P < 0.05), deaths have significantly decreased. Almost 96 % of dying subjects received inadequate antenatal care. However, significantly less number (P < 0.001) of women are delivering at home.
Conclusions
There is a need to stress the importance of good antenatal care in reducing MMR.
Keywords: Maternal mortality, Maternal mortality ratio, Anemia, Eclampsia, Sepsis
Background
Woman plays a pivotal role in the family, and pregnancy care should culminate in healthy mother with a healthy baby. Maternal mortality ratio is a vital index of the effectiveness of prevailing obstetric services and socioeconomic affluence of a country [1, 2]. Various social, cultural and political factors determine the statuses of women, their health, fertility and health-seeking behaviour [2]. The maternal mortality ratio (MMR) of India is 407 and that of the state of Madhya Pradesh (MP) is 498 per 100,000 live births (2007–2008). ‘Institutional mortality rates’ are 2–10 times higher as compared with field surveys because most of the seriously ill patients are referred to the nearest tertiary care centres [2]. The government has launched various incentive-based schemes to promote institutional deliveries and reduce MMR. We undertook this study to evaluate the impact of these schemes on the quality of antenatal care and MMR in our hospital.
Material and Methods
Place of Study
Retrospective analysis of all maternal deaths occurring in the Department of Obstetrics and Gynaecology of Government NSCB Medical College from January 2001 to December 2009 was done. In April, 2005, the Government launched various schemes with the aim to promote institutional deliveries, e.g. Prasuti Parivahan Yojana (financial aid to cover cost of transporting a pregnant woman to the Hospital) and Janani Suraksha Yojana/JSY (financial incentive to all women delivering in Government hospitals and the community workers responsible for her antenatal care). These schemes were extended to the private hospitals upon fulfilment of certain criteria in late 2007.
This study was carried out with the purpose of analysing the impact of these schemes on quality of ante natal care and maternal mortality. Data were analysed in two phases—the first, before the implementation of the JSY, i.e. between 1.1.2001 and 31.12.2005 and the second phase after its complete implementation, i.e. from 1.1.2006 to 31.12.2009. Each record was scrutinized for age, parity, place of delivery, cause of death, admission-to-death interval, etc. The two groups were compared to find out any changing trends of maternal mortality and to evaluate the impact of the schemes on MMR. Maternal death was defined and classified according to the World Health Organisation’s International Classification of Diseases, 10th revision (ICD-10). Deaths were classified as direct, indirect or fortuitous. The MMR is defined as the number of direct and indirect maternal deaths per 100,000 live births up to 42 days after the termination of pregnancy.
Statistical Analysis
Data were analysed using SPSS 11.5 program. Appropriate statistical analysis using t test, χ2 test and Fishers exact test was applied, and the critical level of significance was considered at 0.05 level.
Observations
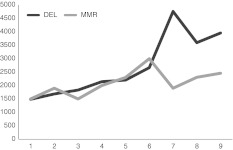
The total number of deliveries has been steadily rising from 1,685 in 2001 to 3,957 in 2009. The maternal mortality ratio has also simultaneously increased reaching a peak of 3,000/100,000 live births in 2006 (Fig. 1). The total number of deliveries in the first phase is 9,348 and that in second phase is 11,724 (P < 0.05). The MMR which is 1,951/100,000 live births in phase 1 is significantly less than 2363.6/100,000 live births in phase 2 (P < 0.0001)!
Fig. 1.
Total deliveries and MMR in
Of the 172 maternal deaths in the first phase, 20.34 % (35) were ≤20 years and 68.02 % were between 21 and 30 years, 44.76 % were P0-1, 78.48 % were from rural areas and 96.51 % received no or inadequate antenatal care either in terms of the quality of care or the number of visits (Table 1). Majority of the subjects, i.e. 63 % died within 24 h of admission to the hospital (Table 2). Amongst the direct causes (62.7 %), eclampsia and pre-eclampsia together accounted for 31.4 % of the deaths, while obstetric hemorrhage stood second at 14.5 %. Amongst the indirect killers (37.2 %), anemia topped at 42.3 % (Table 3). 38 % were admitted antenatal and 36.7 % in labour, 28.5 % died undelivered, and 58.7 % died in the postnatal period; 26.7 % delivered at home, while only 10.9 % delivered at a Community Health Centre (CHC)/Primary Health Centre (PHC)/District Hospital or a private nursing home (Table 4).
