Abstract
Diagnosis of traumatic diaphragmatic hernia due to blunt abdominal trauma requires a high index of suspicion. This study was conducted to assess the accuracy of multidetector computed tomogram (MDCT) in the diagnosis of traumatic diaphragmatic hernia. All patients with thoracoabdominal blunt trauma with diaphragmatic hernia diagnosed on radiologic evaluation during a 3-year period (i.e., from June 2004 to June 2007) were analyzed. Nineteen patients with diaphragmatic injuries in 117 patients with blunt thoracoabdominal injury (16.23%) were studied. Age range was 8–60 years (mean 34 years). Male–female ratio was 18:1. Various features seen on CT scan were diaphragmatic discontinuity in 13 (68.42%), thickened diaphragm in 10 (52.63%), “collar sign” in 8 (42.10%), visceral herniation in 12 (63.15%), dependent viscera sign in 8 (42.10%), and segmental nonrecognition of the diaphragm in 1 patient (5.88%). Two patients presented with delayed rupture. In the rest mean duration between time of injury and performance of CT scan was 44.35 h (range 3–288 h). Fourteen patients underwent operative management. Sensitivity, specificity, and accuracy of MDCT scan were 100, 93, and 95%, respectively. Three patients (15.78%) expired. MDCT is a highly accurate modality for detecting traumatic diaphragmatic hernia.
Keywords: Diaphragm, Injury, Blunt, Trauma, Computed tomography
Introduction
Diaphragmatic injuries remain a diagnostic challenge for both radiologists and surgeons. The detection of traumatic diaphragmatic rupture in the acute setting is problematic because specific clinical signs are usually not evident [1]. Furthermore, the high frequency of associated injuries (52–100%) may distract from diaphragmatic injury [2, 3].
In conservatively managed patients, the rate of initially missed diaphragmatic injuries ranges from 12 to 66%, and they may even be overlooked at laparotomy [4, 5]. Diagnosis of a diaphragmatic injury requires a high index of suspicion, as delayed diagnosis increases the chance of visceral herniation and strangulation, which has mortality as high as 60% [6]. Thus, the ability to detect diaphragmatic injuries with noninvasive techniques is increasingly important [7].
Initial reports found CT to have sensitivity equal to that of chest radiography (i.e., 0–50%) [1, 8]. Because of a dramatic reduction in motion and beam-hardening artifacts and significant improvement of spatial resolution, especially along the z-axis, helical CT and multisection CT allow better demonstration of most subtle signs of diaphragmatic herniation. In addition, these are also useful tools in the evaluation of patients with multiple traumatic injuries [7].
Material and Methods
All patients with thoracoabdominal blunt trauma with diaphragmatic hernia diagnosed on multidetector computed tomogram (MDCT) during a period of 3 years from June 2004 to June 2007 were analyzed. We assessed variables such as age, gender, mechanism of trauma, methods of diagnosis, herniated organs and associated lesions, time of evolution, morbidity, and mortality. Anteroposterior supine chest radiograph, which was performed in all patients, was also analyzed. Computed tomogram (CT) was performed on four-slice MDCT after an IV bolus of iodinated contrast agents. A slice thickness of 4 mm at a pitch of 1.5 was useful to evaluate thorax and abdomen with reconstruction at 1 mm reconstruction increment. An oral contrast agent was given whenever required. Multiplanar reconstruction was done in sagittal and coronal planes. Images were read in lung parenchyma, soft tissues, and bone windows. Findings were analyzed in a prospective manner to evaluate their use as a diagnostic modality as well as to determine their contribution to patient management.
Observations
Nineteen patients with diaphragmatic injuries were detected in 117 patients with thoracoabdominal injury (16.23%). Their age ranged from 8 to 60 years (mean 34 years). There were 18 male and 1 female patients. Fourteen patients (70.59%) were involved in road traffic accidents, while the rest were due to blunt trauma of various other causes. Eleven patients had involvement on the left side (Figs. 1 and 2), while eight had involvement on the right side (Figs. 3 and 4). Out of 19 patients, 10 were detected on chest radiographs (52.63%) and all 10 of them were on the left side (Fig. 1a). Sensitivity, specificity, and accuracy of diaphragmatic injury by chest radiographs were 52.63, 100, and 92.3%, respectively. Various radiographic features seen are detailed in Table 1.
