Abstract
Context:
Femoroacetabular impingement (FAI) is a common cause of intra-articular hip pathology and secondary osteoarthritis. It affects athletes at a young age as they push their bodies beyond the diminished physiologic limits imposed by the altered joint morphology. Understanding the cause of this condition and its assessment in athletes is important.
Evidence Acquisition:
The scientific literature was reviewed to reflect the current understanding of hip joint pathology among athletic individuals. Focus is given to the literature since 2003, when FAI was first reported as a cause of joint damage in the native hip.
Results:
There are 3 types of FAI: pincer, cam, and combined. The pathomechanics and pattern of secondary intra-articular pathology are different among the types. History and examination usually reflect findings of joint damage among athletes, and radiographs can reveal the presence of underlying FAI. Other imaging studies may variably aid in detecting the pathology.
Conclusions:
FAI is a common cause of hip problems in athletes. Early recognition is an important first step in order to avoid the severe secondary damage that can occur.
Keywords: femoroacetabular impingement, athletes, hip arthroscopy, cause, assessment
The implications of abnormal hip morphology leading to secondary joint damage have been described for almost 100 years.17-19 However, the concept of femoroacetabular impingement (FAI) as a cause of osteoarthritis is credited to Professor Reinhold Ganz and his colleagues from Bern, Switzerland.10 Early-age onset osteoarthritis among adults in their fourth and fifth decades is often attributed to this process. It is now recognized that FAI can cause serious joint damage among young athletes, even in their second and third decades.4 As athletes push their bodies beyond physiologic limits, breakdown occurs. Among athletes with impingement, the threshold for breakdown is much lower, occurring with loads and activities tolerated by their counterparts with normal joint morphology. Thus, severe joint damage is often encountered in athletes who, if otherwise were less active, would only start to present with findings of osteoarthritis at a later age. FAI refers to the process by which a malformed hip joint secondarily leads to breakdown of the intra-articular structures, causing pain and associated dysfunction, followed by premature osteoarthritis. There is a pincer type, a cam type, and combined impingement.10
Pincer impingement is caused by an excessive prominence of the anterolateral rim of the acetabulum.10 This can occur simply from overgrowth of the anterior edge or retroversion of the acetabulum, which is a condition where the face of the acetabulum tilts slightly backward instead of its normal, forward position. Sometimes there is a separate piece of bone along the anterolateral rim, an os acetabulum.12 With hip flexion, the prominent rim of the acetabulum crushes the labrum against the femoral neck (Figure 1). This cyclical submaximal repetitive microtrauma leads to breakdown and failure of the acetabular labrum. Secondarily, over time, a variable amount of articular failure within the adjacent acetabulum will occur. Pincer impingement occurs about equally in men and women and often starts to cause symptoms in middle age.5
Figure 1.
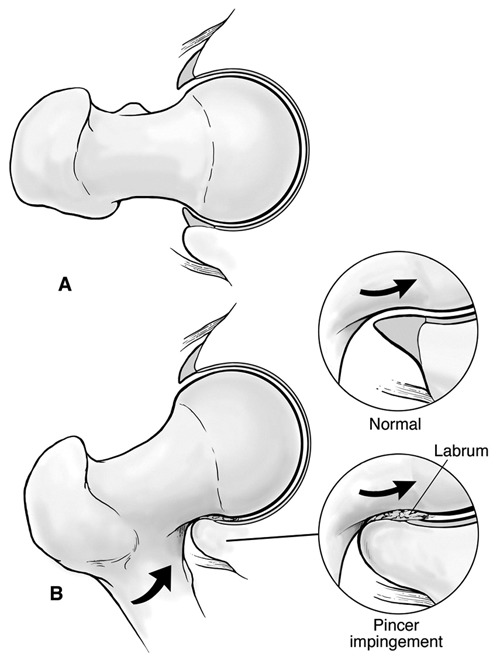
Pincer impingement occurs from a bony prominence of the anterior acetabulum crushing the labrum against the neck of the femur (A → B). Secondary articular failure occurs over time.
Cam impingement refers to a cam effect caused by a nonspherical femoral head rotating inside the acetabulum.10 This has long been recognized as a sequela of a slipped capital femoral epiphysis where posterior displacement of the capitis leaves a prominence of the anterior neck, resulting in severely limited internal rotation of the hip.9 Operations performed to excise this bony prominence have been referred to as a cheilectomy.9 However, more subtle forms of an aspherical femoral head are much more common and only more recently recognized as a cause of problems. This has been described as a “pistol grip” deformity, seen in association with early-onset osteoarthritis in adults.18 This may be due to premature eccentric closure of the capital physis in adolescence, resulting in the nonspherical shape of the femoral head. Intense physical activity at a young age may somehow precipitate this partial physeal arrest and cause the cam lesion. This concept has not yet been substantiated. Although cam impingement is clearly a causative factor in joint damage among athletic individuals, it is not clear whether athletic activity causes the impingement. With flexion, the nonspherical portion of the head rotates into the acetabulum, creating a shear force on the anterolateral edge of the acetabular articular surface (Figure 2). With repetitive motion, this eventually results in articular delamination and failure of the acetabular articular cartilage. In this condition, there is preferential articular pathology and relative labral preservation. Over time, the labrum will eventually start to fail but only after the process is advanced on the articular surface. Cam impingement has an approximately 3:1 predilection for men and often presents with problems in young adulthood.4
Figure 2.
