Abstract
Context:
Symptomatic scapulothoracic bursitis and crepitus are disorders of the scapulothoracic articulation that are often poorly understood. They can be a source of persistent pain and dysfunction in the active overhead throwing athlete. It is important to distinguish between scapulothoracic bursitis and scapulothoracic crepitus. Scapulothoracic bursitis refers to inflammation of the bursae secondary to trauma or overuse owing to sports activities or work. Scapulothoracic crepitus is defined by a grinding, popping, or thumping sound or sensation secondary to abnormal scapulothoracic motion.
Evidence Acquisition:
This article presents the causes, diagnosis, and management of these shoulder conditions in a manner that is relevant to clinicians, athletic trainers, and physical therapists, and it reviews relevant studies to determine the consensus on nonoperative treatment, as well as open and arthroscopic surgical treatment.
Results:
The causes of scapulothoracic bursitis and crepitus include direct or indirect trauma, overuse syndromes, glenohumeral joint dysfunction, osseous abnormalities, muscle atrophy or fibrosis, and idiopathic causes. Scapulothoracic bursitis and crepitus remain primarily clinical diagnoses; however, imaging studies or local injections may also be helpful. The initial treatment of scapulothoracic bursitis and scapulothoracic crepitus should be nonoperative. Surgical treatment options include partial scapulectomy or resection of the superomedial angle of the scapula, open bursal resection, and arthroscopic bursectomy. Despite the lack of agreement among orthopaedic surgeons concerning which procedure is best for treating symptomatic scapulothoracic bursitis and crepitus, most reports have demonstrated good to excellent outcomes in a significantly high percentage of patients.
Conclusion:
Clearly, the best initial approach to these conditions is a nonoperative treatment plan that combines scapular strengthening, postural reeducation, and core strength endurance. The addition of local modalities, nonsteroidal anti- inflammatory drugs, and localized injections may also be helpful. If an appropriate trial of nonoperative management proves unsuccessful, surgical correction can produce good results.
Keywords: shoulder, scapulothoracic bursitis, snapping scapula
The scapula is a thin triangular-shaped bone that serves as an attachment site for most of the extrinsic and intrinsic muscles providing movement and stability to the glenohumeral and scapulothoracic joints. Its function is crucial to maintaining a stable base of support for the humerus and allowing dynamic positioning of the glenoid fossa during glenohumeral elevation.27 The scapula is attached to the axial skeleton via the clavicle, which acts as a strut allowing scapular rotation and translation along the thoracic wall and opposing medially directed forces of the periscapular muscles.28 This biomechanical construct provides the smooth gliding movement of the relatively concave scapula on the convex thoracic cage. Symptomatic scapulothoracic bursitis and scapulothoracic crepitus are uncommon and often poorly understood disorders of the scapulothoracic articulation. In the active athlete, however, they can be a source of persistent pain and dysfunction.
It is important to realize the subtle differences between scapulothoracic bursitis and scapulothoracic crepitus. Scapulothoracic crepitus was first described by Boinet5 in 1867. Milch49 later added to the understanding by identifying 2 types of scapulothoracic crepitus. An osseous lesion, such as an osteochondroma in the scapulothoracic space, produces a loud grinding, thumping, or popping sound with scapulothoracic motion. These noises are amplified by the thoracic cavity, which acts as a resonance chamber, similar to a stringed instrument.2 Milch48 called this type of severe scapulothoracic crepitus the “snapping scapula.”
The other, less severe symptomatic scapulothoracic crepitus has a soft tissue cause, such as bursitis. Codman15 described the bursa of the scapulothoracic joint and believed that scapulothoracic crepitus was caused by irritation of these bursae. It is important to appreciate that painful scapulothoracic bursitis may be present without associated crepitus.35 Furthermore, scapulothoracic crepitus may not always be pathologic. For example, Grünfeld22 reported finding scapular crepitus in 31% of 100 normal asymptomatic persons. As a result, patients with psychiatric conditions may not respond to treatment as well as other patients.
Anatomy
It is crucial, clinically and surgically, to have a clear understanding of the anatomy and biomechanics of the scapulothoracic articulation when treating scapulothoracic bursitis and scapulothoracic crepitus.42 The scapula is the essential link for coordinated upper extremity activity. However, there is no true bony attachment from the scapula to the axial skeleton; its stability is provided by the surrounding musculature. These muscles can be divided into 3 major groups: the scapulothoracic muscles, which coordinate scapulothoracic motion; the rotator cuff muscles, which regulate activities of the glenohumeral articulation; and the scapulohumeral muscles, which provide power to the humerus.19 At rest, the scapula is rotated anteriorly approximately 30° relative to the trunk and is tilted forward about 20° in the sagittal plane when viewed from the side.36,37,69 This static position is commonly referred to as the “plane of the scapula.”14,24,65 During arm elevation, the first 30° of elevation occurs at the glenohumeral joint, whereas the next 60° of elevation is accomplished by equal contributions of scapulothoracic and glenohumeral motion.4,19,73 Therefore, although variations do exist among people, there is approximately a 2:1 ratio of glenohumeral:scapulothoracic motion with arm elevation to 90°.33
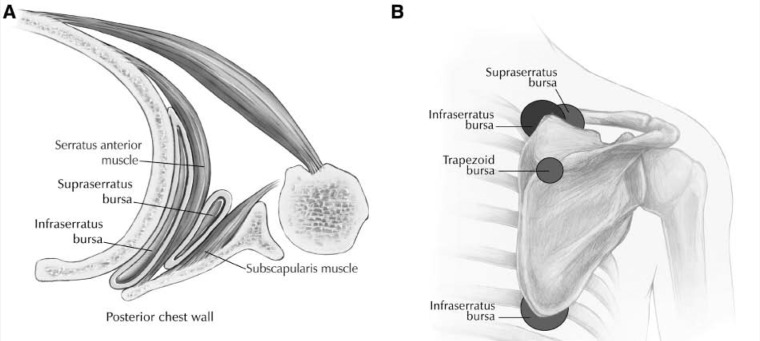
The scapulothoracic bursae are frequently neglected or incompletely discussed in standard anatomy texts.35 These bursae allow for smooth, gliding scapulothoracic motion. Two major (or anatomic) bursae and four minor (or adventitial) bursae have been described in the scapulothoracic articulation (Figure 1).14,33,75 The first major bursa, the infraserratus bursa, is located between the serratus anterior muscle and the chest wall. The second major bursa, the supraserratus bursa, is found between the subscapularis and serratus anterior muscles.35 The anatomic reproducibility of these bursae is well documented.75 However, minor bursae that have been identified are adventitial, arising as a response to abnormal biomechanics of the scapulothoracic articulation.59 Two have been described as lying at the superomedial angle of the scapula. A third site of pathoanatomy is at the inferior angle of the scapula and is considered by most authors to rest between the serratus anterior muscle and the chest wall. Finally, Codman14 believed that the fourth site of pathology, the trapezoid bursa, was the site of painful crepitus in scapulothoracic crepitus. This bursa is found over the triangular surface at the medial base of the spine of the scapula under the trapezius muscle.
