Abstract
Background:
The objective of this study is to assess the effectiveness of extracorporeal shock wave therapy in the management of calcifying tendinitis of the shoulder. Furthermore, a dose-response relationship was sought as a secondary confirmation of effectiveness.
Hypothesis:
Focused extracorporeal shock wave therapy has a high, dose-responsive effectiveness in the management of calcifying tendinitis of the shoulder.
Study Design:
Meta-analysis.
Methods:
Studies were identified from online databases (MEDLINE, EMBASE, and Cochrane Controlled Trials Register), manual searches, and personal communication with experts in the field. After assessment of heterogeneity, a random effects model was generated. The primary end points were identified as pain and function by using the visual analog scale and the Constant-Murley Score, respectively. These end points were pooled and the weighted mean differences and 95% confidence intervals were estimated. Odds ratios of the secondary end point deposit resorption were pooled.
Results:
In 14 studies, shock wave therapy led to a significantly higher reduction of pain (weighted mean difference, −2.8 points; 95% confidence interval, −4.2 to −1.5 points) and improvement of function (weighted mean difference, 19.8 points; 95% confidence interval, 13.4-26.3 points), compared to other treatments and placebo. High-energy treatment produced significantly better results than low-energy treatment for pain reduction (weighted mean difference, 1.7 points; 95% confidence interval, 0.7-2.6 points) and improvement of function (weighted mean difference, 10.7 points; 95% confidence interval, 7.2-14.1 points). These results are consistent with a dose-response relationship supporting the effectiveness of shock wave therapy.
Conclusion:
Shock wave therapy for calcifying tendinitis of the shoulder is effective in pain relief, function restoration, and deposit resorption; however, these conclusions are susceptible to bias arising from the limitations of the included studies.
Keywords: extracorporeal shock wave therapy, calcifying tendinitis, meta-analysis
Calcifying tendinitis is a fairly common cause of shoulder pain. Estimates of the incidence rate of this disease range from 2.5% to 20%.8 Its course may be self-limiting, but protracted suffering is not uncommon. Management usually is conservative, including subacromial injections, nonsteroidal anti-inflammatory drugs, and physical therapy.8 Chronic and recalcitrant cases might need surgical treatment.12,19,23 Calcifying tendinitis of the shoulder is also frequently treated with extracorporeal shock wave therapy. The exact mechanisms of action are still elusive, but clinical results have been reassuring. There are a vast number of trials reporting on cohorts of patients undergoing this procedure; however, only a few controlled trials tested the effectiveness and safety of this procedure and its application is still somewhat controversial.
The primary objective of this study was to assess the effectiveness of shock wave therapy in calcifying tendinitis of the shoulder in comparison with a placebo or other treatments. The secondary research question was whether there is a dose-response relationship for high-energy versus low-energy shock wave therapy.
Methods
This study was performed in accordance with the Quality of Reporting of Meta-Analysis (QUOROM) Statement and the Consolidated Standards of Reporting Trails (CONSORT) Statement (www.consort-statement.org).14
The online databases MEDLINE, EMBASE, and the Cochrane Controlled Trials Register (CCTR) were searched without restrictions in language or publication date. The search string was “shoulder,” “wave,” and “tendinitis” or “tendinosis” or “tendonitis” or “tendonosis.” These terms were used as exploded keywords and medical subject headings (MeSH terms) where possible. Results were filtered for controlled trials using validated and highly sensitive strategies.20,24 Identified studies were obtained and reviewed by 2 investigators (P.V. and J.H.) for inclusion. The references of included studies, as well as the “related article” function in PubMed, were used to search for additional studies. The authors also searched relevant journals by hand and interviewed experts in the field to identify additional papers. The last search was performed in July 2008.
Study Selection
We included peer-reviewed articles reporting on controlled trials of shock wave therapy in the management of calcifying tendinitis of the shoulder. The diagnosis of calcifying tendinitis had to be confirmed clinically and radiologically. The cutoff for high-energy and low-energy shock wave was set at 0.2 mJ/mm2.