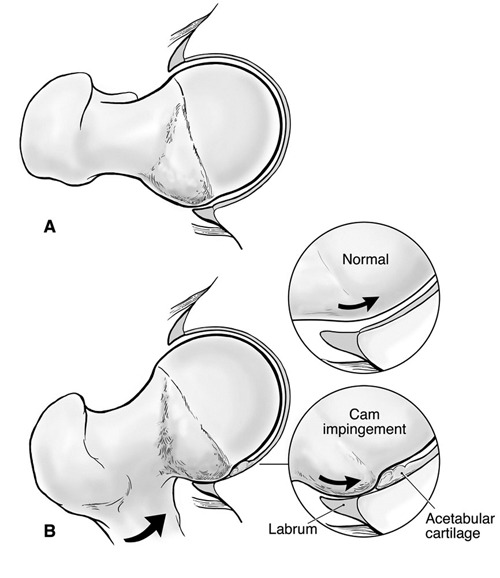
Cam impingement occurs with hip flexion as the bony prominence of the nonspherical portion of the femoral head (cam lesion) glides under the labrum, engaging the edge of the articular cartilage and resulting in progressive delamination (A → B). Initially, the labrum is relatively preserved, but secondary failure occurs over time.
Combinations of pincer and cam impingement can occur. The demographics are intermediate between pincer and cam forms. One pattern or the other may predominate, or athletes may have an equal contribution from both. This may have some influence on the optimal method of treatment.
Impingement (or FAI) has gained much attention in the past few years. In the past, this pathological process simply went undiagnosed. Athletes often experienced poorly explained groin pain that eventually ended their competitive careers with an ill-defined, unsolved problem. With growing recognition and treatment, many athletes have been able to resume competitive activities and thus created more awareness of the disorder. It is important not to neglect findings of impingement, but it is also important not to overtreat abnormal radiographic findings. There is much to be learned about why some athletes with impingement-shaped hips may continue to function at high levels for years without developing secondary joint damage.
Assessment
Overview
Assessment of the hip joint is fairly succinct, but assessment of the hip region can be quite complex. The clinician must assess for coexistent disease, compensatory disorders, and coincidental findings.
Coexistent disorders
Hip joint disease and lumbar spine disease often coexist. This is common in sports where rotational velocity is a premium, such as baseball and golf. As failure of one region occurs, the athlete loses the ability to compensate for the other. Thus, symptoms and the focus of treatment may be constantly changing.
Athletic pubalgia (or sports hernia) is a condition that can be confused with a hip joint problem, given that the symptoms emanate from the groin area.14 Hip disorders often coexist with athletic pubalgia.15 Increased pelvic motion compensates for reduced rotation of the hip, which puts greater stress on the pelvic stabilizers and can thus result in breakdown of these soft tissue structures, ie, athletic pubalgia. Evaluation can challenge the diagnostic acumen of the clinician, but with care, the 2 conditions can usually be distinguished. Athletic pubalgia is characterized by localized tenderness to palpation around the pubic ramus, including the insertion of the rectus abdominis and the origin of the hip adductors. Resisted sit-ups or hip adduction may exacerbate symptoms. Hip joint pathology does not usually have accompanying tenderness to palpation. Athletic pubalgia should not be aggravated by passive hip flexion with extremes of rotation, which typically exacerbates a hip joint problem.
Compensatory disorders
Hip joint disorders often go undetected for a protracted period. In one study of athletes, 60% were treated for an average of 7 months before it was recognized that the joint may be the source of symptoms.7 As athletes attempt to compensate for the damaged joint, they may develop symptoms associated with secondary disorders created by compensating for the hip. For example, chronic gluteal discomfort may be present, or lateral pain from trochanteric bursitis and abductor irritability. On examination, these secondary findings may be more evident, obscuring the underlying element of primary hip dysfunction.
Coincidental findings
As an incidental asymptomatic finding, snapping of the iliopsoas tendon is present in 10% of an active population.1 Thus, snapping of the tendon might coincidentally be present in athletes with a hip joint problem. The clinician must distinguish whether symptoms are emanating from the joint or are due to the snapping iliopsoas tendon. Simple questioning will usually distinguish whether the snapping is painful to the athlete or just a coincidental observation. On examination, snapping of the iliopsoas is characteristically reproduced while bringing the hip from a flexed abducted externally rotated position into extension with internal rotation, with the tendon snapping across the front of the hip and the pectineal eminence (Figure 3). It is often a dynamic process that the athlete can demonstrate better than what the examiner can detect. Maneuvers performed by the athlete to elicit snapping are variable in the sitting, standing, or supine position, but the consistent feature is that snapping occurs while going from flexion to extension. Iliopsoas bursography and ultrasonography have been described for investigating the painful snapping iliopsoas tendon.1 These studies are approximately 80% reliable, with 20% false-negative findings. Thus, the clinician’s interview of the athlete and examination are the most reliable features of the evaluation.
Figure 3.
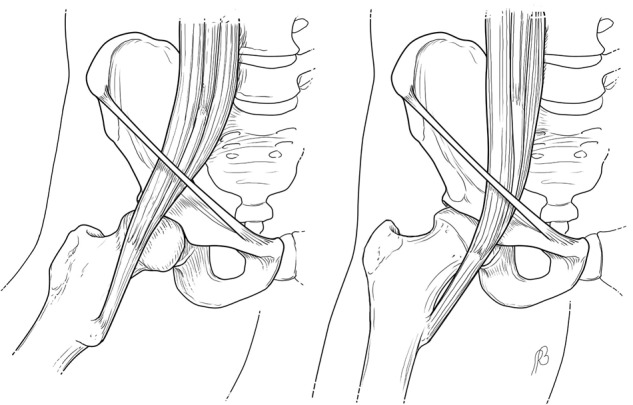
The iliopsoas tendon flipping back and forth across the anterior hip and pectineal eminence: A, with flexion of the hip, the iliopsoas tendon lies lateral to the center of the femoral head; B, with extension of the hip, the iliopsoas shifts medial to the center of the femoral head.
