Abstract
Context:
Femoroacetabular impingement (FAI) is a common cause of hip pathology and secondary dysfunction among athletes. Much information has been gained regarding the cause and pathomechanics of this disorder. Now, efforts are focusing on treatment to restore the joint and reduce the secondary damage that causes painful dysfunction.
Evidence Acquisition:
This article reviews the scientific literature in reference to treatment of FAI in athletes.
Results:
Several studies reported reasonably successful outcomes in the arthroscopic management of FAI in athletes, and 1 study reported on open surgical correction of this disorder. Few major complications have been described.
Conclusions:
When the diagnosis is given early, some athletes may benefit from a rehabilitation strategy that includes training modifications to protect the at-risk hip. When indicated, arthroscopic surgery can address the joint damage and correct the underlying impingement. Although the joint may not be normal, successful results with return to sports can often be expected.
Keywords: femoroacetabular impingement, athletes, hip arthroscopy, etiology, assessment
Femoroacetabular impingement (FAI) may exist as an incidental asymptomatic finding. It is unclear what portion of asymptomatic athletes will eventually develop progressive secondary joint damage. However, many athletes have significant grade III and grade IV articular lesions at the time of arthroscopic intervention, suggesting that secondary damage occurs by the time the clinical circumstances are sufficient to recommend surgery. Thus, a cautious watchful approach is important, even with the mildest symptoms associated with FAI. Progressively worsening symptoms necessitate a proactive approach in the treatment strategy.
Prevention
There are currently no formal prevention programs for FAI. For athletes who develop symptoms from intra-articular pathology, the causal relationship of the underlying impingement and the importance of its correction are well understood.6 However, some athletes have abnormally shaped hips (impingement morphology) that do not necessarily develop secondary joint damage (impingement pathology). Thus, the value or efficacy of preventative programs is uncertain until there are good demographic data to understand the risk of impingement morphology causing impingement pathology. Nonetheless, a current sense of awareness is important.
Better programs are needed to screen for underlying impingement as evidenced by reduced internal rotation. Radiographs may be appropriate for those deemed at risk. It is difficult to recommend substantial alterations in activity for an asymptomatic athlete; however, providing an early warning for any future symptoms can be part of conservative treatment.
Conservative Treatment
Conservative treatment begins with an emphasis on early recognition. Pain in an athlete with FAI should be taken as a worrisome warning sign of progressive damage within the joint. Many athletes demonstrate high pain tolerance, sometimes to the point of true insensitivity to pain, and the damage to the joint can be severe, even in individuals who continue to function at a high level. Thus, although it may not be appropriate to intercede in someone who is asymptomatic, it should not be a matter of simply waiting to see how severe the symptoms become. If mild symptoms are stable, a trial of conservative management is certainly reasonable.
The mainstay of treatment lies in identifying and modifying offending activities that precipitate symptoms. Efforts are made to optimize mobility of the joint, but these are only modestly effective because motion is limited by the bony architecture, which cannot be corrected by manual techniques. Decompensatory disorders may develop as an athlete struggles to compensate for the chronic limitations imposed by the impingement. Optimizing core strength can aid the athlete’s ability to compensate.
Squats, long a mainstay of most weight programs, are especially deleterious to a hip at risk. A normal joint may tolerate these well, but with impingement, these can cause or perpetuate problems. Squats can often be completely eliminated because few sporting activities necessitate them as a functional training tool. They can also be modified by limiting hip flexion to 45° to protect the joint from the forces encountered with greater amounts of flexion.
Surgical Treatment
Surgical intervention is indicated in symptomatic cases with imaging evidence of joint damage secondary to impingement (JWT Byrd and KS Jones, unpublished data, 2010). Imaging studies do not often detail the severity of the damage. Surgical intervention is often recommended for impingement that is recalcitrant or progressive and unresponsive to conservative measures.
Arthroscopic Technique
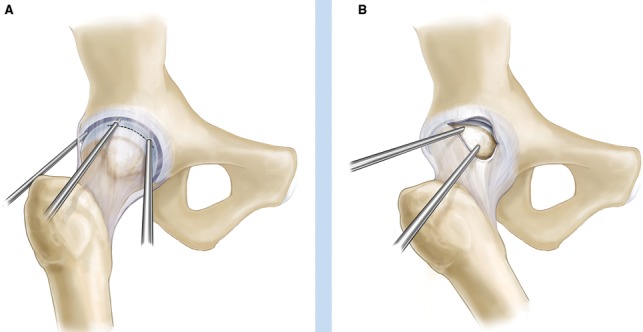
Arthroscopic management of FAI begins with the central compartment. The patient is positioned supine with traction applied, and 3 standard portals provide optimal access for surveying and accessing intra-articular pathology (Figure 1).2-4
Figure 1.
