Abstract
Background:
Medial epicondylitis, or golfer’s/pitcher’s elbow, develops as a result of medial stress overload on the flexor muscles at the elbow and presents as pain at the medial epicondyle. Cervical radiculopathy has been associated with lateral epicondylitis, but few associations between the cervical spine and medial epicondylitis have been made. Researchers propose that there is an association, suggesting that the weakness and imbalance in the elbow flexor and extensor muscles from C6 and C7 radiculopathy allow for easy onset of medial epicondylitis.
Hypothesis:
Medial epicondylitis will present in over half the patients diagnosed with C6 and C7 radiculopathy.
Methodology:
A total of 102 patients initially presenting with upper extremity or neck symptoms were diagnosed with cervical radiculopathy. They were then examined for medial epicondylitis. Data were collected by referring to patient charts from February 2008 until June 2009.
Results:
Fifty-five patients were diagnosed with medial epicondylitis. Of these, 44 had C6 and C7 radiculopathy whereas 11 presented with just C6 radiculopathy.
Conclusion:
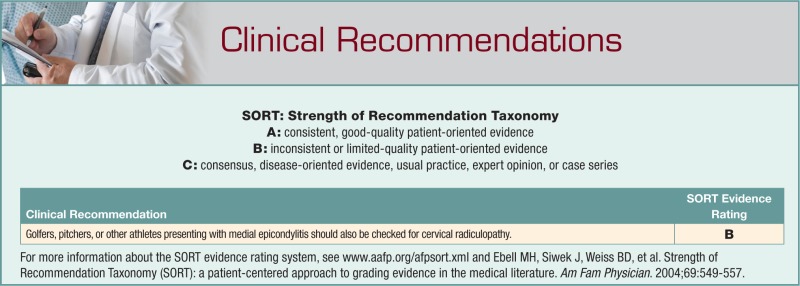
Medial epicondylitis presented with cervical radiculopathy in slightly more than half the patients. Weakening of the flexor carpi radialis and pronator teres and imbalance of the flexor and extensor muscles from the C6 and C7 radiculopathy allow for easy onset of medial epicondylitis. Patients with medial epicondylitis should be examined for C6 and C7 radiculopathy to ensure proper treatment. Physicians dealing with golfers, pitchers, or other patients with medial epicondylitis should be aware of the association between these 2 diagnoses to optimize care.
Keywords: cervical radiculopathy, epicondylitis, golfer’s elbow
Medial epicondylitis, a condition seen commonly in golfers and pitchers, develops as a result of medial stress overload on the flexor musculature at the elbow.2,14 The medial elbow muscle overload is typically obtained by repetitive golf swings or pitching—hence, the term golfer’s elbow or pitcher’s elbow. Most pathology occurs in the musculotendinous origin of the flexor carpi radialis and pronator teres.1,8 Large diffuse tears can also occur in the palmaris longus, flexor digitorum superficialis, and flexor carpi ulnaris.10,11 The injury is a result of tendinous microtearing owing to muscle-tendon overload.13 Following the overload, tendon degeneration occurs instead of repair.10,11 Medial epicondylitis presents as pain at the medial epicondyle, aggravated by activities that resist the flexor muscles of the wrist. Medial epicondylitis can cause pain and weakness throughout the upper extremity and can result in impairment or disability.9,11 Treatment of medial epicondylitis before surgery includes anti-inflammatory drugs, massages, elbow braces, and steroid injections.5
Cervical radiculopathy can radiate pain, paresthesia, numbness, or weakness into the arms.12,15 Multiple associations of lateral epicondylitis (tennis elbow) to the cervical spine have been made, but minimal association between the medial epicondylitis and the cervical spine has been proposed.9 Gunn documented 50 patients with nonresolving lateral elbow symptoms.7 Cervical spine treatment produced improvement of elbow symptoms within 5.25 weeks. Gunn concluded that the patients had cervical degeneration before the onset of their elbow symptoms and that cervical therapy alleviated the elbow symptoms.7 C6 and C7 radiculopathy affects muscles that are injured with medial epicondylitis: pronator teres, flexor carpi radialis, palmaris longus, flexor digitorum superficialis, and flexor carpi ulnaris.4
Although few cases are documented where the cervical spine is the cause of medial epicondylitis, an association between cervical radiculopathy at the C6 and C7 level and medial epicondylitis may exist. Medial epicondylitis is commonly seen in golfers and pitchers.8 A group of patients were diagnosed with cervical radiculopathy after initially presenting with upper extremity or neck symptoms. C6 and C7 radiculopathy results in weakness and dysfunction of pronator teres, flexor carpi radialis, palmaris longus, flexor digitorum superficialis, and flexor carpi ulnaris.4 These are the muscles involved with medial epicondylitis.3 The developed weakness in these flexor muscles may allow for onset of medial epicondylitis.