Snapping of the iliotibial band occurs as the tensor fascia lata flips back and forth across the greater trochanter with rotational motion of the hip (Figure 4).3 The athlete can usually demonstrate this to the examiner better than what the examiner can detect on passive examination. The visual appearance may give the impression that the hip is subluxing, but it is simply the tensor fascia lata moving across the greater trochanter. Snapping of the iliotibial band is not commonly confused with a hip joint disorder, but it can mimic instability.
Figure 4.
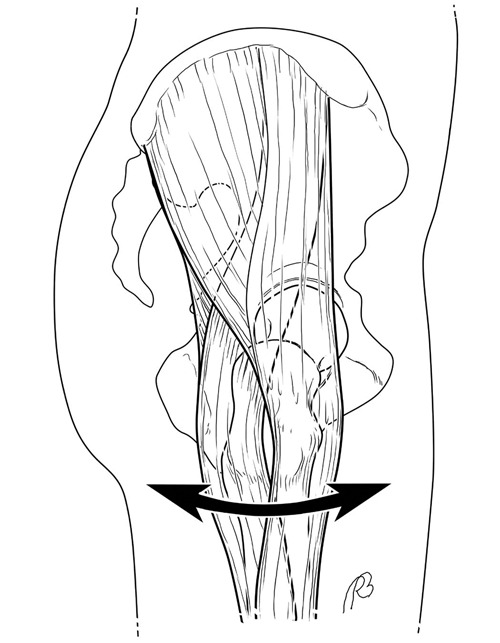
As the iliotibial band snaps back and forth across the greater trochanter, the tendinous portion may flip across the trochanter with flexion and extension, or the trochanter may move back and forth underneath the stationary tendon with internal and external rotation.
In general, snapping of the iliopsoas tendon produces an audible clunk that can usually be heard from across the room, and snapping of the iliotibial band can easily be seen with the visual prominence of the abductor mechanism flipping back and forth.
History
The onset of symptoms associated with FAI in athletes is variable, but the damage results from the cumulative effect of cyclical abnormal wear associated with the altered joint morphology.4 The onset may be gradual, or athletes may recount an acute precipitating episode. However, on close questioning, the athlete will frequently recall prior nonspecific symptoms of a groin strain. Also, many athletes who develop pathological impingement will recount that they were never as flexible as their teammates. Although they may demonstrate poor flexibility, this is rarely a functional problem. Increased pelvic and lumbosacral motion compensate for diminished range of hip motion. These compensatory pathomechanics create other problems that commonly coexist with FAI.14
Hip joint symptoms typically emanate from the anterior groin and may radiate to the medial thigh (Figure 5).2 Athletes often demonstrate the C sign in describing deep interior hip pain (Figure 6): The hand is cupped above the greater trochanter with the fingers gripping into the anterior groin. Mechanical symptoms associated with intra-articular pathology are typically characterized by intermittent sharp stabbing pain or catching often precipitated by turning, twisting, pivoting, or lateral movement. Maximal flexion is uncomfortable, and extension of the flexed hip against resistance may elicit pain (eg, rising from a squatted or seated position). With chronic degeneration, the symptoms may become constant.
Figure 5.
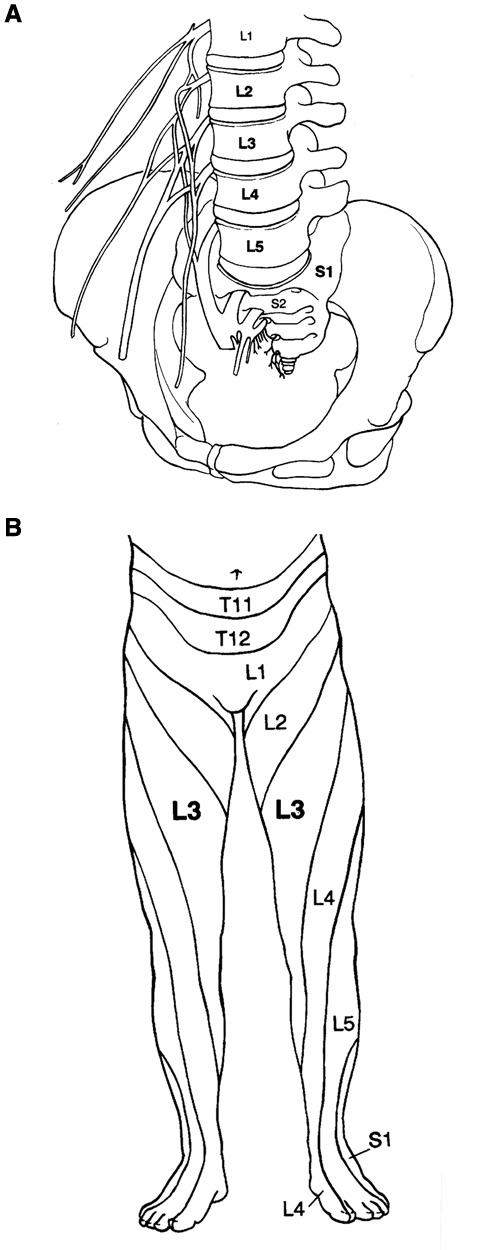
A, the hip joint receives innervation from branches of L2 to S1 of the lumbosacral plexus but predominantly from the L3 nerve root. B, the L3 dermatome crosses the anterior thigh and extends distally along the medial thigh to the level of the knee.
Figure 6.