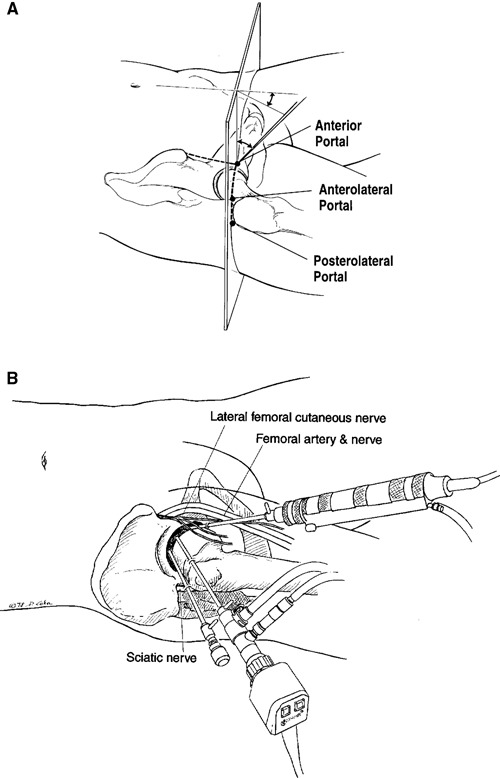
A, the anterior portal coincides with the intersection of a sagittal line drawn distally from the anterior superior iliac spine and a transverse line across the superior margin of the greater trochanter. The portal courses approximately 45° cephalad and 30° toward the midline. The anterolateral and posterolateral portals are positioned directly over the superior aspect of the trochanter at the anterior and posterior borders. B, the femoral artery and nerve lie well medial to the anterior portal. The sciatic nerve lies posterior to the posterolateral portal. The lateral femoral cutaneous nerve lies close to the anterior portal.
Pincer Assessment
There are 3 arthroscopic parameters of pincer impingement: anterior labral pathology; a bony prominence of the anterolateral acetabulum, which may make positioning of the anterior portal difficult despite adequate distraction; and bone overhanging the labrum where a capsular reflection should be.
By middle age, labral degeneration is often extensive and best managed with simple debridement.5 Debridement of the deteriorated portion of the labrum exposes the abnormal overhanging bone, which can be shaped to eliminate the pincer lesion (Figure 2). The labrum may not be salvaged, but recontouring the acetabulum opens the joint and may substantially improve mobility and symptoms.5
Figure 2.
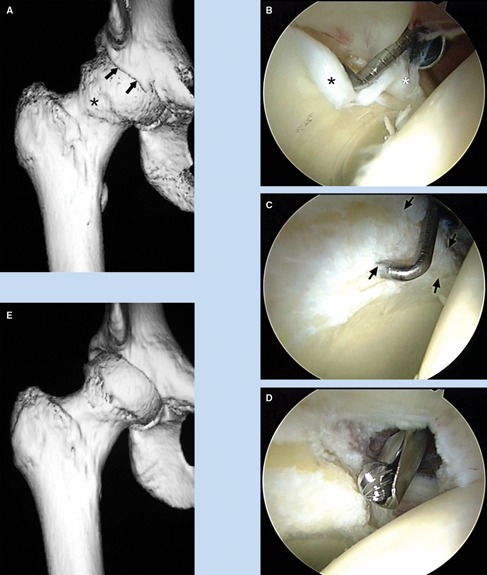
A 38-year-old woman with progressive pain and loss of motion of the right hip. A, 3-dimensional computed tomography scan illustrates pincer impingement (arrows) and a kissing lesion characterized by osteophyte formation on the femoral head (asterisk). B, as viewed from the anterolateral portal, there is maceration of the anterior labrum (white asterisk) and associated articular delamination (black asterisk). C, debridement of the degenerate labrum exposes the pincer lesion (arrows). D, the pincer lesion is recontoured with a burr. E, a postoperative 3-dimensional computed tomography scan demonstrates the extent of bony recontouring of the acetabulum and the femoral head.
With good labral tissue, preservation is preferred.7 Sometimes the bony lesion can be exposed on the capsular side of the labrum and recontoured without compromising the labrum’s structural integrity. More often, when the labrum is failing owing to pincer impingement but is still good tissue, it can be mobilized to correct the pincer lesion and then refixed (Figure 3). The labrum can be sharply dissected from the overlying bone to expose the pincer lesion. The acetabulum can then be recontoured with a high-speed burr, taking care to preserve the mobilized labrum, which can then be refixed with suture anchors. Anchor placement usually requires a more distal entry site to ensure divergence from the joint while avoiding perforation of the articular surface.
