Abstract
Context:
Exercise-associated muscle cramps (EAMC) are a common condition experienced by recreational and competitive athletes. Despite their commonality and prevalence, their cause remains unknown. Theories for the cause of EAMC are primarily based on anecdotal and observational studies rather than sound experimental evidence. Without a clear cause, treatments and prevention strategies for EAMC are often unsuccessful.
Evidence Acquisition:
A search of Medline (EBSCO), SPORTDiscus, and Silverplatter (CINHAL) was undertaken for journal articles written in English between the years 1955 and 2008. Additional references were collected by a careful analysis of the citations of others’ research and textbooks.
Results:
Dehydration/electrolyte and neuromuscular causes are the most widely discussed theories for the cause of EAMC; however, strong experimental evidence for either theory is lacking.
Conclusions:
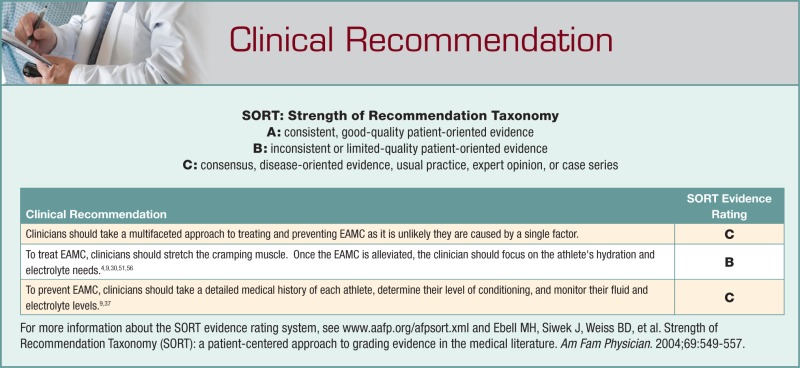
EAMC are likely due to several factors coalescing to cause EAMC. The variety of treatments and prevention strategies for EAMC are evidence of the uncertainty in their cause. Acute EAMC treatment should focus on moderate static stretching of the affected muscle followed by a proper medical history to determine any predisposing conditions that may have triggered the onset of EAMC. Based on physical findings, prevention programs should be implemented to include fluid and electrolyte balance strategies and/or neuromuscular training.
Keywords: cramping, dehydration, electrolytes, fatigue, stretching
Skeletal muscle cramps that occur during or shortly following exercise in healthy individuals with no underlying metabolic, neurological, or endocrine pathology have been termed exercise-associated muscle cramps (EAMC).51 Though controversial, an important differentiation in determining the cause of EAMC may be the number and location of muscles affected. EAMC typically occur in single, multijoint muscles (eg, triceps surae, quadriceps, hamstrings) when contracting in a shortened state,51 whereas generalized EAMC occur in multiple, usually bilateral muscles. Clinically, EAMC may be recognized by acute pain, stiffness, visible bulging or knotting of the muscle, and possible soreness that can last for several days.37,40 Although EAMC can be isolated, athletes often complain of EAMC symptoms up to 8 hours after exercise.18 This postexercise period of increased susceptibility to EAMC has been termed the cramp prone state.50 Although some EAMC do not appear to affect athletic performance,38,52 other times, EAMC can be completely debilitating.11,41
The clinical presentation of EAMC is easily recognized, but its cause continues to be unresolved. A better understanding of the underlying mechanisms causing EAMC may allow better prevention and treatments, thus reducing the incidence rate. Norris et al43 reported that 95% of physical education students (115 of 121) had experienced spontaneous cramps in their lifetimes with 26% (31 of 121) experiencing cramps after exercise. Kantarowski et al32 reported that 67% of triathletes (1631 of 2438) complained of EAMC under a variety of training conditions. More recently, a subset of American football players who experienced exertional heat illness reported concomitant skeletal muscle cramping.16 Thus, EAMC are common in both the recreational and the competitive athlete.