The C sign: A, the shape of the hand when a patient describes deep interior hip pain; B, the hand is cupped above the greater trochanter, with the thumb posterior and the fingers gripping deep into the anterior groin.
Physical Examination
Physical examination will usually elicit evidence of hip joint irritability.2 However, keep in mind that examiners will not create the level of force across the joint that an athlete can generate with physical activities that precipitate symptoms.
The trademark feature of FAI is that of diminished internal rotation caused by the altered bony architecture of the joint,10 although there is much variation in the normative data on hip range of motion. Also, although only one hip may be symptomatic, the altered morphology is usually present in both hips, and there may not be much asymmetry in motion when the symptomatic side is compared with asymptomatic side. Many athletes may demonstrate reduced internal rotation and not suffer from pathological impingement. Also, though uncommon, pathological impingement is occasionally observed in athletes with normal or even increased internal rotation.
The log roll test, although not sensitive, is the most specific test for hip joint pathology independent of its cause (Figure 7).2 Internal and external rotation of the femoral head to the acetabulum should not stress any of the surrounding structures. Forced flexion, adduction, and internal rotation constitute the impingement test and elicit symptoms associated with impingement (Figure 8).10 However, virtually any irritable hip, regardless of the cause, will be uncomfortable with this maneuver. Thus, although the test is quite sensitive, it is not necessarily specific for impingement. The maneuver may be uncomfortable on the asymptomatic side, so comparison is helpful. Most important is whether it re-creates the characteristic pain that the athlete experiences with activities.
Figure 7.

Log roll test—the most specific test for hip pathology. With the patient supine, gently roll the thigh internally (A) and externally (B) to move the articular surface of the femoral head in relation to the acetabulum without stressing any of the surrounding extra-articular structures.
Figure 8.

The impingement test is performed by provoking pain with flexion, adduction, and internal rotation of the symptomatic hip.
These conditions often have a chronic component, even at the initial evaluation. Thus, secondary findings may be present because of compensatory mechanisms: Lateral pain may be present from trochanteric bursitis, and posterior tenderness within the gluteal muscles may be present protecting the hip joint. These secondary features may be more apparent on examination and can obscure the underlying primary joint pathology.
The anterior groin, lower abdominal, and adductor area must be carefully palpated to localize tenderness suggestive of athletic pubalgia (Figure 9),14 which can mimic FAI. Tenderness with resisted sit-ups, hip flexion, or adduction should raise an index of suspicion for athletic pubalgia. Pain with passive flexion and internal rotation is more indicative of an intra-articular source.
Figure 9.

Carefully palpating the anterior hip, groin, lower abdominal, and adductor region aids in assessing for the presence of soft tissue pelvic pathology.
Snapping of the iliopsoas tendon is assessed by bringing the hip from a flexed, abducted, externally rotated position into extension with internal rotation (Figure 10). Alternatively, the athlete may better demonstrate the audible clunk when taking the hip from a flexed to extended position. The snapping can be a source of symptoms and thus warrant treatment, or it may just be an incidental finding. Because it is usually noticeable to the athlete, it is important that the clinician assess its contribution to the individual’s symptoms when determining the appropriate treatment algorithm.
Figure 10.

Examination maneuver for snapping of the iliopsoas tendon: A, the hip is initially placed in abduction, flexion, and external rotation; B, the hip is then brought into extension with internal rotation, producing the snap of the iliopsoas tendon.
Imaging
Radiographs
If an athlete has persistent symptoms, radiographs should be obtained. This should include a well-centered anteroposterior pelvis and a lateral view of the affected hip (Figure 11).16 These are important for assessing impingement, joint space preservation, and other bony changes, including an os acetabulum. Overcoverage of the anterior acetabulum, characteristic of pincer impingement, is suggested by a crossover sign (Figure 12), which can be due to acetabular retroversion indicated by the posterior wall sign (Figure 13). An os acetabulum can also be evaluated (Figure 14). The cause of an os acetabulum is variable, ranging from an unfused apophysis to a traction phenomenon (from pull of the rectus femoris origin) to a rim fracture secondary to cam impingement.
Figure 11.

A properly centered anteroposterior radiograph must be controlled for rotation and tilt. Proper rotation is confirmed by alignment of the coccyx over the symphysis pubis (vertical line). Proper tilt is controlled by maintaining the distance between the tip of the coccyx and the superior border of the symphysis pubis (1- to 2-cm).
Figure 12.
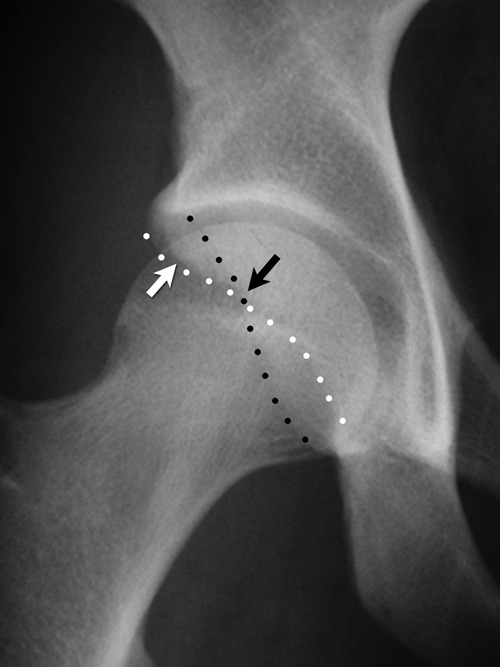
Anteroposterior view of the right hip. The anterior and posterior rims of the acetabulum are marked (white dots and black dots, respectively). The superior portion of the anterior rim lies lateral to the posterior rim (white arrow) indicating overcoverage of the acetabulum. Anteriorly, it assumes a more normal medial position, creating the crossover sign (black arrow) as a positive indicator of pincer impingement.