Trials comparing shock wave therapy with other treatments or sham treatment were included to answer this study’s primary question. Articles comparing shock wave therapy of different energy levels were included for the study’s secondary question. The internal validity of studies was classified using the Jadad scale.10 This score attributes 0 to 2 points for randomization and blinding and 0 or 1 point for description of attrition.
Data Extraction and Analysis
Data extraction was duplicated independently by 2 investigators (P.V. and J.H.), using digital spreadsheets for the end points: reduction in pain, improvement of function, and deposit resorption. All end points were abstracted at, or as close as possible to, 6 months of follow-up. In case of incomplete description of study results, numbers were taken from graphs or the authors were contacted for clarification. After completion, these spreadsheets were cross-checked for mistakes and disagreement. Disagreement was resolved by consensus or this study’s senior author (R.D.) was consulted.
Data were analyzed separately concerning the 2 study questions. Study heterogeneity was assessed using the Q test and quantified by the I2 index. The Q test is a statistical method to test whether the individual study results are within a pooled estimate of all results (ie, are homogenous and all differences are due to random chance) or if they derive from a distribution around these pooled results (ie, are heterogeneous). This test depends on sample size, thus the threshold of significance was set at P ≤ .1 to account for the test’s low power in small samples. In contrast to the sample-dependent, sizeless “yes/no” answer from the Q test, the I2 index gives a percent value of difference between studies beyond differences due to random chance. This percent value allows an investigator to judge the clinical importance of differences. To study possible sources of heterogeneity, subgroup analyses were done for high-energy and low-energy treatment and for different control groups (sham vs other treatment). Additionally, variables describing the studied populations (age and gender distribution), the provided treatment (absolute high-energy level, absolute low-energy level, ratio of energy levels, ratio of total energy administered, difference in energy levels, difference in total energy administered), and the precision of study estimates (standard errors of effect sizes) were tested for their association with absolute treatment effect and treatment effect size using forward stepwise multivariate meta-regression models, which apply multivariate regression to pooled estimates from meta-analyses to assess their role in between-study heterogeneity.
Data were pooled using the Cochrane Collaboration’s Review Manager (RevMan 4.2, Nordic Cochrane Centre, Copenhagen, Denmark). Weighted mean differences (WMDs) and 95% confidence intervals (CIs) were calculated to pool continuous estimates for the end points. Weighted mean differences are the mean difference from all included studies multiplied by a parameter of the precision of the estimate of the individual studies. In this case, the inverse variance was used to account for differences in study size and precision of outcome assessment. Pooling was done using the DerSimonian-Laird random effects method, which is based on the assumption that the outcomes in the included studies are distributed around a common overall effect.5 Such models assume that the estimates of the individual studies are normally distributed around the pooled effect and can thus compensate for heterogeneity. For the binary outcome complete deposit resorption, the pooled odds ratio with 95% CI was calculated. Because in some groups there was no patient with complete resorption, 1 patient was added to all groups to allow for calculation of odds. Intercooled Stata 10 (StataCorp LP, College Station, Texas) was used to build regression models. An alpha level of 5% was considered significant.
Results
Fourteen studies were included in the quantitative data synthesis (Figure 1).‖ All studies were published from 1998 to 2008 in German and English, reporting on a total of 995 patients (716 treated and 279 controls). Tables 1 and 2 provide information on basic parameters of patient demographics and treatments, respectively.
Figure 1.
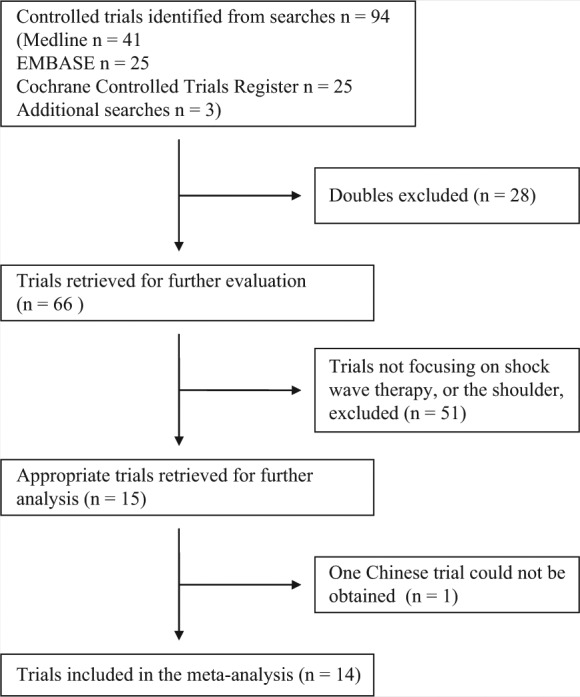
The flow of trials from searches to inclusion.