Figure 3.
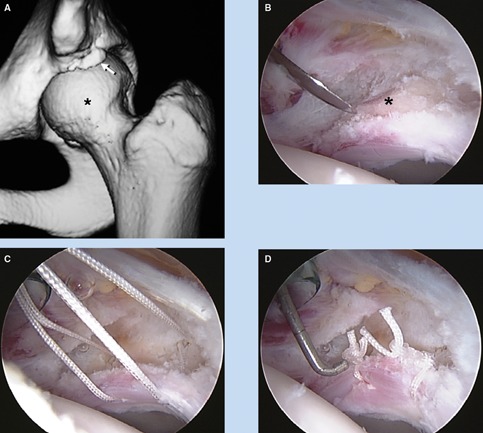
A 15-year-old female gymnast with pain and reduced internal rotation of the left hip. A, a 3-dimensional computed tomography scan defines a pincer lesion with accompanying os acetabulum (arrow) and cam lesion (asterisk). B, as viewed from the anterolateral portal, the pincer lesion and os acetabulum (asterisk) are exposed, with the labrum being sharply released with an arthroscopic knife. C, the acetabular fragment has been removed and the rim trimmed with anchors placed to repair the labrum. D, the labrum has been refixed.
Management of cam impingement also begins with arthroscopy of the central compartment, to assess the articular cartilage of the anterolateral acetabulum for pathological cam impingement (Figure 4). After the intra-articular damage is addressed, attention can turn to the cam lesion in the peripheral compartment.
Figure 4.
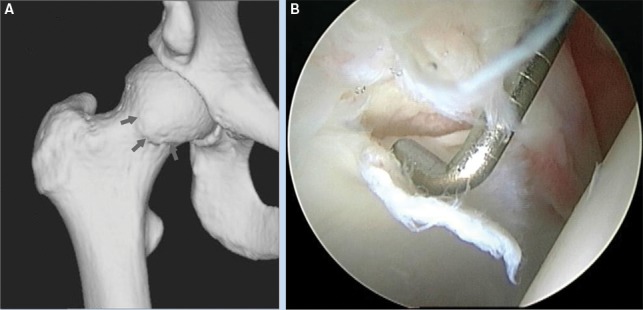
A 20-year-old hockey player with a 4-year history of right hip pain. A, a 3-dimensional computed tomography scan defines the cam lesion (arrows). B, as viewed from the anterolateral portal, the probe introduced anteriorly displaces an area of articular delamination from the anterolateral acetabulum characteristic of the peel-back phenomenon created by the bony lesion shearing the articular surface during hip flexion.
A capsular window can be created by connecting the anterior and anterolateral portals. When these 2 portals are maintained just outside the joint and traction is released with the hip slightly flexed, the cam lesion becomes visible within the peripheral compartment (Figure 5). Further capsular dissection can fully expose the abnormal bone; a proximal anterolateral portal improves access. After the lesion is fully defined, the overlying fibrous and fibrocartilaginous tissue is removed. The bone is reshaped, re-creating a more normal concave relationship at the junction of the articular surface, eliminating the cam lesion (Figure 6). The lateral retinacular vessels should be identified and protected.
Figure 5.
A, a capsulotomy performed by connecting the anterior and anterolateral portals is necessary for the instruments to pass freely from the central to peripheral compartment as the traction is released and the hip flexed. B, with the hip flexed, the anterolateral portal is now positioned along the neck of the femur. A cephalad (proximal) anterolateral portal has been placed, and the original anterior and posterolateral portals have been removed. These 2 portals allow access to the entirety of the cam lesion in most cases. Their position also allows an unhindered view with the c-arm.
Figure 6.
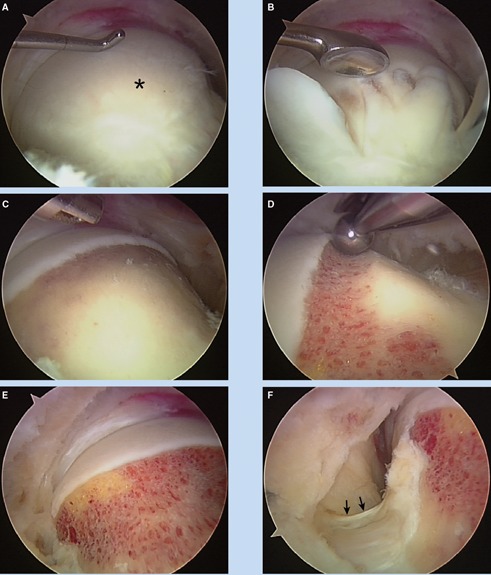
View from the periphery. A, a cam lesion covered with fibrocartilage (asterisk). B, an arthroscopic curette used to denude the abnormal bone. C, excision area is fully exposed. D, bony resection at the articular margin. E, the completed recontouring. F, lateral view on the base of the neck; the lateral retinacular vessels identified (arrows) and preserved.