Figure 13.
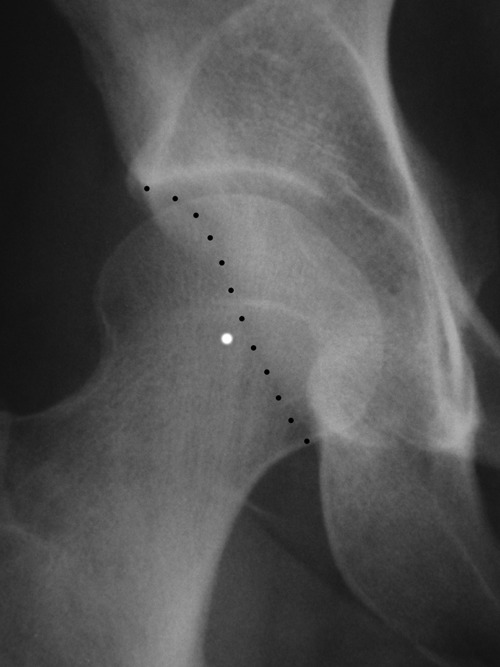
Anteroposterior view of the right hip. Acetabular retroversion as a cause of pincer impingement is indicated by a shallow posterior wall in which the posterior rim of the acetabulum (black dots) lies medial to the center of rotation of the femoral head (white dot).
Figure 14.
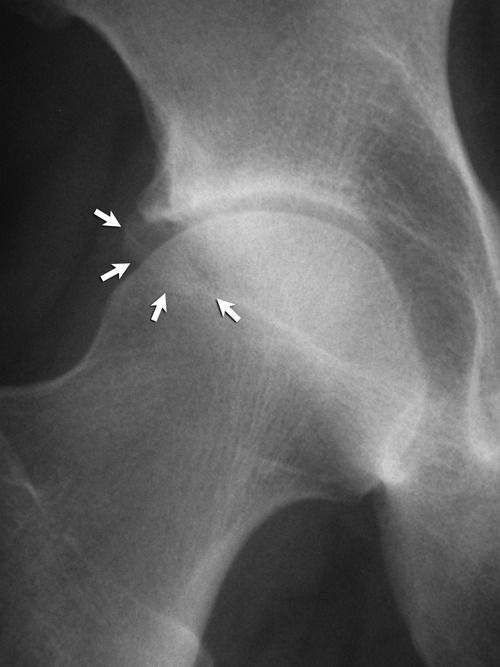
Anteroposterior radiograph of a right hip. An os acetabulum (arrows) is present, and although the cause is variable, it is often associated with femoroacetabular impingement.
The sphericity of the femoral head should be assessed on both the anteroposterior view and the lateral view (Figure 15). There is some controversy regarding the optimal lateral radiograph. The 40° Dunn view may best demonstrate the cam lesion.13 The variable shape and location of the lesion makes various views helpful. A frog lateral view is reproducible and has demonstrated efficacy in assessing the cam lesion.8 A herniation pit may be present at the anterolateral femoral head–neck junction, which can obscure the extent of a cam lesion (Figure 16). This has been reported in 30% of pathological cases of FAI but can be present in asymptomatic individuals.11 Repetitive compression of the cam lesion against the surface of the acetabulum can result in cystic erosion into the subcortical femoral surface.11 This cystic structure can become large and difficult to distinguish from a benign neoplasm (Figure 17).
Figure 15.
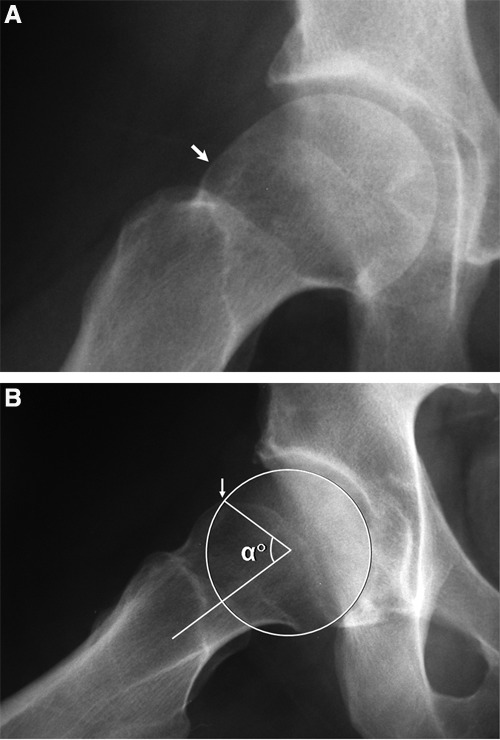
A frog lateral view of the right hip: A, the cam lesion (arrow) is evident as the convex abnormality at the head–neck junction, where there should normally be a concave slope of the femoral neck; B, the alpha angle is used to quantitate the severity of the cam lesion. A circle is placed over the femoral head. The alpha angle is formed by a line along the axis of the femoral neck and a line from the center of the femoral head to the point where the head diverges outside of the circle (arrow).
Figure 16.