Table 1.
Demographical profile of dead subjects
| Profile | Group 1 2001–2005 (n = 172) | (%) | Group 2 2006–2009 (n = 341) | (%) |
|---|---|---|---|---|
| Age in years | ||||
| <20 years | 35 | 20.34 | 48 | 14.1 |
| 21–30 years | 117 | 68.02 | 260 | 76.2 |
| >30 years | 20 | 11.62 | 33 | 9.7 |
| Mean | 24.63 ± 5.60 | 25.12 ± 5.89 | ||
| P > 0.05 | ||||
| Parity | ||||
| P0–P1 | 77 | 44.76 | 169 | 49.6 |
| P2–P3 | 60 | 34.88 | 98 | 78.8 |
| ≥P4 | 35 | 20.34 | 74 | 21.7 |
| χ2 = 2.04; P > 0.05 | At 2 df | |||
| Residence | ||||
| Rural | 135 | 78.48 | 267 | 78.3 |
| Urban | 37 | 21.51 | 74 | 21.7 |
| χ2 = 0.002; P > 0.05 | At 1 df | |||
| Antenatal care | ||||
| Yes | 6 | 3.48 | 15 | 4.44 |
| No | 166 | 96.51 | 326 | 95.6 |
| χ2 = 0.2414; P > 0.05 | At 1 df | |||
Table 2.
Admission-to-death interval
| Group 1 number (n = 172) | (%) | Group 2 number (n = 341) | (%) | |
|---|---|---|---|---|
| <24 h | 108 | 63 | 205 | 60.1 |
| 24–72 h | 49 | 28 | 89 | 26.1 |
| >72 h | 15 | 08 | 47 | 13.8 |
χ2 = 2.8; P > 0.05 at 2df
Table 3.
Cause of death
| Group 1 | (%) | Group 2 | (%) | t Value | P value | |
|---|---|---|---|---|---|---|
| Direct causes | ||||||
| Eclampsia | 44 | 25.6 | 117 | 34.3 | 2.076 | P < 0.05 |
| Pre-eclampsia | 10 | 5.8 | 24 | 7.0 | 0.542 | P > 0.05 |
| Sepsis | 20 | 11.6 | 9 | 2.6 | 3.465 | P < 0.001 |
| Obstructed labour | 4 | 2.3 | 12 | 3.5 | 0.784 | P > 0.05 |
| Hemorrhage | 25 | 14.5 | 24 | 7.0 | 2.48 | P < 0.05 |
| Embolism | 5 | 2.9 | 7 | 2.1 | 0.572 | P > 0.05 |
| Total | 108 | 193 | ||||
| Indirect causes | ||||||
| Severe anemia | 34 | 19.8 | 98 | 28.74 | 2.299 | P < 0.05 |
| Hepatitis | 10 | 5.8 | 24 | 7.038 | 0.542 | P > 0.05 |
| Heart disease | 3 | 1.7 | 4 | 1.173 | 0.494 | P > 0.05 |
| Malaria | 4 | 2.3 | 11 | 3.226 | 0.602 | P > 0.05 |
| BT reaction | 0 | 0.0 | 1 | 0.293 | 1.001 | P > 0.05 |
| Unrelated | 13 | 7.6 | 10 | 2.9 | 2.09 | P < 0.05 |
| Total | 64 | 148 | ||||
Table 4.