Figure 1.
A, in this axial view of the scapulothoracic articulation, 2 major anatomic bursae can be seen: the supraserratus bursa and the infraserratus bursa; B, minor adventitial bursae of the scapulothoracic articulation are believed to develop in response to pathomechanics—they include 2 infraserratus bursae, a supraserratus bursa, and a trapezoid bursa.
Causes
The causes of scapulothoracic bursitis and crepitus include abnormalities of the bone, muscle, and bursae involved with scapulothoracic function (see Milch 1933 in Bergmann4). Carlson10 reviewed 89 cases of scapulothoracic crepitus. The most common causes included skeletal abnormalities (43%) and idiopathic causes (30%). These were followed by patients who had first rib resection (15%) and muscle or bursal changes (12%). Each cause leads to the common pathway of disruption of the normal motion between the anterior surface of the scapula and the underlying bony thorax.
As mentioned, several key bursae are thought to cause lesions in the scapulothoracic joint. These bursae can become inflamed secondary to trauma or overuse owing to sports activities or work.1,44 McCluskey and Bigliani43 reported on a series of 9 patients with refractory scapulothoracic bursitis, of which a traumatic episode was reported in 6. Trauma may be direct, as in injury from a motor vehicle accident, or indirect, as the result of a fall to an outstretched extremity that injures the soft tissues of the scapulothoracic articulation. Overuse syndromes—including those caused by overhead sports (eg, throwing, swimming, tennis) or any type of work that requires repetitive or constant movement of the scapula against the posterior chest wall—can irritate the infraserratus and supraserratus bursae. Furthermore, Sisto and Jobe67 deduced that symptoms in their group of major league baseball pitchers were due to a flaw in delivery technique and to repetitive irritation and pressure between the scapula and posterior thorax. This repetitive irritation can lead to chronic bursitis and inflammation. The bursa then undergoes scarring and fibrosis, leading to crepitus and pain.
Milch and Burman50 and Codman14 believed that an osseous lesion in the scapulothoracic space may lead to symptomatic scapulothoracic crepitus. The most common bony pathology in the scapulothoracic space that gives rise to scapulothoracic crepitus is the osteochondroma,48,50,56 which is the most common scapular tumor and can arise from the ribs or the scapula.17,49,56 The majority of osteochondromas occur as single lesions that project from either the anterior aspect of the scapula or the posterior thorax. “Pseudo-winging” of the scapula has been described in cases where a large osteochondroma forces apart the scapula and posterior chest wall. In addition, the superomedial and inferomedial angles of the scapula can be excessively long and hooked.50,60 Furthermore, the superomedial angle can have a bony prominence known as Luschka’s tubercle,70,72 which has been implicated as a source for scapulothoracic crepitus. Malunited fractures of the ribs or scapula can also cause symptoms.49,70 Researchers have also implicated reactive bone spurs that are created by the microtrauma of chronic, repeated periscapular muscle avulsions.34,62,71 Finally, it is important to realize that any bony pathology that causes scapulothoracic crepitus is capable of forming a reactive bursa around the area of pathology.16,66 In fact, at the time of resection of these bony lesions, a bursa is frequently identified.
Pathologic conditions affecting muscle in the scapulothoracic articulation include fibrotic muscle,8,48,74 muscle atrophy and edema,10 and anomalous muscle insertions.59,68 Muscle fibrosis from a previous traumatic event can cause symptoms. In addition, scapulothoracic crepitus has been reported with serratus anterior muscle atrophy secondary to long thoracic nerve palsy and with subscapularis atrophy secondary to glenohumeral fusion.77
Although rare, other soft tissue pathology has been implicated in scapulothoracic crepitus, including syphilitic or tuberculosis lesions49 and elastofibroma dorsi,45 a nonneoplastic soft tissue lesion on the chest wall. Several cases of subscapular elastofibroma have been implicated in causing scapular snapping in younger pitchers.23
Yet another source of scapulothoracic crepitus includes anatomic variances that can lead to scapulothoracic incongruence.18,76 For example, structural spinal deformities (eg, scoliosis and kyphosis) resulting in alterations of the scapulothoracic articulation have been implicated as causes of scapulothoracic crepitus.57
Diagnosis
Scapulothoracic bursitis and crepitus remain primarily clinical diagnoses. Clinical evaluation of the painful shoulder begins with a thorough history and physical examination. Patients most often complain of pain with increasing activity and may have audible and palpable crepitus with motion of the scapula. The crepitus associated with bursitis is usually much less intense than that which occurs with a bone lesion.35 Some patients have no pain,49 whereas others may have an extreme tenderness at the superior angle and medial border of the scapula.47,48,63,64,77 In severe cases, patients may report pain at rest. In addition, scapulothoracic crepitus is bilateral in some patients.7 A history of overuse during sports13,32,34,44,59,67 such as pitching, swimming, football, gymnastics, and weight training has been implicated in the onset of symptoms, as has work59 and local trauma.40,44 Furthermore, it is not uncommon for patients to complain of a sensation of fatigue before the onset of symptoms. Finally, some authors have suspected a familial tendency toward developing symptoms.13
Inspection of the scapula may reveal fullness or winging, which suggests a space-occupying lesion in the scapulothoracic space.35 Visual inspection may also reveal dyskinesis, an alteration of the normal position or motion of the scapulothoracic joint. As previously mentioned, the normal overall ratio of glenohumeral:scapulothoracic rotation is 2:1 throughout the full range of elevation. Defective patterns commonly observed include decreased glenohumeral motion with increased scapular motion during elevation, which may lead to a clinically apparent protrusion at the lateral border of the axilla.40 In addition, attention to the patient’s posture may reveal moderate to severe forward head position and rounded shoulders, which has been shown to contribute to scapular symptoms.54,77
Although the neuromuscular examination in patients with scapulothoracic bursitis and crepitus is often normal, assessment of muscle strength remains critical. Basic manual muscle testing26 should focus on the strength of the scapular muscles—including the trapezius (upper, middle, and lower), levator scapula, serratus anterior, latissimus dorsi, deltoids, and rotator cuff muscles. A loss of muscle tone or an alteration of scapulothoracic rhythm may lead to increased friction between the medial border of the scapula and the rib cage, resulting in crepitus or snapping.59
