Abstract
We use a small animal model, based on guinea pigs infected with a non-pathogenic Pichinde virus (PICV), to understand the virulence mechanisms of arenavirus infections in the hosts. PICV P2 strain causes a mild febrile reaction in guinea pigs, while P18 causes severe disease with clinical and pathological features reminiscent of Lassa hemorrhagic fever in humans. The envelope glycoproteins (GPC) of P2 and P18 viruses differ at positions 119, 140, and 164, all localized to the receptor-binding G1 subunit. We found that lentiviral pseudotyped virions (VLPs) bearing P18 GPC show more efficient cell entry than those with P2 GPC, and that the E140 residue plays a critical role in this process. Infection of guinea pigs with the recombinant viruses containing the E140K change demonstrated that E140 of GPC is a necessary virulence determinant of P18 infections, possibly by enhancing the ability of virus to enter target cells.
Keywords: virulence, arenavirus, Pichinde virus, glycoprotein, entry
Introduction
Lassa virus (LASV), an Old World (OW) arenavirus, causes endemic Lassa fever in West Africa with estimated 300,000 to 500,000 infections and 5,000 deaths annually (Khan et al., 2008; McCormick and Fisher-Hoch, 2002). In South America, several New World (NW) arenaviruses, such as Junin (JUNV) and Machupo (MACV), cause sporadic hemorrhagic fever diseases (Buchmeier et al., 2007). Novel arenaviruses that can cause hemorrhagic fever diseases have also been identified in recent years (Briese et al., 2009; Delgado et al., 2008), highlighting the urgency to develop much-needed preventive and therapeutic measures. Efforts to develop antiviral approaches, however, have been hampered by the lack of in-depth understanding of the mechanisms of arenavirus replication and pathogenesis due to the strict requirement of Biosafety-Level 4 (BSL-4) containment to work with these live pathogenic arenaviruses.
Pichinde virus (PICV) is a NW arenavirus that is non-pathogenic in humans and can be safely studied at BSL-2. Its natural host is the Columbian rice rat Oryzomys albigularis (Trapido and Sanmartin, 1971). Whereas a low number of passages of PICV in inbred guinea pigs produce an avirulent virus that causes a brief febrile reaction, extended passage in inbred guinea pigs has led to the isolation of highly pathogenic strains that cause severe disease characterized by fever, severe weight loss, terminal shock syndrome, and death, similar to those found in human Lassa fever (Aronson et al., 1994; Jahrling et al., 1981; Lucia et al., 1990; McCormick et al., 1987; Qian et al., 1994). Due to the difficulty in maintaining inbred strain 13 guinea pigs, Aronson and her colleagues have shown that similar distinct disease patterns were also observed in outbred Hartley guinea pigs infected by a low passge (e.g., strain P2) and a high passage (e.g., strain P18) PICV strains (Zhang et al., 2001). PICV infection in guinea pigs, therefore, represents a safe, convenient, and economical small animal model to investigate the pathogenesis of arenavirus hemorrhagic fevers (Aronson et al., 1994; Cosgriff et al., 1987; Jahrling et al., 1981; Schaeffer et al., 1993). Understanding the virulence mechanisms by which the two closely related PICV strains cause distinct disease outcomes in guinea pigs is expected to shed important lights into those of pathogenic arenaviruses in humans. We have identified several amino acid differences in the viral coding sequences, including three mutations in the viral envelop glycoprotein (GPC) (Lan et al., 2008). We propose that these GPC mutations may be important virulence determinants.
Arenavirus envelope glycoprotein is translated as a precursor protein that is cleaved by signal peptidase and the SKI-1/S1P protease into three subunits: 58-aa stable signal peptide (SSP) as well as the canonical receptor-binding and transmembrane fusion subunits (G1 and G2, respectively) (Buchmeier et al., 2007). Arenavirus SSP is unique in that it is a component of the mature GPC complex and plays important roles not only in regulating the intracellular trafficking and proteolytic maturation of the GPC complex, but also in pH-induced membrane fusion activity and virus entry (Agnihothram et al., 2006; York and Nunberg, 2006, 2009). G1 is variable among arenaviruses and determines receptor specificity. So far two arenavirus receptors have been identified, the alpha-dystroglycan used by OW and NW Clade C arenaviruses such as LASV and LCMV (Cao et al., 1998; Spiropoulou et al., 2002), and transferrin receptor 1 used by NW Clade B arenaviruses such as JUNV and MACV(Abraham et al., 2009; Radoshitzky et al., 2007). The receptor for NW Clade A arenaviruses such as PICV is unknown. The G2 subunit contains a fusion peptide and a transmembrane (TM) domain, and is involved in fusion activity (Buchmeier et al., 2007).
A virulent P2 GPC differs from virulent P18 by three residues at positions 119, 140, and 164, all localized to the receptor-binding G1 subunit (Lan et al., 2008). In this study, we characterized the effects of these GPC mutations on viral entry using a pseudotyped lentivirus system, and on viral virulence in guinea pigs using recombinant PICV mutants (Lan et al., 2009). Our studies reveal that a single amino acid E140 in GPC increases the GPC-dependent virus entry in vitro and is also a necessary virulence determinant of P18 infections in vivo.