Status at admission, death and place of delivery
| Status at admission | Group 1 number (n = 150) | (%) | Group 2 number (n = 318) | (%) | t Value | P value |
|---|---|---|---|---|---|---|
| Antenatal (>28 weeks pregnancy) | 57 | 38 | 142 | 44.7 | 1.373 | >0.05 |
| Intranatal | 55 | 36.7 | 111 | 34.9 | 0.37 | >0.05 |
| Postnatal | 38 | 29.3 | 65 | 20.4 | 1.162 | >0.05 |
| Status at death | Number (n = 172) | (%) | Number (n = 341) | (%) | ||
|---|---|---|---|---|---|---|
| Abortion + ectopic | 12 + 10 | 6.9 + 5.9 | 12 + 11 | 3.5 + 3.2 | 2.09 | <0.05 |
| Antenatal | 18 | 10.5 | 49 | 14.4 | 1.29 | >0.05 |
| Intranatal | 31 | 18 | 67 | 19.6 | 0.44 | >0.05 |
| Postnatal | 101 | 58.7 | 202 | 59.2 | 0.112 | >0.05 |
| Place of delivery | Number (n = 101) | (%) | Number (n = 202) | (%) | ||
|---|---|---|---|---|---|---|
| NSCB | 63 | 62.4 | 139 | 68.8 | 1.106 | >0.05 |
| District hospital | 1 | 1 | 16 | 7.9 | 3.238 | <0.05 |
| CHC/PHC | 2 | 2 | 18 | 8.9 | 2.84 | <0.05 |
| Private hospital | 8 | 7.9 | 10 | 5 | 0.9 | >0.05 |
| Home | 27 | 26.7 | 19 | 9.4 | 3.56 | <0.001 |
Of the 341 maternal deaths in the second phase, 14.1 % were ≤20 years and 76.2 % were between 21 and 30 years; 49.6 were P0-1; 78.3 % were from rural areas and 95.6 % received no or inadequate antenatal care (Table 1). 60.1 % of the subjects died within 24 h of admission to the hospital (Table 2). Amongst the direct causes (56.5 %), eclampsia and pre-eclampsia together accounted for 41.3 % of the deaths while obstetric hemorrhage was second at 7 %. Amongst the indirect killers (43.4 %), anemia continued at the top at 28.74 %. 44.7 % were admitted antenatally and 34.9 % in labor, 34.0 % died undelivered and 59.2 % died in the postnatal period (Table 3); 9.4 % of the subjects in phase 2 as against 26.7 % of the subjects in phase 1 had home deliveries (t = 3.56; P < 0.001) while 21.8 % as against 3.0 % delivered at a CHC, PHC or a District Hospital (P < 0.001) (Table 4).
Discussions
NSCB Medical College and Hospital is situated on the outskirts of Jabalpur city and as such was not a choice site for confinement for the urban populace until recently, with the city expanding and numerous settlements coming up in the vicinity. A major part of the captive population is tribal and no proper health care or transportation is available in these remote areas. Being a predominantly referral hospital, most of the women coming in have risk factors and many are in a moribund state. As such, the hospital based MMR has always remained high. Unfortunately, JSY has put an undue stress on institutional deliveries without making as earnest an effort to promote the importance of good antenatal care in reducing maternal morbidity and mortality. While the total number of institutional deliveries has steadily increased (Fig. 1), simply those women who were dying at home are being brought in a moribund state to die in hospitals with the MMR also simultaneously aiming skyward. This seems to be specifically true in 2006 (MMR—3,000/100,0000) when the family of a woman dying during delivery in a hospital received an insurance amount of INR 50,000 under the Vijay Raje Scindia Prasuti (pregnancy) Bima (insurance) Yojana (plan). This scheme has since been withdrawn.
Table 1 shows that the age, parity and residence profiles of the two phases are similar (P > 0.05) implying that our poor village girls are still married early and die young, maternity remaining a preventable cause of these tragic deaths. Kulkarni Sunanda and Huligol [2], Sharma [3] and the ICMR Task Force Study of 1993–1994 reported an almost similar demographic profile [4]. While 96.51 and 95.6 % (χ2 = 0.2414; P > 0.05) of the subjects dying in the first and second phases received no or inadequate antenatal care (ANC), 90.6 % in Kulkarni Sunanda and Huligol [2] study and 88 % in Sharma [3] (2001) study were unbooked. A similar study in our institute between 1985 and 2000 found that 84–85 % of deaths were amongst unbooked mothers [5]. This does not imply that fewer pregnant women are receiving ANC, but that, those women who comply with their prescribed plan of ante natal care are rescued from the tragedy of death. Poverty, illiteracy, casual acceptance of child bearing together with a shortage of trained and more importantly, dedicated health professionals remain a major hurdle in providing good antenatal care [4].