Manske et al40 suggested a thorough assessment of muscle flexibility and soft tissue tightness of the shoulder girdle. Chronic overuse or postures that hold the trapezius and levator scapulae in shortened positions can negatively affect scapular mechanics and function. The examiner can test the tightness of the trapezius by having the patient turn his or her head as much as possible toward the affected side, with his or her neck in slight extension. With the examiner standing behind the seated patient, the ipsilateral upper extremity is lifted from below the flexed elbow. This maneuver places slack on the upper trapezius and therefore allows further motion if the trapezius is the cause of limited motion. A tight pectoralis minor can also contribute to poor scapular mechanics. Tightness of the pectoralis minor causes the affected shoulder to rest in a more anterior position than that of the unaffected shoulder while the patient is supine.40 The tightness is usually the result of a tight glenohumeral capsule causing secondary impingement and subsequent protraction of the scapula. Mild cases demonstrate cuff impingement, whereas more severe cases show scapular dyskinesia. All patients have a loss of normal rotational arc of the shoulder, which is best demonstrated as a loss of internal rotation with the shoulder abducted 90° and the elbow bent 90°. Furthermore, tightness of the latissimus dorsi, pectoralis major, and rotator cuff muscles can lead to abnormal motion between the scapula and humerus.
Palpation or auscultation while putting the shoulder through a full range of motion may detect the source of periscapular crepitus. Palpation may also reveal localized tenderness over the inflamed area. The superomedial border of the scapula is the most common location, but the inferomedial border is also a site of the disorder. The best way to palpate the medial border of the scapula is to have the patient adduct and internally rotate the shoulder while touching the opposite scapula. The presence of a palpable mass, crepitus, prominence at rest, and normal scapulothoracic motion will help to delineate scapular winging owing to a mass versus a neurologic deficit.34
Injection of local anesthetic and corticosteroid may help to confirm the diagnosis. These injections may also prove therapeutic, which can further facilitate physical therapy and recovery.
After a complete history and physical examination, imaging studies may also be useful. Radiographs, computed tomography (CT), or magnetic resonance imaging (MRI) scans may identify anatomic pathology. An anteroposterior view and a tangential view (or Y view) should be obtained to detect osseous abnormalities. If these radiographic studies are negative and the examiner still suspects a bony abnormality, a CT scan may be helpful. Mozes et al52 recommended 3-dimensional CT scans for assessing bony incongruity between the anterior aspect of the scapula and chest wall in patients with symptomatic scapulothoracic crepitus. They discovered bony incongruity in 26 of 26 scapulae. Finally, an MRI can be used to identify a soft tissue lesion. It is especially helpful in identifying the size and location of an inflamed bursa. In severe cases, MRI can show fluid-filled regions, usually between the serratus anterior and chest wall, with high signal in T2-weighted images.25
Because focal muscle weakness or atrophy can play a role in idiopathic cases of scapulothoracic bursitis or crepitus, electrodiagnostic studies that include the shoulder girdle musculature should be considered.10 Electromyography and nerve conduction studies are also useful in determining whether the cause of scapular winging is due to a neurologic lesion.
The differential diagnosis of scapulothoracic bursitis and crepitus includes elastofibroma (which can be confirmed by MRI) and referred pain from the cervical spine or glenohumeral joint. Cervical spine problems at levels C5 to C8 can lead to pain in the periscapular region.6,39 Neer53 stated that problems in the glenohumeral joint can commonly cause referred pain in the scapula. Conditions of the glenohumeral joint that can lead to scapular pain include shoulder impingement and glenohumeral instability.21
Nonoperative Management
The initial treatment of scapulothoracic bursitis and scapulothoracic crepitus should be nonoperative. Nonoperative management seems to be most beneficial if a soft tissue disorder, altered posture, scapular dyskinesia, or scapular winging is the source of scapulothoracic crepitus.12,43,49 Initial treatment consists of rest, systemic nonsteroidal anti-inflammatory drugs, activity modification, and shoulder rehabilitation.
The planned rehabilitation program should be comprehensive and multifactorial, focusing on posture, strength, and endurance. As previously mentioned, postural dysfunction is an important contributor to the development of scapulothoracic crepitus. For those with aggravating factors such as kyphosis or scapular protraction,29 postural exercises designed to strengthen the upper thoracic musculature may prevent sloping of the shoulders.12,46 In addition, a figure-of-8 harness may be a useful tool to remind patients to attain normal posture.
Rehabilitation exercises should focus on strengthening the periscapular muscles and stretching their antagonist counterparts. Exercises that add physical bulk to the subscapularis and serratus anterior elevate the scapula further off the chest wall. This prevents “washboarding” of the scapula over the ribs, which can irritate the bursae. Furthermore, restoring periscapular strength establishes static proximal stability to provide a stable base.30 The periscapular muscles’ primary function is static posturing of the shoulder girdle (an activity of prolonged duration); therefore, endurance training should also be emphasized.40 Endurance training consists of low-intensity exercises with high volume. Hence, to simulate the true function of the scapular stabilizers during sporting or repetitive work activities, 15 to 20 repetitions with lighter loads should be performed. The rehabilitation protocol should progress along a continuum: from isometric and isotonic periscapular and rotator cuff strengthening to endurance eccentric strengthening of the periscapular muscles. Scapular core exercises—such as scaption (scapular plane elevation), rowing, press-up, and push-up plus (ie, a push-up with increased protraction of the scapula)—should be emphasized early on (Figure 2).51 Exercises can then be advanced to include plyometric exercises such as Plyoback (AliMed Inc, Dedham, Massachusetts), proprioceptive neuromuscular facilitation, and Swiss ball isometric-hold scapular stabilization exercises.40 Finally, attention must be given to strengthening of the core stabilizers (lumbar-pelvis-hip complex). A carefully designed rehabilitation program should continue for at least 3 to 6 months or until goals are met, with an emphasis on form and function. Failure to properly train the patient in functional activities can be a common reason for poor results.
