Synopsis
The article focuses on the evidence basis for the management of benign paroxysmal positional vertigo (BPPV), the most common diagnosis of vertigo in both primary care and subspecialty settings. Like all articles in this compilation of evidence-based practice, an overview is presented along with evidence based clinical assessment, diagnosis, and management. Summaries of differential diagnosis of vertigo and outcomes are presented.
Keywords: Vertigo, Dizziness, Evidence based otolaryngology, Vestibular, BPPV, Otolaryngologic symptoms
PROBLEM OVERVIEW
Vertigo
Vertigo is a symptom, not a disease. Effective diagnosis and management of vertigo begins with understanding what the symptom may represent. A survey of the members of the American Otological Society and the American Neurotology Society revealed that 75% of respondents agreed or agreed strongly that the definition of vertigo in clinical practice should be more precise. (1) Whereas 45% of respondents favored restricting vertigo to describe a sensation of spinning or turning only, 40% of respondent favored including any sensation of movement in the definition of vertigo. Since acute inner ear pathology typically produces a spinning sensation, the more restrictive definition of vertigo renders it a more specific clue for a possible otologic vestibular disorder. A narrow focus on spinning may not be sensitive to chronic or milder inner ear pathology, however, where sensation of movement other than spinning might be elicited. Even though a consensus has not been reached on the precise definition of vertigo, it is reasonable to infer from the survey results that the overwhelming majority of otologists would recognize vertigo as distinct from other flavors of dizziness, such as presyncopal lightheadedness, disequilibrium, or other unsettling sensations. (2)
Epidemiological surveys showed that 20% to 30% of the population may have experienced vertigo or dizziness in their lifetime. (3-6) A German national telephone health survey followed by structured neurotologic interview identified the lifetime prevalence of vestibular vertigo to be 7.8% with an annual incidence of 1.5%. (7) In the United States 1.7% of ambulatory medical care visits recorded vertigo or dizziness among the chief complaints. (8) Vertigo or dizziness also accounted for 2.5% of presentations to US emergency department in the years 1995 to 2004. (9)
Vertigo is a symptom in a wide range of disorders (Table 1). The article focuses on the evidence basis for the management of benign paroxysmal positional vertigo (BPPV), the most common diagnosis of vertigo in both primary care and subspecialty settings. (10,11)
Table 1.
Basic differential diagnosis of vertigo
| Otological conditions | Neurologic conditions | Others |
|---|---|---|
| Benign paroxysmal positional vertigo | Migraine-associated vertigo | Postural hypotension |
| Vestibular neuritis/labyrinthitis | Vertebrobasillar insufficiency | Medication side effects |
| Meniere's disease | Demyelinating diseases | Anxiety or panic disorder |
| Superior semicircular canal dehiscence | CNS lesions | Cervical vertigo |
Adapted from Bhattacharyya et al 2008 (12)
Benign paroxysmal positional vertigo (BPPV)
Benign paroxysmal positional vertigo (BPPV) is a disorder of the inner ear characterized by episodes of vertigo triggered by changes in head position. (12) BPPV is thought to be caused by the presence of endolymphatic debris in one or more semicircular canals. Direct evidence of such debris or canaliths has been demonstrated for posterior canal BPPV. (13) The presence of debris in lateral canal BPPV has not been demonstrated directly but can be inferred indirectly from the phenomenon of canal switch when repositioning maneuver to treat posterior canal BPPV leads to lateral canal BPPV or vice versa. (14,15)
A population-based study estimates BPPV has a life-time prevalence of 2.4% and accounts for 8% of the individuals with moderate to severe dizziness or vertigo. (16)
Posterior canal BPPV account for about 90% of the cases, and lateral canal BPPV accounts for about 8% of the cases, according to a review of 10 series with a total of 3342 patients. (17) In rare instances the anterior canal, or multiple canals might be involved. (18)
EVIDENCE BASED CLINICAL ASSESSMENT
Diagnosis of posterior canal BPPV
The diagnosis of BPPV affecting the posterior semicircular canal is established by a history of episodic vertigo with changes in head position and the presence of characteristic nystagmus provoked by the Dix-Hallpike test according to a guideline from the American Academy of Otolaryngology-Head and Neck Surgery. (12)
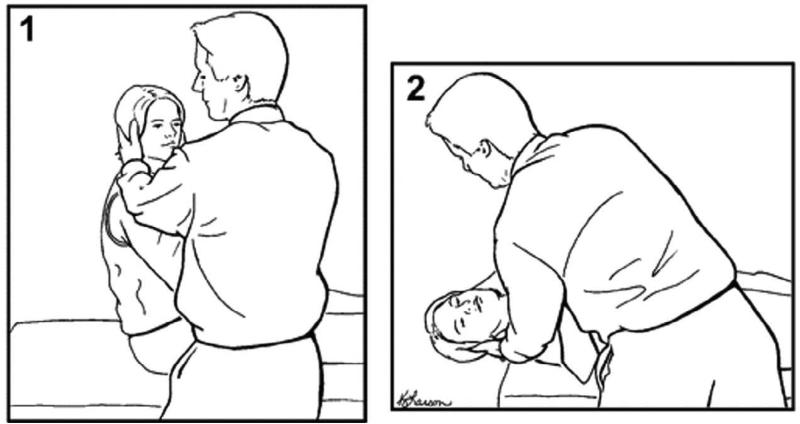
The Dix-Hallpike test (19) (Figure 1) is generally considered the gold standard test for the diagnosis of posterior canal BPPV in that it is the most common diagnostic criterion required for entry into clinical trials and for inclusion of such trials in meta-analyses. (20,21) The Dix-Hallpike test is not truly 100% sensitive, however, since BPPV is an intermittent condition and variations in examiners’ technique and experience might affect the test outcome. The sensitivity of the Dix-Hallpike test has been estimated at 48 to 88% according to a structured review of published literature. (22) The same review found that estimates for specificity is lacking. In the primary care setting, the Dix-Hallpike test reportedly has a negative predictive value of 52% for the diagnosis of BPPV. (10) In a different series of 95 patients diagnosed and treated for posterior canal BPPV in a specialty clinic, 11 patients did not have a positive Dix-Hallpike on initial exam, and 28 presented with an atypical history that did not suggest BPPV. (23) Given the above considerations, the Dix-Hallpike test should be routinely performed if possible in the evaluation of vertigo/dizziness. Whereas a positive test should be considered sufficient for the diagnosis of BPPV in the clinical setting, a negative test should not rule out BPPV completely.
Figure 1.