63 and 60.1 % (χ2 = 2.8; P > 0.05), respectively, of the subjects gave up their battle with life within 24 h of hospital admission. Other studies have reported an incidence ranging from 54 to 70 % [1–3, 6, 7]. The subjects or more truly, their families, compounded by poor transportation, bring them late to the hospitals, and very little time in positive intervention is available. Eclampsia, which if not absolutely preventable is well treatable, has led to significantly more deaths in Phase 2 (P < 0.05) [1–11]. Anemia which is an absolutely preventable cause of death continues to be the most important indirect cause of maternal death (P < 0.05) (Table 3) revealing the dismal nature of primary prevention from childhood through adolescence into pregnancy, although claims to the contrary are far too many. Availability of better antibiotics on demand (below poverty line card holders are provided free medicines by the Government under different schemes) has resulted in lesser number of subjects dying of infection in phase 2 (t = 3.465, P < 0.001). Similarly, good blood banking and transfusion services, have shown a positive impact in reducing mortality due to obstetric hemorrhage (Table 3) (t = 2.48, P < 0.05). For the above reasons as well as due to better diagnostic modalities, death from ectopic pregnancy (3.2 %) and abortions (3.5 %) has also significantly decreased (P < 0.05) (Table 4). This is due to increasing awareness about contraception, legal abortion services and better methods and drugs for abortion and prophylactic antibiotic use. Sharma [3] ICMR Task Force Study [4] Jayaram [6] and Patel et al. [7] reported abortion to be responsible for 25.9, 12.5, 6.7 and 5.17 % deaths, respectively, in their studies.
Although more pregnant women are accessing the health services, lack of adequately trained and motivated personnel at these sites probably resulted in the unfortunate women being picked up and referred late to a tertiary centre. For each pregnant woman who dies, there remain a countless number of those who suffer from short- or long-term morbidities, with most of them remaining unreported. Preventive obstetrics has taken a backseat to the telescopic goal of institutional deliveries providing financial gains for the patients’ family and health care providers irrespective of the outcome of pregnancy.
Conclusions
The schemes need to be remodelled so that the incentives may be phased out to cover antenatal care as well. There is also a need to make these incentives limited by the number of living issues, for in practice, they promote multiparity and associated risks. Death reviews attended by all personnel (health and administrative; public and private) [11] involved in the care of pregnant women should be held, and accountability discussed and fixed (presently, there is no such system in place). Despite Government efforts, MMR in India is unacceptably high. A holistic approach including literacy, nutrition and social and economic empowerment alone can relieve the burden of MMR from the National Health Statistics of India.
References
- 1.Shankar J, Seetharam S. Maternal mortality: 10 years review a decade of safe motherhood. J Obstet Gynecol India. 2001;51:108–110. [Google Scholar]
- 2.Kulkarni Sunanda R, Huligol A. Maternal mortality: 10 years study. J Obstet Gynecol India. 2001;51:73–76. doi: 10.1159/000052897. [DOI] [Google Scholar]
- 3.Sharma N. Maternal mortality: a retrospective study of 10 years. J Obstet Gynecol India. 2001;51:60–62. doi: 10.1159/000052893. [DOI] [Google Scholar]
- 4.Bedi N, Kambo I, Dhillon BS, et al. Maternal deaths in India—preventable tragedies (An ICMR Task Force Study) J Obstet Gynecol India. 2001;51:86–92. [Google Scholar]
- 5.Khare S, Singh KN, Kalkur S. Maternal mortality in Jabalpur Medical College (A 15 years study) J Obstet Gynecol India. 2002;52:51–52. [Google Scholar]
- 6.Jayaram Kamala V. Review of maternal mortality. J Obstet Gynecol India. 2001;51:80–82. [Google Scholar]
- 7.Patel DA, Gangopadhyay S, Vaishnav SB, et al. Maternal mortality at Karamsad—the only Rural Medical College in Gujarat (January 1994 to December 1997) J Obstet Gynecol India. 2001;51:63–66. [Google Scholar]
- 8.Bhattacharjee S. A study on maternal mortality in Silchar Medical College & Hospital. J Obstet Gynecol India. 2001;51:67–70. [Google Scholar]
- 9.Verma A, Minhas S, Sood A. A study on maternal mortality. J Obstet Gynecol India. 2008;58:226–229. [Google Scholar]
- 10.Sahu L, Rani R, Soundararaghavan S. Changing trends in maternal mortality (MMR is a good healthcare index) Int J Gynaecol Obstet India. 2008;11:24–29. [Google Scholar]
- 11.Veille J-C. Maternal mortality. Prog Obstet Gynaecol. 2008;18:125–142. [Google Scholar]