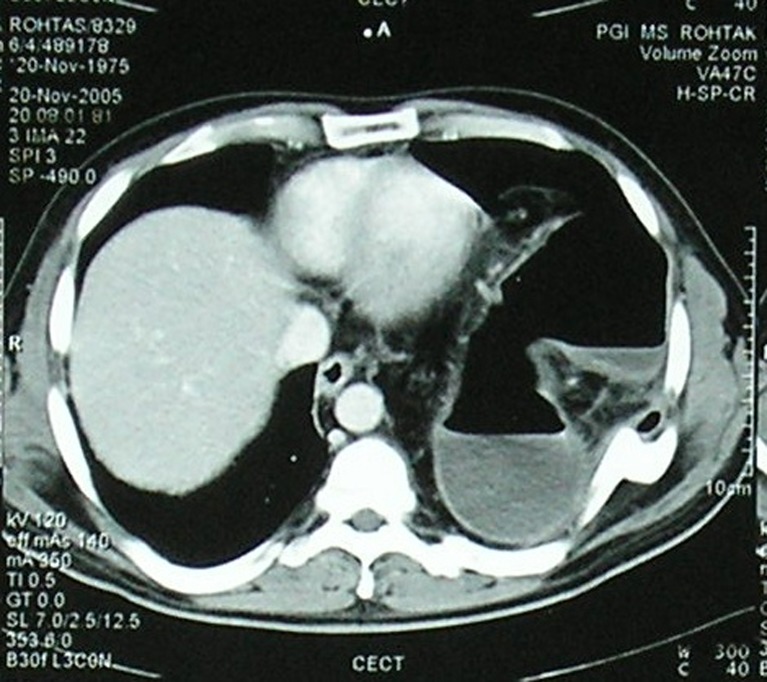
Fig. 1.
a Chest radiograph of an 8-year-old boy showing the air-fluid level in the left hemithorax. It was misdiagnosed as hydropneumothorax and a chest tube was inserted. b Reformatted coronal CT image of the same patient showing the left-sided hydropneumothorax and a well-defined thick-walled cystic structure. This proved to be diaphragmatic hernia at surgery
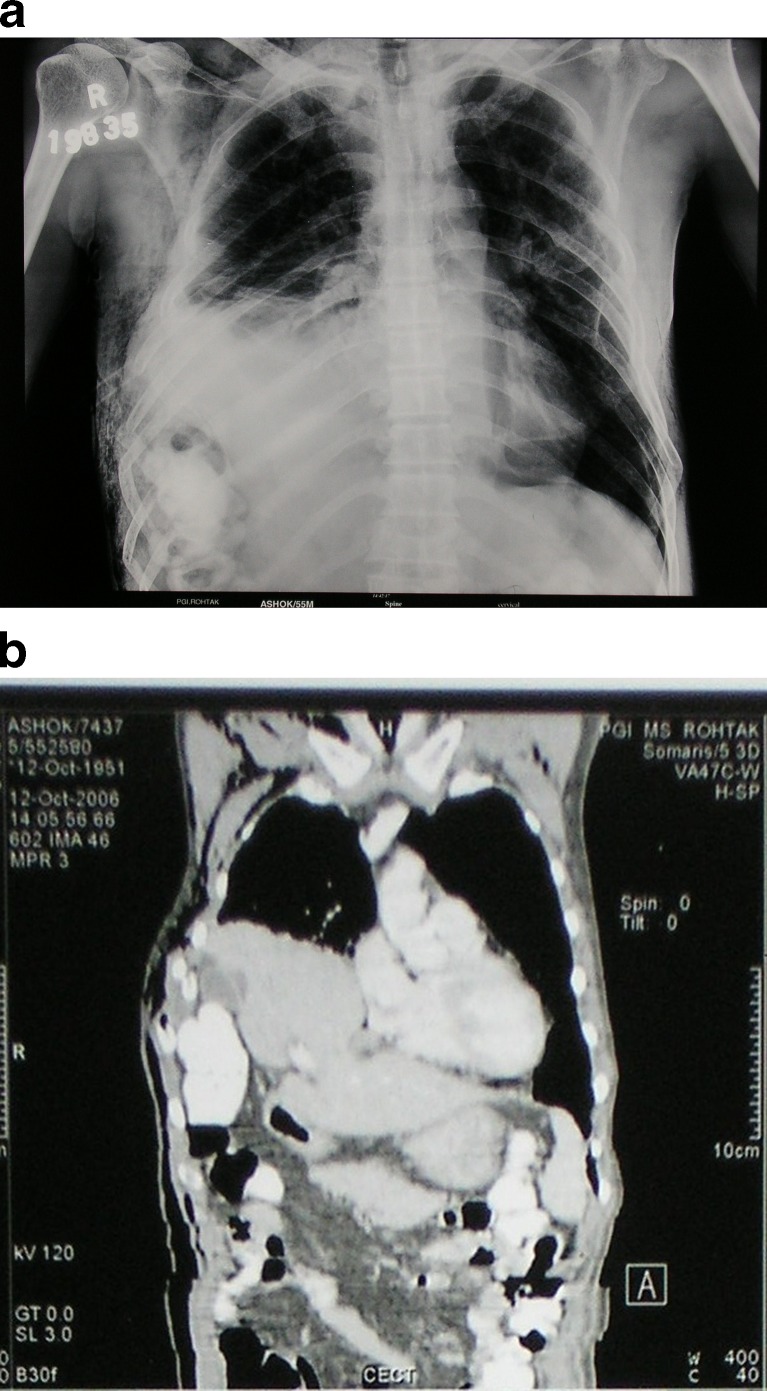
Fig. 2.