Figure 2.

The rehabilitation protocol should include scapular core exercises such as scaption, or elevation in the scapular plane.
Other means of nonoperative management include local modalities, such as heat, massage, ultrasound, and ionophoresis. Ciullo and Jones12 used iontophoresis and ultrasound applied to the undersurface of the medial border of the scapula in combination with periscapular strengthening to treat symptomatic scapulothoracic crepitus. The application of ethyl chloride to trigger points has also been described.59 Sterile injection of corticosteroid and local anesthetics is also a viable option. The bursae can be injected safely and easily with the patient’s arm in a position of extension, adduction, and internal rotation trying to reach for the opposite scapula while prone (Figure 3). Caution must be used to stay in the proper plane parallel to the undersurface of the scapula, to reduce the risk of pneumothorax.7,61 As previously noted, a local injection can prove diagnostic as well as therapeutic.
Figure 3.
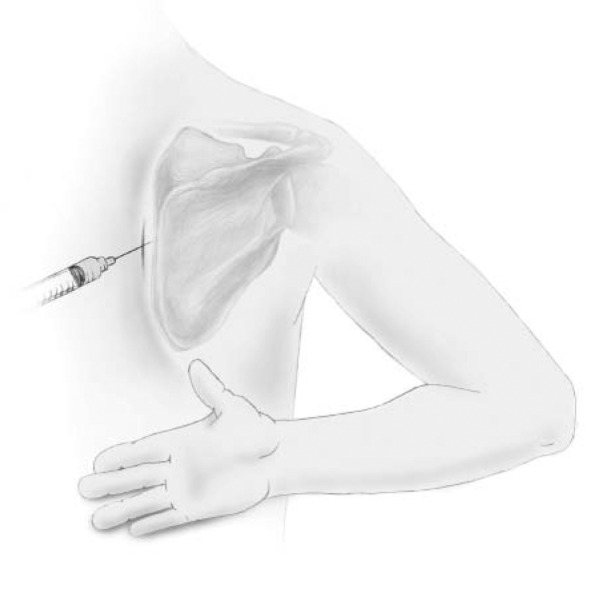
Scapulothoracic injection at the medial border of the scapula. The limb is placed in the “chicken wing” position.
Operative Management
Most patients improve with nonoperative measures, but for patients who fail nonoperative measures and for whom the diagnosis is certain, surgery may be beneficial. The decision for and timing of operative management should be individualized for each patient. Operative options include partial scapulectomy and open versus arthroscopic bursectomy. Most authors have recommended partial scapulectomy or resection of the superomedial angle of the scapula1,9,13,32,60,76 in patients with scapular crepitus and pain caused by bony incongruity. With the patient in the prone position, an incision is made over the medial spine of the scapula, and the soft tissue is dissected down to the spine (Figure 4). The periosteum over the spine is incised, and the supraspinatus, rhomboid, and levator scapulae are dissected in a subperiosteal fashion just to the edge of the scapular notch to avoid injury to the suprascapular nerves and vessels. The dissection is then carried around the medial edge of the scapula posteriorly to the undersurface of the scapula where the subscapularis and serratus are elevated subperiosteally from the region where the resection will occur. This technique allows placement of a protective retractor behind the scapula to control the depth of the saw. The exposed superomedial angle of the scapula is then resected with an oscillating saw, and the edges are smoothed with a rongeur. After the resection, the reflected muscles tend to fall back into place. The periosteum is reapproximated to the scapular spine by suturing through drill holes. Postoperatively, the patient is placed in a sling and begins immediate passive motion. Active motion is initiated at 8 weeks, followed by resistance exercises at 12 weeks. Overall, outcomes following this procedure are reportedly very good.1,13,32,60 For example, Arntz and Matsen1 reported complete relief of pain and crepitus in 12 of 14 shoulders (86%) with a 42-month follow-up after resection of the superomedial border of the scapula. Interestingly, the resected bone was noted to appear normal on gross and histologic inspection. This finding has prompted others to pursue bursectomy and avoid partial scapulectomy.67
Figure 4.