Although EAMC are common in athletes, the cause is unknown and controversial.8,50,51 Traditionally thought to be caused by factors associated with exercise in hot and humid environments (eg, dehydration and/or electrolyte imbalances),8 evidence suggests a neuromuscular cause.51 The inference from several studies is that EAMC have a singular, unknown cause.3,35,50,51 Authors have also suggested that there may be different kinds of EAMC and thus different causes (eg, isolated and generalized).8 Without a clear cause, the treatments and prevention strategies for EAMC vary considerably and have limited perceived effectiveness by health professionals.56 One approach to determining cause and the effectiveness of treatments is to examine the published studies and determine their level of evidence.
Theories for the Cause of EAMC
The dehydration–electrolyte imbalance theory is the most common among health care professionals.56 Proponents state that because the body does not store enough water for exercise46 and athletes do not ingest enough water to replace the amounts they lose during exercise,23 EAMC are the result of fluid and electrolyte depletion, which results in the sensitization of select nerve terminals.34 The resulting contracture of the interstitial space increases the mechanical pressure on select motor nerve endings and finally results in EAMC.8,34 Exercise in hot and humid conditions exacerbates the amount of fluid and electrolytes lost, thereby facilitating cramps.
Support for the dehydration–electrolyte imbalance theory comes mainly from research classified as level 4 and 5 evidence. Miners develop cramps because of their sweat losses while working in hot and humid conditions.41,60 More recently, researchers observed that the majority of cramping (95%, 87 of 92) occurred in hot months—specifically, when football players exercised in environmental conditions in which the risk of developing heat illness was “high” or “extreme.”16 Other evidence for this theory comes from case studies and other observational work in which large sweat losses occurred in exercising athletes.6,7,54 Some health professionals postulate that sweat glands are unable to reabsorb sodium at “high” sweat rates.20 The prevailing belief is that EAMC are a warning sign of dehydration–electrolyte imbalance.21
The dehydration–electrolyte imbalance theory does not, however, explain EAMC in athletes exercising in cool,29 temperature-controlled environments.6 For example, Maughan38 reported that marathoners (18%, 15 of 82) still developed EAMC even though the ambient temperature was 10 to 12°C. Thus, it is unlikely that a hot and humid environment is required for the development of EAMC, although they may occur more frequently under conditions of elevated ambient temperatures.16
Regarding fluid losses in crampers and noncrampers, plasma volume losses in runners with EAMC (5.2%) were not significantly different from those of runners without EAMC (4.4%), nor were losses in blood volume (1.7% vs 1.3%) or body weight.38 Moreover, sweat rate and sodium/fluid losses are often not different in athletes who develop EAMC.2,22,54,57 Finally, a correlation between body weight losses and EAMC has not been established in several groups of athletes.32,52,57
The treatment for EAMC also fails to support the dehydration–electrolyte imbalance theory. If EAMC were due to dehydration, the simple cure would be fluid replacement. However, when carbohydrate-electrolyte fluids were ingested at a rate that matched sweat loss, EAMC still occurred in 69% of athletes (9 of 13).30 Moreover, athletes who develop EAMC often ingest similar amounts of fluid during exercise as do their noncramping counterparts.54 Oral fluid ingestion may be ineffective, and intravenous fluid may provide a faster delivery for athletes suffering from acute EAMC.22 It is interesting that stretching the affected muscle almost immediately relieves EAMC51 and yet has no effect on the fluid conditions of the body.
Overall, the dehydration–electrolyte imbalance theory has limitations: First, inferences of cause and effect cannot be made from observational data (eg, field studies); causation may be inferred only from meta-analyses and randomized, experimental research designs (evidence levels 1 and 2, respectively).45 Second, although EAMC may appear in the presence of significant electrolyte and/or fluid losses during exercise, numerous other variables associated with exercise may be factors (eg, accumulation of metabolites, intensity of exercise, and acclimatization). Because athletes who experience EAMC often have significant fluid deficits,54 restoring body fluids is an appropriate precautionary measure against the development of more serious forms of heat illness (eg, exertional hyponatremia, heat stroke).