The Dix-Hallpike test for the diagnosis of posterior canal BPPV [COMP, USE FULL PAGE WIDTH OR NEARLY FULL PAGE WIDTH FOR FIGURE 1]
The patient begins by sitting up right with head is turned 45 degrees toward the side to be tested (1). The patient is then laid back to supine position with head still turned and slightly extended (2). In a positive test torsional nystagmus with the upper pole of the eyes beating toward the dependent ear appears within a few seconds and disappears in less than a minute. A positive Dix-Hallpike test indicates the presence of posterior canal BPPV in the dependent ear. (Adapted from Fife et al. 2008 (25), used with permission)
Repeated testing in separate occasions may be necessary to avoid missing the diagnosis. Failure to diagnose BPPV may lead to costly diagnostic work up. (24)
Diagnosis of lateral canal BPPV
The diagnosis of BPPV affecting the lateral semicircular canal is established with a history of episodic vertigo with changes in head position and the presence of horizontal nystagmus provoked by the supine roll test according to a guideline from the American Academy of Otolaryngology-Head and Neck Surgery. (12)
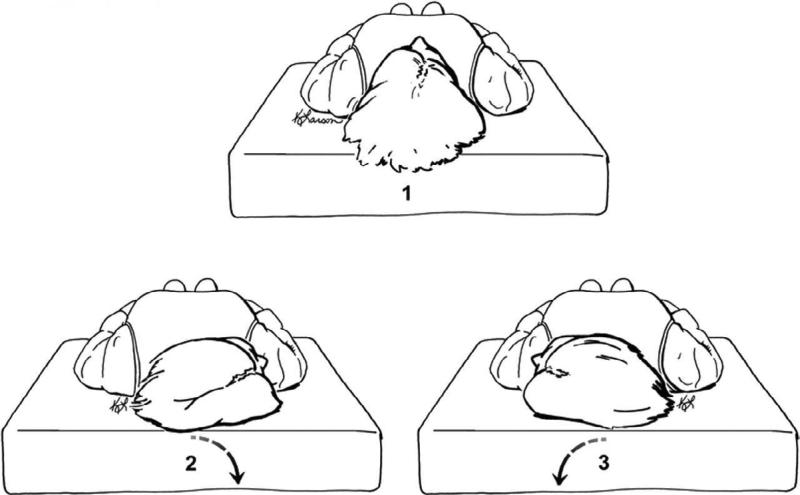
The supine roll test (Figure 2) is performed by rotating the patient's head from neutral to one side while the patient is lying supine. (25) After waiting for any nystagmus or vertigo to subside the test is performed to the opposite side. In a positive test horizontal nystagmus is observed, either beating toward the dependent ear (geotropic) or beating away from the dependent ear (apogeotropic) on both sides. For geotropic nystagmus the side associated with the stronger nystagmus is likely the affected ear. (26,27) For apogeotropic nystagmus the side associated with the weaker nystagmus is the likely the affected ear. (28) Geotropic nystagmus is more common and suggests that the canaliths are located in the long arm of the lateral canal far from the cupula. Apogeotropic nystagmus is less common and suggests that the canaliths are located very close to the cupula or possibly embedded in it. In a review of 9 series with a total of 257 patients with lateral canal BPPV geotropic nystagmus accounts for about 70% of the cases and apogeotropic nystagmus accounts for about 30% of the cases. (17)
Figure 2.
The supine roll test for the diagnosis of lateral canal BPPV [COMP, USE FULL PAGE WIDTH OR NEARLY FULL PAGE WIDTH FOR FIGURE 2]
The patient begins by lying supine with head in neutral position (1). The head is turned to the right side (2) with observation of nystagmus and then turned back to neutral (1). Then the head is turned to the left side (3). The direction of nystagmus in each position is geotropic if it beats toward the lower ear or ageotropic if it beats toward to upper ear. For geotropic nystagmus the side associated with the stronger nystagmus is likely the affected ear. For ageotropic nystagmus the side associated with the weaker nystagmus is the likely the affected ear. (Adapted from Fife et al. 2008 (25), used with permission)
The supine roll test is the most commonly accepted criterion for the diagnosis of lateral canal BPPV in clinical trials. (29-31) There is no literature on the sensitivity or specificity of this test in the diagnosis of lateral canal BPPV partly because clinical history alone is often not sufficient for diagnosis and there is no other gold-standard test to which the supine roll test can be compared.
Limitations of diagnostic maneuvers for BPPV
Patients with the following physical limitations may not be good candidate for Dix-Hallpike or supine head roll test: cervical stenosis, severe kyphoscoliosis, limited cervical range of motion, Down syndrome, severe rheumatoid arthritis, cervical radiculopathies, Paget's disease, ankylosing spondylitis, low back dysfunction, spinal cord injuries, and morbid obesity. (12) A power-driven, multi-axial positioning chair (32) may facilitate testing of such patients. Alternative to the Dix-Hallpike test for the diagnosis of posterior canal BPPV has not been well established. (33)
EVIDENCE BASED MEDICAL AND SURGICAL MANAGEMENT
Natural remission of vertigo in BPPV
BPPV is termed “benign” because it is a naturally resolving condition. In 70 patients with posterior canal BPPV who were observed without treatment, the average time to resolution of vertigo was 39 days, but it took up to 6 months in the extreme. (34) In 16 patients with geotropic variant of lateral canal BPPV who were observed without treatment the average time to resolution of vertigo was 16 days, and all were free of vertigo in 2.5 months. (34) In 14 patients with apogeotropic variant of lateral canal BPPV, the average time to resolution of vertigo was 13 days, and maximum time was 35 days. (35) Despite its favorable prognosis, BPPV is not an entirely benign condition, especially in the elderly, in whom it is often unrecognized and can lead to falls. (36)
Repositioning maneuvers for posterior canal BPPV
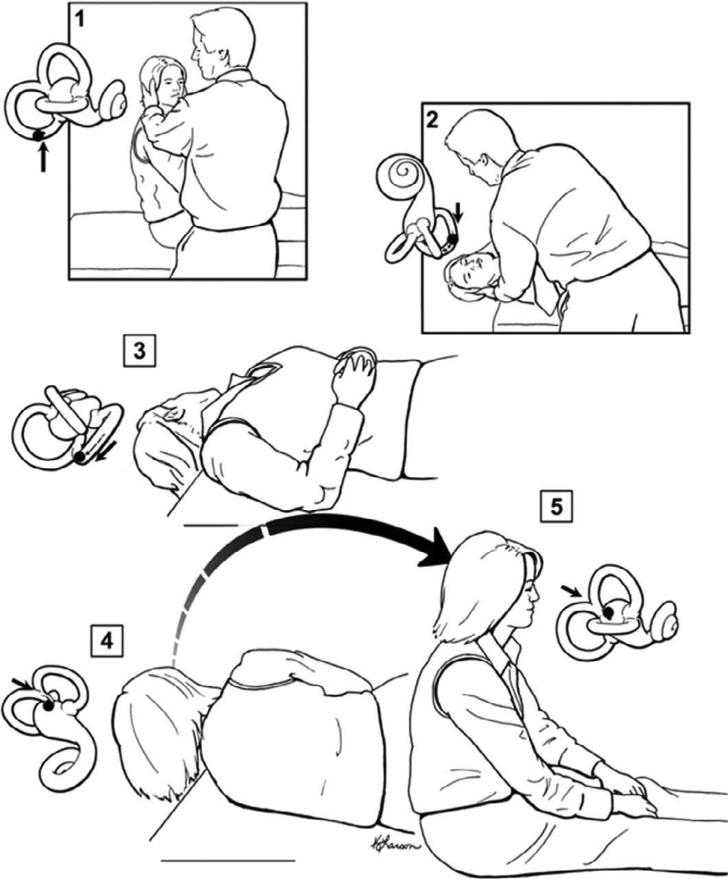
