Abstract
Objective
To ascertain the age and gender distribution of patients receiving anticoagulant (AC) treatment with warfarin, and to establish the prevalence of AC treatment and its indications among the Finnish population.
Design
A cross-sectional study in which the patients were identified from the patient records of health centres.
Setting
Primary health care in the Hospital District of South Ostrobothnia in Finland.
Patients
Those inhabitants of 15 municipalities in the study area who received AC treatment with warfarin on 1 April 2004. The total number of inhabitants was 132 621 at the end of 2003.
Main outcome measures
Patient age and gender distributions, the prevalence of AC treatment in the study area, and indications for AC treatment.
Results
Altogether 2389 patients were identified, 51.4% of them men. The mean age of the patients was 72.4 years. The prevalence of AC treatment was 1.8%; when age-adjusted to match the Finnish population it was 1.64%. The proportion of men receiving AC treatment was higher than that of women in all age groups. Atrial fibrillation (AF) was the most common main (60.2%) and second (7.2%) indication for AC treatment.
Conclusion
Compared with Finnish figures 12 years earlier the prevalence of AC treatment has more than doubled, and the proportion of AF among indications has increased from 47% to 67%. New current care guidelines on AF and the increasing proportion of the elderly among the population are probable explanations.
Key Words: Anticoagulation treatment, atrial fibrillation, general practice, prevalence, primary health care, warfarin
According to a Finnish study in 1992 the prevalence of anticoagulant (AC) treatment was 0.65% when age-adjusted to match the Finnish population. Atrial fibrillation was the most common main indication.
According to the present study the prevalence of AC treatment has since more than doubled, being 1.64%.
The proportion of atrial fibrillation among the indications for AC treatment has increased from 47% to 67%.
About half of the patients were 75 years old or older.
Warfarin, a coumarin derivative, produces an anticoagulant effect by inhibiting the vitamin K conversion cycle [1]. The clinical effectiveness of oral anticoagulants has been established by well-designed clinical trials in a variety of disease conditions, e.g. for the prevention of systemic embolism in patients with atrial fibrillation. In 1992 the prevalence of anticoagulant (AC) treatment was 0.65% in a Finnish population study [2]. The most common main indication for this treatment was atrial fibrillation (38%) [3].
The aim of this study was to establish the age and gender distributions of patients receiving AC treatment, and the prevalence of AC treatment in the study population. A further aim was to examine the indications for AC treatment.
Material and methods
The study covered those inhabitants of 15 municipalities in the Hospital District of South Ostrobothnia who received AC treatment with warfarin on 1 April 2004. The number of inhabitants in these municipalities was 132 621 at the end of 2003. These municipalities were served by eight health centres.
The health centre doctors, who were also members of the research group at that time, gathered data from the patient records of their own health centre. The list of patients with name and identification number remained within the health centre. The patient data were entered in the pooled research data without personal identification.
The patients were identified as follows: the health centre doctors (n = 9 at the time) drew from the electronic files of their own health centre a list of all patients whose INR had been examined during the period 1 January 2004–31 March 2004. They confirmed from patient records that the subject was on warfarin treatment on 1 April 2004. The data gathered included for example patient's year of birth, gender, municipality, health centre, main indication for AC treatment (International Classification of Diseases, version 10, the code with three characters), and second indication for AC treatment when needed. The latter was used only when it had really contributed to the initiation of AC therapy. A patient may for example have had atrial fibrillation (AF) for a longer time, but AC treatment had not been started before cerebral thrombosis occurred. The latter was the main indication and AF the second. The two latest INR values and the interval between them were registered, as well as whether the patients had a prosthetic valve.
Frequency distributions and cross-tabulations were used in statistical analysis. The prevalence of AC treatment in the study population was age-adjusted to match the Finnish population as follows: the prevalence figure in each five-year age group was multiplied by the number of inhabitants in that age group and divided by the total number of inhabitants. These figures were then summed up.