Table 1.
Characteristics of the included studies.
| High Energy | Low Energy | Controls | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Study | N | Males:Females | Age (Range) | N | Males:Females | Age | N | Males:Females | Age (Range) |
| Albert et al1 | 40 | 31:9 | 46.6 (31-64) | 40 | 30:10 | 47.5 (32-69) | |||
| Buch et al2 | 15 | 8:7 | 56.2 | 15 | 9:6 | 49.9 | 15 | 11:4 | 52.5 |
| Cacchio et al3 | 45 | 27:18 | 56.1 ± 1.9 | 45 | 28:17 | 56.4 ± 2.1 | |||
| Cosentino et al4 | 35 | 20:15 | 51.8 | 35 | 23:12 | 51.8 | |||
| Gerdesmeyer et al7 | 48 | 13:35 | 51.6 ± 8.5 | 48 | 16:32 | 47.3 ± 8.5 | 48 | 28:20 | 52.3 ± 9.8 |
| Hsu et al9 | 33 | 15:18 | 54.4 (30-70) | 13 | 4:9 | 57.8 (44-82) | |||
| Loew et al13 | 20 | 37.8% female | 46 | 20 | 37.8% female | 46 | 20 | 37.8% female | 46 |
| Pan et al15 | 32 | 12:20 | 55.2 ± 2.0 | 28 | 9:19 | 58 ± 1.83 | |||
| Perlick et al16 | 40 | 55% female | 48.4 (38-64) | 40 | 55% female | 48.4 (38-64) | |||
| Peters et al17 | 31 | 19:12 | 52 ± 6 | 30 | 18:12 | 52 ± 6 | 29 | 18:11 | 52 ± 6 |
| Pleiner et al18 | 23 | 8:15 | 54 ± 11 | 20 | 4:16 | 50 ± 8 | |||
| Rompe et al21 | 50 | 25:25 | 49 | 50 | 31:19 | 47 | |||
| Sabeti et al22 | 23 | 60% female | 53.6 ± 8.8 | 21 | 60% female | 49.4 ± 8.4 | |||
| Wang et al26 | 37 | 14:23 | 51 | 6 | 3:3 | 53 | |||
Table 2.
Characterictics of treatment groups of the included studies.a
| High Energy | Low Energy | Controls | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Duration of Sx(mo) | Energy Level (mJ/mm2) × Impulses | Longest Follow-up (mo) | Duration of Sx(mo) | Energy Level (mJ/mm2) × Impulses | Longest Follow-up (mo) | Duration of Sx(mo) | Energy Level (mJ/mm2) × Impulses | Longest Follow-up (mo) | Controls Are | Anesthetic |
| Albert et al1 | 41.2 | 0.45 × 2500, 2 sessions | 3 | 36.4 | 0.01-0.06 × 2500, 2 sessions | Low energy | Yes | ||||
| Buch et al2 | 35.8 | 0.28, 2 sessions | 12 | 69.1 | 0.08, 4 sessions | 12 | 63.3 | 0 | 12 | Low energy and needling | Not reported |
| Cacchio et al3 | 14 ± 4.95 | 0.1 × 2500, 4 sessions | 6 | 13 ± 5.03 | 0 | 6 | Sham | No | |||
| Cosentino et al4 | 15 | 0.28 × 1200, 4 sessions | 6 | 14.5 | 0 | 6 | Sham | No | |||
| Gerdesmeyer et al7 | 42.6 ± 23.2 | 0.32 × 1500, 2 sessions | 12 | 42.8 ± 25.2 | 0.08 × 6000, 2 sessions | 12 | 41.3 ± 28.6 | 12 | Low energy and sham | No | |
| Hsu et al9 | 12.3 (6-72) | 0.55 x 1000, 2 sessions | 12 | 11.1 (6-30) | 0 | 12 | Sham | Yes | |||
| Loew et al13 | 36 | 0.3 × 2000, 1 session | 36 | 0.1 × 2000, 1 session | 36 | 0 | Low energy and sham | Yes | |||
| Pan et al15 | 24.55 ± 6,45 | 0.26-0.32 × 2000 | 3 | 23.90 ± 5.32 | 0 | 3 | TENS | Not reported | |||
| Perlick et al16 | >12 | 0.42 × 2000, 2 sessions | 12 | >12 | 0.23 × 2000, 2 sessionsb | 12 | Low energy | Yes | |||
| Peters et al17 | >6 | 0.44 × 1500 | 6 | >6 | 0.15 × 1500 | 6 | >6 | 0 | 6 | Sham | No |
| Pleiner et al18 | 0.28 × 2000, 2 sessions | 7 | <0.07 × 2000, 2 sessions | 7 | Low energy | Not reported | |||||