Results
P18 GPC protein mediates more efficient cell entry than P2 GPC protein in a pseudotyped virus system
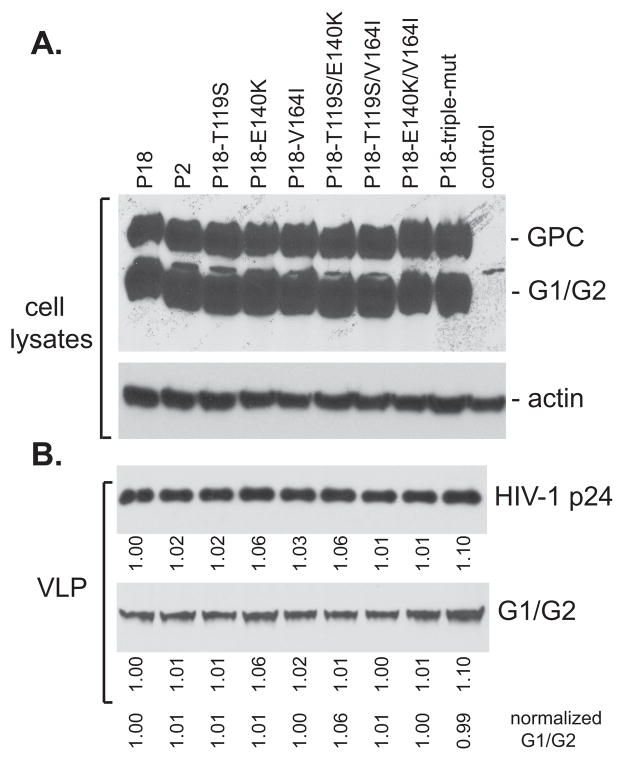
Studies from our laboratory as well as others have shown that P18 PICV causes severe hemorrhagic fever-like disease in guinea pigs, in contrast to the avirulent P2 strain (Lan et al., 2009; Zhang et al., 1999; Zhang et al., 2001). The molecular mechanisms underlying these differences in pathogenesis are unknown. We have shown that the P2 and P18 genomes differ by several encoded amino acids, including three missense mutations located within the receptor-binding G1 subunit of the GPC protein (Lan et al., 2008), which we hypothesize to affect the efficiency of GPC-mediated cell entry. To compare entry efficiency mediated by P2 and P18 GPC, we generated lentivirus-like particles containing P2 or P18 GPC proteins using an established three-plasmid system (Naldini et al., 1996). Briefly, 293T cells were transfected with: pCMV-DR8.2, a plasmid containing the HIV genome except for the packaging signal and envelope gene; pHR’, a plasmid containing a GFP expression cassette and HIV packaging signal; and a pCAGGS expression vector expressing either P2 or P18 GPC proteins. Pseudotyped viral-like particles (VLPs) incorporating the respective GPC protein were harvested from the cell-culture supernatants. P2 and P18 GPC proteins were expressed at similar levels in transfected 293T cells (Fig. 1A) and showed similar cleavage of precursor GPC into mature G1 and G2 (Fig. 1A). Purified GPC-pseudotyped VLPs contained similar ratios of G1/G2 to HIV-1 capsid (p24) protein (Fig. 1B), demonstrating that P2 or P18 GPCs were incorporated into VLPs with similar efficiencies. Upon transduction of guinea pig fibroblast JH4 cells with similar amounts of the VLPs, GFP expression was efficiently and consistently detected in cells transduced using P18 VLPs. In contrast, GFP expression was rare in cells transduced using P2 VLPs. Flow cytometric analysis determined transductions efficiencies of 40 and 0.05%, respectively, in P18 and P2 VLP-transduced cultures (Table 1). Similar results were obtained in multiple cell lines, including 293T, human endothelial cells SLK, human foreskin fibroblast (HFF) cells, Chinese hamster ovarian (CHO) cells, human lung epithelial cells A549, and mouse fibroblast cells 3T3 (data not shown), indicating that P18 GPC is significantly more efficient for cell entry independent of host cell species or cell type.
Fig. 1.
Characterization of the GPC-mediated cell entry by GPC-pseudotyped lentiviral VLPs. (A) Expressions of P2, P18, and P18 mutant GPC proteins in the transfected 293T cells. Western blot analysis was conducted using guinea pig anti-PICV serum. (B) Detection of G1/G2 and HIV-1 p24 in the purified VLPs by western blot analysis. Intensity of each band was quantified by the Image J analysis software and normalized to that of P18.
Table 1.
The efficiency of various GPC-incorporated VLPs in transducing guinea pig fibroblast JH4 cells
| GPC constructs | (GFP-positive)%* |
|---|---|
| P18 | 40.03±2.14 |
| P2 | 0.05±0.005 |
| P18-T119S | 34.13±0.78 |
| P18-E140K | 8.94±0.64 |
| P18-V164I | 41.4±0.17 |
| P18-T119S/E140K | 10.22±0.23 |
| P18-T119S/V164I | 25.57±0.45 |
| P18-E140K/V164I | 9.65±0.69 |
| P18-T119S/E140K/V164I | 0.07±0.009 |
results shown are the averages of at least three independent experiments with standard deviation
Amino acid E140 is critical in enhancing pseudotyped virus-mediated cell entry
To identify the P18-specific residue(s) responsible for increased cell entry, we compared the entry efficiency of VLPs bearing one or more P2 mutations in JH4 cells (Table 1). A single P2-specific mutation at residue 140 (E140K), but not at 119 (T119S) or 164 (V164I), caused a significant reduction in VLP entry efficiency from 40 to 9%, suggestive of a critical role of E140 in enhancing GPC-mediated cell entry. It is noteworthy that the E140K VLPs were still more efficient than P2 GPC-containing VLPs in transducing cells (9% vs. 0.05%), implying that the other two amino acid substitutions may also participate at some levels to optimize cell entry. Indeed, the T119S/V164I double mutant caused a moderate reduction in cell entry at a level of ~ 26% transduction efficiency, whereas the triple mutant (T119S/E140K/V164I) reduced cell entry to a similar level (~ 0.07%) as that of the P2-GPC containing VLPs. Collectively, our data suggest that the E140 residue is critical in enhancing GPC-mediated cell entry, and this effect is potentiated by T119 and/or V164 residue.