Results
Who
Altogether 2389 patients who received AC treatment with warfarin were identified. Of these, 51.4% were men. The overall age range was 4–99 years; mean age was 72.4 years. The mean age of men was 70.0 years; median age 72.0 years. The corresponding figures for women were 75.7 years and 78.0 years. The proportion of patients 59 years or younger was 13.2%. The prevalence of AC treatment in the study population was 1.8%. In different study municipalities the prevalence varied between 1.28% and 2.32%. When this was age-adjusted with the population of Finland at the end of the year 2003, the prevalence of AC therapy was 1.64%.
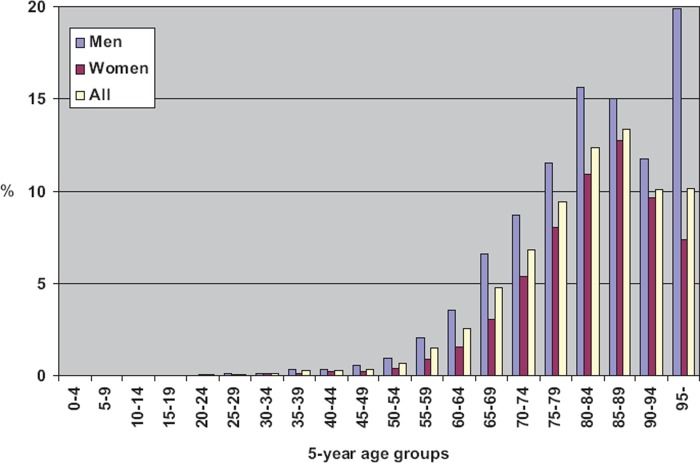
When the prevalence of AC therapy was studied by five-year age groups the figure was found to be highest in the age group 85–89 years old (Figure 1). For women the prevalence was highest in this same age group, while among men it was highest in the oldest (95+ years) group, 31%. This may be due to chance, as the number of patients in this group was small (n = 4) and the number of inhabitants of that age was also small (n = 11). The prevalence of AC treatment was higher among men than among women in all age groups.
Figure 1.
Prevalence of AC treatment in the population of 15 municipalities in South Ostrobothnia as at 1 April 2004 by five-year age groups and gender. (For men 95 years and older the prevalence was 31%.)
A total of 27 patients (1.1%) had a longer than 90-day interval between the two latest INR tests. It is thus likely that some patients who actually received AC therapy on 1 April are missing from the material.
Why
The main indication was found in almost all cases (99.9%) (Table I), and the second was recorded for 25.5% of patients. There were altogether 70 different indications for AC treatment. Altogether 33 indications were recognized as both main and second indications. The most common main indication was AF (Table I). This was also the most common second indication, which means that AF was the indication for AC treatment in 67.4% of patients. AF was also the most common indication for AC treatment in the age group “under 60 years” (Table I). One-fifth of the patients in this age group had deep vein thrombosis as main or second indication.
Table I.
Distribution of main and second indications for AC treatment of all AC patients by age group in 15 municipalities in South Ostrobothnia in Finland, 1 April 2004.
| Age < 60 years n = 317 |
Age ≥ 60 years n = 2072 |
All n = 2389 |
||||
| Indications ICD 10 code and name | Main indication (%) | Second indication (%) | Main indication (%) | Second indication (%) | Main indication (%) | Second indication (%) |
| I48 Atrial fibrillation | 32.5 | 4.4 | 64.5 | 7.6 | 60.2 | 7.2 |
| I80 Deep vein thrombosis of lower extremity | 18.3 | 2.5 | 8.1 | 1.1 | 9.4 | 1.3 |
| I63 Brain infarction | 8.5 | 0.6 | 7.0 | 4.3 | 7.2 | 3.8 |
| I26 Pulmonal emboli | 8.2 | 3.2 | 5.7 | 1.4 | 6.0 | 1.6 |
| I35 Lesions of aortic valve | 15.5 | 1.6 | 4.3 | 1.0 | 5.8 | 1.1 |
| I65 Occlusion and stenosis of precerebral arteries which has not caused brain infarction | 0.6 | 0.6 | 2.3 | 0.8 | 2.1 | 0.8 |
| Other diagnoses | 16.1 | 14.9 | 8.0 | 8.9 | 9.2 | 9.7 |
| No indication | 0.3 | 72.2 | 0.1 | 74.9 | 0.1 | 74.5 |
| Altogether | 100 | 100 | 100 | 100 | 100 | 100 |
Altogether 169 (7.1%) patients had a prosthetic valve. Of these 63% were men; 69% were 60 years or older. The most common main indication was lesions of aortic valve. Thirteen patients had AF as main indication while the AC treatment had been started because of this before the valve operation.