| Rompe et al21 | 25 (12-84) | 0.28 × 1500, 1 session | 6 | 33 (12-120) | 0.06 × 1500, 1 session | 6 | Low energy | No | |||
| Sabeti et al22 | >6 | 0.2 × 2000, 2 sessions | 3 | >6 | 0.08 × 1000, 3 sessions | 3 | High vs low | Only for high energy | |||
| Wang et al26 | 8 (6-12) | 0.18 × 1000 | 36 | 8.6 (6-24) | 0 | 6 | Sham | Yes | |||
Sx, shock wave therapy; TENS, transcutaneous electric nerve stimulator.
Both treatments in this study were high energy according to our classification criteria (>0.2 mJ/mm2).
Using the Jadad scale, the overall quality of the studies was measured at a mean of 2.6 (95% CI,1.8-3.4), which is good compared to a study by Vavken et al25 of the average quality scores for orthopaedic studies.
Shock Wave Treatment Versus Other Treatments
Hsu et al9 published the most recent trial in 2008, studying 33 patients treated with high-energy shock wave therapy and 13 receiving sham treatment. One major flaw of this study was that the randomization sequence was based on the order of presentation of patients, thus not appropriately randomized, but also not blinded. This study showed significantly better results in both pain reduction and improvement of function measured on the Constant-Murley score (CMS). Reduction of calcium deposits was significantly better in the exposed group, but independent of Gaertner stage. The authors reported no significant adverse effects with treatment.
A randomized trial of 60 patients receiving high-energy and low-energy shock wave therapy compared to treatment with a transcutaneous electric nerve stimulator (TENS) was published by Pan et al in 2003.15 Constant-Murley score, pain on a visual analog scale (VAS), and manual muscle tests were assessed at 2, 4, and 12 weeks. Deposit resorption was monitored with sonography at the same intervals. Shock wave treatment showed significantly better results for pain, as well as higher rates of deposit resorption.
Cosentino et al4 conducted a single-blinded randomized study, with 70 patients undergoing either shock wave therapy or sham treatment.4 Pain and function were measured at 6 months using a VAS and CMS. Radiographs were used to assess deposit resorption. This study showed significant improvements in pain and function for shoulders treated with shock wave therapy, as well as complete resorption of 31% of deposits.
Gerdesmeyer et al7 published the largest of the included studies in 2003. A total of 144 patients were allocated to either high-energy or low-energy shock wave therapy or placebo treatment in a randomized, double-blinded study. The primary end point was the 6-month CMS. Secondary end points were CMS at 3 months, pain at 6 months, and radiographs at 3, 6, and 12 months. Ten patients were lost to follow-up. Significant improvements in all end points were seen in both high-energy and low-energy groups compared to sham treatment 6 months after treatment, but significantly better results were seen for high-energy treatment. The same pattern could be shown for 3 and 24 months of follow-up.