There are two effective particle repositioning methods for treatment of posterior canal BPPV: the Epley maneuver (37) (Figure 3) and the Semont maneuver (38) (Figure 4). Both are designed to move the endolymphatic debris from the posterior semicircular canal into the vestibule, where it does not cause vertigo. The Epley maneuver has been extensively studied and is recommended as the first-line treatment of posterior canal BPPV in guidelines from both the American Academy of Otolaryngology-Head and Neck Surgery and the American Academy of Neurology. (12,25)
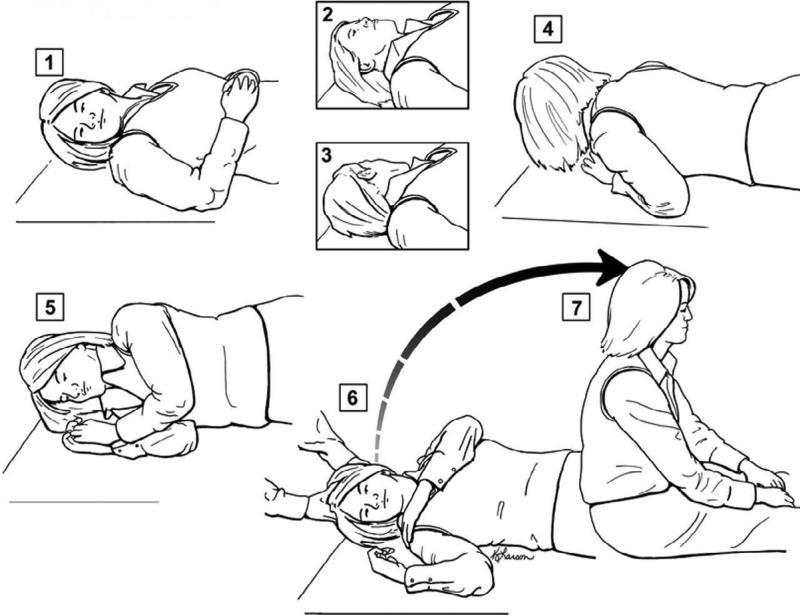
Figure 3.
The Epley maneuver for treatment of posterior canal BPPV [COMP, USE FULL PAGE WIDTH OR NEARLY FULL PAGE WIDTH FOR FIGURE 3]
Steps (1) and (2) of the Epley maneuver are the steps of a positive Dix-Hallpike test. After holding for 20 sec in position (2) the head is turned 90 degrees toward the unaffected side (3). After holding for 20 sec in position (3) the head is turned again 90 degrees in the same direction to a nearly face-down position with the body also turned to accommodate the head movement (4). After holding for 20 sec in position (4) the patient is brought to a sitting up position. The movement of the otolith material within the labyrinth is depicted with each step, showing how otoliths are moved from the semicircular canal to the vestibule. (Adapted from Fife et al. 2008 (25), used with permission)
Figure 4.
The Semont maneuver for treatment of posterior canal BPPV [COMP, USE FULL PAGE WIDTH OR NEARLY FULL PAGE WIDTH FOR FIGURE 4]
The patient begins by sitting upright (1). For a right posterior canal BPPV the patient's head is turned 45 degrees toward the left side, and then the patient is rapidly moved to the side-lying position as depicted in position (2). After holding for 30 sec in position (2) the patient is then moved quickly to the opposite side-lying position (3) without head turning or pausing in the middle. (Adapted from Fife et al. 2008 (25), used with permission)
A Cochrane systematic review (20) included 5 randomized control trials (15,39-42) of the Epley maneuver versus placebo, other active treatment or no treatment for a total of 292 adults diagnosed with posterior canal BPPV. Updated in 2010, the review excluded other RCTs with inadequate concealment of randomization or inadequate masking of outcome assessors. Outcome measures included resolution vertigo, and conversion of a positive Dix-Hallpike test to a negative Dix-Hallpike test. The pooled data showed a statistically significant effect in favor of the Epley maneuver over controls. An odds ratio of 4.2 (95% confidence interval, 2.0 to 9.1) was found in favor of treatment for resolution of vertigo. An odds ratio of 5.1 (95% confidence interval, 2.3 to 11.4) was found in favor of treatment for conversion of Dix-Hallpike test result.
In addition to the Cochrane review, five other meta-analyses also supported the effectiveness of the Epley maneuver for the treatment of posterior canal BPPV. (21,43-46) There were no serious adverse effects of treatment reported in clinical trials. Minor side effects such as nausea, vomiting, fainting, and conversion of posterior canal BPPV to BPPV involving other canals occurred in a 12% of treated patients. (25) The rate of canal switching after treatment of posterior canal BPPV has been reported in the range of 6-7%. (14,15)
Almost all RCTs of the Epley maneuver have been conducted in specialty clinics. The only RCT of the Epley maneuver conducted in primary care setting (42) did not show a statistically significant benefit for the Epley maneuver in term of symptom resolution and reported lower Dix-Hallpike conversion rate than other RCTs. (12) Whether the differences are due to differences in patient populations, reporting of symptoms or performance of the maneuver is not clear.
There are variations to the Epley maneuver (37) in clinical trials as well as in clinical practice. For example, several RCTs did not include mastoid vibration, which was originally recommended. (15,39-41) Some RCTs maintain upright posture and limit cervical motion after treatment (39,40) whereas other did not. (15,41) A meta-analysis showed postural restriction after Epley maneuver had no effect on outcome. (47) There were also differences in the number of Epley maneuver performed in the same visit ranging from one to five. Since the success rates among different RCTs overlap, it is likely that these variations have little effect on the end results. (20)
The Semont maneuver has not been as extensively studied as the Epley maneuver, but the available evidence also support its effectiveness in treatment of posterior canal BPPV. In one RCT involving 342 patients the Semont maneuver achieved resolution of vertigo in 79% and 87% of treated patients at 1 hour and 24 hours after treatment, respectively, whereas no sham maneuver-treated patient had resolution of vertigo at such times. (48) Other prospective studies also demonstrated the effectiveness of the Semont maneuver over sham maneuver (49), over no treatment (50), and over Brandt-Darroff exercises (51). There is no high-quality clinical trial comparing the Semont and Epley maneuvers.