Axial CT section of a 30-year-old man showing herniation of the stomach on the left side with fracture of ribs: “collar sign” and “dependent viscera” sign
Fig. 3.
a Chest radiograph of a 55-year-old man showing multiple rib fractures on the right side with homogenous opacity in the right lower zone. There is the raised right hemidiaphragm with obliteration of its outline. b Coronal multiplanar reconstruction (MPR) of the same patient through the lung base showing herniation of the liver, gallbladder, and large bowel through the right hemidiaphragm
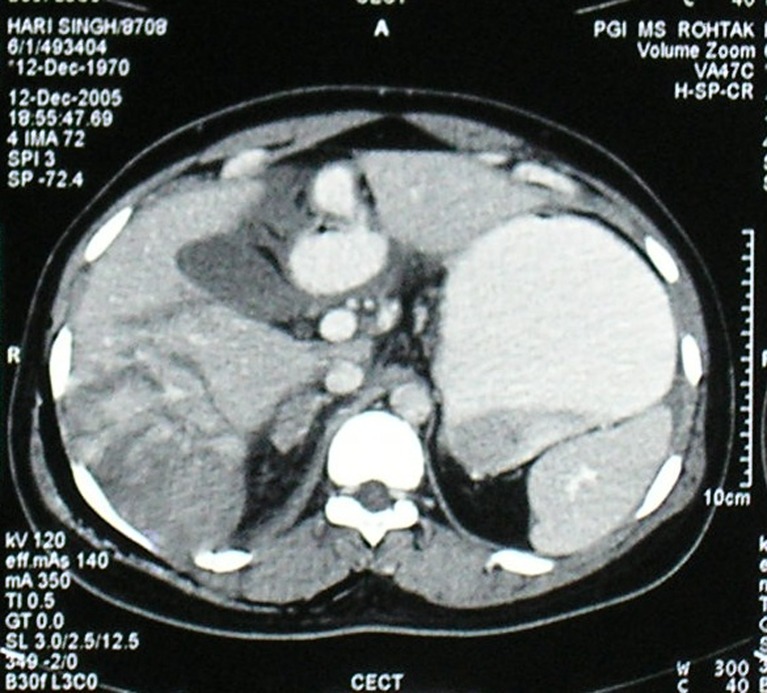
Fig. 4.
Axial CT section of a 35-year-old male patient showing “thickened right crus” with the liver and right adrenal laceration
Table 1.
