Shoulder pain is the most common orthopaedic complaint of competitive swimmers. Epidemiological studies have reported the incidence and recurrence rates of shoulder pain to be as high as 80% among top US competitors.16 Although the precise origin of pain may be elusive, the term “swimmer’s shoulder” has been used to describe the inflammation resulting from dynamic impingement of the rotator cuff and coracoacromial arch. Long training seasons, repetitive overhead arm motion, overuse fatigue, increased glenohumeral laxity, and poor swimming technique may all contribute to the shoulder pain that frequently occurs in this unique group of athletes.2,10,11,15,17
In this report, we present a female Division I collegiate swimmer with shoulder pain secondary to a symptomatic os acromiale. This patient’s presentation serves to provide clinicians a sentinel reminder to consider all potential causes of shoulder pain in competitive athletes, particularly in the setting of a more common, confounding diagnosis.
Case Report
A 19-year-old, right-hand-dominant collegiate swimmer presented with insidious-onset left shoulder discomfort present for the past 3 years. She denied any history of antecedent trauma and reported the gradual onset of symptoms during her junior year in high school. She reported no episodes of shoulder subluxation or dislocation and had no obvious symptoms of instability.
She was first evaluated for her shoulder by her primary physician and orthopaedic surgeon at the completion of her junior year season. She had an anteroposterior and oblique radiograph of her left shoulder, which were reportedly normal, and “swimmer’s shoulder” was diagnosed. She underwent two 6-week sessions of supervised physical therapy with multiple therapists, including posterior capsular stretching, rotator cuff strengthening, and scapular stabilization exercises. She also used nonsteroidal, anti-inflammatory medications for 6 weeks. Her symptoms only modestly improved, and she continued to experience significant discomfort during practice sessions. The pain was most severe with freestyle swimming, at the beginning of the pull-through phase of her stroke. She was unable to compete secondary to pain and ultimately sought repeat consultation from her treating orthopaedic surgeon. Impingement syndrome was diagnosed, and she was provided a subacromial corticosteroid injection. She refrained from swimming for 2 months and experienced relief of her pain. Upon returning to competitive swimming at the collegiate level, she had a complete recurrence of shoulder discomfort. The pain was limiting overhead motion and precluded training or competing in freestyle or backstroke events.
At the time of our evaluation, physical examination revealed normal scapulothoracic rhythm with no evidence of winging or scapulothoracic dyskinesia. Her left upper extremity neurological examination was normal. Rotator cuff strength appeared normal, but supraspinatus strength testing was limited secondary to pain. She experienced discomfort with active forward flexion beyond 90° but had full passive forward flexion to 170°. Internal and external rotation was 100° and symmetric with the unaffected right side. Abduction and adduction were 180° and 30°, respectively, and symmetric bilaterally. Hawkins and Neer impingement signs were positive. She was mildly tender over the bicipital groove, and Speed’s and Yergason’s provocative tests were negative for pain. The Jobe test was negative for apprehension, the load and shift test demonstrated normal stability that was symmetric with the contralateral side, and sulcus sign was not present. She was exquisitely tender to palpation over the anterolateral acromion and acromioclavicular joint. She stated that firm pressure over the acromion reproduced her usual symptoms.
Plain radiographs, including an anteroposterior, internal rotation, and axillary view of the left shoulder revealed an os acromiale–mesoacromiale variant (Figure 1). A double density sign was not appreciated on the anteroposterior view, likely contributing to the previously missed diagnosis. The contralateral shoulder radiographs were normal. Magnetic resonance imagining (MRI) of the left shoulder confirmed the presence of the os acromiale with edema at the nonunion site. The rotator cuff and labrum were intact and without abnormality.
Figure 1.