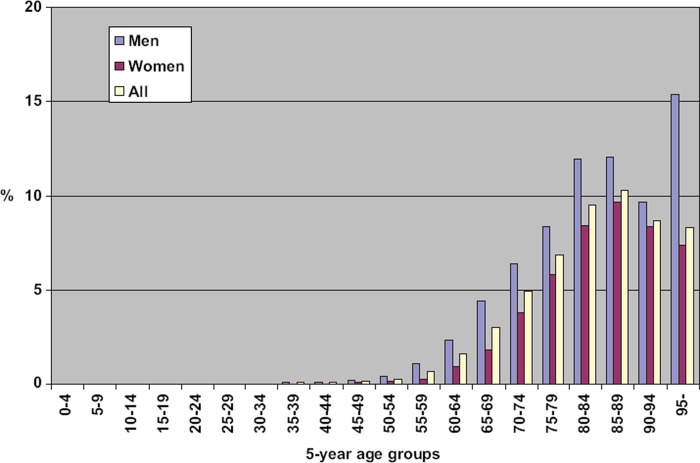
Some 1611 patients had AF and AC treatment, which constitutes 1.2% of the population. The proportion of such patients was highest (10.3%) in the age group 85 – 89 years (Figure 2). This proportion was in all five-year age groups higher among men than among women. Among patients who had AF and AC treatment 89.3% had AF as main indication and 10.7% as second indication.
Figure 2.
Proportion of patients who had atrial fibrillation and AC treatment in the population of 15 municipalities in South Ostrobothnia as at 1 April 2004 in five-year age groups by gender.
Discussion
The prevalence of AC treatment with warfarin had more than doubled from 1992 to 2004. The share of AF as the main indication had increased from 38% to 60%. The mean age of all patients was now 3.5 years higher than that in 1992 (68.9 years) [2].
The results can be compared with the earlier Finnish study. The data were gathered in the same way, but from patient records on paper [2]. In 1992 the study area included 18 municipalities. Of the 15 municipalities in the present study, six were the same and others were situated in the vicinity. The services offered by the health centres, and the population do not differ considerably from the average in Finland. Thus the prevalence of AC treatment age-adjusted to match the Finnish population can indicate the situation in the whole country.
The material included nearly all AC-treated patients. Using the electronic patient records all patients whose INR had been examined during a period of three months could be identified. Some patients are followed up at hospital policlinics for, e.g., their heart disease, but the INR tests are taken in the laboratory of the health centre, and health centre doctors adjust the warfarin dose. Some patients may have visited only private doctors. However, since they mostly use the health centre laboratory for INR testing, there should be no impact on prevalence figures. Self-monitoring of care was very rare in 2004. Also these patients used the health centre laboratory for quality control of monitoring. There were 27 patients who had a longer than 90-day interval between the two latest INR tests. It is thus likely that the prevalence of AC treatment was in reality a little higher than the found 1.8%.
The health centre physicians in the research group themselves drew the requisite data from the patient records. The data gathered – especially information on main and second indications – is thus of good quality. There are few other studies to compare our results concerning prevalence of AC treatment. In a Swedish study with 170 AC patients the prevalence of AC treatment was 0.52% in 1997 [4]. When this was age-adjusted to the Swedish population, the prevalence was 0.88%.
Concerning patients who had AF and AC treatment our results can be compared with two Swedish studies where the prevalence was much lower. In primary health care in Stockholm 827 patients were on warfarin treatment for AF; the prevalence in the population was 0.41%. [5]. Among a population registered in five primary health care centres in Stockholm 419 patients with AF were found, giving a prevalence of 0.60% [6]; 50.4% of these patients received warfarin treatment (0.28% of the population).