The neuromuscular theory of EAMC proposes that muscle overload and neuromuscular fatigue cause an imbalance between excitatory impulses from muscle spindles and inhibitory impulses from Golgi tendon organs (GTOs). These localized EAMC tend to occur when the muscle is contracting in an already-shortened position.51 The reduced tension in the muscle tendon likely reduces the inhibitory feedback from GTO afferents, thereby predisposing the muscle to cramp from the imbalance between inhibitory and excitatory drives to the alpha motor neuron.33 This enhanced excitability at the spinal level results in an increase in alpha motor neuron discharge to the muscle fibers, producing a localized muscle cramp.51
Study designs that examine the plausibility of the neuromuscular system’s role in EAMC are stronger than those for dehydration (levels 3 to 5): animal,28,42 exercising humans,43,51 and stretching for EAMC.27,52 These varying models and treatment observations are more consistent with the neuromuscular theory than with the dehydration–electrolyte imbalance theory.
In felines, muscle spindle42 and GTO28 activity were measured following neuromuscular fatigue induced by supramaximal stimulation (100 Hz). Fifty percent of type Ia (25 of 49) and 55% of IIa (18 of 33) muscle spindle afferents increased their resting discharge following fatiguing electrical stimulation.42 Similarly, feline GTO discharge rate was lowered and delayed with fatigue induced with a similar protocol.28 Thus, neuromuscular fatigue appeared to decrease the inhibition from the GTO and increase the excitatory stimuli from muscle spindles. These effects may result in a heightened excitatory state at the spinal level.
In humans, EAMC occurs more frequently at the end of competitions and physical work32,38,41 and when the muscle contracts while it is already shortened.51 Stretching, the primary treatment for acute EAMC,56 is thought to relieve EAMC via autogenic inhibition. Stretching increases the tension in the muscle’s tendon, resulting in GTO activation and an increase in inhibition of the alpha motor neuron, which may restore the physiological relationship between excitatory and inhibitory impulses to the alpha motor neuron.50
The neuromuscular theory also has limitations. The report of altered muscle spindle and GTO activity relies on difficult methodologies that have produced inconsistent results. The majority of GTO Ib afferents (5 of 8, 63%) have only a slight decline or no change in firing in response to stretching of a fatigued muscle.26 Neuromuscular fatigue often induces muscle afferent fatigue with supramaximal electrical stimulation (eg, 100 Hz).28,42 Normal human muscle recruitment patterns indicate stimulation frequencies much lower (eg, < 30 Hz) than those used to induce fatigue in animal studies (eg, 100 Hz).48 Low electrical stimulation frequencies closer to normal recruitment patterns (eg, 16 to 32 Hz) have successfully induced cramps in humans.39,53,55 Thus, the frequencies used to support the neuromuscular theory28,42 do not match normal neuromuscular signaling in humans. Finally, it is unclear how fatigued a muscle needs to become for an EAMC to occur or whether the neuromuscular fatigue is occurring peripherally (ie, in the muscle) and/or centrally (in the spinal cord or brain). Moreover, it is unlikely that neuromuscular fatigue induced with electrical stimulation is the same as fatigue induced with volitional muscle contractions, given that larger diameter motor neurons/units are stimulated first with electrical stimulation and last with volitional contractions.10,24 Muscle fatigue is a continuum rather than an absolute condition. It is likely that the degree of fatigue required to elicit cramping is unique to each athlete.
Because EAMC occur in a variety of situations, environmental conditions, and populations, it is unlikely that a single factor (eg, dehydration, electrolyte imbalance, or neuromuscular factors) is responsible for causing them directly. It is more likely that EAMC are due to a combination of factors that simultaneously occur under specific physiological circumstances in each athlete.
Treatment of EAMC
The paucity of experimental data regarding the cause of EAMC has led to a plethora of treatments for EAMC, confirming the lack of understanding and consensus for EAMC etiology. Many of these treatment options are anecdotal and unsupported by experimental research: ingesting mustard, pickle juice, sports drinks, cryotherapy, thermotherapy, massage, decreasing exercise intensity, body position, intravenous infusion, and TENS (transcutaneous electric nerve stimulation) therapy.