Surgical treatment for posterior canal BPPV
In extreme circumstances, patients with intractable posterior canal BPPV, which shows no sign of spontaneous remission or response to repositioning maneuvers, may require or seek surgical treatment options. In one option the singular nerve which selectively supplies the posterior semicircular canal is identified and divided to prevent aberrant signal generated in the canal from reaching the CNS. (52,53) In another option, the posterior semicircular canal is exposed in the mastoid bone, fenestrated and occluded to prevent the canal from generating aberrant signal. (54)
Table 2 summarizes the outcome of six retrospective case series of singular nerve neurectomy. 96% of patients were completely cured of BPPV in the affected canal. 7% sustained various degrees of postoperative hearing loss greater than 10 dB pure tone average. In a limited number of patients in whom postoperative ENG/VNG were obtained 43% showed absent or reduced caloric response in the operated ear. Given that the caloric test measures response from the lateral semicircular canal whereas the surgery target the posterior semicircular canal, the reduced vestibular function suggest the occurrence of unintended surgical trauma or postoperative labyrinthitis. Several authors of the case series acknowledged that singular nerve neurectomy is a technically challenging operation.
Table 2.
Outcome of singular nerve section for BPPV
| Study | Cases | Cure of BPPV | Follow up | Postop Audio | ↓ Hearing > 10dB | Postop ENG/VNG | ↓ Caloric or absent |
|---|---|---|---|---|---|---|---|
| Epley 1980 (52) | 11 | 10 | 2-20 mo | 11 | 5 | 1? | 1 |
| Meyerhoff 1985 (69) | 18 | 15 | ≥ 6 mo | 18 | 3 | ? | ? |
| Silverstein 1990 (53) | 58 | 46 | 6 mo - 18 yr | 56 | 5 | 14 | |
| Fernandes 1993 (70) | 7 | 6 | ? | 7 | 2 | ? | |
| Gacek 2002 (71) | 252 | 244 | > 1 mo | 252 | 9 | ? | ? |
| Pournaras 2008 (72) | 8 | 8 | 1 mo - 9 yr | 8 | 1 | ? | ? |
| Total | 344 | 329/344 (95.6%) | 342/344 (99.4%) | 25/342 (7.3%) | 35/344 (13.9%) | 15/35 (42.9%) |
→ indicates that the relevant information was not reported. In the case of Epley 1980, one patient was reported to have severe vestibular loss post-operatively, but it was not specified how many patients had postoperative ENG/VNG.
Table 3 summarizes the outcome of retrospective case series of posterior semicircular canal occlusion showed resolution of BPPV in virtually all treated patients. 100% of patients were completely cured of BPPV in the affected canal. 7% sustained various degrees of postoperative hearing loss greater than 10 dB pure tone average The percentage of patients exhibiting reduced caloric response after surgery appears less with posterior canal occlusion (22%) than with singular nerve section, but remains a significant consideration. Overall, posterior canal occlusion appears to be a highly effective treatment option for intractable BPPV with some associated risks to hearing and vestibular function.
Table 3.
Outcome of posterior semicircular canal plugging for BPPV
| Study | Cases | Cure of BPPV | Follow up | Postop Audio | ↓ Hearing > 10dB | Postop ENG/VNG | ↓ Caloric or absent |
|---|---|---|---|---|---|---|---|
| PaceBalzan 1991 (73) | 5 | 5 | 12-36 mo | 5 | 1 | 5 | 3 |
| Hawthorne 1994 (74) | 15 | 15 | 14-40 mo | 15 | 1 | 8 | 3 |
| Zappia 1996 (75) | 8 | 8 | 3 wk- 3 mo | 8 | 0 | 1 | 0 |
| Pulec 1997 (76) | 17 | 17 | 1-13 mo | 17 | 0 | 17 | 0 |
| Walsh 1999 (77) | 13 | 13 | 29-119 mo | 13 | 13 | 2 | |
| Agrawal 2001 (78) | 44 | 44 | 6 mo - 12 yr | 40 | 2 | ? | ? |
| Shaia 2006 (79) | 20 | 20 | 6-64 mo | 20 | 1 | ? | ? |
| Kisilevsky 2009 (80) | 32 | 32 | 2-205 mo | 32 | 4 | 23 | 7 |
| Total | 154 | 154/154 (100%) | 150/154 (97.4%) | 10/150 (6.7%) | 67/154 (43.5%) | 15/67 (22.4%) |
↓ indicates that the relevant information was not reported.
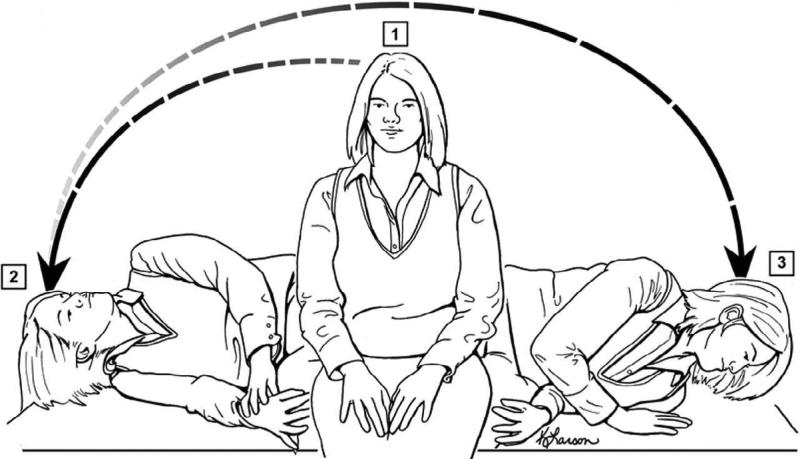
Repositioning maneuvers for lateral canal BPPV
There are three particle repositioning methods for treatment of lateral canal BPPV:
All three are designed to move the endolymphatic debris from the lateral semicircular canal into the vestibule, where it does not cause vertigo.
Figure 5.