During the same year, Wang et al26 published the results from a prospective, blinded, nonrandomized trial of shock wave therapy versus sham treatment. However, most patients refused participation once allocated to sham treatment. Eventually, 33 patients received shock wave therapy, but only 6 patients were included in the control group. The CMS and pain on the VAS were recorded at 2 and 4 weeks, 3, 6, and 12 months, and yearly thereafter. Significantly more excellent and good results and a higher rate of deposit resorption in the exposed group were reported.
Buch et al2 reported on a prospective, controlled, but not randomized trial. Pain on the VAS, deposit resorption on radiography, subjective improvement, and the Roles and Maudsley score at 12 weeks were given for 15 patients allocated to high-energy, low-energy, or needling. Best, and persistent, results were shown for high-energy shock wave therapy, while the low-energy group had significantly more recurrences. The needling group experienced higher rates of adverse effects.
High-Energy Versus Low-Energy Studies
In 2007, Albert et al1 used sample size calculations based on CMS and enrolled 80 patients in a blinded randomized trial of high-energy versus low-energy shock wave therapy on shoulder function. Secondary end points were change in intensity of self-rated shoulder pain and subjective success of treatment. In an intention-to-treat analysis, high-energy treatment showed significantly better results than low-energy treatment. Low-energy treatment produced no significant improvement from the baseline value. The rates of deposit resorption over an average of 110 days of follow-up were 15% and 5% for high-energy and low-energy treatment, respectively. Treatments were well accepted by all patients, although some petechiae or small bruises were reported in the high-energy group.
In 2006, Cacchio et al3 reported on a prospective, randomized, single-blinded trial of 90 patients treated with high-energy shock waves or sham treatment. Primary end points were improvement in the University of California at Los Angeles (UCLA) score or VAS pain scale at 6 months. The secondary end point was deposit resorption on plain radiographs, and attrition was considered in the final analysis.3 This study found significant reduction of pain and increases in function from 4 weeks to 6 months of follow-up; 86.6% of all deposits in the treatment group completely resorbed by 6 months.
Sabeti et al22 published results of a blinded, randomized, controlled trial of high-energy versus low-energy shock wave therapy in 50 patients. Forty-four patients completed the study and showed significant improvement in VAS and CMS scores, but no significant differences were found between groups. This might be explained by the fact that both energy levels were low-energy treatments.
Pleiner et al18 performed a randomized, double-blinded study on 45 patients. Pain on VAS, improvement on the CMS, and radiologic deposit resorption were used as end points in 2 groups receiving either low-energy and high-energy intensity treatment.18 Seven months before final analysis, 10 patients (22%) were lost to follow-up, raising questions on the validity of this study. Throughout the duration of follow-up, the high-energy group showed significantly higher CMS results, but better VAS results only during the first week after treatment. At 7 months, 19% of the calcifications in the high-energy group and 8% in the low-energy group were dissolved.
In the same year, Peters et al17 published the results from their randomized study on 90 patients receiving shock wave therapy on 2 energy levels and a placebo. Pain during treatment, symptoms, and deposit resorption were recorded at 6 months. The low-energy group had less pain during treatments, but needed more treatments and had more residual calcification than the high-energy group. Both treatment groups showed better results than the sham treatment.
Perlick et al16 included 80 patients in a blinded, randomized, controlled trial of high-energy versus low-energy shock wave treatment. Significant increases in CMS were reported at 3 months after treatment but attenuation of this effect after 1 year. There were no significant differences between groups, most likely due to the similar high-energy intensity exposure (0.23 and 0.42 mJ/mm2).
A trial of 80 patients in 4 groups receiving different levels of shock wave therapy or placebo treatment was published by Loew et al.13 End points (subjective, CMS, and deposit resorption at 3 months), showed significant improvements in a dose-response–dependent manner for all end points.
The first randomized, blinded study to be included in our analysis was performed by Rompe et al21 in 1998. One hundred patients were allocated to either high-energy or low-energy treatment with end points measured at 24 weeks after treatment. Constant-Murley score, subjective rating, and plain radiographs were used. Both groups showed significant improvement over time, but results were significantly better for the high-energy group compared to the low-energy group.