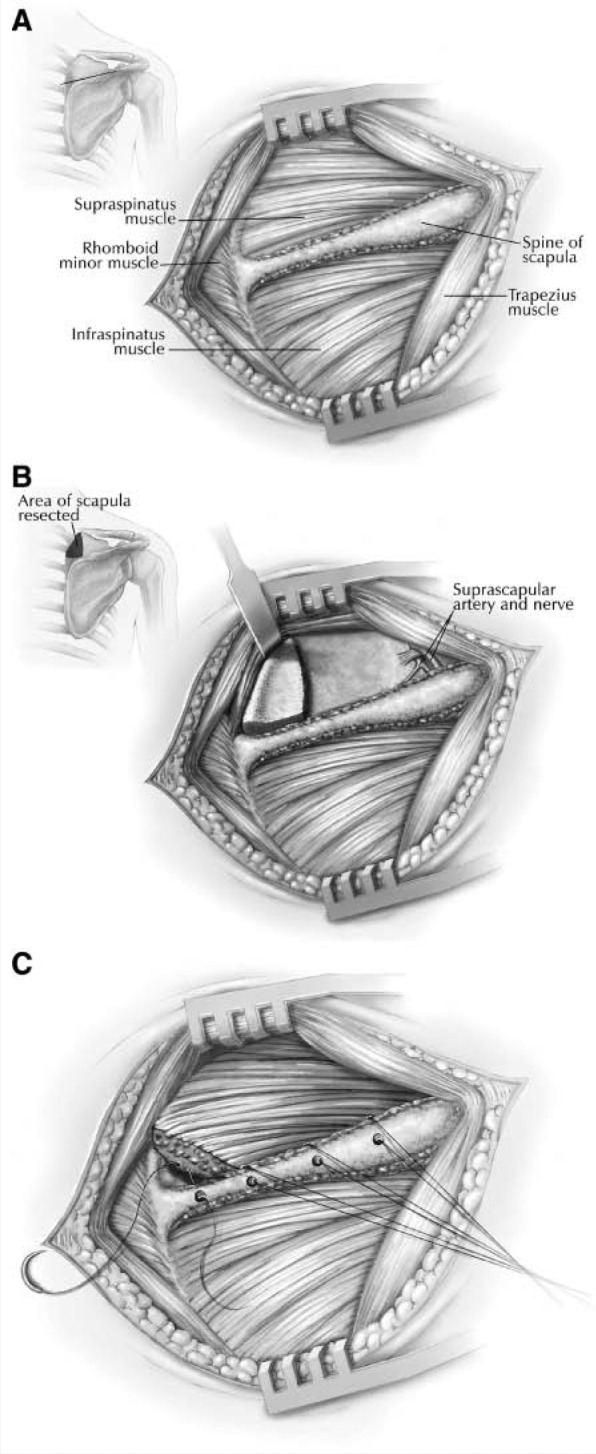
Resection of the superomedial border of the scapula: A, after an incision is made over the medial spine of the scapula, the trapezius muscle is elevated from the spine; B, the supraspinatus, rhomboids, and serratus muscles are reflected, and the superomedial angle of the scapula is resected; C, the supraspinatus is sutured through drill holes to the spine of the scapula.
Sisto and Jobe67 described an open technique for resecting the bursa at the inferior angle of the scapula. Their patients were 4 major league baseball pitchers who complained of pain during the early cocking, late cocking, and acceleration phases and could no longer pitch. Only 1 of the 4 pitchers demonstrated scapulothoracic crepitus, but all had a tender, palpable bursal sac at the inferior angle of the scapula (Figure 5). The pitchers did not respond to nonoperative management and underwent bursal excision through an oblique incision made just distal to the inferior angle of the scapula. The trapezius and latissimus muscles were split in line with their fibers, exposing the underlying bursa; the bursa was excised and any osteophytes were removed. The incision was closed with a drain and compression dressing, and physical therapy exercises were initiated after 1 week. Activity was increased, and all 4 pitchers were able to return to their previous level of pitching. McCluskey and Bigliani43,44 also described an open procedure to resect the superomedial bursa. With their technique, 8 of 9 patients (89%) with symptomatic scapulothoracic bursitis had good or excellent results. Nicholson and Duckworth55 performed open scapulothoracic bursectomy in a series of 17 patients with painful, unremitting scapulothoracic crepitus: 12 patients related a history of trauma and 5 had insidious onset of symptoms. At an average follow up of 2.5 years, each of the 17 patients reported resolution of the painful crepitus sensation, with a mean improvement of the American Shoulder and Elbow Surgeons score from 48 to 91.
Figure 5.
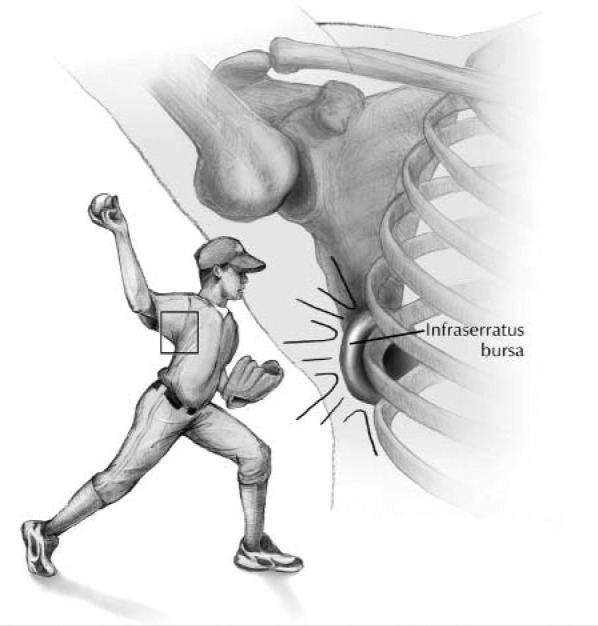
Development of an infraserratus bursa at the inferior angle of the scapula in a baseball pitcher.
Resection of the symptomatic scapulothoracic bursa has also been reported using an arthroscopic technique.12,20,31,38,41,58 Matthews et al41 described a technique in which a patient is placed in either the prone or lateral decubitus position with the free arm placed behind the back in the surgical “chicken wing” position. Portals are placed at least 2 cm medial to the vertebral border of the scapula to prevent injury to the dorsal scapular nerve (Figure 6). The initial portal is created using a spinal needle inserted midway between the scapular spine and inferior angle, and it is directed in the plane between the posterior thoracic wall and the serratus anterior. This bursal space can then be distended with at least 30 mL of saline before a stab wound is made and a blunt obturator is inserted. A 30° arthroscope is inserted, and under direct visualization, a superior and inferior portal can be made. The superior portal is usually placed just below the scapular spine, whereas the inferior portal lies 7 to 8 cm inferior to the spine. Portals placed superior to the scapular spine risk injury to neurovascular structures and should therefore be avoided.3 A motorized shaver or a monopolar radiofrequency cautery device is commonly used for debridement. One of the more common difficulties with arthroscopic surgery compared with open surgery relates to access and visualization of the superior angle of the scapula with standard portals. Chan et al11 described an alternative portal for scapulothoracic arthroscopy. They described an inside-out technique to create a superior portal that allows easier access to the superomedial border of the scapula.
Figure 6.