The Lempert roll maneuver for treatment of lateral canal BPPV [COMP, USE FULL PAGE WIDTH OR NEARLY FULL PAGE WIDTH FOR FIGURE 5]
The patient begins by lying supine with head turned 45 degrees toward the affected side (1). The patient is then brought a series of step-wise 90-degree roll away from the affected side holding each position for 10 to 30 seconds. From position (5), the patient returns to lying supine (6) in preparation for the rapid and simultaneous movement from the supine face up to the sitting position. (Adapted from Fife et al. 2008 (25), used with permission)
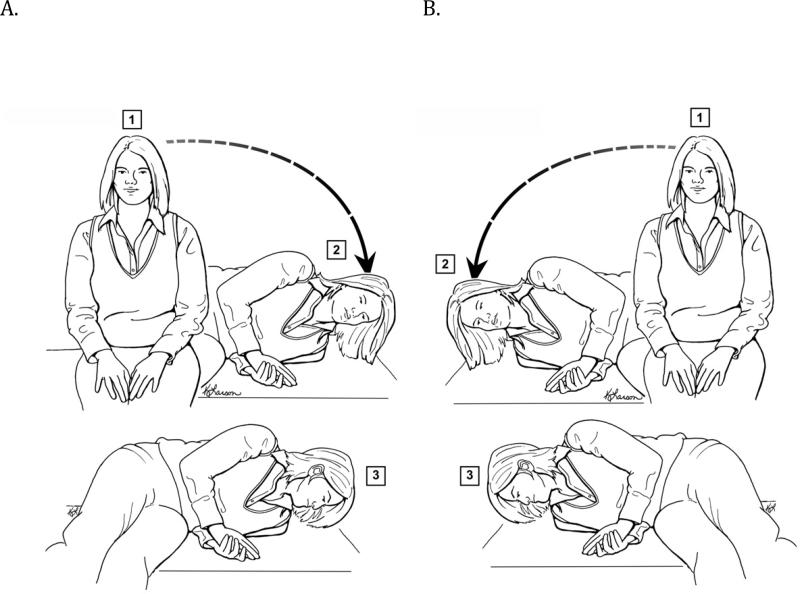
Figure 6.
The Gufoni maneuver for treatment of lateral canal BPPV [COMP, USE FULL PAGE WIDTH OR NEARLY FULL PAGE WIDTH FOR FIGURE 6]
A. For lateral canal BPPV with geotropic nystagmus, the patient is taken from the sitting position (Step 1) to the straight side lying position on the unaffected side (left in this case) for 1 minute. Then the patient's head is quickly turned toward the ground 45 to 60 degrees and held in position for 2 minutes. The patient then sits up again, with the head in the same position over the left shoulder.
B. For lateral canal BPPV with apogeotropic nystagmus, the patient is taken from the sitting position (Step 1) to the straight side lying position on the affected side (right in this case) for 1 minute. Then the patient's head is quickly turned toward the ground 45 to 60 degrees and held in position for 2 minutes. The patient then sits up again with the head in the same position over the right shoulder. (Adapted from Fife et al. 2008 (25), used with permission)
The Lempert roll and its variations appear to be the most commonly used techniques based on prospective cohorts and retrospective case series. (29,30,55,58-63) Success rates ranged from 50% for the apogeotropic variant to 100% for the geotropic variant although the endpoints differ widely among series and there was no appropriate untreated or sham-treated control.
Forced prolonged positioning with the affected ear up and the unaffected ear down can be performed either alone or following the Lempert roll. In case series (56,58,60,64,65) its success rates were 75 to 90%, but with the lack of control the prolonged end points can be difficult to distinguish from the relatively quick natural resolution of lateral canal BPPV.
The Gufoni maneuver is less well known, but it has garnered more support in recent literature. (57,66-68) A randomized controlled trial of 112 patients with geotropic variant of lateral canal BPPV compared Lempert roll plus forced prolonged position with Gufoni maneuver. The Gufoni maneuver was found to be statistically more successful than Lampert roll plus forced prolonged position after one treatment (86% vs 61%) (31)
BOTTOM LINE: WHAT DOES THE EVIDENCE TELL US?
BPPV is the most common diagnosis of vertigo in both primary care and subspecialty settings. A positive Dix-Hallpike maneuver is diagnostic for posterior canal BPPV. A positive supine roll test is diagnostic for lateral canal BPPV. Both Dix-Hallpike maneuver and supine roll test should be performed in the evaluation of vertigo or dizziness. Epley maneuver is the first-line treatment for posterior canal BPPV with Semont maneuver an alternative treatment. Posterior semicircular canal occlusion is an effective treatment for recalcitrant posterior canal BPPV, with some risks to hearing and vestibular function. Lateral canal BPPV can be treated with Lempert roll, forced prolonged positioning, or Gufoni maneuver although more controlled studies are needed to demonstrate efficacy of treatment since lateral canal BPPV has a quick natural course of remission.
The following points list the level of evidence as based on Oxford Centre for Evidence-Based Medicine.
BPPV is the most common diagnosis of vertigo (Level 4)
Dix-Hallpike maneuver is the diagnostic test for posterior canal BPPV (Level 1)
Supine roll test is the diagnostic test for lateral canal BPPV (Level 2)
Epley maneuver is the first-line treatment for posterior canal BPPV (Level 1)
Posterior semicircular canal occlusion is an effective treatment for recalcitrant posterior canal BPPV. (Level 4)
Lateral canal BPPV can be treated with a variety of repositioning maneuvers (Level 2)
Acknowledgements
The author would like to thank Louis Prahl for his assistance in the preparation of the manuscript.