Quantitative Data Synthesis
Data concerning this study’s primary research question from all eligible studies were assessed for heterogeneity by the Q test and the I2 index and showed 91.7% between-study variability for reduction of pain, 79.1% for improvement of function, and 66.1% for resorption of deposits. Graphical representation of the individual study estimates in forest plots revealed a more or less normal distribution of variability, thus the authors chose to employ a DerSimonian-Laird random effects model. For the second study question, there was clearly less, but still significant, heterogeneity for reduction in pain (I2 = 61.2%) and improvement of function (I2 = 45.65). Again, the forest plots suggested a normal distribution of the effects of individual studies around a pooled estimate from a random effects model.
Before data were pooled, further assessment of potential sources of heterogeneity was done by analyzing subgroups by level of energy and type of control. The analysis showed only marginal reduction of the amount of between-study variability for improvement of function. For reduction of pain, between-study heterogeneity was virtually eliminated in both high-energy subgroups, demonstrating this variable as a source of heterogeneity.
Concerning the primary study question, regression analysis of the effect sizes showed significant positive associations with age (P = .002) and a negative association with percentage of females (P = .008), after Bonferroni adjustment for multiple testing. There was no significant association with study precision as measured by standard errors of effects (P = .932). Concerning the second study question, a borderline significant association was apparent between effect size and age (P = .056), but no associations of effect size with percentage of female patients, standard errors, or any variable describing differences in treatment regimens.
Concerning the primary question, a significant result could be seen in pain reduction for high-energy treatment levels versus other treatments with a WMD of −1.99 points and a 95% CI of −2.96 to −1.03, and a WMD of −4.43 points and a 95% CI of −5.23 to −3.64 for high-energy versus placebo treatment. Low-energy treatment versus placebo treatment resulted in a WMD of −3.76 points and a 95% CI of −6.57 to −0.96. There was no significant difference in the reduction of pain after low-energy shock wave or other treatments (WMD, 0.02 points; 95% CI, −1.79 to 1.83).
There were significantly higher improvements in CMS for high-energy treatment compared with other treatments (WMD, 16.45 points; 95% CI, 9.92-22.98), compared with placebo (WMD, 21.77 points; 95% CI, 13.51-30.03), as well as for low-energy treatment compared to controls (WMD, 19.18 points; 95% CI, 0.92-37.45).
The odds ratio of complete deposit resorption clearly favored shock wave therapy over controls at 3.67 (95% CI, 1.93-6.98; P < .001).
Comparing the effectiveness of high-energy and low-energy treatments, there were significantly better results with the former. The reduction in pain was 1.66 points (95% CI, 0.68-2.64) higher, and thus significantly better (P < .001) in the high-energy group. There was also a significantly higher improvement in CMS results in the high-energy group (WMD, 10.66 points; 95% CI, 7.22-14.10; P < .001).
Our calculations also revealed that the odds for complete deposit resorption were 14.11 times (95% CI, 3.02-65.96) higher in the high-energy group.
Discussion
The objective of this study was 2-fold: first, to assess the evidence for the effectiveness of shock wave therapy compared to placebo and other treatments; and second, to confirm such an anticipated effect by proving a dose-response relationship of shock wave energy and treatment effect.
We chose to perform calculations for 6-month follow-up because of the frequent self-limiting natural history of this condition, although some studies reported longer follow-up. Pain was considered the most important end point as it usually is the chief complaint of the patient. The effect on pain was measured on a VAS, which was not only statistically significant but also clinically significant in absolute values. Restoration of function was ranked as a secondary end point. Deposit resorption was considered as a third end point. Comparison of high-energy and low-energy shock wave therapy showed significantly better results for both pain and function in high-energy treatment. We consider this dose-response relationship as evidence that there is a true treatment effect. Shock wave therapy is a promising option in the conservative management of calcifying tendinitis of the shoulder.