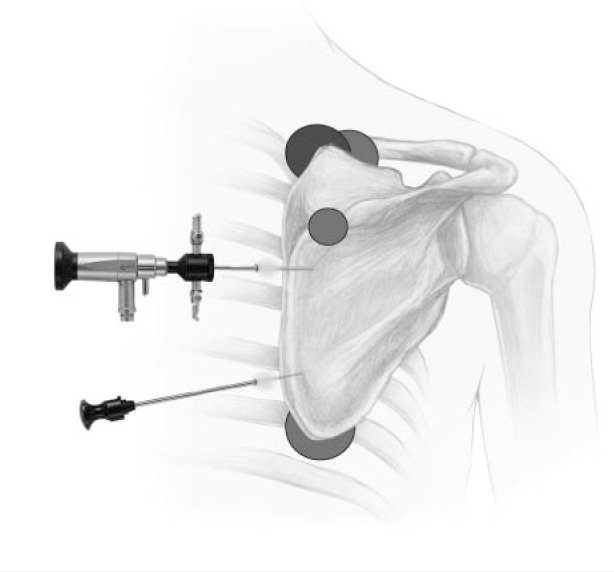
Portals used for bursectomy in arthroscopic treatment of scapulothoracic bursitis and crepitus.
Ciullo and Jones,12 in the largest published arthroscopic series to date, reported their results in 13 patients who underwent subscapular arthroscopy for painful scapulothoracic bursitis. They were able to resect fibrous adhesions in the supraserratus and infraserratus bursae as well as any abnormal bony prominences through the arthroscope. All 13 patients returned to their preinjury activity levels.
The results of arthroscopic bursectomy in 25 patients with scapulothoracic bursitis who did not respond to nonoperative treatment were recently presented (C. L. Baker, MD, unpublished data, October 2008). On average, the patients were 40 years old (range, 15 to 77) and the duration of symptoms was 48 months (range, 2 to 240 months). Seven patients had surgery on the affected shoulder. At a mean follow-up of 22 months, patients improved from an average preoperative UCLA Shoulder Score of 16.3 to a postoperative score of 28.6 (> 27, good/excellent; < 27, fair/poor). Of the 18 patients who responded to their questionnaire, 11 would “definitely have the surgery again”; 1, “probably”; 4, maybe; 1, “likely not”; 1, “definitely not.” Preliminary data from this study show the procedure to be effective as an isolated procedure but not as an adjunct in the multiply operated shoulder with global pain.
The complications associated with open or arthroscopic bursectomy include pneumothorax, postoperative hematoma, potential long thoracic nerve injury, potential damage to the dorsal scapular nerve, and recurrence of the bursitis.34 Despite the lack of agreement among orthopaedic surgeons concerning which procedure is best for treating symptomatic scapulothoracic bursitis and crepitus, most reports have shown good to excellent outcomes in a significantly high percentage of patients.40 Most patients returned to sports or work within 4 months, usually after thoracic posture, scapular control, and strength were obtained with rehabilitation.
Summary
The importance of the scapulothoracic articulation has gained attention as of late, and our understanding of symptomatic scapulothoracic bursitis and crepitus continues to evolve. These are conditions commonly seen by sports medicine clinicians, athletic trainers, and physical therapists. Clearly, the best initial approach is a nonoperative treatment plan that combines scapular strengthening, postural reeducation, and core strength endurance. The addition of local modalities, nonsteroidal anti-inflammatory drugs, and localized injections may also be helpful. If an appropriate trial of nonoperative management proves unsuccessful, surgical correction can produce good results.
Footnotes
No potential conflict of interest declared.
References
- 1. Arntz CT, Matsen FA. Partial scapulectomy for disabling scapulo-thoracic snapping. Orthop Trans. 1990;14:252-253 [Google Scholar]
- 2. Bateman JE. The Shoulder and Neck. 2nd ed. Philadelphia, PA: WB Saunders; 1978:185-194 [Google Scholar]
- 3. Bell SN, van Riet RP. Safe zone for arthroscopic resection of the superomedial scapular border in the treatment of snapping scapula syndrome. J Shoulder Elbow Surg. 2008;17:647-649 [DOI] [PubMed] [Google Scholar]
- 4. Bergmann G. Biomechanics and pathomechanics of the shoulder joint with reference to prosthetic joint replacement. In: Kolbel R, Helbig B, Blauth W, eds. Shoulder Replacement. Berlin: Springer-Verlag; 1987:33-43 [Google Scholar]
- 5. Boinet W. Bulletin de la Societe Imperiale de Chirurgie dr Paris. 2nd ser. 1867;8:458 [Google Scholar]
- 6. Brown C. Compressive, invasive referred pain to the shoulder. Clin Orthop Relat Res. 1983;173:55-62 [PubMed] [Google Scholar]
- 7. Butters KP. The scapula. In: Rockwood CA, Matsen F, III, eds. The Shoulder. Philadelphia, PA: WB Saunders; 1990:335-366 [Google Scholar]
- 8. Butters KP. The scapula. In: Rockwood CA, Matsen F, III, eds. The Shoulder. 2nd ed. Philadelphia, PA: WB Saunders; 1998:391-427 [Google Scholar]
- 9. Cameron H. Snapping scapulae: a report of three cases. Eur J Rheumatol Inflamm. 1984;7:66-67 [PubMed] [Google Scholar]
- 10. Carlson HL, Haig AJ, Stewart DC. Snapping scapula syndrome: three case reports and an analysis of the literature. Arch Phys Med Rehabil. 1997;78:506-511 [DOI] [PubMed] [Google Scholar]
- 11. Chan B-K, Chakrabarti AJ, Bell SN. An alternative portal for scapulothoracic arthroscopy. J Shoulder Elbow Surg. 2002;11:235-238 [DOI] [PubMed] [Google Scholar]
- 12. Ciullo JV, Jones E. Subscapular bursitis: conservative and endoscopic treatment of “snapping scapula” or “washboard syndrome.” Orthop Trans. 1992-1993;16:740 [Google Scholar]
- 13. Cobey MC. The rolling scapula. Clin Orthop Relat Res. 1968;60:193-194 [PubMed] [Google Scholar]
- 14. Codman EA. The anatomy of the human shoulder. In: Codman EA, ed. The Shoulder. Suppl ed. Malabar, FL: Kreiger; 1984:1-31 [Google Scholar]