The dehydration–electrolyte theory suggests that ingesting fluids containing electrolytes is beneficial to treat and alleviate EAMC. However, owing to the minimal amount of electrolytes in many sports drinks, it may be difficult to sufficiently replace the volume of electrolytes lost during exercise even if the athlete has modest sweat losses and sweat sodium content. Assuming that a relationship between dehydration–electrolyte imbalance and EAMC exists, the National Athletic Trainers’ Association recommends that athletes prone to muscle cramping add 0.3 to 0.7 g/L of salt to their drinks to stave off muscle cramps.9 Others have recommended adding higher amounts of sodium (about 3.0 to 6.0 g/L) to sports drinks based on the frequency of EAMC.5 Note that fluids and electrolytes are not absorbed immediately after ingestion; that is, even hypotonic fluids require at least 13 minutes to be absorbed into the circulatory system.61 Theoretically, intravenous infusion of fluids removes this delay, and it has been used to aid athletes who develop acute EAMC.22 However, experimental evidence regarding the effectiveness of intravenous fluid infusion on EAMC is still lacking.
Stretching, quinine, and beta-blockers have stronger levels of evidence (level 2 or 3) to support their use, based on drug trials with human participants19,44 and other research.36,51 If the athlete has no underlying illness, then the most common treatment for EAMC is stretching,56 which has proven to be effective for EAMC and other types of muscle cramps1,17,37,51,52 but may be ineffective for “heat cramps.”4 Therefore, moderate stretching of the affected muscle to alleviate the cramp is recommended.
Once a cramp is alleviated, health care providers should determine what factors may be involved (eg, diabetes mellitus, thyroid disease).47
Prevention of EAMC
Despite the lack of direct evidence, maintaining hydration and adequate electrolyte levels is a good prevention strategy for individuals susceptible to EAMC.56 Fluid volumes of 1.8 L per hour have been well tolerated by tennis athletes who are susceptible to EAMC.6 Health professionals should monitor each athlete’s fluid losses and recommend replacement during and after exercise (eg, obligatory fluid losses). Both the National Athletic Trainers’ Association and the American College of Sports Medicine recommend a volume of fluid that allows for less than a 2% body weight reduction.13,49 Monitoring an athlete’s body weight is an easy method of ensuring adequate fluid replacement and individualizes each athlete’s fluid needs.13
An athlete who ingests a liter of water or hypotonic sports drink at least 1 hour before competition can be confident that the majority of the fluid, electrolytes, and nutrients have been absorbed and are available in the body. Fluids should be available and easily accessible throughout practices and competitions. A balanced diet is important given that much of fluid and electrolyte replacement occurs during meals.12
A common perception is that level of conditioning is a factor in the development of EAMC.24,28,44 There is a strong theoretical basis for performing exercises that target the neuromuscular system to prevent EAMC.25,31,58 Prevention exercises that target muscle spindle and GTO receptors should be implemented to delay neuromuscular fatigue onset and, hence, EAMC. Plyometric exercises may be beneficial to elicit neural adaptations in muscle spindle and GTO receptor firing, enhancing efficiency and sensitivity of reflexive and descending pathways used for neuromuscular control.14,59,62 Endurance training may also serve as an effective means of preventing EAMC by expanding plasma volume and the extracellular fluid compartment15 and delaying neuromuscular fatigue.25
Summary
EAMC are common and affect several different populations. Despite the prevalence of EAMC, few experimental data exist on their cause, treatment, and prevention. Although several theories have been postulated for their cause, much of the evidence is nonscientific or observational; thus, causation cannot be inferred. Numerous untested, anecdotal prevention strategies exist for the prevention of EAMC (eg, pickle juice). The level of evidence for these prevention strategies is low (level 4 or 5). It is likely that the cause of EAMC is multifactorial. Stretching appears to be effective regardless of the cause of EAMC.
Footnotes
NATA Members: Receive 3 free CEUs each year when you subscribe to Sports Health and take and pass the related online quizzes! Not a subscriber? Not a member? The Sports Health–related CEU quizzes are also available for purchase. For more information and to take the quiz for this article, visit www.nata.org/sportshealthquizzes.
No potential conflict of interest declared.