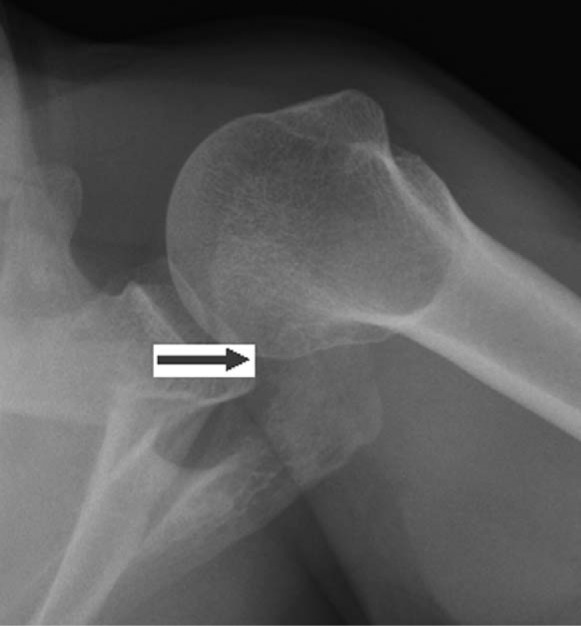
Axillary view of left shoulder demonstrating os acromiale–mesoacromiale variant. The arrow marks the nonunion between the meta- and mesoacromial junction.
Given the reproducibility of her symptoms on provocative examination and her prolonged course, the patient elected to undergo surgical stabilization of the os acromiale. Examination under anesthesia revealed no evidence of pathologic hyperlaxity or instability, with negative load and shift examinations bilaterally. Diagnostic arthroscopy revealed no evidence of synovitis or intra-articular pathology. The biceps anchor, labrum, articular surface, and rotator cuff were intact. The subacromial space revealed only mild bursal inflammation and no evidence of outlet impingement. The os acromiale was mobile.
A longitudinal saber incision was made directly over the anterolateral acromion. The deltoid muscle was split in line with its fibers to allow for subperiosteal exposure of the os acromiale and nonunion site. The os fragment was unstable. The nonunion was curetted and debrided to bleeding, cancellous bone on apposing surfaces. The os fragment was rigidly fixed with two 4.0-cancellous screws and 18-gauge tension band wires. Fluoroscopy with multiple oblique views and direct palpation beneath the acromion confirmed satisfactory hardware position and avoidance of screw tip penetration into the subacromial space. A corticocancellous graft was harvested from the left iliac crest and placed into a burred trough at the nonunion site (Figure 2).
Figure 2.

Postoperative axillary radiograph demonstrating cannulated screw and tension band wire fixation of the os acromiale. A corticocancellous bone autograft has been incorporated into the repair at the nonunion site.
Postoperatively, the patient’s shoulder was immobilized in a sling, and she was instructed on immediate elbow, wrist, and hand active-motion exercises. Gentle passive range of motion of the shoulder was allowed after 1 week. Active range of motion of the shoulder was initiated at 3 weeks with formal physical therapy. An external bone stimulator was also initiated at 3 weeks to maximize the likelihood of union. Two months after surgery, she achieved full range of motion and initiated strengthening exercises for her left upper extremity. She was allowed to return to a supervised swimming program at school. By 3 months, a computed tomographic (CT) scan confirmed a complete union with bridging trabeculation across the nonunion site (Figure 3). She increased her training exercises and was able to return to competition 5 months after surgery. She experienced intermittent episodes of soreness around the incision after prolonged freestyle events, but otherwise noted complete resolution of her preoperative symptoms. At final examination, she had achieved nearly full preoperative range of motion with a slight reduction of 10° of forward flexion and external rotation relative to the contralateral side. The surgical scar and acromion were nontender to palpation and well healed.
Figure 3.

Sagittal computed tomography (CT) images demonstrating bridging trabeculation across the nonunion site.
She underwent elective hardware removal and subacromial bursectomy at 1 year postoperatively. She has subsequently continued to swim competitively and has experienced intermittent mild discomfort with overhead activities.