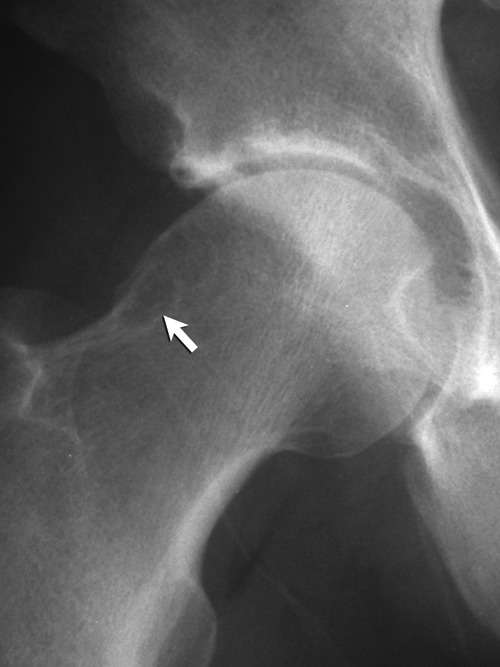
Anteroposterior radiograph of a right hip. A herniation pit is present (arrow), often associated with cam impingement.
Figure 17.
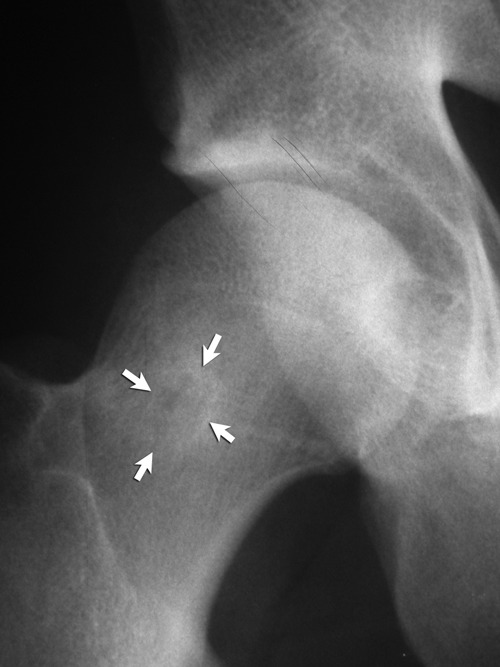
Anteroposterior radiograph of a right hip. A large cystic lesion is present (arrows), which can be confused with a neoplasm but simply represents a large herniation pit.
There are several caveats regarding radiographic interpretation of FAI. Indices of pincer impingement are assessed on a supine pelvis radiograph; the relationship of this view to the standing orientation of the pelvis is not clear. Dynamic positioning of the pelvis can be influenced by lumbar lordosis or kyphosis. The shape of cam lesions is variable, and its epicenter may be anterior or lateral. As such, radiographs represent only a 2-dimensional image of the lesion’s 3-dimensional anatomy.
Magnetic resonance imaging
Low-resolution images provided by open scanners and small magnets are ineffective at demonstrating most hip joint pathology.6 High-resolution small-field images necessitate a 1.5-T magnet with surface coils.6 The thick, noncompliant capsule does not allow for significant effusion accumulation in the joint; any effusion in a symptomatic hip is significant indirect evidence of joint pathology. The sensitivity of conventional magnetic resonance imaging (MRI) to detect labral pathology is much improved, but the ability to detect articular damage, which is usually present in association with FAI, is variable and often poor.6 If labral pathology is evident, there is likely associated articular damage. Increased signal on T2-weighted images in the anterior acetabulum may be indicative of subchondral edema, which may be incorrectly interpreted as a stress fracture of the anterior inferior iliac spine. It is more likely indicative of a subchondral stress reaction in the anterior acetabulum due to failure of the subjacent articular surface. Thus, anterior acetabular subchondral edema is suggestive of significant articular pathology (Figure 18). Increased activity within the herniation pit may be associated with active degenerative disease secondary to cam impingement. The differential diagnosis may include osteoid osteoma and other benign tumors. Other reliable indirect indicators of joint pathology include a paralabral cyst, which is pathognomonic for labral pathology. Subchondral cysts usually indicate articular pathology (Figure 19).
Figure 18.
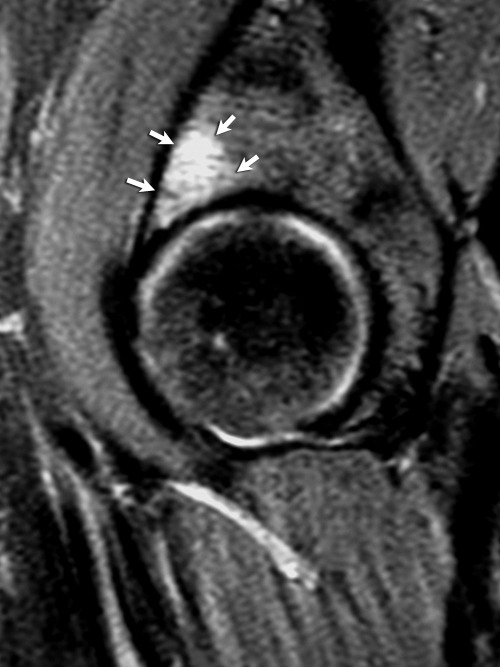
A sagittal T2-weighted MRI of a right hip. Subchondral edema of the acetabulum (arrows) is present as an indicator of subjacent articular failure seen in association with cam impingement.
Figure 19.
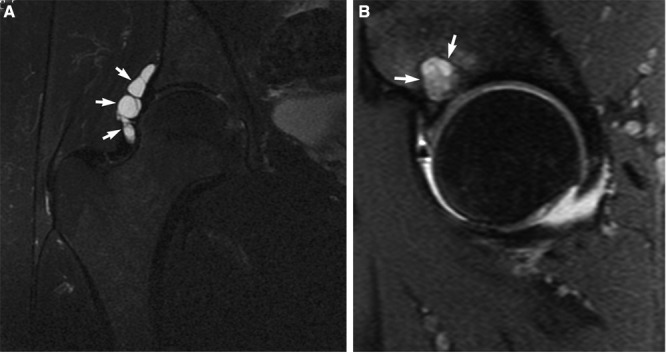
A, a coronal T2 MRI of a right hip illustrates a paralabral cyst (arrows) pathognomonic of associated labral pathology; B, a sagittal T2-weighted MRI of a right hip demonstrates a subchondral cyst (arrows) indicative of associated articular damage.