Generation of recombinant P18 viruses with P2-specific residues in GPC
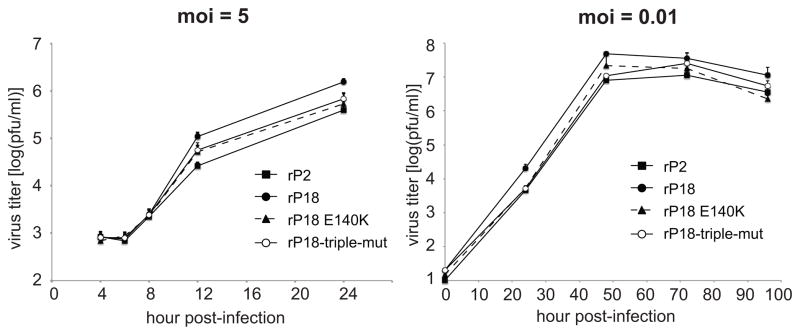
Taking advantage of our PICV reverse genetics system (Lan et al., 2009), we generated recombinant PICV viruses carrying a single E140K or triple T119S/E140K/V164I mutation in the P18 virus backbone (rP18-E140K and rP18-triple-mut, respectively). The recombinant viruses were plaque-purified and mutations were confirmed by sequence analysis. Viral growth was compared in BHK-21 cells with both high and low moi (Fig. 2). Differences seen in virus entry using pseudotyped VLPs were reduced in the context of recombinant virus. Nonetheless, rP18 replicated to slightly higher titer than rP2 (~ 0.5 log), as we have previously reported (Lan et al., 2009; Liang et al., 2009), while the mutants grew intermediately at high moi and aligned more with rP2 than with rP18 at low moi (Fig. 2). Similar growth kinetics were also observed in U937 cells (data not shown).
Fig. 2.
Comparison of recombinant PICV strains in viral growth in vitro. BHK-21 cells were infected at high moi (moi = 5) or low moi (moi = 0.01) with various PICV strains. Viral production at various time points was quantified by plaque assay. Results shown are the average of triplicates with error bars showing standard deviations. Experiments were conducted as described in Materials and Methods. Results shown are the average of triplicates, with error bars showing standard deviations.
E140 is a virulence determinant of PICV infection in vivo
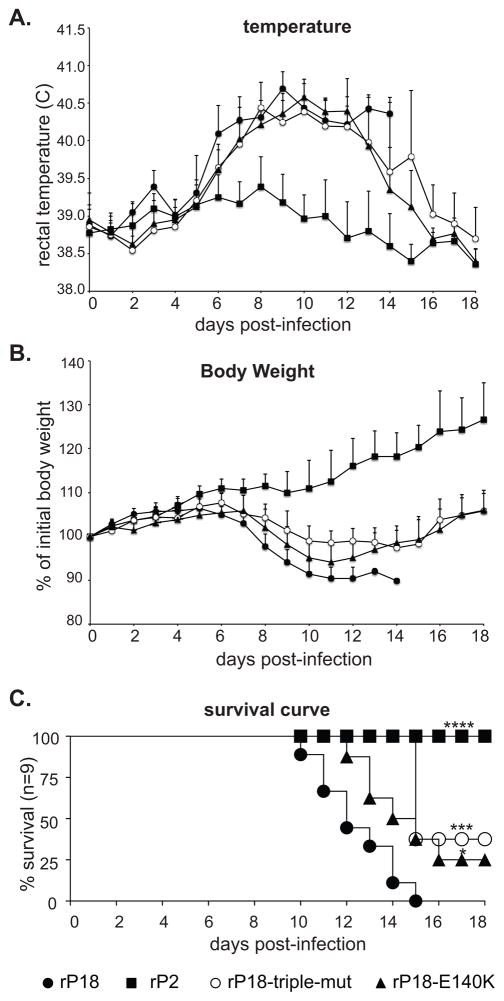
We compared the degrees of virulence of the recombinant PICV strains in guinea pigs by following the established protocol (Lan et al., 2009). Briefly, male Hartley guinea pigs (n=9) were infected i.p. with 104 pfu of rP2, rP18, rP18-E140K, and rP18-triple-mut, respectively, and monitored daily of body weight and rectal temperature for up to 18 days post infection (dpi). Animals were euthanized when they have reached predetermined terminal points as approved by our institutional IACUC committee. As previously reported, all animals that have been infected with the avirulent rP2 experienced a brief period of fever (average of 1–2 days) but maintained their body weights (Fig. 3A–B). In contrast, all 9 animals that have been infected with virulent rP18 suffered from a long duration of fever (average of 8–9 days) and significant body weight loss, and had to be euthanized (100% mortality due to reaching terminal points) (Fig. 3A–B). Animals infected with either of the two GPC mutant viruses, however, showed variable outcomes: some showing similar consequences as rP18-infected ones and euthanized when reaching terminal points, others recovered from the infections as evidenced by increased body weight and fever reduction (Fig. 3A–B). As shown in the survival curve (Fig. 3C), virulent rP18 caused 100% mortality within 15 dpi, in contrast to 0% for avirulent rP2. The rP18-triple-mut and rP18-E140K viruses each showed 33–40% survival rate that is significantly different from the rP18 control (Fig. 3C), suggesting that both GPC mutant viruses are less virulent than rP18. There is, however, no significant difference in the survival curves between animals infected with the single and triple mutant viruses.