- 15. Codman EA. Rupture of the supraspinatus tendon and other lesions in or about the subdeltoid bursa. In: Codman EA, ed. The Shoulder. Suppl ed. Malabar, FL: Krieger; 1984:123-177 [Google Scholar]
- 16. Cuomo F, Blank K, Zuckerman JD, Present DA. Scapular osteochondroma presenting with exostosis bursata. Bull Hosp Joint Dis. 1993;52:55-58 [PubMed] [Google Scholar]
- 17. DeMarquay J. Exostosis of rib. In: Dictionaire de Medicine et de Chirugie Practique. Paris: Baillière; 1868 [Google Scholar]
- 18. Edelson JG. Variations in the anatomy of the scapula with reference to the snapping scapula. Clin Orthop Relat Res. 1996;322:111-115 [PubMed] [Google Scholar]
- 19. Freedman L, Munro RH. Abduction of the arm in scapular plane: scapular and glenohumeral movements. J Bone Joint Surg Am. 1966;18:1503. [PubMed] [Google Scholar]
- 20. Gillogly SD, Bizousky DT. Arthroscopic evaluation of the scapulothoracic articulation. Orthop Trans. 1992-1993;16:196 [Google Scholar]
- 21. Glousman R, Jobe FW, Tibone JE, Moynes D, Antonelli D, Perry J. Dynamic electromyographic analysis of the throwing shoulder with glenohumeral instability. J Bone Joint Surg Am. 1988;70:220-226 [PubMed] [Google Scholar]
- 22. Grünfeld G. Beitrag zur Genese des Skapularkrachens und der Skapulargeräusche. Arch Orthop. 1927;24:610-615 [Google Scholar]
- 23. Haney TC. Subscapular elastofibroma in a young pitcher: a case report. Am J Sports Med. 1990;18:642-644 [DOI] [PubMed] [Google Scholar]
- 24. Johnston TB. The movements of the shoulder joint: a plea for the use of the plane of the scapula as the plane of reference in movements occurring at the humero-scapular joint. Br J Surg. 1937;25:252 [Google Scholar]
- 25. Ken O, Hatori M, Kokubun S. The MRI features and treatment of scapulothoracic bursitis: report of four cases. Ups J Med Sci. 2004; 109:57-64 [DOI] [PubMed] [Google Scholar]
- 26. Kendall FP, McCreary EK, Provance PG. Muscles Testing and Function. 4th ed. Baltimore, MD: Williams & Wilkins; 1993:81 [Google Scholar]
- 27. Kibler WB. Role of the scapula in the overhead throwing motion. Contemp Orthop. 1991;22:525-532 [Google Scholar]
- 28. Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26:325-337 [DOI] [PubMed] [Google Scholar]
- 29. Kisner C, Colby LA. Therapeutic Exercise: Foundation and Techniques. 4th ed. Philadelphia, PA: FA Davis; 2002 [Google Scholar]
- 30. Knott M, Voss D. Proprioceptive Neuromuscular Facilitation. New York: Harper & Row, 1968 [Google Scholar]
- 31. Kolodychuk LB, Regan WD. Visualization of the scapulothoracic articulation using an arthroscope: a proposed technique. Orthop Trans. 1993-1994;17:1142 [Google Scholar]
- 32. Kouvalchouk JF. Subscapular crepitus. Orthop Trans. 1985;9:587-588 [Google Scholar]
- 33. Kuhn JE. The scapulothoracic articulation: anatomy, biomechanics, pathophysiology, and management. In: Iannotti JP, Williams GR, eds. Disorders of the Shoulder: Diagnosis and Management. Philadelphia, PA: Lippincott Williams & Wilkins; 1999:817-845 [Google Scholar]
- 34. Kuhn JE. The scapulothoracic articulation: anatomy, biomechanics, pathophysiology, and management. In: Iannotti JP, Williams GR, eds. Disorders of the Shoulder: Diagnosis and Management. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2006:1057-1086 [Google Scholar]
- 35. Kuhn JE, Plancher KD, Hawkins RJ. Symptomatic scapulothoracic crepitus and bursitis. J Am Acad Orthop Surg. 1998;6:267-273 [DOI] [PubMed] [Google Scholar]
- 36. Laumann U. Kinesiology of the shoulder joint. In: Kolbel R, Helbig B, Blauth W, eds. Shoulder Replacement. Berlin: Springer-Verlag; 1987:23-31 [Google Scholar]
- 37. Lewitt K. Manipulative Therapy in Rehabilitation of the Locomotor System. London: Butterworth-Heinemann, 1985 [Google Scholar]
- 38. Lehtinen JT, Macy JC, Cassinelli E, Warner JJ. The painful scapulothoracic articulation: surgical management. Clin Orthop Relat Res. 2004;423: 99-105 [DOI] [PubMed] [Google Scholar]
- 39. Makin GJ, Brown WF, Ebers GC. C7 radiculopathy: importance of scapular winging in clinical diagnosis. J Neurol Neurosurg Psychiatry. 1986;49:640-644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Manske RC, Reiman MP, Stovak ML. Nonoperative and operative management of snapping scapula. Am J Sports Med. 2004;32:1554-1565 [DOI] [PubMed] [Google Scholar]
- 41. Matthews LS, Poehling GC, Hunter DM. Scapulothoracic endoscopy: anatomical and clinical considerations. In: McGinty JB, Caspari RB, Jackson RW, Poehling GG, eds. Operative Arthroscopy. 2nd ed. Philadelphia, PA: Lippincott-Raven; 1996:813-820 [Google Scholar]
- 42. Matthews LS, Yurkofsky JB. Scapulothoracic endoscopy: anatomic, clinical, and surgical perspectives. In: Chow JCY, ed. Advanced Arthroscopy. New York, NY: Springer; 2001:141-146 [Google Scholar]
- 43. McCluskey GM, Bigliani LU. Partial scapulectomy for disabling scapulothoracic snapping. Orthop Trans. 1990;14:252-253 [Google Scholar]
- 44. McCluskey GM, Bigliani LU. Scapulothoracic disorders. In: Andrews JR, Wilk KE, eds. The Athlete’s Shoulder. New York, NY: Churchill Livingstone; 1994:305-316 [Google Scholar]