Radiographic findings in patients with rupture of diaphragm
| S. No. | Radiographic features | No. of patients |
|---|---|---|
| 1 | Obliteration/distortion of outline of hemidiaphragm | 5 |
| 2. | Elevation of hemidiaphragm | 7 |
| 3. | Pleural effusion | 6 |
| 4. | Air-fluid levels in thorax | 7 |
| 5. | Mediastinal shift | 5 |
| 6. | Visualization of nasogastric tube/viscus in thorax | 6 |
| 7. | Fracture of lower ribs | 2 |
Various features seen on CT scan were (Table 2) diaphragmatic discontinuity in 13 patients (Fig. 2); thickened diaphragm was seen in 10 patients (Fig. 4); “collar sign” was seen in 8 patients (Figs. 2 and 3b); visceral herniation was seen in 12 patients (Figs. 1b, 2 and 3b); dependent viscera sign was seen in 8 patients (Fig. 2); and segmental nonrecognition of the diaphragm was seen in 1 patient. Most common herniated contents were stomach and bowel loops on the left side (Fig. 2) and the liver on the right side (seen in two cases) (Fig. 3b). Associated finding including bilateral hemothorax was seen in 5 patients, left-sided hemothorax was seen in 4 patients, and right-sided hemothorax was seen in 3 patients. Hemoperitoneum was seen in 4 patients. Associated solid organ injuries were liver injuries in 9 (Fig. 4), splenic injury in 1, pancreatic injury in 2, kidney injury in 5, adrenal injury in 3 (Fig. 4), and small bowel injury in 2 patients. Fracture of ribs was seen in 7 patients (41.17%), fracture of the pelvis was seen in 2 patients (10.52%), and fracture sternum and thoracic vertebrae were seen in 1 case (5.2%) each.
Table 2.
MDCT findings of diaphragmatic hernia
| Case No. | Age (years) | Sex | Mode of injury | Side of rupture | CT findings | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Diaphragm discontinuity/defect | Collar sign | Thickened diaphragm | Visceral herniation | Dependent viscera sign | Others | |||||
| 1 | 40 | Male | RSA | Left | + | + | − | Present (stomach and omentum) | + | B/L hemothorax, # Rt. ribs |
| 2 | 8 | Male | History of fall into a pond | Left | + | + | − | Present (stomach and gut loops) | − | – |
| 3 | 18 | Male | RSA | Left | + | + | − | Present (stomach and colon) | + | Left hemothorax, hemoperitoneum |
| 4 | 48 | Male | RSA | Right | − | − | + | – | − | B/L hemothorax |
| 5 | 20 | Male | RSA | Left | + | + | + | Present (stomach and colon) | − | Left hemothorax |
| 6 | 25 | Male | RSA | Right | + | − | + | Present (liver) | − | B/L hemothorax, Hemoperitoneum, # Rt. ribs |
| 7 | 35 | Male | RSA | Right | − | − | + | – | − | Right hemothorax, hemoperitoneum # Rt. ribs |
| 8 | 18 | Male | RSA | Right | − | − | + | – | − | right hemothorax, hemoperitoneum # Rt. ribs |
| 9 | 20 | Male | RSA | Right | − | − | + | – | − | – |
| 10 | 31 | Male | History of assault (2 years back) | Left | + | + | − | Present (splenic flexure, stomach, and omentum) | + | Left hemothorax # Lt. ribs |
| 11 | 45 | Male | RSA | Left | − | − | − | – | − | Left hemothorax# Lt. ribs |
| 12 | 50 | Female | RSA | Left | + | − | − | Stomach and bowel loops | + | Right hemothorax |
| 13 | 55 | Male | History of fall of a heavy object | Right | + | + | + | Liver, gall bladder, and gut loops | + | B/L hemothorax # Rt. ribs |
| 14 | 25 | Male | RTA | Left | + | − | − | Stomach and colon | − | B/L hemothorax |
| 15 | 45 | Male | RTA (SWI)* | Right | + | − | + | – | − | – |
| 16 | 40 | Male | Fall of the wall | Left | + | − | − | Stomach and colon | + | – |
| 17 | 36 | Male | Hit by the stick | Right | − | − | + | − | − | – |
| 18 | 28 | Male | RTA | Left | + | + | − | Stomach and colon | + | – |
| 19 | 60 | Male | RTA | Left | + | + | + | Stomach and colon | + | Left hydropneumothorax |
*SWI, steer wheel injury; RTA, road traffic accident; RSA, road side accident
Two patients presented in the delayed phase, one after 2 years and another after 20 years. Mean duration between time of injury and performance of CT scan in the rest of the patients was 44.35 h (range 3–288 h).
Forty-one patients with thoracoabdominal injury were operated. There were 14/19 patients with diaphragmatic hernia. Thirteen patients were operated for diaphragmatic repair (Fig. 5) and one was for bowel injury along with suspected diaphragmatic injury. Two patients were found false-positive. The remaining 5/19 patients were conservatively managed. Out of these, 3/19 patients expired and all three had undergone operative management. In two of these patients, it was for diaphragmatic repair and one was for bowel injury.