Fig. 3.
Virulence determination of recombinant PICV strains in guinea pigs. Each group (n=9) of male outbred Hartley guinea pigs were infected intraperitoneally with 10,000 PFU of recombinant viruses rP18, rP2, rP18-triple-mut, or rP18-E140K for up to 18 days. (A) The average of daily rectal temperature is shown. (B) The average of daily body weight is shown. (C) The survival curve of animals infected with recombinant viruses. Statistical significance was as determined by Log-rank (Mantel-Cox) χ2 Test.
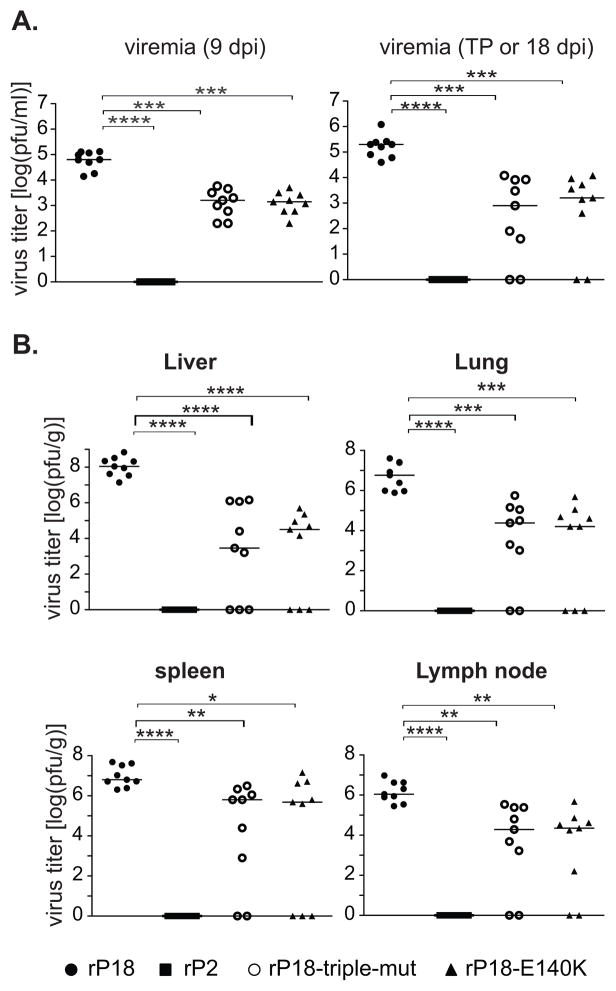
As arenavirus virulence correlates with the level of viral replication in vivo, we quantified titers of the viruses in blood and in different organs of infected animals. Viremia level was compared at 9 dpi and at 18 dpi or terminal points (Fig. 4A). At both time points, the rP2-infected animals had below-the-threshold viremia level, whereas the rP18-infected animals all contained high (~ 105 pfu/ml) viral titers in blood. Animals infected with the GPC mutant viruses (rP18-E140K and rP18-triple-mut) had ~ 2 log lower viremia (~ 103 pfu/ml) at 9 dpi than those with rP18. These GPC mutants-infected animals had very low (< 100 pfu/ml) to undetectable viral titers in blood at 18 dpi if they have survived the infections, and had ~ 2 log in average lower viremia than rP18-infected ones at terminal points (TP) (Fig. 4A). Consistent to viremia level, the rP2-infected animals completely cleared virus infections from tested organs such as liver, lung, spleen, and lymph nodes at the end of experiment (18 dpi), whereas the rP18-infected animals contained high titers of viruses, ranging from 106 pfu/g in lymph nodes to 108 pfu/g in livers, at terminal points (Fig. 4B). The GPC mutants-infected animals had very low (< 1000 pfu/g) to undetectable viral titers in the tested organs at 18 dpi if they have survived from the infections, and had significantly lowered viral titers in organs than rP18-infected ones even when they have succumbed to the infections (Fig. 4B). On average, the differences in viral titers in various organs between the GPC mutant viruses and rP18 are ~ 1 log in spleens, ~ 2 logs in lymph nodes, 3 logs in lungs, and 3 – 4 logs in livers (Fig. 4B). Taken together, our results clearly show that the GPC mutants replicate at much lower level than rP18 does in vivo.
Fig. 4.
Comparison of recombinant PICV strains in viral replication in vivo. (A) Viremia levels of infected animals at day 9 and day 15 post-infection. (B) Viral titers in internal organs (liver, lung, spleen and lymph nodes) at terminal points or at the end of infection (18 dpi). Statistical analysis was conducted using the Student’s t-test. p < 0.05, p < 0.01 indicated by **, P < 0.001 by ***, and P < 0.0001 by ****.