This work was supported by grants KL2RR024141 and 5R33DC008632 from the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
OCEBM Levels of Evidence Working Group*. “The Oxford 2011 Levels of Evidence”. Oxford Centre for Evidence-Based Medicine. http://www.cebm.net/index.aspx?o=5653
OCEBM Levels of Evidence Working Group = Jeremy Howick, Iain Chalmers (James Lind Library), Paul Glasziou, Trish Greenhalgh, Carl Heneghan, Alessandro Liberati, Ivan Moschetti, Bob Phillips, Hazel Thornton, Olive Goddard and Mary Hodgkinson
References
- 1.Blakley BW, Goebel J. The meaning of the word “vertigo”. Otolaryngol Head Neck Surg. 2001;125:147–150. doi: 10.1067/mhn.2001.117869. [DOI] [PubMed] [Google Scholar]
- 2.Drachman DA, Hart CW. An approach to the dizzy patient. Neurology. 1972;22:323–334. doi: 10.1212/wnl.22.4.323. [DOI] [PubMed] [Google Scholar]
- 3.Kroenke K, Price RK. Symptoms in the community. Prevalence, classification, and psychiatric comorbidity. Arch Intern Med. 1993;153:2474–2480. [PubMed] [Google Scholar]
- 4.Yardley L, Owen N, Nazareth I, Luxon L. Prevalence and presentation of dizziness in a general practice community sample of working age people. Br J Gen Pract. 1998;48:1131–1135. [PMC free article] [PubMed] [Google Scholar]
- 5.Hannaford PC, Simpson JA, Bisset AF, Davis A, McKerrow W, Mills R. The prevalence of ear, nose and throat problems in the community: results from a national cross-sectional postal survey in Scotland. Fam Pract. 2005;22:227–233. doi: 10.1093/fampra/cmi004. [DOI] [PubMed] [Google Scholar]
- 6.Mendel B, Bergenius J, Langius-Eklöf A. Dizziness: A common, troublesome symptom but often treatable. J Vestib Res. 2010;20:391–398. doi: 10.3233/VES-2010-0370. [DOI] [PubMed] [Google Scholar]
- 7.Neuhauser HK, von Brevern M, Radtke A, et al. Epidemiology of vestibular vertigo: a neurotologic survey of the general population. Neurology. 2005;65:898–904. doi: 10.1212/01.wnl.0000175987.59991.3d. [DOI] [PubMed] [Google Scholar]
- 8.Sloane PD. Dizziness in primary care. Results from the National Ambulatory Medical Care Survey. J Fam Pract. 1989;29:33–38. [PubMed] [Google Scholar]
- 9.Kerber KA, Meurer WJ, West BT, Fendrick AM. Dizziness presentations in U.S. emergency departments, 1995-2004. Acad Emerg Med. 2008;15:744–750. doi: 10.1111/j.1553-2712.2008.00189.x. [DOI] [PubMed] [Google Scholar]
- 10.Hanley K, O'Dowd T. Symptoms of vertigo in general practice: a prospective study of diagnosis. Br J Gen Pract. 2002;52:809–812. [PMC free article] [PubMed] [Google Scholar]
- 11.Kentala E, Rauch SD. A practical assessment algorithm for diagnosis of dizziness. Otolaryngol Head Neck Surg. 2003;128:54–59. doi: 10.1067/mhn.2003.47. [DOI] [PubMed] [Google Scholar]
- 12.Bhattacharyya N, Baugh RF, Orvidas L, et al. Clinical practice guideline: benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2008;139:S47–S81. doi: 10.1016/j.otohns.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 13.Welling DB, Parnes LS, O'Brien B, Bakaletz LO, Brackmann DE, Hinojosa R. Particulate matter in the posterior semicircular canal. Laryngoscope. 1997;107:90–94. doi: 10.1097/00005537-199701000-00018. [DOI] [PubMed] [Google Scholar]
- 14.Herdman SJ, Tusa RJ. Complications of the canalith repositioning procedure. Arch Otolaryngol Head Neck Surg. 1996;122:281–286. doi: 10.1001/archotol.1996.01890150059011. [DOI] [PubMed] [Google Scholar]
- 15.Yimtae K, Srirompotong S, Srirompotong S, Sae-Seaw P. A randomized trial of the canalith repositioning procedure. Laryngoscope. 2003;113:828–832. doi: 10.1097/00005537-200305000-00011. [DOI] [PubMed] [Google Scholar]
- 16.von Brevern M, Radtke A, Lezius F, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry. 2007;78:710–715. doi: 10.1136/jnnp.2006.100420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cakir BO, Ercan I, Cakir ZA, Civelek S, Sayin I, Turgut S. What is the true incidence of horizontal semicircular canal benign paroxysmal positional vertigo? Otolaryngol Head Neck Surg. 2006;134:451–454. doi: 10.1016/j.otohns.2005.07.045. [DOI] [PubMed] [Google Scholar]
- 18.Tomaz A, Ganança MM, Ganança CF, Ganança FF, Caovilla HH, Harker L. Benign paroxysmal positional vertigo: concomitant involvement of different semicircular canals. Ann Otol Rhinol Laryngol. 2009;118:113–117. doi: 10.1177/000348940911800206. [DOI] [PubMed] [Google Scholar]
- 19.Dix MR, Hallpike CS. The pathology symptomatology and diagnosis of certain common disorders of the vestibular system. Proc R Soc Med. 1952;45:341–354. doi: 10.1177/003591575204500604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hilton M, Pinder D. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2004:CD003162. doi: 10.1002/14651858.CD003162.pub2. [DOI] [PubMed] [Google Scholar]
- 21.Teixeira LJ, Machado JN. Maneuvers for the treatment of benign positional paroxysmal vertigo: a systematic review. Braz J Otorhinolaryngol. 2006;72:130–139. doi: 10.1016/S1808-8694(15)30046-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Halker RB, Barrs DM, Wellik KE, Wingerchuk DM, Demaerschalk BM. Establishing a diagnosis of benign paroxysmal positional vertigo through the dix-hallpike and side-lying maneuvers: a critically appraised topic. Neurologist. 2008;14:201–204. doi: 10.1097/NRL.0b013e31816f2820. [DOI] [PubMed] [Google Scholar]
- 23.Norré ME. Diagnostic problems in patients with benign paroxysmal positional vertigo. Laryngoscope. 1994;104:1385–1388. doi: 10.1288/00005537-199411000-00012. [DOI] [PubMed] [Google Scholar]
- 24.Li JC, Li CJ, Epley J, Weinberg L. Cost-effective management of benign positional vertigo using canalith repositioning. Otolaryngol Head Neck Surg. 2000;122:334–339. doi: 10.1016/S0194-5998(00)70043-X. [DOI] [PubMed] [Google Scholar]
- 25.Fife TD, Iverson DJ, Lempert T, et al. Practice parameter: therapies for benign paroxysmal positional vertigo (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2008;70:2067–2074. doi: 10.1212/01.wnl.0000313378.77444.ac. [DOI] [PubMed] [Google Scholar]
- 26.McClure JA. Horizontal canal BPV. J Otolaryngol. 1985;14:30–35. [PubMed] [Google Scholar]