Possible sources of heterogeneity were explored using stratification and meta-regression. Stratification by energy level and type of control (ie, placebo or other treatments) only minimally attenuated heterogeneity. Further analysis revealed significant associations between different treatment effects, between studies, and differences in age and percentage of female patients, thus suggesting this was a source of heterogeneity. Yet the most likely source of heterogeneity is differences within the treatments themselves—for example, some studies classify energy levels as high that are well below the low-energy levels classified in others. What some consider an untreated control is a low-energy group for others. However, we could not find associations between these differences and differences in outcomes for pain or function, leading to the conclusion that there is an independent, consistent dose-response relationship at all studied levels.
Finally, the graphical representation of the effects of the included studies suggested that these individual results were more or less normally distributed around, rather than forming clusters as would be expected in the case of 1 or more influential covariates. In the face of such a distribution of heterogeneity, pooling may be done using random effects models without jeopardizing the validity of results. However, we recommend cautiously interpreting all results and following the confidence intervals rather than the absolute values of the mean differences.
The Jadad scale was used to assess the internal validity of the included trials, the results of which were encouragingly good. A potential downside of any method of quality assessment is not the quality of the study, but rather the quality of the reporting measured.6,11
Some studies might very well be considerably underpowered, thus showing spuriously insignificant results.
Conclusion
Shock wave therapy is a heterogeneous but effective treatment for calcifying tendinitis of the shoulder. One source of heterogeneity is patient selection, suggesting that not all patients benefit equally. Currently, only ambiguous guidelines for the optimal number of sessions or impulses per session exist. These parameters did not appear to outweigh absolute energy levels in importance. Treatment effects may be substantially improved through addressing this problem.
Footnotes
References
- 1. Albert JD, Meadeb J, Guggenbuhl P, et al. High-energy extracorporeal shock-wave therapy for calcifying tendinitis of the rotator cuff: a randomised trial. J Bone Joint Surg Br. 2007;89:335-341 [DOI] [PubMed] [Google Scholar]
- 2. Buch M, Hahne H, Klatt J, Träger D, Siebert W. Ergebnisse der Stosswellentherapie bei der Tendinosis Calcarea der Schulter aus der Orthopädischen Klink Kassel. Orthop Prax. 1999;35:143-149 [Google Scholar]
- 3. Cacchio A, Paoloni M, Barile A, et al. Effectiveness of radial shock wave therapy for calcific tendinitis of the shoulder: single-blind, randomized clinical study. Phys Ther. 2006;86:672-682 [PubMed] [Google Scholar]
- 4. Cosentino R, Stefano RD, Selvi E, et al. Extracorporeal shock wave for chronic calcific tendinitis of the shoulder: single blind study. Ann Rheum Dis. 2003;62:248-250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177-188 [DOI] [PubMed] [Google Scholar]
- 6. Emerson J, Burdick E, Hoaglin D, Mosteller F, Chalmers T. An empirical study of the possible relation of treatment differences to quality scores in controlled randomized clinical trials. Control Clin Trial. 1990;11:339-352 [DOI] [PubMed] [Google Scholar]
- 7. Gerdesmeyer L, Wagenpfeil S, Haake M, et al. Extracorporeal shock wave therapy for the treatment of chronic calcifying tendonitis of the rotator cuff: a randomized controlled trial. JAMA. 2003;290:2573-2580 [DOI] [PubMed] [Google Scholar]