References
- 1. Baldissera F, Cavallari P, Dworzak F. Motor neuron “bistability”: a pathogenetic mechanism for cramps and myokymia. Brain. 1994;117:929-939 [DOI] [PubMed] [Google Scholar]
- 2. Bartolozzi A, Godek S, Greene R, Burkholder R, Dorshimer G. Blood electrolytes in NFL players while experiencing EAMC compared to when they are not cramping after similar practice conditions. Med Sci Sports Exerc. 2007;39:S15 [Google Scholar]
- 3. Bentley S. Exercise-induced muscle cramp: proposed mechanisms and management. Sports Med. 1996;21:409-420 [DOI] [PubMed] [Google Scholar]
- 4. Bergeron M. Exertional heat cramps. In:Armstrong L, ed. Exertional Heat Illnesses. Champaign, IL: Human Kinetics; 2003:91-102 [Google Scholar]
- 5. Bergeron M. Exertional heat cramps: recovery and return to play. J Sport Rehabil. 2007;16:190-196 [DOI] [PubMed] [Google Scholar]
- 6. Bergeron M. Heat cramps during tennis: a case report. Int J Sport Nutr. 1996;6:62-68 [DOI] [PubMed] [Google Scholar]
- 7. Bergeron M. Heat cramps: fluid and electrolyte challenges during tennis in the heat. J Sci Med Sport. 2003;6:19-27 [DOI] [PubMed] [Google Scholar]
- 8. Bergeron M. Muscle cramps during exercise: is it fatigue or electrolyte deficit? Curr Sports Med Rep. 2008;7:S50-S55 [Google Scholar]
- 9. Binkley H, Beckett J, Casa D, Kleiner D, Plummer P. National Athletic Trainers’ Association position statement: exertional heat illnesses. J Athl Train. 2002;37:329-343 [PMC free article] [PubMed] [Google Scholar]
- 10. Brooks G, Fahey T, Baldwin K. Exercise Physiology: Human Bioenergetics and Its Applications. Boston: McGraw-Hill; 2005 [Google Scholar]
- 11. Brubaker D, Whitesel J, Barth B. Quinine sulfate: a treatment for recurrent muscle spasms. Athl Train (Greenville, NC). 1985;20:121-123 [Google Scholar]
- 12. Bye A, Kan A. Cramps following exercise. Aust Paediatr J. 1988;24:258-259 [DOI] [PubMed] [Google Scholar]
- 13. Casa D, Armstrong L, Hillman S, et al. National Athletic Trainers’ Association position statement: fluid replacement for athletes. J Athl Train. 2000;35:212-224 [PMC free article] [PubMed] [Google Scholar]
- 14. Chimera N, Swanik K, Swanik C, Straub S. Effects of plyometric training on muscle activation strategies and performance in female athletes. J Athl Train. 2004;39:24-31 [PMC free article] [PubMed] [Google Scholar]
- 15. Convertino V. Blood volume: its adaptation to endurance training. Med Sci Sports Exerc. 1991;23:1338-1348 [PubMed] [Google Scholar]
- 16. Cooper E, Ferrara M, Broglio S. Exertional heat illness and environmental conditions during a single football season in the Southeast. J Athl Train. 2006;41:332-336 [PMC free article] [PubMed] [Google Scholar]
- 17. Daniell H. Simple cure for nocturnal leg cramps. N Eng J Med. 1979;301:216. [PubMed] [Google Scholar]
- 18. Dickhuth H, Rocker K, Niess A, Horstmann T, Mayer F, Striegel H. Exercise-induced, persistent and generalized muscle cramps. J Sports Med Phys Fitness. 2002;42:92-94 [PubMed] [Google Scholar]
- 19. Diener H, Dethlefsen U, Dethlefsen-Gruber S, Verbeek P. Effectiveness of quinine in treating muscle cramps: a double-blind, placebo-controlled parallel-group, multicentre trial. Int J Clin Pract. 2002;56:243-246 [PubMed] [Google Scholar]
- 20. Eichner E. Heat cramps: salt is simplest, most effective antidote. Sports Med Dig. 1999;21:88 [Google Scholar]
- 21. Eichner E. Treatment of suspected heat illness. Int J Sports Med. 1998;19:S150-S153 [DOI] [PubMed] [Google Scholar]
- 22. Fowkes G, Bartolozzi A, Peduzzi C, Burkholder R, Dorshimer G. A comparison of blood measures while NFL players are experiencing EAMC and after IV treatment when EAMC are alleviated. J Athl Train. 2008;43:S61 [Google Scholar]