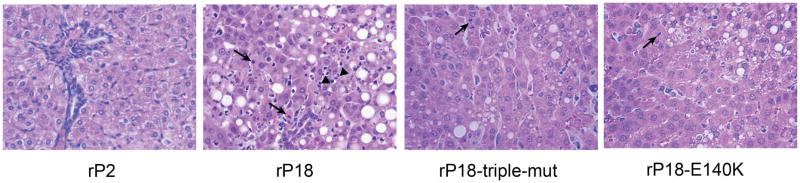
Comparison of liver histopathology also showed differential degrees of virulence in animals infected by different virus strains. The rP2-infected animals did not show any obvious liver pathology, the rP18-infected ones showed most severe lesions, whereas the GPC mutants caused intermediate levels of pathology (Fig. 5). For rP18-infected animals, the normal architecture of the hepatic cords is distorted due to marked hepatocellular vacuolar degeneration, and necrotic hepatocytes are scattered with possible lymphocyte infiltration (Fig. 5). Guinea pigs that recovered from either GPC mutant infection did not show any obvious liver pathology (data not shown), similar to the rP2-infected animals. The moribund animals infected with either GPC mutant virus exhibited a generally less liver pathology than the rP18-infected ones as evidenced by less hepatocellular vacuolar degeneration and less hepatocellular necrosis (Fig. 5), which correlates with the average 3–4 logs lower levels of mutant viruses than rP18 in the livers (Fig. 4B). Therefore, the GPC mutant viruses also caused less pathogenesis in animals than the virulent rP18 virus.
Fig. 5.
Histopathological analysis of liver specimens from guinea pigs infected with recombinant PICV strains after hematoxylin and eosin staining. Arrow shows necrotic hepatocytes and arrowhead shows infiltrated lymphocytes.
Collectively, these in vivo data demonstrate that the introduction of P2-specific residue(s) to P18 GPC significantly reduced the P18 virulence in vivo, as demonstrated by the increased survival rate (Fig. 3), the decreased viral titers (Fig. 4), and the reduced liver pathogenesis (Fig. 5). No obvious difference in the degree of virulence (survival curve, viral titer, and liver pathology) was detected between the single (E140K) and the triple GPC mutants. Therefore, we conclude that the single E140 residue of GPC is an important virulence determinant of P18 infections in vivo.
Discussion
Among Arenaviridae family members, only a few can cause virulent infections in unnatural hosts, such as arenavirus-induced hemorrhagic fevers in humans, the reasons of which are largely unknown. A postulated hypothesis proposes that the viral genome may encode critical determinants for virulence. We use a safe small animal model, in which two PICV strains derived from low (P2) and high (P18) passages in guinea pigs can respectively cause avirulent and virulent infections with opposing outcomes in the animals, to characterize the virulence-associated determinants in arenavirus genome. Compared to the variable mortality rates of outbred guinea pigs infected with virulent PICV in previous studies (Jahrling et al., 1981; Scott and Aronson, 2008), we have observed more consistent high mortality rate and hemorrhagic fever symptoms in our infected animals (Figs 3–5), which is likely due to different experimental settings between our study and others. Knowledge of virulence mechanisms learned from the PICV-guinea pig model can be extrapolated to other pathogenic arenaviruses in humans. Through site-directed mutagenesis and comprehensive characterization of the mutant viruses in this study, we have shown that the E140 residue within the receptor-binding GP1 subunit is an essential virulence determinant of P18 infection of guinea pigs, as the E140K substitution can significantly reduced viral replication and pathogenesis in vivo (Figs 3–5). We have also provided evidence to suggest that the molecular mechanism by which the E140 residue enhances viral replication and virulence is possibly due to its ability to enhance cell entry efficiency as demonstrated in the pseudotyped lentiviral system (Table 1).
Using pseudotyped VLPs, we have shown that GPC of virulent P18 virus can mediate a much more efficient cell entry than that of avirulent P2 into a variety of cell lines (data not shown). The correlation of cell entry efficiency and viral virulence in vivo have led us to believe that GPC-mediated cell entry may be an important virulence mechanism of arenavirus infection in vivo. As P2 and P18 GPC proteins differ at three amino acids, 119, 140, and 164, within the G1 subunit that mediates specific binding to host receptor(s) (Lan et al., 2008), we hypothesize that these residues can affect virus-cell binding to influence the virus entry efficiency. By systematic mutagenesis, we learn that the K140E substitution with a change from positive to negative side chain of the amino acid during the P2→P18 adaptation is essential in enhancing cell entry, which can be further augmented by the S119T or I164V substitution (Table 1). However, the exact molecular mechanism by which these amino acid substitutions enhance GPC-mediated cell entry requires a better understanding of PICV GPC interaction with its host receptor(s) at the atomic level, information of which is not available at the moment. The entry receptor of PICV as well as other members of Clade A NW arenaviruses has not yet been identified, although we have produced preliminary data to suggest that PICV does not primarily use a-DG or TfR1 for entry (unpublished data).