Fig. 5.

Peroperative photograph during a thoracotomy showing omentum in pleural cavity
Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of CT scan were 100, 93, 8, 100, and 95%, respectively. Comparison of our findings with those reported in the literature is shown in Table 3. Sensitivity for various CT signs such as direct discontinuity of diaphragm, “collar sign,” intrathoracic herniation of abdominal contents, and “dependent viscera sign” was 100, 66.66, 100, 66.66, respectively.
Table 3.
Comparison of findings of our study with that of other authors
| Series | Sensitivity (%) | Specificity (%) | Positive predictive value (%) | Negative predictive Value (%) | Accuracy (%) |
|---|---|---|---|---|---|
| Murray et al. [5] | 61 | 87 | – | – | – |
| Killeen et al. [16] | 71 | 100 | – | – | – |
| Larici et al. [11] | 84 | 77 | 81 | 81 | 83 |
| Nachimi et al. [18] | 100 | 94.6 | – | – | – |
| Magu et al. [21] | 100 | 96 | 88 | 100 | 97 |
| Our study (2008) | 100 | 93 | 86 | 100 | 95 |
Discussion
The incidence of diaphragmatic rupture varies from 0.8 to 8% following major blunt trauma [9–11]. Sennertus was the first to describe a traumatic diaphragmatic hernia in 1541 [4, 12]. Bowditch made an antemortem diagnosis of a traumatic diaphragmatic rupture in 1853 [13]. Shanmuganathan et al. [9] has stated that more than 90% of blunt traumatic diaphragmatic ruptures occur following motor vehicle accident. There were 12 patients in our study (70.59%). The mechanism of injury is thought to be a lateral impact distorting the chest wall and shearing the diaphragm or a direct frontal impact causing a sudden increase in intra-abdominal pressure [5].
Carter et al. proposed three time phases for patients with diaphragmatic injury. The acute phase extends from the time of injury to 14 days afterward. If the patient survives the initial trauma and the hernia is not manifest within the first 14 days, the second or interval phase is entered. This interval phase extends until the third stage, which is the phase of obstruction or strangulation [6]. Seventeen of our patients presented in the acute phase, while two presented in the delayed phase. We did not pick up any patient in the interval phase.
Injuries to the left hemidiaphragm occur three times more frequently than to the right side following blunt trauma. On the left side, the left posterolateral aspect is the commonest site. This is structurally weak area as it originates from the pleuroperitoneal membrane [14]. The right hemidiaphragm is congenitally stronger and is partially protected by the liver, preventing the transmission of force through the abdominal viscera to the right hemidiaphragm. Bilateral hemidiaphragm injuries are uncommon and are seen in up to 4.5% of patients. There was no case in our study. The left-sided diaphragmatic rupture following blunt trauma is seen in 68.5–87% cases [9, 15]. Eleven patients (57.89%) had the left-sided diaphragmatic rupture in our study.
Although multiple imaging modalities are available to evaluate the diaphragm following major blunt trauma, chest radiographs are the initial and the most commonly performed imaging study. The initial radiographs are diagnostic in 27–60% of cases with the left-sided injury, but only 17% in the right-sided injury [9]. Attempts have been made to improve the sensitivity of plain chest radiographs by repeating films after nasogastric tube placement and contrast-enhanced gastrointestinal tract studies [16]. Chest radiographs were positive in 52.63% in our series and all of them were on the left side.
Diagnosing a diaphragmatic hernia as hydropneumothorax on radiographs is not an uncommon mistake that is made and is well identified in the literature [17]. In our series, one of the cases highlights this mistake (Fig. 1a and b).
Helical CT is valuable in the preoperative detection of diaphragmatic ruptures [5, 16]. Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy reported by various authors [5, 11, 16, 18] are shown in Table 3. Findings are comparable with the findings of our study.
Of the two false-positive cases found in our study, one was a small tear seen in the left diaphragm found on CT scan, which was not confirmed by surgical intervention. Small defect seen in 6% of general population is a normal variant and is seen more commonly in older patients, in women, and in those with emphysema [18]. The second case was diagnosed on the basis of the thickened right hemidiaphragm. Nachimi et al. [18] also found a high degree of false-positivity in their study for this sign.
The most common viscera to herniate is the stomach and colon on the left side and the liver on the right side, as seen in our series [18].