In the earlier Finnish study it was estimated that less than half of AF patients received AC treatment [3]. At that time, for example the prevalence of AF patients treated with AC was 1.3% in the age group 65–74, and 2.5% in the group over 74 [3]. The prevalence of AF in the corresponding age groups was 2.8% and 9.0% [7]. There are no newer data regarding the prevalence of AF in Finland. While the prevalence of AF patients treated with AC in the present study was 12% among men aged 80–84 and 85–89, and about 10% among women in the same age groups, it may be assumed that the majority of elderly AF patients receive AC treatment.
In Finland a current care guideline concerning AF was given at the end of 2005 [8]. It was recommended to administer warfarin (INR 2–3) to all patients with AF except those with lone AF and aged less than 60 years [9]. The treatment of AF had been a theme in many continuing educational events for physicians for a couple of years before the current care guideline was given. Also the health centre physicians were thus aware of the coming new guidelines. It is in fact surprising how quickly the change took place. Formerly old age was regarded as a contraindication for AC treatment. It is not self-evident that physicians follow clinical guidelines. This is usually interpreted as indicating that the clinicians are not “good enough” [10]. It is also possible to argue that perhaps the guidelines are not good enough. Here the health centre doctors probably saw the new guidelines as reasonable in their work.
AC treatment entails a considerable workload for primary health care. Self-monitoring and self-adjusting medications have been found to be effective methods of monitoring oral AC therapy, but the patients in question must be appropriately selected [11]. Some do not wish to make health-related measurements at home [12]. In the present study nearly 70% of AC patients were aged 70 years or older. Patient education is a challenge even if it does not include self-testing and adjustment of medication.
During the last few years new anticoagulant drugs have come onto the market to take the place of warfarin [13–16]. Even though some seem to be promising, there are problems. The experience with these drugs is rather short and they do not have a specific antidote to be used in emergency situations like vitamin K is for warfarin. Thus warfarin will probably remain in use for many years.
Among patients treated with warfarin, age has been shown to be continuously and independently associated with increased bleeding risk [17]. It is estimated that the proportion of old persons in the population will rise considerably in the near future [18], and the age-adjusted incidence of AF is expected to increase significantly [19]. AF can thus be seen as a growing public health problem. It is a huge challenge to primary health care to offer safe and high-quality care for patients needing oral AC treatment.
Acknowledgements
The authors would like to thank Drs Anna-Maija Koivukoski, Matti Kähärä and Vilho Vuotari, who participated in the work of the research group in its earlier phases and in gathering the data for this study.
Ethics
The Ethics Committee of the hospital district of South Ostrobothnia has approved the study. The local boards of health or executive committees of all eight health centres gave permission for the study.
Funding for the study
The Hospital District of South Ostrobothnia.
Conflict of interest statement
None of the authors has any conflict of interest to declare.
References
- 1.Hirsh J, Fuster V, Ansell J, Halperin JL. American Heart Association/American College of Cardiology. Foundation guide to warfarin therapy. Circulation. 2003;107:1692–1711. doi: 10.1161/01.CIR.0000063575.17904.4E. [DOI] [PubMed] [Google Scholar]
- 2.Eskola K, Aittoniemi P, Kurunmäki H, Latva-Nevala A, Paloneva M, Wallin A-M, Viitaniemi M, Virjo I, Ylinen S, Öhman S, Isokoski M. Anticoagulant treatment in primary health care in Finland. Scand J Prim Health Care. 1996;14:165–70. doi: 10.3109/02813439609024172. [DOI] [PubMed] [Google Scholar]
- 3.Viitaniemi M, Eskola K, Kurunmäki H, Latva-Nevala A, Wallin A-M, Paloneva M, Virjo I, Ylinen S, Öhman S, Isokoski M. Anticoagulant treatment of patients with atrial fibrillation in primary health care. Scand J Prim Health Care. 1999;17:59–63. doi: 10.1080/028134399750002926. [DOI] [PubMed] [Google Scholar]