Additionally, we have provided evidence to demonstrate the important role of the E140 residue in mediating PICV replication and virulence in vivo. We have shown that a single amino acid substitution of E140 with the P2-specific residue K in the genome of virulent rP18 virus has improved survival rate of infected animals (Fig. 3). Furthermore, this E140K single substitution has led to significantly lower level of viral replication in vivo by at least 2 logs in blood and by 1–4 logs in various organs (Fig. 4), and subsequently less liver pathogenesis (Fig. 5), even in the moribund animals. Our in vivo data have provided evidence for E140 as one of the important virulence determinants of P18 infection in guinea pigs, which correlates well with its role in increasing GPC-dependent virus entry in vitro. It is noteworthy that compared to the pronounced 1–4 log difference in viral replication in vivo (Fig. 4), the GPC mutant viruses replicate only slightly less than the parental rP18 virus by < 0.5 log in vitro (Fig. 2A). This could be explained by the differences between the in vivo and in vitro experimental conditions, among which host immunity may play an important role in amplifying the differential infectivity of viral strains in vivo. As early target cells of arenavirus infections are macrophages and DCs, which are immune cells important for both innate and adaptive immune responses, differential entry efficiency into these early target cells due to GPC mutations not only can lead to intrinsically different viral replication levels but may also affect host immunity that in return leads to even greater differences in viral growth in vivo. Regardless of the mechanisms, our data show that the GPC-mediated differential cell entry into host target cells leads to the differences in viral growth in vivo.
This GPC-dependent virulence mechanism is also supported by a recent report demonstrating that a single mutation in LCMV GPC is necessary and sufficient for receptor binding, dendritic cell infection, and long-term persistence (Sullivan et al., 2011). It is important to note, however, that mutations in GPC alone did not reduce PICV viral virulence to the level of rP2 (Figs 3–5), suggesting the contribution of other possible viral virulence factors besides GPC. We have recently produced evidence to demonstrate that both viral L polymerase and nucleoprotein (NP) may also play important roles in mediating virus virulence ((Liang et al., 2009) and our unpublished data). Efforts to characterize the virulence-associated mutations in the NP and L proteins are currently underway. Taken together, our study suggests that virulent arenavirus infections are a complex process that requires the synergetic functions of different viral proteins, including but not necessarily limited to GPC, to increase viral entry and RNA synthesis, and to effectively evade host immune detection (Fan et al., 2010; Martinez-Sobrido et al., 2006; Qi et al., 2010).
Materials and Methods
Cells
293T (human kidney epithelial), SLK (human endothelial), HFF (human skin fibroblast), A549 (human embryonic lung epithelial) and NIH 3T3 (mouse embryonic fibroblast) were grown in DMEM supplanted with 10% fetal bovine serum (FBS). JH4 (guinea pig lung fibroblast) and CHO (Chinese hamster ovary epithelial) were grown in DMEM F12 supplemented with 10% FBS. Vero cells were grown in MEM supplemented with 10% FBS. Human monocytic U937 cells were grown in RPMI-1640 supplemented with 10% FBS.
GPC protein vector construction, mutagenesis, and expression
We amplified the GPC genes from P2, and P18 virion RNAs and subcloned each into pCAGGS expression vectors. The resulted plasmids are named pCAGGS-P2-GPC, and pCAGGS-P18-GPC. Single, double, and triple mutations were introduced into the P18 GPC protein at three residues (T119S, E140K, and V164I) by PCR-mediated site-directed mutagenesis and confirmed by sequencing. Expression of various GPC proteins was examined by transfection of 293T cells with the individual expression vectors, followed by Western blot analysis using anti-PICV guinea pig sera.
Generation of pseudotyped lentivirus-like particles (VLPs)
293T cells were transfected with pHR’GFP, pCMVRΔ8.91, and the individual GPC expression vectors using Lipofectamine 2000 (Invitrogen). Supernatants of the transfected cells were collected at different time points up to 96 h post-transfection and filtered through a 0.45 μm filter. After purification through sucrose gradient ultracentrifugation, the pseudotyped VLPs were resuspended in DMEM, aliquoted, and stored at − 80°C. The amount of VLPs was normalized by the HIV-1 p24 levels as determined by Western blot analysis using an anti-HIV-1 p24 antibody, which is kindly provided by Dr. E. Hunter (Emory University).
Quantification of GPC-mediated cell entry efficiency of VLPs
Target cells were infected with pseudotyped VLPs at moi of 1 in the presence of 2 μg/ml polybrene for 2 h, and replaced with fresh media. GFP protein expression was detected at 72 h post-infection (hpi), either under a fluorescent microscope or by flow cytometric analysis. The efficiency of cell entry was measured by the percentage of cells expressing the GFP protein (GFP+%).
Generation of recombinant viruses
Respective GPC mutations (single E140K and triple T119S/E140K/V164I mutations) were introduced to the plasmid encoding the full-length anti-sense S segment of P18 virus by PCR-mediated mutagenesis and confirmed by sequencing. Recombinant PICV viruses were generated as described before (Lan et al., 2009). Briefly, plasmid encoding either WT or mutant P18 S segment, together with plasmid encoding P18 L segment, was transfected into BSRT7–5 cells that stably express T7 polymerase. Recombinant viruses were plaque purified from the supernatants of the transfected cells, sequence verified by RT-PCR, and amplified in BHK-21 cells. Viral titer was determined by plaque assay.
Determination of viral growth kinetics in vitro
BHK-21 cells were infected with WT or mutant recombinant PICV viruses at moi of 5 or 0.01 for 1 h. After PBS wash for three times, cells were replaced with fresh media. At various times post-infection, viral titers in the supernatants were determined by plaque assay. Viral production at various time points was similarly quantified by plaque assay as described above.