Nachimi et al. [18] described 11 signs of blunt diaphragmatic rupture on CT scan. They found that any positive finding significantly increased the likelihood of blunt diaphragmatic rupture (p < 0.001). Multivariate logistic regression found six signs to be isolated good predictors (p < 0.001) of blunt diaphragmatic rupture: diaphragmatic discontinuity, segmental unrecognized diaphragm, intrathoracic herniation of abdominal content, elevated abdominal organs, thickened diaphragm, and presence of both hemothorax and hemoperitoneum. Murray et al. [5] evaluated 11 cases of diaphragmatic rupture and found that diaphragmatic discontinuity was seen in 8, visceral herniation was seen in 6, and the collar sign was seen in 4 patients.
Dependent viscera sign occurs when the herniated organs directly abut the posterior ribs due to absence of posterior support by the diaphragm, which ruptures in case of diaphragmatic hernia. It is described in the literature to be up to 100% sensitive [19]. Intrathoracic herniation has been found to be 32–64% sensitive. Diaphragmatic discontinuity is 71–80% sensitive and the “collar sign” up to 63% with helical CT [16]. The finding in our series is described in Table 2.
Other signs described in the literature are contrast medium extravasation at the level of the diaphragm described by Larici et al. [11] and hypoattenuation of the hemidiaphragm due to devascularization described by Nachimi et al. [18]. Nachimi et al. found 0% sensitivity for the first sign, as also seen in our series. To the best of our knowledge, no other author has reported the second sign. These signs were not observed in our series.
Both Killeen et al. [16] and Larici et al. [11] found that helical CT performed better for the left-sided injuries, while we found the sensitivity and specificity to be equal on both sides. Also, in contrast to Killeen et al. [16], Larici et al. [11] found that sagittal and coronal reformation added little to the ability to diagnose diaphragmatic injury. It was helpful only in three of our cases.
High incidence of associated injuries such as pelvic fractures, thoracic aortic injury, hepatic, and splenic injuries has been reported in up to 100% of patients with diaphragmatic injury [9]. Brasness et al. [20] have found that associated abdominal injuries are common with liver (38%), spleen (34%), and renal injuries in (30%) and splenic injuries were seen in 7%. Similar findings were seen in our series.
Conclusion
MDCT is a highly accurate modality for diagnosing traumatic diaphragmatic hernia. In addition, it is fast and compatible with various life-support systems; hence, it can be used in acute trauma setting for making a diagnosis and helping in the management.
Footnotes
Authors contribution: Guarantors of the manuscript: SM, SA; Concepts, design, definition of intellectual content, manuscript editing, data analysis: SM, SA, SS; Clinical study, data acquisition: SM, SA, SS; Literature search, manuscript preparation: SA; Manuscript review: SM,SS.
Contributor Information
Sarita Magu, Phone: +91-1262-213967, Phone: +91-9355-622099, Email: snkmagu@gmail.com.
Shalini Agarwal, Email: agarwalsdr@gmail.com.
References
- 1.Gelman R, Mirvis SE, Gens D. Diaphragmatic rupture due to blunt trauma: sensitivity of plain chest radiographs. Am J Roentgenol. 1991;156:51–57. doi: 10.2214/ajr.156.1.1898570. [DOI] [PubMed] [Google Scholar]
- 2.Mirvis SE, Shanmuganathan K. MR imaging of thoracic trauma. Magn Reson Imaging Clin N Am. 2000;8:91–104. [PubMed] [Google Scholar]