- 27.Pagnini P, Nuti D, Vannucchi P. Benign paroxysmal vertigo of the horizontal canal. ORL J Otorhinolaryngol Relat Spec. 1989;51:161–170. doi: 10.1159/000276052. [DOI] [PubMed] [Google Scholar]
- 28.Baloh RW, Jacobson K, Honrubia V. Horizontal semicircular canal variant of benign positional vertigo. Neurology. 1993;43:2542–2549. doi: 10.1212/wnl.43.12.2542. [DOI] [PubMed] [Google Scholar]
- 29.Nuti D, Agus G, Barbieri MT, Passali D. The management of horizontal-canal paroxysmal positional vertigo. Acta Otolaryngol. 1998;118:455–460. doi: 10.1080/00016489850154559. [DOI] [PubMed] [Google Scholar]
- 30.White JA, Coale KD, Catalano PJ, Oas JG. Diagnosis and management of lateral semicircular canal benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2005;133:278–284. doi: 10.1016/j.otohns.2005.03.080. [DOI] [PubMed] [Google Scholar]
- 31.Casani AP, Nacci A, Dallan I, Panicucci E, Gufoni M, Sellari-Franceschini S. Horizontal semicircular canal benign paroxysmal positional vertigo: effectiveness of two different methods of treatment. Audiol Neurootol. 2011;16:175–184. doi: 10.1159/000317113. [DOI] [PubMed] [Google Scholar]
- 32.Nakayama M, Epley JM. BPPV and variants: improved treatment results with automated, nystagmus-based repositioning. Otolaryngol Head Neck Surg. 2005;133:107–112. doi: 10.1016/j.otohns.2005.03.027. [DOI] [PubMed] [Google Scholar]
- 33.Cohen HS. Side-lying as an alternative to the Dix-Hallpike test of the posterior canal. Otol Neurotol. 2004;25:130–134. doi: 10.1097/00129492-200403000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Imai T, Ito M, Takeda N, et al. Natural course of the remission of vertigo in patients with benign paroxysmal positional vertigo. Neurology. 2005;64:920–921. doi: 10.1212/01.WNL.0000152890.00170.DA. [DOI] [PubMed] [Google Scholar]
- 35.Imai T, Takeda N, Ito M, Inohara H. Natural course of positional vertigo in patients with apogeotropic variant of horizontal canal benign paroxysmal positional vertigo. Auris Nasus Larynx. 2011;38:2–5. doi: 10.1016/j.anl.2010.05.011. [DOI] [PubMed] [Google Scholar]
- 36.Oghalai JS, Manolidis S, Barth JL, Stewart MG, Jenkins HA. Unrecognized benign paroxysmal positional vertigo in elderly patients. Otolaryngol Head Neck Surg. 2000;122:630–634. doi: 10.1016/S0194-5998(00)70187-2. [DOI] [PubMed] [Google Scholar]
- 37.Epley JM. The canalith repositioning procedure: for treatment of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 1992;107:399–404. doi: 10.1177/019459989210700310. [DOI] [PubMed] [Google Scholar]
- 38.Semont A, Freyss G, Vitte E. Curing the BPPV with a liberatory maneuver. Adv Otorhinolaryngol. 1988;42:290–293. doi: 10.1159/000416126. [DOI] [PubMed] [Google Scholar]
- 39.Lynn S, Pool A, Rose D, Brey R, Suman V. Randomized trial of the canalith repositioning procedure. Otolaryngol Head Neck Surg. 1995;113:712–720. doi: 10.1016/S0194-59989570010-2. [DOI] [PubMed] [Google Scholar]
- 40.Froehling DA, Bowen JM, Mohr DN, et al. The canalith repositioning procedure for the treatment of benign paroxysmal positional vertigo: a randomized controlled trial. Mayo Clin Proc. 2000;75:695–700. doi: 10.4065/75.7.695. [DOI] [PubMed] [Google Scholar]
- 41.von Brevern M, Seelig T, Radtke A, Tiel-Wilck K, Neuhauser H, Lempert T. Short-term efficacy of Epley's manoeuvre: a double-blind randomised trial. J Neurol Neurosurg Psychiatry. 2006;77:980–982. doi: 10.1136/jnnp.2005.085894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Munoz JE, Miklea JT, Howard M, Springate R, Kaczorowski J. Canalith repositioning maneuver for benign paroxysmal positional vertigo: randomized controlled trial in family practice. Can Fam Physician. 2007;53:1049–53, 1048. [PMC free article] [PubMed] [Google Scholar]
- 43.López-Escámez J, González-Sánchez M, Salinero J. [Meta-analysis of the treatment of benign paroxysmal positional vertigo by Epley and Semont maneuvers]. Acta Otorrinolaringol Esp. 1999;50:366–370. [PubMed] [Google Scholar]
- 44.Woodworth BA, Gillespie MB, Lambert PR. The canalith repositioning procedure for benign positional vertigo: a meta-analysis. Laryngoscope. 2004;114:1143–1146. doi: 10.1097/00005537-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 45.Prim-Espada MP, De Diego-Sastre JI, Pérez-Fernández E. [Meta-analysis on the efficacy of Epley's manoeuvre in benign paroxysmal positional vertigo]. Neurologia. 2010;25:295–299. [PubMed] [Google Scholar]
- 46.Helminski JO, Zee DS, Janssen I, Hain TC. Effectiveness of particle repositioning maneuvers in the treatment of benign paroxysmal positional vertigo: a systematic review. Phys Ther. 2010;90:663–678. doi: 10.2522/ptj.20090071. [DOI] [PubMed] [Google Scholar]
- 47.Devaiah AK, Andreoli S. Postmaneuver restrictions in benign paroxysmal positional vertigo: an individual patient data meta-analysis. Otolaryngol Head Neck Surg. 2010;142:155–159. doi: 10.1016/j.otohns.2009.09.013. [DOI] [PubMed] [Google Scholar]
- 48.Mandalà M, Santoro GP, Asprella Libonati G, et al. Double-blind randomized trial on short-term efficacy of the Semont maneuver for the treatment of posterior canal benign paroxysmal positional vertigo. J Neurol. 2011 doi: 10.1007/s00415-011-6272-x. [DOI] [PubMed] [Google Scholar]
- 49.Cohen HS, Kimball KT. Effectiveness of treatments for benign paroxysmal positional vertigo of the posterior canal. Otol Neurotol. 2005;26:1034–1040. doi: 10.1097/01.mao.0000185044.31276.59. [DOI] [PubMed] [Google Scholar]
- 50.Salvinelli F, Casale M, Trivelli M, et al. Benign paroxysmal positional vertigo: a comparative prospective study on the efficacy of Semont's maneuver and no treatment strategy. Clin Ter. 2003;154:7–11. [PubMed] [Google Scholar]
- 51.Soto Varela A, Bartual Magro J, Santos Pérez S, et al. Benign paroxysmal vertigo: a comparative prospective study of the efficacy of Brandt and Daroff exercises, Semont and Epley maneuver. Rev Laryngol Otol Rhinol (Bord) 2001;122:179–183. [PubMed] [Google Scholar]
- 52.Epley JM. Singular neurectomy: hypotympanotomy approach. Otolaryngol Head Neck Surg. 1980;88:304–309. doi: 10.1177/019459988008800320. [DOI] [PubMed] [Google Scholar]