- 4.Wändell PE. Anticoagulant patients in Swedish primary health care: A comparison 5 years apart. Scan J Prim Health Care. 1998;16:183–7. doi: 10.1080/028134398750003151. [DOI] [PubMed] [Google Scholar]
- 5.Nilsson GH, Björholt I, Krakau I. Anticoagulant treatment of patients with chronic atrial fibrillation in primary health care in Sweden: A retrospective study of incidence and quality in a registered population. BMC Fam Pract. 2004;21:612–6. doi: 10.1093/fampra/cmh606. [DOI] [PubMed] [Google Scholar]
- 6.Nilsson GH, Björholt I. Occurrence and quality of anticoagulant treatment of chronic atrial fibrillation in primary health care in Sweden: A retrospective study on electronic patient records. BMC Clin Pharmacol. 2004;4:1. doi: 10.1186/1472-6904-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aromaa A, Heliövaara M, Impivaara O, Knekt P, Maatela J, Joukamaa M. English summary, AL:32. Helsinki and Turku, Finland: Publications of Social Insurance Institution; 1989. Terveys, toimintakyky ja hoidontarve Suomessa. Mini-Suomi terveystutkimuksen perustulokset [Health, functional limitations and need of care in Finland. Basic results from the Mini-Finland Health Survey] [Google Scholar]
- 8.Käypä hoito-suositus. Suomen Kardiologisen Seuran asettama työryhmä. Eteisvärinä (Current care guidelines: Working group set up by the Finnish Cardiac Society. Atrial fibrillation) Duodecim. 2005;121:2470–94. [Google Scholar]
- 9.Atrial fibrillation. Current care summary. Working group set up by the Finnish Cardiac Society. http://www.kaypahoito.fi/kotisivut/sivut.koti?p_sivusto=6&p_navi=1303&p_url= http://www.kaypahoito.fi/kh/kh_julkaisu.suositukset (accessed 21 January 2009)
- 10.Petursson H, Linn G, Sigurdsson JA, Hetlevik I. Current European guidelines for management of arterial hypertension: Are they adequate for use in primary care? Modelling study based on the Norwegian HUNT 2 population. BMC Fam Pract. 2009;10:70. doi: 10.1186/1471-2296-10-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ansell J, Jakobson A, Levy J, Völler H, Hasenkam J. Guidelines for implementation of patient self-testing and patient self-management of oral anticoagulation. International consensus guidelines prepared by International Self-Monitoring Association for Oral Anticoagulation. Int J Cardiol. 2005;99:37–45. doi: 10.1016/j.ijcard.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 12.Lamminen H, Niiranen S, Niemi K, Mattila H, Kalli S. Personal health care and the new media in anticoagulant treatment. Scan J Prim Health Care. 2002;20:123–5. [PubMed] [Google Scholar]
- 13.Berry C, Norrie J, McMurray JJ. Ximelagatran compared with warfarin for the prevention of systemic embolism and stroke: An imputed placebo analysis. Cardiovasc Drugs Ther. 2005;19:149–51. doi: 10.1007/s10557-005-3405-4. [DOI] [PubMed] [Google Scholar]
- 14.Weitz JI, Hirsh J, Samama MM. American College of Chest Physicians. Chest. 2008;133((6 Suppl)):234S–256S. doi: 10.1378/chest.08-0673. Erratum in: Chest 2008;134:473. [DOI] [PubMed] [Google Scholar]
- 15.Rosencher N, Arnaout L, Chabbouh T, Bellamy L. [Rivaroxaban (Xarelto): efficacy and safety] Ann Fr Anesth Reanim. 2008;((Suppl 3)):S22–7. doi: 10.1016/S0750-7658(08)75143-8. Review. In French. [DOI] [PubMed] [Google Scholar]
- 16.Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. the RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–51. doi: 10.1056/NEJMoa0905561. [DOI] [PubMed] [Google Scholar]
- 17.Wallvik J, Själander A, Johansson L, Bjuhr Ö, Jansson J-H. Bleeding complications during warfarin treatment in primary healthcare centres compared with anticoagulation clinics. Scand J Prim Health Care. 2007;25:123–8. doi: 10.1080/02813430601183108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Population and cause of death statistics. Statistics Finland: Population projection 2007–2040. http://www.stat.fi/til/vaenn/2007/vaenn_2007_2007–05–31_tie_001_en.html. [Google Scholar]
- 19.Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Abhayaratna WP, Seward JB, Tsang TSM. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006;114:119–25. doi: 10.1161/CIRCULATIONAHA.105.595140. [DOI] [PubMed] [Google Scholar]