Discussion
Shoulder pain in the swimming athlete is remarkably common. Frequently referred to as “swimmer’s shoulder,” the incidence of shoulder pain and discomfort among competitive swimmers is as high as 50% to 80% in recent studies.2,10,11,15,17 These symptoms are generally attributed to dynamic impingement between the rotator cuff and coracoacromial arch. The long season, high training intensity, and repetitive overhead motions required of elite swimmers puts them at significant risk for overuse trauma and shoulder complaints.2,10,11,15-17 Muscle fatigue and decreased ability of the rotator cuff to stabilize the humeral head may precipitate mechanical impingement, especially in the setting of underlying laxity, which is common in swimmers. Poor swimming technique, particularly during the pull-through phase of freestyle swimming, or the use of certain training equipment can also increase the risk of dynamic outlet impingement.2,10,11,15-17 Treatment often consists of a comprehensive program to improve technique as well as strength, endurance, and balance of the shoulder muscle groups.
Recent arthroscopic studies, however, have suggested that “swimmer’s shoulder” encompasses a variety of different pathologies, including instability, labral tears, subacromial impingement, and rotator cuff lesions.2,10,11,15-17 This term must therefore be used with caution, as it represents a constellation of symptoms rather than a specific diagnosis. Swimmers often have some degree of increased laxity that likely contributes to secondary impingement.
We report a unique case of a symptomatic os acromiale as a cause for shoulder discomfort in a collegiate swimmer. Although uncommon, this case serves as a sentinel reminder to clinicians that an os acromiale must be considered in the differential diagnosis of the young swimming athlete. The symptoms of a painful os acromiale may strongly resemble those seen with dynamic impingement from overuse fatigue, making the diagnosis subtle and sometimes difficult.1,3,4,8 A careful physical examination and review of imaging studies can avoid a delay to definitive diagnosis. Incomplete relief from physical therapy or subacromial injection should also prompt the physician to reevaluate the working diagnosis. Further imaging using either MRI or bone scan can be helpful. Magnetic resonance imaging may demonstrate marrow edema at an unstable os acromiale, while a bone scan often demonstrates increased radiotracer uptake in the region. Verification that the os acromiale is the cause of symptoms can also be done using a diagnostic lidocaine injection into the nonunion site.1,4,5,8,13,14,22 Precise localization of the injection may be done using ultrasound or fluoroscopic guidance. In our patient, the os acromiale was recognized in a delayed fashion and successfully treated with surgical stabilization.
A symptomatic os acromiale as a cause of shoulder pain has been reported in competitive athletes of other sports.1,4-9,12-14,18-22 Pagnani et al13 reported on the successful surgical treatment of 9 football and basketball players with symptomatic nonunion. Demetracopoulos et al5 have recently presented favorable outcomes after operative stabilization of an unstable os acromiale in an elite pitcher. As with our case, recognition of the diagnosis was critical given the myriad confounding causes of shoulder pain in these athletes.
Conclusion
Shoulder pain is a remarkably common complaint among elite swimmers. Although these symptoms are most commonly the result of muscle fatigue and rotator cuff overload, other diagnoses must also be considered. The treating physician should perform a thorough and complete evaluation to avoid a missed diagnosis. An os acromiale should be included in the differential diagnosis of the swimming athlete who presents with shoulder pain, particularly in the setting of a failed response to physical therapy, activity modification, or steroid injection.
Footnotes
No potential conflict of interest declared.