- 3.Shanmuganathan K, Killeen K, Mirvis SE, White CS. Imaging of diaphragmatic injuries. J Thorac Imaging. 2000;15:104–111. doi: 10.1097/00005382-200004000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Reber PU, Schmied B, Seiler CA, Baer HU, Patel AG, Büchler MW. Missed diaphragmatic injuries and their long-term sequelae. J Trauma. 1998;44:183–188. doi: 10.1097/00005373-199801000-00026. [DOI] [PubMed] [Google Scholar]
- 5.Murray JG, Caoili E, Gruden JF, Evan SJ, Halvorsen RA, Jr, Mackersie RC. Acute rupture of the diaphragm due to blunt trauma: diagnostic sensitivity and specificity of CT. Am J Roentgenol. 1996;166:1035–1039. doi: 10.2214/ajr.166.5.8615237. [DOI] [PubMed] [Google Scholar]
- 6.Carter BN, Guiseffi J, Felson B. Traumatic diaphragmatic hernia. Am J Roentgenol. 1951;65:56–72. [PubMed] [Google Scholar]
- 7.Iochum S, Ludig T, Walter F, Sebbag H, Grosdidier G, Blum AG. Imaging of Diaphragmatic injury: a diagnostic challenge. Radiographics. 2002;22:S103–S106. doi: 10.1148/radiographics.22.suppl_1.g02oc14s103. [DOI] [PubMed] [Google Scholar]
- 8.Shapiro MJ, Heiberg E, Durham RM, Luchtefeld W, Mazuski JE. The unreliability of CT scans and initial chest radiographs in evaluating blunt trauma inducing traumatic rupture. Clin Radiol. 1996;51:27–30. doi: 10.1016/S0009-9260(96)80214-5. [DOI] [PubMed] [Google Scholar]
- 9.Shanmuganathan K, Mirvis SE. Imaging diagnosis of nonaortic thoracic injury. Radiol Clin N Am. 1999;37:533–551. doi: 10.1016/S0033-8389(05)70110-X. [DOI] [PubMed] [Google Scholar]
- 10.Rivas LA, Fishman JE, Mứnera F, Bajayo DE. Multislice CT in thoracic trauma. Radiol Clin N Am. 2003;41:599–616. doi: 10.1016/S0033-8389(03)00027-7. [DOI] [PubMed] [Google Scholar]
- 11.Larici AR, Gotway MB, Litt HI, Reddy GP, Webb WR, Gotway CA, Dawn SK, Marder SR, Storto ML. Helical CT with sagittal and coronal reconstruction: Accuracy for detection of diaphragmatic injury. Am J Roentgenol. 2002;179:451–457. doi: 10.2214/ajr.179.2.1790451. [DOI] [PubMed] [Google Scholar]
- 12.Shah R, Sabnathan S, Mearns AJ, Choudhury AK. Traumatic rupture of diaphragm. Ann Thorac Surg. 1995;60:1444–1449. doi: 10.1016/0003-4975(95)00629-Y. [DOI] [PubMed] [Google Scholar]
- 13.Mansoor KA. Trauma to the diaphragm. Chest Surg Clin N Am. 1997;7:373–383. [PubMed] [Google Scholar]
- 14.Kuhlman JE, Pozniak MA, Collins J, Knisely BL. Radiographic and CT findings of blunt chest trauma: aortic injuries and looking beyond them. Radiographics. 1998;18:1085–1106. doi: 10.1148/radiographics.18.5.9747609. [DOI] [PubMed] [Google Scholar]
- 15.Mihos P, Potaris K, Gakidis J. Traumatic rupture of the diaphragm, experience with 65 cases. Injury. 2003;34:169–172. doi: 10.1016/S0020-1383(02)00369-8. [DOI] [PubMed] [Google Scholar]
- 16.Killeen KL, Mirvis SE, Shanmuganathan K. Helical CT of diaphragmatic rupture caused by blunt trauma. Am J Roentgenol. 1999;173:1611–1616. doi: 10.2214/ajr.173.6.10584809. [DOI] [PubMed] [Google Scholar]
- 17.Zieren J, Enzweiler C, Muller JM. Tube thoracostomy complicates unrecognized diaphragmatic rupture. Thorac Cardiovasc Surg. 1999;47:199–202. doi: 10.1055/s-2007-1013144. [DOI] [PubMed] [Google Scholar]
- 18.Nachimi A, Szapiro D, Ghaye B. Helical CT of blunt diaphragmatic rupture. Am J Roentgenol. 2005;184:24–30. doi: 10.2214/ajr.184.1.01840024. [DOI] [PubMed] [Google Scholar]
- 19.Colin P, Cantwell MD. The dependent viscera sign. Radiology. 2006;238:752–753. doi: 10.1148/radiol.2382031931. [DOI] [PubMed] [Google Scholar]
- 20.Brasness KA, Bensard DD, Patric DA. Blunt diaphragmatic rupture in children. J Trauma. 2004;56:80–82. doi: 10.1097/01.TA.0000103989.78049.46. [DOI] [PubMed] [Google Scholar]
- 21.Magu S, Yadav A, Agarwal S. Computed tomography in blunt chest trauma. Indian J Chest Dis Allied Sci. 2009;51:75–81. [PubMed] [Google Scholar]