Gadolinium arthrography with MRI
MRI enhanced with intra-articular contrast (magnetic resonance arthrography; MRA) demonstrates greater sensitivity in detecting intra-articular pathology,6 including labral lesions. A normal separation between the labrum and the rim of the acetabulum may be evident when contrast separates these structures. This labral cleft should not be interpreted as a tear; it has smooth margins and lacks interdigitation of labral tissue (Figure 20). Posterior labral tears are uncommon, and separation of the posterior labrum can be assumed to be a normal cleft in most cases. A most useful aspect of MRA is the concomitant injection of long-acting anesthetic with the contrast. Whether the athlete experiences a temporary period of pain relief is usually more relevant information than the interpretation of the images. For example, the study may not fully define joint damage responsible for the athlete’s symptoms, but it can be indirectly substantiated by the response to the injection. Conversely, imaging abnormalities may be present but not responsible for the athlete’s symptoms. If the injection does not provide some pain relief, the clinician must look closely for other causes. The validity of this response depends on 2 factors: First, the athlete must be able to perform activities that can predictably generate pain before the injection; second, the athlete must perform these activities postinjection for accurate assessment of the response, which usually means returning the athlete to pain-provoking activities.
Figure 20.
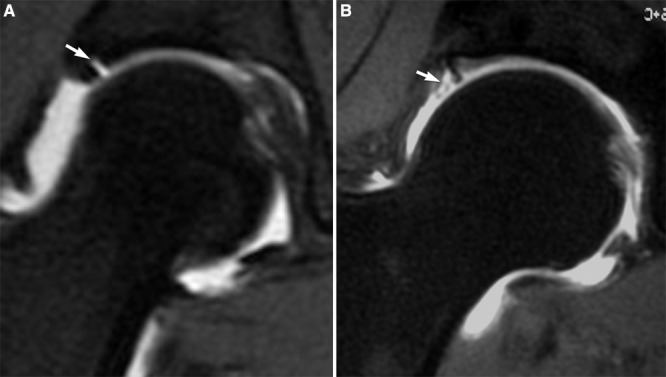
A, coronal MRA image of a right hip demonstrates contrast separating the lateral acetabulum from the labrum (arrow). Although a labral detachment cannot be ruled out, the smooth margins suggest a normal labral cleft. B, a coronal MRA image of a right hip demonstrates contrast interdigitating within the substance of the lateral labrum (arrow) indicative of true labral pathology.
There are disadvantages of MRA over conventional MRI: The contrast eliminates the opportunity to assess for an effusion. Also, contrast may obscure subchondral signal changes present within the bone (Figure 21). An optimal protocol includes a select series of both precontrast and postcontrast images.
Figure 21.
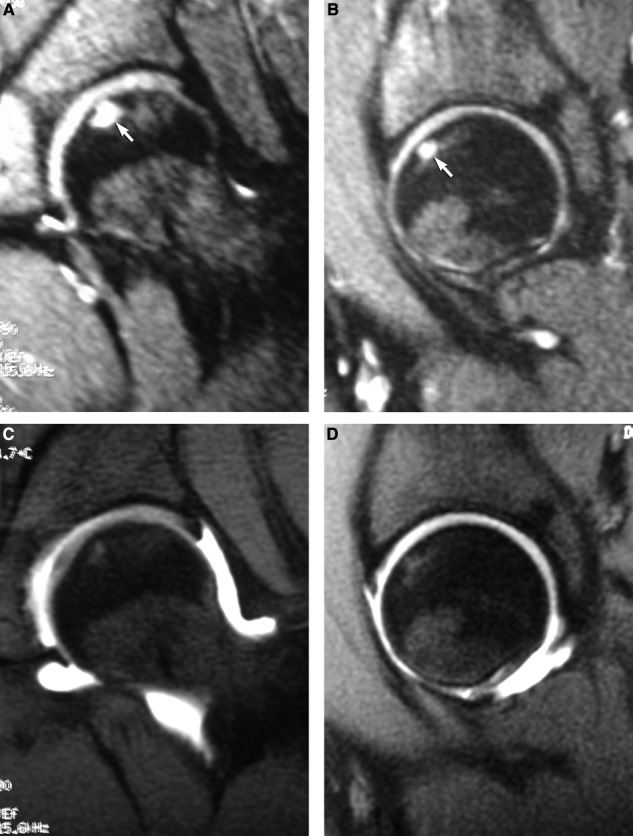
T2-weighted MRI in the coronal (A) and sagittal (B) planes demonstrates significant subchondral edema (arrows). On postcontrast MRA images in the coronal (C) and sagittal (D) planes, the subchondral changes are only subtly evident.
Computed tomography
Computed tomography (CT) is much better at showing bone architecture and structure. MRI and MRA cannot often distinguish an os acetabulum nor determine the degree of joint space narrowing. CT may complement other studies. However, planar 2-dimensional images, regardless of imaging techniques, may poorly quantitate cam lesions. Unless the image bisects the apex of the cam lesion, it often underestimates its magnitude. CT with 3-dimensional reconstructions provides the clearest image of the cam lesion and its morphology (Figure 22) and is especially helpful in the arthroscopic management. CT scans can detect the exact shape of the abnormal bone that must be exposed and resected. These images are not necessary with traditional open surgical techniques, because of the exposure provided by the extensile approach.