Guinea pig experiments
The experimental procedures for guinea pigs followed the approved protocol of the Institutional Animal Care and Use Committee (IACUC) of the Emory University. Briefly, healthy 400g to 500g male outbreed Hartley guinea pigs were housed to acclimatize for 5 to 7 days after which each group (n=9) of animals were injected intraperitoneally with 10,000 PFU of rP18, rP2, rP18-triple-mut (T119S/E140K/V164I) and rP18-E140K, respectively. Rectal temperature and body weight were measured daily for up to 18 days. Blood was drawn from the marginal ear vein at different days post-infection (dpi). Guinea pigs were declared moribund and euthanized if body weight decreased by 30% when compared to the control group or if animals reached other set terminal points as approved by Emory University IACUC. Virus titration in serum and in tissue specimens was determined by plaque assay in vero cells as described before (Lan et al., 2009). Histopathological analysis was conducted after hematoxylin and eosin staining of formalin-fixed tissue section. Statistical analyses of the survival curve by Log-rank (Mantel-Cox) χ2 Test were conducted using GraphPad prism 5 software. Statistical significance of viral titers in serum and in different tissue sample was analyzed by “t” test.
Acknowledgments
We thank Dr. Johnson (National Animal Disease Center, Ames, IA) for consultation on histopathological analyses of the guinea pig liver samples, Dr. Aronson (University of Texas Medical Branch) for providing P2 and P18 viruses, Dr. Hunter (Emory University) for providing anti-HIV-1 p24 antibody, and Dr. Nunberg (University of Montana) for discussion and sage advice. This work was supported by NIH grant AI083409 to YL, and R56AI091805 and R01AI093580 to HL.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abraham J, Kwong JA, Albarino CG, Lu JG, Radoshitzky SR, Salazar-Bravo J, Farzan M, Spiropoulou CF, Choe H. Host-species transferrin receptor 1 orthologs are cellular receptors for nonpathogenic new world clade B arenaviruses. PLoS pathogens. 2009;5:e1000358. doi: 10.1371/journal.ppat.1000358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agnihothram SS, York J, Nunberg JH. Role of the stable signal peptide and cytoplasmic domain of G2 in regulating intracellular transport of the Junin virus envelope glycoprotein complex. J Virol. 2006;80:5189–5198. doi: 10.1128/JVI.00208-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aronson JF, Herzog NK, Jerrells TR. Pathological and virological features of arenavirus disease in guinea pigs. Comparison of two Pichinde virus strains. Am J Pathol. 1994;145:228–235. [PMC free article] [PubMed] [Google Scholar]
- Briese T, Paweska JT, McMullan LK, Hutchison SK, Street C, Palacios G, Khristova ML, Weyer J, Swanepoel R, Egholm M, Nichol ST, Lipkin WI. Genetic detection and characterization of Lujo virus, a new hemorrhagic fever-associated arenavirus from southern Africa. PLoS pathogens. 2009;5:e1000455. doi: 10.1371/journal.ppat.1000455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchmeier MJ, De La Torre JC, Peters CJ. Arenaviridae: The Viruses and Their Replication. In: Knipe DM, Howley PM, editors. Fields Virology. 5. Lippincott Williams & Wilkins; Philadelphia, PA: 2007. pp. 1791–1827. [Google Scholar]
- Cao W, Henry MD, Borrow P, Yamada H, Elder JH, Ravkov EV, Nichol ST, Compans RW, Campbell KP, Oldstone MB. Identification of alpha-dystroglycan as a receptor for lymphocytic choriomeningitis virus and Lassa fever virus. Science. 1998;282:2079–2081. doi: 10.1126/science.282.5396.2079. [DOI] [PubMed] [Google Scholar]
- Cosgriff TM, Jahrling PB, Chen JP, Hodgson LA, Lewis RM, Green DE, Smith JI. Studies of the coagulation system in arenaviral hemorrhagic fever: experimental infection of strain 13 guinea pigs with Pichinde virus. Am J Trop Med Hyg. 1987;36:416–423. doi: 10.4269/ajtmh.1987.36.416. [DOI] [PubMed] [Google Scholar]
- Delgado S, Erickson BR, Agudo R, Blair PJ, Vallejo E, Albarino CG, Vargas J, Comer JA, Rollin PE, Ksiazek TG, Olson JG, Nichol ST. Chapare virus, a newly discovered arenavirus isolated from a fatal hemorrhagic fever case in Bolivia. PLoS pathogens. 2008;4:e1000047. doi: 10.1371/journal.ppat.1000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan L, Briese T, Lipkin WI. Z proteins of New World arenaviruses bind RIG-I and interfere with type I interferon induction. J Virol. 2010;84:1785–1791. doi: 10.1128/JVI.01362-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahrling PB, Hesse RA, Rhoderick JB, Elwell MA, Moe JB. Pathogenesis of a pichinde virus strain adapted to produce lethal infections in guinea pigs. Infect Immun. 1981;32:872–880. doi: 10.1128/iai.32.2.872-880.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan SH, Goba A, Chu M, Roth C, Healing T, Marx A, Fair J, Guttieri MC, Ferro P, Imes T, Monagin C, Garry RF, Bausch DG. New opportunities for field research on the pathogenesis and treatment of Lassa fever. Antiviral Res. 2008;78:103–115. doi: 10.1016/j.antiviral.2007.11.003. [DOI] [PubMed] [Google Scholar]