- 53.Silverstein H, White DW. Wide surgical exposure for singular neurectomy in the treatment of benign positional vertigo. Laryngoscope. 1990;100:701–706. doi: 10.1288/00005537-199007000-00005. [DOI] [PubMed] [Google Scholar]
- 54.Parnes LS, McClure JA. Posterior semicircular canal occlusion in the normal hearing ear. Otolaryngol Head Neck Surg. 1991;104:52–57. doi: 10.1177/019459989110400111. [DOI] [PubMed] [Google Scholar]
- 55.Lempert T, Tiel-Wilck K. A positional maneuver for treatment of horizontal-canal benign positional vertigo. Laryngoscope. 1996;106:476–478. doi: 10.1097/00005537-199604000-00015. [DOI] [PubMed] [Google Scholar]
- 56.Vannucchi P, Giannoni B, Pagnini P. Treatment of horizontal semicircular canal benign paroxysmal positional vertigo. J Vestib Res. 1997;7:1–6. [PubMed] [Google Scholar]
- 57.Gufoni M, Mastrosimone L, Di Nasso F. [Repositioning maneuver in benign paroxysmal vertigo of horizontal semicircular canal]. Acta Otorhinolaryngol Ital. 1998;18:363–367. [PubMed] [Google Scholar]
- 58.Appiani GC, Gagliardi M, Magliulo G. Physical treatment of horizontal canal benign positional vertigo. Eur Arch Otorhinolaryngol. 1997;254:326–328. doi: 10.1007/BF02630724. [DOI] [PubMed] [Google Scholar]
- 59.Fife TD. Recognition and management of horizontal canal benign positional vertigo. Am J Otol. 1998;19:345–351. [PubMed] [Google Scholar]
- 60.Casani AP, Vannucci G, Fattori B, Berrettini S. The treatment of horizontal canal positional vertigo: our experience in 66 cases. Laryngoscope. 2002;112:172–178. doi: 10.1097/00005537-200201000-00030. [DOI] [PubMed] [Google Scholar]
- 61.Tirelli G, Russolo M. 360-Degree canalith repositioning procedure for the horizontal canal. Otolaryngol Head Neck Surg. 2004;131:740–746. doi: 10.1016/j.otohns.2004.01.021. [DOI] [PubMed] [Google Scholar]
- 62.Prokopakis EP, Chimona T, Tsagournisakis M, et al. Benign paroxysmal positional vertigo: 10-year experience in treating 592 patients with canalith repositioning procedure. Laryngoscope. 2005;115:1667–1671. doi: 10.1097/01.mlg.0000175062.36144.b9. [DOI] [PubMed] [Google Scholar]
- 63.Escher A, Ruffieux C, Maire R. Efficacy of the barbecue manoeuvre in benign paroxysmal vertigo of the horizontal canal. Eur Arch Otorhinolaryngol. 2007;264:1239–1241. doi: 10.1007/s00405-007-0337-6. [DOI] [PubMed] [Google Scholar]
- 64.Chiou WY, Lee HL, Tsai SC, Yu TH, Lee XX. A single therapy for all subtypes of horizontal canal positional vertigo. Laryngoscope. 2005;115:1432–1435. doi: 10.1097/01.mlg.0000168092.91251.d3. [DOI] [PubMed] [Google Scholar]
- 65.Boleas-Aguirre MS, Pérez N, Batuecas-Caletrío A. Bedside therapeutic experiences with horizontal canal benign paroxysmal positional vertigo (cupulolithiasis). Acta Otolaryngol. 2009;129:1217–1221. doi: 10.3109/00016480802631958. [DOI] [PubMed] [Google Scholar]
- 66.Asprella Libonati G. Diagnostic and treatment strategy of lateral semicircular canal canalolithiasis. Acta Otorhinolaryngol Ital. 2005;25:277–283. [PMC free article] [PubMed] [Google Scholar]
- 67.Appiani GC, Catania G, Gagliardi M, Cuiuli G. Repositioning maneuver for the treatment of the apogeotropic variant of horizontal canal benign paroxysmal positional vertigo. Otol Neurotol. 2005;26:257–260. doi: 10.1097/00129492-200503000-00022. [DOI] [PubMed] [Google Scholar]
- 68.Riggio F, Francesco R, Dispenza F, et al. Management of benign paroxysmal positional vertigo of lateral semicircular canal by Gufoni's manoeuvre. Am J Otolaryngol. 2009;30:106–111. doi: 10.1016/j.amjoto.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 69.Meyerhoff WL. Surgical section of the posterior ampullary nerve. Laryngoscope. 1985;95:933–935. doi: 10.1288/00005537-198508000-00009. [DOI] [PubMed] [Google Scholar]
- 70.Fernandes CM. Singular neurectomy in South African practice. S Afr J Surg. 1993;31:79–80. [PubMed] [Google Scholar]
- 71.Gacek RR, Gacek MR. Results of singular neurectomy in the posterior ampullary recess. ORL J Otorhinolaryngol Relat Spec. 2002;64:397–402. doi: 10.1159/000067572. [DOI] [PubMed] [Google Scholar]
- 72.Pournaras I, Kos I, Guyot JP. Benign paroxysmal positional vertigo: a series of eight singular neurectomies. Acta Otolaryngol. 2008;128:5–8. doi: 10.1080/00016480701275279. [DOI] [PubMed] [Google Scholar]
- 73.Pace-Balzan A, Rutka JA. Non-ampullary plugging of the posterior semicircular canal for benign paroxysmal positional vertigo. J Laryngol Otol. 1991;105:901–906. doi: 10.1017/s0022215100117785. [DOI] [PubMed] [Google Scholar]
- 74.Hawthorne M, el-Naggar M. Fenestration and occlusion of posterior semicircular canal for patients with intractable benign paroxysmal positional vertigo. J Laryngol Otol. 1994;108:935–939. doi: 10.1017/s0022215100128579. [DOI] [PubMed] [Google Scholar]
- 75.Zappia JJ. Posterior semicircular canal occlusion for benign paroxysmal positional vertigo. Am J Otol. 1996;17:749–754. [PubMed] [Google Scholar]
- 76.Pulec JL. Ablation of posterior semicircular canal for benign paroxysmal positional vertigo. Ear Nose Throat J. 1997;76:17–22, 24. [PubMed] [Google Scholar]
- 77.Walsh RM, Bath AP, Cullen JR, Rutka JA. Long-term results of posterior semicircular canal occlusion for intractable benign paroxysmal positional vertigo. Clin Otolaryngol Allied Sci. 1999;24:316–323. doi: 10.1046/j.1365-2273.1999.00266.x. [DOI] [PubMed] [Google Scholar]
- 78.Agrawal SK, Parnes LS. Human experience with canal plugging. Ann N Y Acad Sci. 2001;942:300–305. doi: 10.1111/j.1749-6632.2001.tb03754.x. [DOI] [PubMed] [Google Scholar]
- 79.Shaia WT, Zappia JJ, Bojrab DI, LaRouere ML, Sargent EW, Diaz RC. Success of posterior semicircular canal occlusion and application of the dizziness handicap inventory. Otolaryngol Head Neck Surg. 2006;134:424–430. doi: 10.1016/j.otohns.2005.10.035. [DOI] [PubMed] [Google Scholar]
- 80.Kisilevsky V, Bailie NA, Dutt SN, Rutka JA. Lessons learned from the surgical management of benign paroxysmal positional vertigo: the University Health Network experience with posterior semicircular canal occlusion surgery (1988-2006). J Otolaryngol Head Neck Surg. 2009;38:212–221. [PubMed] [Google Scholar]