Figure 22.
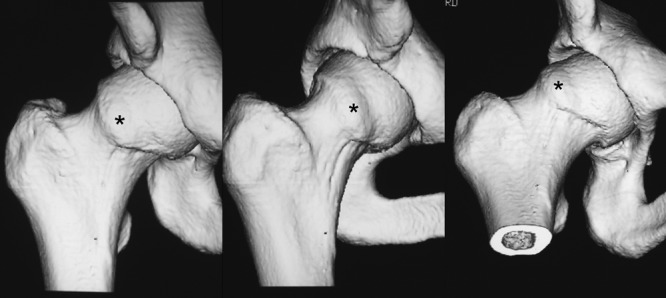
Computed tomography 3-dimensional reconstructed images of a right hip illustrate a characteristic cam lesion (asterisks).
Conclusions
Substantial strides have been made in understanding the role of hip joint pathology as a source of dysfunction and disability among athletes. With careful evaluation, the clinician can accurately assess hip disorders, including joint damage and other associated conditions that can mimic or coexist with joint pathology. Historically, most of these problems went unrecognized and untreated, often ending competitive careers. FAI is one common cause of hip joint damage among athletes. The key to recognizing FAI lies in maintaining a sense of awareness. It is unknown what portion of athletes with asymptomatic impingement morphology will develop secondary pathology. However, early recognition among athletes with symptomatic impingement is an important first step in avoiding the severe secondary damage that can occur.
Footnotes
One or more authors declared a potential conflict of interest: The authors are consultants and received research support from Smith & Nephew and own stock in A2 Surgical.
References
- 1. Byrd JWT. Evaluation and management of the snapping iliopsoas tendon. Instr Course Lect. 2006;55:347-355 [PubMed] [Google Scholar]
- 2. Byrd JWT. Physical examination. In: Byrd JWT, ed. Operative Hip Arthroscopy. 2nd ed. New York, NY: Springer; 2005:36-50 [Google Scholar]
- 3. Byrd JWT. Snapping hip. Oper Tech Sports Med. 2005;13(1):46-54 [Google Scholar]
- 4. Byrd JWT, Jones KS. Arthroscopic “femoroplasty” in the management of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2009;467:739-746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Byrd JWT, Jones KS. Arthroscopic management of femoroacetabular impingement. Instr Course Lect. 2009;58:231-239 [PubMed] [Google Scholar]
- 6. Byrd JWT, Jones KS. Diagnostic accuracy of clinical assessment, MRI, gadolinium MRI, and intraarticular injection in hip arthroscopy patients. Am J Sports Med. 2004;32(7):1668-1674 [DOI] [PubMed] [Google Scholar]
- 7. Byrd JWT, Jones KS. Hip arthroscopy in athletes. Clin Sports Med. 2001;20(4):749-762 [PubMed] [Google Scholar]
- 8. Clohisy JC, Nunley RM, Otto RJ, Schoenecker PL. The frog-leg lateral radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop Rel Res. 2007;462:115-121 [DOI] [PubMed] [Google Scholar]
- 9. Erard MC, Drvaric DM. Cheilectomy of the hip in children. J Surg Orthop Adv. 2004;13(1):20-23 [PubMed] [Google Scholar]
- 10. Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003:417;112-120 [DOI] [PubMed] [Google Scholar]
- 11. Leunig M, Beck M, Kalhor M, Kim Y, Werlen S, Ganz R. Fibrocystic changes at anterosuperior femoral neck: prevalence in hips with femoroacetabular impingement. Radiology. 2005;236:237-246 [DOI] [PubMed] [Google Scholar]
- 12. Martinez AE, Li SM, Ganz R, Beck M. Os acetabuli in femoro-acetabular impingement: stress fracture or unfused secondary ossification centre of the acetabular rim? Hip Int. 2006;16(4):281-286 [DOI] [PubMed] [Google Scholar]
- 13. Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res. 2006;445:181-185 [DOI] [PubMed] [Google Scholar]
- 14. Meyers WC, Foley DP, Garrett WE, Lohnes JH, Mandlebaum BR. Management of severe lower abdominal or inguinal pain in high-performance athletes: PAIN (Performing Athletes with Abdominal or Inguinal Neuromuscular Pain Study Group). Am J Sports Med. 2000;28(1):2-8 [DOI] [PubMed] [Google Scholar]
- 15. Meyers WC, McKechnie A, Philippon MJ, Horner MA, Zoga AC, Devon ON. Experience with “sports hernia” spanning two decades. Ann Surg. 2008;4:656-665 [DOI] [PubMed] [Google Scholar]
- 16. Parvizi J, Leunig M, Ganz R. Femoroacetabular impingement. J Am Acad Orthop Surg. 2007;15(9):561-570 [DOI] [PubMed] [Google Scholar]
- 17. Smith-Petersen MN. Treatment of malum coxae senilis, old slipped upper femoral epiphysis, intrapelvic protrusion of the acetabulum, and coxa plana by means of acetabuloplasty. J Bone Joint Surg Am. 1936;18:869-880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Stulberg SD, Cordell LD, Harris WH, Ramsey PL, MacEwen GD. Unrecognized childhood hip disease: a major cause of idiopathic osteoarthritis of the hip. In: The Hip: Proceedings of the Third Open Scientific Meeting of the Hip Society. St. Louis, MO: Mosby; 1975:212-228 [Google Scholar]
- 19. Vulpius O, Stöffel A. Orthopäadische Operationslehre. Stuttgart, Germany: Enke; 1913 [Google Scholar]