Methods
A total of 102 patients were studied, as evaluated and treated at the office of a physical medicine and rehabilitation specialist. Patients were originally referred with complaints of neck pain and upper extremity weakness, numbness, tingling, or pain. All patients in this study were diagnosed with cervical radiculopathy. Diagnosis of cervical radiculopathy was reached using a combination of physical examination, symptoms, and cervical magnetic resonance imaging (MRI) results.2,3 The patient group was a sample of convenience from February 2008 until June 2009.
The level of cervical radiculopathy was noted, along with whether the patient was diagnosed with medial epicondylitis. The sex, age, and involvement of medial epicondylitis were noted. Medial epicondylitis was diagnosed by palpating 1 cm distal and anterior to the medial epicondyle and noting whether the patient reported tenderness or not. What led to the diagnosis were a reported increase of medial elbow pain with wrist flexion or pronation resistance and reports of increased pain during activities that required wrist flexion.5,6
Results
Medial epicondylitis was diagnosed in 55 (54%) of the 102 patients (Tables 1 and 2). Of the 55 patients, 39 (71%) presented with bilateral medial epicondylitis, whereas 16 (29%) were one-sided. Furthermore, of the 55 patients, 11 patients (20%) had abnormal C5-6 MRI findings consistent with C6 radiculopathy. The remaining 44 (80%) had abnormal C5-6 and C6-7 cervical MRI findings and overall presentation consistent with C6 and C7 radiculopathy. No patients diagnosed with C6-7 disc displacement and C7 radiculopathy presented with medial epicondylitis.
Table 1.
Women diagnosed with medial epicondylitis, sorted by age.
| Age Range, y | |||||
|---|---|---|---|---|---|
| 20-39 | 40-59 | 60-79 | > 79 | All Women | |
| Total patients, n | 10 | 29 | 32 | 1 | 72 |
| Medial epicondylitis, n | 7 | 20 | 15 | 1 | 43 |
| Medial epicondylitis, % | 70 | 69 | 47 | 100 | 61 |
| Bilateral, n | 6 | 15 | 10 | 1 | 32 |
| One-sided, n | 1 | 5 | 5 | 0 | 11 |
Table 2.
Men diagnosed with medial epicondylitis, sorted by age.
| Age Range, y | |||||
|---|---|---|---|---|---|
| 20-39 | 40-59 | 60-79 | > 79 | All Men | |
| Total patients, n | 2 | 17 | 8 | 3 | 30 |
| Medial epicondylitis, n | 2 | 5 | 4 | 1 | 12 |
| Medial epicondylitis, % | 100 | 29 | 50 | 33 | 40 |
| Bilateral, n | 2 | 3 | 2 | 0 | 7 |
| One-sided, n | 0 | 2 | 2 | 1 | 5 |
Discussion
Fifty-four percent of patients with C6 and C7 radiculopathy were also diagnosed with medial epicondylitis, approximately 20% of whom had only C6 radiculopathy. Women had a higher incidence of medial epicondylitis than that of men, which may be due to the larger sample size of the former.
These data suggest that medial epicondylitis occurs with C6 and C7 radiculopathy. The patients did not sustain medial stress overload at the elbow by swinging a golf club or throwing a ball. This implies that an underlying condition made them more susceptible to the injury, allowing onset to occur without the repetitive medial muscle stress that is usually connected with medial epicondylitis.