Postoperative Rehabilitation
The recovery strategy depends on the extent of pathology and the subsequent procedure. For simple labral debridement and recontouring of the acetabular rim, the athlete can bear weight as tolerated with an emphasis on range of motion and joint stabilization. If the labrum is refixed, then the repair site should be protected during the early healing phase by protected weightbearing and by avoiding extremes of flexion and external rotation for the first 4 to 6 weeks.
Reshaping of the femoral head-neck junction requires caution. Fracture of the femoral neck is an unlikely but potentially serious complication.9 The athlete is allowed to bear full weight, but he or she needs to use crutches to avoid twisting movements during the first 4 weeks. Once full motor control has been regained, light activities are allowed, such as closed chain and low impact exercise. Full bony remodeling takes 3 months, during which time high-impact and/or torsional forces should be avoided. If microfracture is performed, the athlete is kept partial weightbearing for 2 months to optimize the early maturation of the fibrocartilaginous healing response. During this time, gentle range of motion is emphasized to stimulate the healing process.
At 3 months, twisting and impact precautions are lifted, and functional progression is allowed. The speed with which the athlete advances is variable and may require another 1 to 3 months for full return. Athletes are generally advised that return to sports following surgical correction of FAI can take 4 to 6 months.
Results
From a cohort of 172 FAI cases in athletes with 1-year follow-up, the average improvement was 22 points (preoperative, 71; postoperative 93). There were 141 cam, 22 combined, and 9 pincer lesions among 19 professional, 51 intercollegiate, and 102 high school or recreational athletes. Athletes with cam impingement averaged 29 years of age with a man:woman ratio of 2.7:1.0; athletes with pincer impingement averaged 33 years of age with a 1.2:1.0 ratio. In sum, 89% of professional athletes and 90% of intercollegiate athletes were able to return to their previous level of competition.
Philippon et al reported on 45 professional athletes who underwent arthroscopic management of FAI with an average follow-up of 1.6 years.8 Overall, 42 (93%) resumed their sport, although that number declined to 35 (78%) over the follow-up period. These results are still favorable to the only other report of FAI correction in athletes. Bizzini et al found that 3 of 5 professional hockey players (60%) were able to resume their previous level of competition when treated with open surgery.1
Conclusions
FAI is a common cause of joint damage among athletes. Recognition of this entity and the development of arthroscopic techniques to address it have allowed many athletes to resume their athletic careers. Surgical intervention can never restore a joint to normal. The emphasis should remain on early recognition of injury and prevention of degeneration.
Footnotes
One or more authors has declared a potential conflict of interest: J. W. Thomas Byrd is a consultant for Smith & Nephew and A2 Surgical and has received research funding from Smith & Nephew.
References
- 1. Bizzini M, Notzli HIP, Maffiuletti NA. Femoroacetabular impingement in professional ice hockey players. a case series of five athletes after open surgical decompression of the hip. Am J Sports Med. 2007;35:1955. [DOI] [PubMed] [Google Scholar]
- 2. Byrd JWT. Hip arthroscopy by the supine approach. Instr Course Lect. 2006;55:325-336 [PubMed] [Google Scholar]
- 3. Byrd JWT. Hip arthroscopy utilizing the supine position. Arthroscopy. 1994;10:275-280 [DOI] [PubMed] [Google Scholar]
- 4. Byrd JWT. The supine approach. In: Byrd JWT, ed. Operative Hip Arthroscopy. 2nd ed. New York, NY: Springer; 2005:145-169 [Google Scholar]
- 5. Byrd JWT, Jones KS. Arthroscopic management of femoroacetabular impingement. Instr Course Lect. 2009;58:231-239 [PubMed] [Google Scholar]
- 6. Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Rel Res. 2003:417;112-120 [DOI] [PubMed] [Google Scholar]
- 7. Larson CM, Giveans MR. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25:369-376 [DOI] [PubMed] [Google Scholar]
- 8. Philippon M, Schenker M, Briggs K, Kuppersmith D. Femoroacetabular impingement in 45 professional athletes: associated pathologies and return to sport following arthroscopic decompression. Knee Surg Sports Traumatol Arthrosc. 2007;15:908-914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sampson T. Arthroscopic treatment of femoroacetabular impingement. Am J Orthop. 2008;37:608-612 [PubMed] [Google Scholar]