- 23. Galloway S. Dehydration, rehydration, and exercise in the heat: rehydration strategies for athletic competition. Can J Appl Physiol. 1999;24:188-200 [DOI] [PubMed] [Google Scholar]
- 24. Gersh M, ed. Electrotherapy in Rehabilitation. Philadelphia, PA: FA Davis Co; 1992 [Google Scholar]
- 25. Hakkinen K, Komi P. Fatiguability in voluntary and reflex contraction after conditioning of human skeletal muscle. Electromyogr Clin Neurophysiol. 1985;25:319-330 [PubMed] [Google Scholar]
- 26. Hayward L, Wesselmann U, Rymer W. Effects of muscle fatigue on mechanically sensitive afferents of slow conduction velocity in the cat triceps surae. J Neurophysiol. 1991;65:360-370 [DOI] [PubMed] [Google Scholar]
- 27. Helin P. Physiotherapy and electromyography in muscle cramp. Br J Sports Med. 1985;19:230-231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hutton R, Nelson D. Stretch sensitivity of golgi tendon organs in fatigued gastrocnemius muscle. Med Sci Sports Exerc. 1986;18:69-74 [PubMed] [Google Scholar]
- 29. Jones B, Rock P, Smith L, et al. Medical complaints after a marathon run in cool weather. Phys Sportsmed. 1985;13:103-110 [DOI] [PubMed] [Google Scholar]
- 30. Jung A, Bishop P, Al-Nawwas A, Dale R. Influence of hydration and electrolyte supplementation on incidence and time to onset of exercise-associated muscle cramps. J Athl Train. 2005;40:71-75 [PMC free article] [PubMed] [Google Scholar]
- 31. Kandel E, Schwartz J, Jessell T. Principles of Neural Science. 3rd ed Norwalk, CT: Appleton & Lange; 1996 [Google Scholar]
- 32. Kantarowski P, Hiller W, Garrett W. Cramping studies in 2600 endurance athletes. Med Sci Sports Exerc. 1990;22:S104 [Google Scholar]
- 33. Khan S, Burne J. Reflex inhibition of normal cramp following electrical stimulation of the muscle tendon. J Neurophysiol. 2007;98:1102-1107 [DOI] [PubMed] [Google Scholar]
- 34. Layzer RB. The origin of muscle fasciculations and cramps. Muscle Nerve. 1994;17:1243-1249 [DOI] [PubMed] [Google Scholar]
- 35. Levin S. Investigating the cause of muscle cramps. Phys Sportsmed. 1993;21:111-113 [DOI] [PubMed] [Google Scholar]
- 36. Manjra S, Schwellnus M, Noakes T. Risk factors for exercise associated muscle cramping (EAMC) in marathon runners. Med Sci Sports Exerc. 1996;28:S167 [Google Scholar]
- 37. Maquirriain J, Merello M. The athlete with muscular cramps: clinical approach. J Am Acad Orthop Surg. 2007;15:425-431 [DOI] [PubMed] [Google Scholar]
- 38. Maughan R. Exercise induced muscle cramp: a prospective biochemical study in marathon runners. J Sports Sci. 1986;4:31-34 [DOI] [PubMed] [Google Scholar]
- 39. Miller K, Knight K. Pain and soreness associated with a percutaneous electrical stimulation muscle cramping protocol. Muscle Nerve. 2007;36:711-714 [DOI] [PubMed] [Google Scholar]
- 40. Miller T, Layzer RB. Muscle cramps. Muscle Nerve. 2005;32:431-442 [DOI] [PubMed] [Google Scholar]
- 41. Moss K. Some effects of high air temperatures and muscular exertion upon colliers. Proc R Soc Lond B Biol Sci. 1923;95:181-200 [Google Scholar]
- 42. Nelson D, Hutton R. Dynamic and static stretch responses in muscle spindle receptors in fatigued muscle. Med Sci Sports Exerc. 1985;17:445-450 [DOI] [PubMed] [Google Scholar]
- 43. Norris F, Gasteiger E, Chatfield P. An electromyographic study of induced and spontaneous muscle cramps. Electroencephalogr Clin Neurophysiol. 1956;9:139-147 [DOI] [PubMed] [Google Scholar]