- 8. Green S, Buchbinder R, Glazier R, Forbes A. Systematic review of randomised controlled trials of interventions for painful shoulder: selection criteria, outcome assessment, and efficacy. BMJ. 1998;316:354-360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hsu CJ, Wang DY, Tseng KF, Fong YC, Hsu HC, Jim YF. Extracorporeal shock wave therapy for calcifying tendinitis of the shoulder. J Shoulder Elbow Surg. 2008;17:55-59 [DOI] [PubMed] [Google Scholar]
- 10. Jadad A, Moore R, Carrol D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trial. 1996;17:1-12 [DOI] [PubMed] [Google Scholar]
- 11. Jüni P, Altman D, Egger M. Assessing the Quality of Randomised Controlled Trials. London: BMJ Publishing Group; 2001 [Google Scholar]
- 12. Krasny C, Enenkel M, Aigner N, Wlk M, Landsiedl F. Ultrasound-guided needling combined with shock-wave therapy for the treatment of calcifying tendonitis of the shoulder. J Bone Joint Surg Br. 2005;87:501-507 [DOI] [PubMed] [Google Scholar]
- 13. Loew M, Daecke W, Kusnierczak D, Rahmanzadeh M, Ewerbeck V. Shock wave therapy is effective for chronic calcifying tendinitis of the shoulder. J Bone Joint Surg Br. 1999;81:863-867 [DOI] [PubMed] [Google Scholar]
- 14. Moher D, Cook D, Eastwood S, Olkin I, Stroup D. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Lancet. 1999;354:1896-1900 [DOI] [PubMed] [Google Scholar]
- 15. Pan P, Chou C, Chiou H, Ma H, Lee H, Chan R. Extracorporeal shock wave therapy for chronic calcific tendinitis of the shoulders: a functional and sonographic study. Arch Phys Med Rehabil. 2003;84:988-993 [DOI] [PubMed] [Google Scholar]
- 16. Perlick L, Luring C, Bathis H, Perlick C, Kraft C, Diedrich O. Efficacy of extracorporeal shock-wave treatment for calcific tendinitis of the shoulder: experimental and clinical results. J Orthop Sci. 2003;8:777-783 [DOI] [PubMed] [Google Scholar]
- 17. Peters J, Luboldt W, Schwarz W, Jacobi V, Herzog C, Vogl T. Extracorporeal shock wave therapy in calcific tendinits of the shoulder. Skeletal Radiol. 2004;33:712-718 [DOI] [PubMed] [Google Scholar]
- 18. Pleiner J, Crevenna R, Langenberger H, et al. Extracorporeal shockwave treatment is effective in calcific tendonitis of the shoulder: a randomized controlled trail. Wien Klin Wochenschr. 2004;116:536-541 [DOI] [PubMed] [Google Scholar]
- 19. Porcellini G, Paladini P, Campi F, Paganelli M. Arthroscopic treatment of calcifying tendinitis of the shoulder: clinical and ultrasonographic follow-up findings at two to five years. J Shoulder Elbow Surg. 2004;13:503-508 [DOI] [PubMed] [Google Scholar]
- 20. Robinson KA, Dickersin K. Development of a highly sensitive search strategy for the retrieval of reports of controlled trials using PubMed. Int J Epidemiol. 2002;31:150-153 [DOI] [PubMed] [Google Scholar]
- 21. Rompe J, Bürger R, Hopf C, Eysel P. Shoulder function after extracorporeal shock wave therapy for calcific tendinitis. J Shoulder Elbow Surg. 1998;7:505-509 [DOI] [PubMed] [Google Scholar]
- 22. Sabeti M, Dorotka R, Goll A, Gruber M, Schatz KD. A comparison of two different treatments with navigated extracorporeal shock-wave therapy for calcifying tendinitis—a randomized controlled trial. Wien Klin Wochenschr. 2007;119:124-128 [DOI] [PubMed] [Google Scholar]
- 23. Seil R, Litzenburger H, Kohn D, Rupp S. Arthroscopic treatment of chronically painful calcifying tendinitis of the supraspinatus tendon. Arthroscopy. 2006;22:521-527 [DOI] [PubMed] [Google Scholar]
- 24. SIGN. Scottish Intercollegiate Guideline Network. http://sign.ac.uk/methodology/filters.html Accessed January 13, 2009
- 25. Vavken P, Culen G, Dorotka R. Clinical applicability of evidence-based orthopedics—a cross-sectional study of the quality of orthopedic evidence. Z Orthop Unfall. 2008;146:21-25 [DOI] [PubMed] [Google Scholar]
- 26. Wang C, Yang K, Wang F, Chen H, Wang J. Shock wave therapy for calcific tendinitis of the shoulder: a prospective clinical study with two-year follow-up. Am J Sports Med. 2003;31:425-430 [DOI] [PubMed] [Google Scholar]