- Lan S, McLay L, Aronson J, Ly H, Liang Y. Genome comparison of virulent and avirulent strains of the Pichinde arenavirus. Arch Virol. 2008;153:1241–1250. doi: 10.1007/s00705-008-0101-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lan S, McLay Schelde L, Wang J, Kumar N, Ly H, Liang Y. Development of infectious clones for virulent and avirulent pichinde viruses: a model virus to study arenavirus-induced hemorrhagic fevers. J Virol. 2009;83:6357–6362. doi: 10.1128/JVI.00019-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang Y, Lan S, Ly H. Molecular determinants of Pichinde virus infection of guinea pigs--a small animal model system for arenaviral hemorrhagic fevers. Ann N Y Acad Sci. 2009;1171(Suppl 1):E65–74. doi: 10.1111/j.1749-6632.2009.05051.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucia HL, Coppenhaver DH, Harrison RL, Baron S. The effect of an arenavirus infection on liver morphology and function. Am J Trop Med Hyg. 1990;43:93–98. doi: 10.4269/ajtmh.1990.43.93. [DOI] [PubMed] [Google Scholar]
- Martinez-Sobrido L, Zuniga EI, Rosario D, Garcia-Sastre A, de la Torre JC. Inhibition of the type I interferon response by the nucleoprotein of the prototypic arenavirus lymphocytic choriomeningitis virus. J Virol. 2006;80:9192–9199. doi: 10.1128/JVI.00555-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormick JB, Fisher-Hoch SP. Lassa fever. Curr Top Microbiol Immunol. 2002;262:75–109. doi: 10.1007/978-3-642-56029-3_4. [DOI] [PubMed] [Google Scholar]
- McCormick JB, King IJ, Webb PA, Johnson KM, O’Sullivan R, Smith ES, Trippel S, Tong TC. A case-control study of the clinical diagnosis and course of Lassa fever. J Infect Dis. 1987;155:445–455. doi: 10.1093/infdis/155.3.445. [DOI] [PubMed] [Google Scholar]
- Naldini L, Blomer U, Gallay P, Ory D, Mulligan R, Gage FH, Verma IM, Trono D. In vivo gene delivery and stable transduction of nondividing cells by a lentiviral vector. Science. 1996;272:263–267. doi: 10.1126/science.272.5259.263. [DOI] [PubMed] [Google Scholar]
- Qi X, Lan S, Wang W, Schelde LM, Dong H, Wallat GD, Ly H, Liang Y, Dong C. Cap binding and immune evasion revealed by Lassa nucleoprotein structure. Nature. 2010;468:779–783. doi: 10.1038/nature09605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian C, Jahrling PB, Peters CJ, Liu CT. Cardiovascular and pulmonary responses to Pichinde virus infection in strain 13 guinea pigs. Lab Anim Sci. 1994;44:600–607. [PubMed] [Google Scholar]
- Radoshitzky SR, Abraham J, Spiropoulou CF, Kuhn JH, Nguyen D, Li W, Nagel J, Schmidt PJ, Nunberg JH, Andrews NC, Farzan M, Choe H. Transferrin receptor 1 is a cellular receptor for New World haemorrhagic fever arenaviruses. Nature. 2007;446:92–96. doi: 10.1038/nature05539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaeffer RC, Jr, Bitrick MS, Jr, Connolly B, Jenson AB, Gong F. Pichinde virus-induced respiratory failure due to obstruction of the small airways: structure and function. Exp Lung Res. 1993;19:715–729. doi: 10.3109/01902149309064367. [DOI] [PubMed] [Google Scholar]
- Scott EP, Aronson JF. Cytokine patterns in a comparative model of arenavirus haemorrhagic fever in guinea pigs. J Gen Virol. 2008;89:2569–2579. doi: 10.1099/vir.0.2008/002048-0. [DOI] [PubMed] [Google Scholar]
- Spiropoulou CF, Kunz S, Rollin PE, Campbell KP, Oldstone MB. New World arenavirus clade C, but not clade A and B viruses, utilizes alpha-dystroglycan as its major receptor. J Virol. 2002;76:5140–5146. doi: 10.1128/JVI.76.10.5140-5146.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan BM, Emonet SF, Welch MJ, Lee AM, Campbell KP, de la Torre JC, Oldstone MB. Point mutation in the glycoprotein of lymphocytic choriomeningitis virus is necessary for receptor binding, dendritic cell infection, and long-term persistence. Proc Natl Acad Sci U S A. 2011;108:2969–2974. doi: 10.1073/pnas.1019304108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trapido H, Sanmartin C. Pichinde virus, a new virus of the Tacaribe group from Colombia. Am J Trop Med Hyg. 1971;20:631–641. [PubMed] [Google Scholar]
- York J, Nunberg JH. Role of the stable signal peptide of Junin arenavirus envelope glycoprotein in pH-dependent membrane fusion. J Virol. 2006;80:7775–7780. doi: 10.1128/JVI.00642-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- York J, Nunberg JH. Intersubunit interactions modulate pH-induced activation of membrane fusion by the Junin virus envelope glycoprotein GPC. J Virol. 2009 doi: 10.1128/JVI.02410-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L, Marriott K, Aronson JF. Sequence analysis of the small RNA segment of guinea pig-passaged Pichinde virus variants. Am J Trop Med Hyg. 1999;61:220–225. doi: 10.4269/ajtmh.1999.61.220. [DOI] [PubMed] [Google Scholar]
- Zhang L, Marriott KA, Harnish DG, Aronson JF. Reassortant analysis of guinea pig virulence of pichinde virus variants. Virology. 2001;290:30–38. doi: 10.1006/viro.2001.1127. [DOI] [PubMed] [Google Scholar]