- 44. Obi T, Mizoguchi K, Matsuoka H, Takatsu M, Nishimura Y. Muscle cramp as the result of impaired GABA function: an electrophysiological and pharmacological observation. Muscle Nerve. 1993;16:1228-1231 [DOI] [PubMed] [Google Scholar]
- 45. Ramsey F, Schafer D. Drawing statistical conclusions. In: The Statistical Sleuth: A Course in Data Analysis Methods. 2nd ed Pacific Grove, CA: Duxbury; 2002:1-27 [Google Scholar]
- 46. Rehrer N, Smets A, Reynaert H, Goes E, De Meirleir K. Effect of exercise on portal vein blood flow in man. Med Sci Sports Exerc. 2001;31:701-715 [DOI] [PubMed] [Google Scholar]
- 47. Riley J, Antony S. Leg cramps: differential diagnosis and management. Am Fam Physician. 1995;52(6):1794-1798 [PubMed] [Google Scholar]
- 48. Ross B, Thomas C. Human motor unit activity during induced muscle cramp. Brain. 1995;118:983-993 [DOI] [PubMed] [Google Scholar]
- 49. Sawka M, Burke L, Eichner E, Maughan R, Montain S, Stachenfeld N. ACSM position stand: exercise and fluid replacement. Med Sci Sports Exerc. 2007;39:377-390 [DOI] [PubMed] [Google Scholar]
- 50. Schwellnus M. Cause of exercise associated muscle cramps (EAMC)-Altered neuromuscular control, dehydration, or electrolyte depletion? Br J Sports Med. 2009;43:401-408 [DOI] [PubMed] [Google Scholar]
- 51. Schwellnus M, Derman E, Noakes T. Aetiology of skeletal muscle “cramps” during exercise: a novel hypothesis. J Sports Sci. 1997;15:277-285 [DOI] [PubMed] [Google Scholar]
- 52. Schwellnus M, Nicol J, Laubscher R, Noakes T. Serum electrolyte concentrations and hydration status are not associated with exercise associated muscle cramping (EAMC) in distance runners. Br J Sports Med. 2004;38:488-492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Serrao M, Arendt-Nielsen L, Ge H, Pierelli F, Sandrini G, Farina D. Experimental muscle pain decreases the frequency threshold of electrically elicited muscle cramps. Exp Brain Res. 2007;182:301-308 [DOI] [PubMed] [Google Scholar]
- 54. Stofan J, Zachwieja J, Horswill C, Murray R, Anderson S, Eichner E. Sweat and sodium losses in NCAA football players: a precursor to heat cramps? Int J Sport Nutr Exerc Metab. 2005;15:641-652 [DOI] [PubMed] [Google Scholar]
- 55. Stone M, Edwards J, Babington J, Ingersoll C, Palmieri R. Reliability of an electrical method to induce muscle cramp. Muscle Nerve. 2003;27:122-123 [DOI] [PubMed] [Google Scholar]
- 56. Stone M, Edwards J, Stemmans C, Ingersoll C, Palmieri R, Krause B. Certified athletic trainers’ perceptions of exercise associated muscle cramps. J Sport Rehabil. 2003;12:333-342 [Google Scholar]
- 57. Sulzer N, Schwellnus M, Noakes T. Serum electrolytes in Ironman triathletes with exercise associated muscle cramping. Med Sci Sports Exerc. 2005;37:1081-1085 [DOI] [PubMed] [Google Scholar]
- 58. Swanik C, Lephart SM, Giannantonio F, Fu F. Reestablishing neuromuscular control in the ACL injured athlete. J Sport Rehabil. 1997;6:182-206 [Google Scholar]
- 59. Swanik K, Lephart S, Swanik C, Lephart S, Stone D, Fu F. The effects of shoulder plyometric training on proprioception and muscle performance characteristics. J Shoulder Elbow Surg. 2002;11:579-586 [DOI] [PubMed] [Google Scholar]
- 60. Talbott J. Heat cramps. Medicine. 1935;14:323-376 [Google Scholar]
- 61. Vist G, Maughan R. The effect of osmolality and carbohydrate content on the rate of gastric emptying of liquids in man. J Physiol. 1995;486:523-531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Wilk K, Voight M, Keirns M, Gambetta V, Andrews J, Dillman C. Stretch-shortening drills for the upper extremities: theory and clinical application. J Orthop Sports Phys Ther. 1993;17:225-239 [DOI] [PubMed] [Google Scholar]