Cervical radiculopathy can cause weakness as well as pain to the muscles around the medial epicondyle.3 The primary muscles involved with medial epicondylitis—pronator teres and flexor carpi radialis—are weakened by C6 and C7 radiculopathy.1,8,10,11 The weakness may result in an imbalance of the wrist and finger extensor and flexor muscles. The radiculopathy could also cause the lack of tissue repair that occurs with medial epicondylitis.10,11
From a clinical aspect, whenever a patient is diagnosed with medial epicondylitis, an underlying cervical radiculopathy should be ruled out before treatment. A history of pain, numbness, and weakness of the neck, arm, forearm, or hand is of concern. The physical examination should include a thorough neurological examination of muscle strength, sensory loss, and reflexes.6 In addition, if medial epicondylitis does not respond to the traditional treatment regimens, then consideration of cervical radiculopathy is recommended before surgical treatment.
This study has 2 limitations. Most important, the diagnosis of medial epicondylitis was made with commonly accepted physical examination findings: pain with palpation distal and anterior to the medial epicondyle, an increase in pain with resisted wrist flexion, and increased pain with repetitive wrist flexion.5,6 Imaging and electrodiagnostic studies were not used to confirm the diagnosis of medial epicondylitis. These symptoms are not exclusive to medial epicondylitis, and the association is not concrete. Other processes could have caused these findings.
Conclusion
Medial epicondylitis may frequently occur among patients with C6 and C7 radiculopathy. Patients that present with medial epicondylitis can have an overlying cervical radiculopathy that is responsible for the onset of the medial elbow symptoms.
Footnotes
No potential conflict of interest declared.
References
- 1. Bennett JG. Lateral and medial epicondylitis. Hand Clin. 1994;10:157-163 [PubMed] [Google Scholar]
- 2. Braddom RL, Buschbacher RM, Dumitru D, et al. Physical Medicine and Rehabilitation. Philadelphia, PA: WB Saunders Co; 2000:762-787, 809-810 [Google Scholar]
- 3. Cannon DE, Dillingham TR, Miao H, Andary MT, Pezzin LE. Musculoskeletal disorders in referrals for suspected cervical radiculopathy. Arch Phys Med Rehabil. 2007;88(10):1256-1259 [DOI] [PubMed] [Google Scholar]
- 4. Dumitru D, Amato AA, Zwarts MJ, et al. Electrodiagnostic Medicine. 2nd ed. Philadelphia, PA: Hanley & Belfus; 2002:721 [Google Scholar]
- 5. Dvorkin ML. Office Orthopaedics. East Norwalk, CT: Appleton & Lange; 1993:104-106 [Google Scholar]
- 6. Greene WB, Dehaven KE, Pfeffer GB, et al. Essentials of Musculoskeletal Care. 2nd ed. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2001:176-179 [Google Scholar]
- 7. Gunn CC, Milbrandt WE. Tennis elbow and the cervical spine. Can Med Assoc J. 1976;114(9):803-809 [PMC free article] [PubMed] [Google Scholar]
- 8. Leach RE, Miller JK. Lateral and medial epicondylitis of the elbow. Clin Sports Med. 1987;6:259-272 [PubMed] [Google Scholar]
- 9. O’Dwyer KJ, Howie CR. Medial epicondylitis of the elbow. Int Orthop. 1995;19:69-71 [DOI] [PubMed] [Google Scholar]
- 10. Ollivierre CO, Nirschl RP, Pettrone FA. Resection and repair for medial tennis elbow: a prospective analysis. Am J Sports Med. 1995;23:214-221 [DOI] [PubMed] [Google Scholar]
- 11. Park GY, Lee SM, Lee MY. Diagnostic value of ultrasonography for clinical medial epicondylitis. Arch Phys Med Rehabil. 2008;89(4):738-742 [DOI] [PubMed] [Google Scholar]
- 12. Posner JB. Neurologic Complications of Cancer. Philadelphia, PA: FA Davis; 1995 [Google Scholar]
- 13. Rineer CA, Ruch DS. Elbow tendinopathy and tendon ruptures: epicondylitis, bicep, and triceps ruptures. J Hand Surg [Am]. 2009;34(3):566-576 [DOI] [PubMed] [Google Scholar]
- 14. Shiri R, Viikari-Juntura E, Varonen H, Heliovaara M. Prevalence and determinants of lateral and medial epicondylitis: a population study. Am J Epidemiol. 2006;164:1065-1074 [DOI] [PubMed] [Google Scholar]
- 15. Stubblefield MD, Custodio CM. Upper-extremity pain disorders in breast cancer. Arch Phys Med Rehabil. 2006;87:1. [DOI] [PubMed] [Google Scholar]