References
- 1. Abboud JA, Silverberg D, Pepe M, et al. Surgical treatment of os acromiale with and without associated rotator cuff tears.J Shoulder Elbow Surg. 2006;15(3):265-270 [DOI] [PubMed] [Google Scholar]
- 2. Borsa PA, Scibek JS, Jacobson JA, Meister K. Sonographic stress measurement of glenohumeral joint laxity in collegiate swimmers and age-matched controls. Am J Sports Med. 2005;33(7):1077-1084 [DOI] [PubMed] [Google Scholar]
- 3. Burbank KM, Lemos MJ, Bell G, Lemos DW. Incidence of os acromiale in patients with shoulder pain. Am J Orthop. 2007;36(3):153-155 [PubMed] [Google Scholar]
- 4. Case DT, Burnett SE, Nielsen T. Os acromiale: population differences and their etiological significance. Homo. 2006;57(1):1-18 [DOI] [PubMed] [Google Scholar]
- 5. Demetracopoulos CA, Kapadia NS, Herickhoff PK, Cosgarea AJ, McFarland EG. Surgical stabilization of os acromiale in a fast-pitch softball pitcher. Am J Sports Med. 2006;34(11):1855-1859 [DOI] [PubMed] [Google Scholar]
- 6. Edelson JG, Zuckerman J, Hershkovitz I. Os acromiale: anatomy and surgical implications. J Bone Joint Surg Br. 1993;75(4):551-555 [DOI] [PubMed] [Google Scholar]
- 7. Gonzales JB, Pearson SE, Beach WR. Fusion of unstable os acromiale. J Shoulder Elbow Surg. 2001;10(2):197-198 [DOI] [PubMed] [Google Scholar]
- 8. Kurtz CA, Humble BJ, Rodosky MW, Sekiya JK. Symptomatic os acromiale. J Am Acad Orthop Surg. 2006;14(1):12-19 [DOI] [PubMed] [Google Scholar]
- 9. Lee DH, Lee KH, Lopez-Ben R, Bradley EL. The double-density sign: a radiographic finding suggestive of an os acromiale. J Bone Joint Surg Am. 2004;86A(12):2666-2670 [PubMed] [Google Scholar]
- 10. McMaster WC. Swimming injuries. An overview. Sports Med. 1996;22(5):332-336 [DOI] [PubMed] [Google Scholar]
- 11. McMaster WC. Anterior glenoid labrum damage: a painful lesion in swimmers. Am J Sports Med. 1986;14(5):383-387 [DOI] [PubMed] [Google Scholar]
- 12. Ortiguera CJ, Buss DD. Surgical management of the symptomatic os acromiale. J Shoulder Elbow Surg. 2002;11(5):521-528 [DOI] [PubMed] [Google Scholar]
- 13. Pagnani MJ, Mathis CE, Solman CG. Painful os acromiale (or unfused acromial apophysis) in athletes. J Shoulder Elbow Surg. 2006;15(4):432-435 [DOI] [PubMed] [Google Scholar]
- 14. Peckett WR, Gunther SB, Harper GD, Hughes JS, Sonnabend DH. Internal fixation of symptomatic os acromiale: a series of 26 cases. J Shoulder Elbow Surg. 2004;13(4):381-385 [DOI] [PubMed] [Google Scholar]
- 15. Pink M, Jobe FW, Perry J, Browne A, Scovazzo ML, Kerrigan J. The painful shoulder during the butterfly stroke. An electromyographic and cinematographic analysis of 12 muscles. Clin Orthop Relat Res. 1993;288:60-72 [PubMed] [Google Scholar]
- 16. Richardson AB, Jobe FW, Collins HR. The shoulder in competitive swimming. Am J Sports Med. 1980;8(3):159-163 [DOI] [PubMed] [Google Scholar]
- 17. Ruwe PA, Pink M, Jobe FW, Perry J, Scovazzo ML. The normal and the painful shoulders during the breaststroke. Electromyographic and cinematographic analysis of 12 muscles. Am J Sports Med. 1994;22(6):789-796 [DOI] [PubMed] [Google Scholar]
- 18. Salamon PB. The treatment of symptomatic os acromiale. J Bone Joint Surg Am. 1999;81(8):1198 [PubMed] [Google Scholar]
- 19. Sammarco VJ. Os acromiale: frequency, anatomy, and clinical implications. J Bone Joint Surg Am. 2000;82(3):394-400 [DOI] [PubMed] [Google Scholar]
- 20. Sassmannshausen G, Wilson TC, Mair SD. Operative stabilization of an unstable os acromiale in an adolescent football player. Orthopedics. 2003;26(5):509-511 [DOI] [PubMed] [Google Scholar]
- 21. Sterling JC, Meyers MC, Chesshir W, Calvo RD. Os acromiale in a baseball catcher. Med Sci Sports Exerc. 1995;27(6):795-799 [PubMed] [Google Scholar]
- 22. Youm T, Hommen JP, Ong BC, Chen AL, Shin C. Os acromiale: evaluation and treatment. Am J Orthop. 2005;34(6):277-283 [PubMed] [Google Scholar]