- 45. Majó J, Gracia I, Doncel A, Valera M, Núñez A, Guix M. Elastofibroma dorsi as a cause of shoulder pain or snapping scapula. Clin Orthop Relat Res. 2001;388:200-204 [DOI] [PubMed] [Google Scholar]
- 46. Michele AA, Davies JJ, Krueger FJ, Lichtor JM. Scapulocostal symdrome (fatigue-postural paradox). N Y State J Med. 1950;50:1353-1356 [PubMed] [Google Scholar]
- 47. Michele AA, Eisenberg J. Scapulocostal syndrome. Arch Phys Med Rehabil. 1968;49:383-387 [PubMed] [Google Scholar]
- 48. Milch H. Partial scapulectomy for snapping of the scapula. J Bone Joint Surg Am. 1950;32:561-566 [PubMed] [Google Scholar]
- 49. Milch H. Snapping scapula. Clin Orthop Relat Res. 1961;20:139-150 [PubMed] [Google Scholar]
- 50. Milch H, Burman MS. Snapping scapula and humerus varus: report of six cases. Arch Surg. 1933;26:570-588 [Google Scholar]
- 51. Moseley JB, Jobe FW, Pink M, Perry J, Tibone J. EMG analysis of the scapular muscles during a shoulder rehabilitation program. Am J Sports Med. 1992;20:128-134 [DOI] [PubMed] [Google Scholar]
- 52. Mozes G, Bickels J, Ovadia D, Dekel S. The use of three-dimensional computed tomography in evaluating snapping scapula syndrome. Orthopedics. 1999;22:1029-1033 [DOI] [PubMed] [Google Scholar]
- 53. Neer C. Shoulder Reconstruction. Philadelphia, PA: WB Saunders; 1990:421-485 [Google Scholar]
- 54. Nevaiser RJ. Painful conditions affecting the shoulder. Clin Orthop Relat Res. 1983;173:63-69 [PubMed] [Google Scholar]
- 55. Nicholson GP, Duckworth MA. Scapulothoracic bursectomy for snapping scapula syndrome. J Shoulder Elbow Surg. 2002;11:80-85 [DOI] [PubMed] [Google Scholar]
- 56. Parsons TA. The snapping scapula and subscapular exostoses. J Bone Joint Surg Br. 1973;55:345-349 [PubMed] [Google Scholar]
- 57. Pavlick A, Ang K, Coghlan J, Bell S. Arthroscopic treatment of painful snapping of the scapula by using a new superior portal. Arthroscopy. 2003;19:608-612 [DOI] [PubMed] [Google Scholar]
- 58. Pearse EO, Bruguera J, Massoud SN, Sforza G, Copeland SA, Levy O. Arthroscopic management of the painful snapping scapula. Arthroscopy. 2006;22:755-761 [DOI] [PubMed] [Google Scholar]
- 59. Percy EC, Birbrager D, Pitt MJ. Snapping scapula: a review of the literature and presentation of 14 patients. Can J Surg. 1988;31:248-250 [PubMed] [Google Scholar]
- 60. Richards RR, McKee MD. Treatment of painful scapulothoracic crepitus by resection of the superomedial angle of the scapula: a report of three cases. Clin Orthop Relat Res. 1989;247:111-116 [PubMed] [Google Scholar]
- 61. Rockwood CA, Matsen FW. The Shoulder. 2nd ed. Philadelphia, PA: WB Saunders; 2000 [Google Scholar]
- 62. Roldan R, Warren D. Abduction deformity of the shoulder secondary to fibrosis of the central portion of the deltoid muscle: proceedings of the American Academy of Orthopaedic Surgeons. J Bone Joint Surg Am. 1972;54:1332 [Google Scholar]
- 63. Rose DI, Novak EJ. The painful shoulder: the scapulocostal syndrome in shoulder pain. J Kans Med Soc. 1966;67:112-114 [PubMed] [Google Scholar]
- 64. Russek AS. Diagnosis and treatment of scapulocostal syndrome. J Am Med Assoc. 1952;150:25-27 [DOI] [PubMed] [Google Scholar]
- 65. Saha AK. Mechanism of shoulder movements and a plea for the recognition of “zero position” of glenohumeral joint. Indian J Surg. 1950;12:153-165 [PubMed] [Google Scholar]
- 66. Shogry ME, Armstrong P. Case report 630: reactive bursa formation surrounding an osteochondroma. Skeletal Radiol. 1990;19:465-467 [DOI] [PubMed] [Google Scholar]
- 67. Sisto DJ, Jobe FW. The operative treatment of scapulothoracic bursitis in professional pitchers. Am J Sports Med. 1986;14:192-194 [DOI] [PubMed] [Google Scholar]
- 68. Ssoson-Jaroschewitsch JA. Uber skapularkrachen. Langenbecks Arch Klin Chir Ver Dtsch Z Chir. 1923;123:378 [Google Scholar]
- 69. Steindler A. Kinesiology of the Human Body under Normal and Pathological Conditions. Springfield, IL: Charles C Thomas; 1955 [Google Scholar]
- 70. Steindler A. Traumatic Deformities and Disabilities of the Upper Extremity. Springfield, IL: Charles C Thomas; 1946:112-118 [Google Scholar]
- 71. Strizak AM, Cowen MH. The snapping scapula syndrome. J Bone Joint Surg Am. 1982;64:941-942 [PubMed] [Google Scholar]
- 72. Von Luschka H. Uber ein costo-scapular-gelenk des menschen. Vierteljahrsheft fur die Prakrische Heilkunde. 1870;107:51-57 [Google Scholar]
- 73. Walker PS. Human joints and their artificial replacements. Springfield, IL: Charles C Thomas; 1977 [Google Scholar]
- 74. Weeks LE. Scapular winging due to serratus anterior avulsion fracture. Orthop Trans. 1993;17:184 [Google Scholar]
- 75. Williams GR, Shakil M, Klimkiewicz J, Iannotti JP. Anatomy of the scapulothoracic articulation. Clin Orthop Relat Res. 1999;359:237-246 [DOI] [PubMed] [Google Scholar]
- 76. Wood VE, Marchinski L. Congenital anomalies of the shoulder. In: Rockwood CA, Matsen FA, eds. The Shoulder. Philadelphia, PA: WB Saunders; 1990:98-148 [Google Scholar]
- 77. Wood VE, Verska JM. The snapping scapula in association with the thoracic outlet syndrome. Arch Surg. 1989;124:1335-1337 [DOI] [PubMed] [Google Scholar]