Abstract
A normally functioning hip joint is imperative for athletes who use their lower extremities with running, jumping, or kicking activities. Sports-related injuries of the hip and groin are far less frequent than injuries to the more distal aspect of the extremity, accounting for less than 10% of lower extremity injuries. Despite the lower incidence, hip and groin injuries can lead to significant clinical and diagnostic challenges related to the complex anatomy and biomechanical considerations of this region. Loads up to 8 times normal body weight have been documented in the joint in common daily activities, such as jogging, with significantly greater force expected during competitive athletics. Additionally, treatment for hip and groin injuries can obviate the participation of medical and surgical specialties, with a multidisciplinary approach frequently required. Delay in diagnosis and triage of these injuries may cause loss of time from competition and, potentially, early onset of degenerative changes. Magnetic resonance imaging (MRI) of the hip has proven to be the gold standard for the diagnosis of sports-related hip and groin injuries in the setting of negative radiographs. With its exquisite soft tissue contrast, multiplanar capabilities, and lack of ionizing radiation, MRI is unmatched in the noninvasive diagnosis of intra-articular and extra-articular pathology, as well as intraosseous processes. This review focuses on MRI of common athletic injuries of the hip and groin, including acetabular labral tears, femoral acetabular impingement syndrome, muscle injuries around the hip and groin (including athletic pubalgia), and athletic osseous injuries.
Keywords: labrum, athletic pubalgia, femoroacetabular impingement, magnetic resonance imaging
Sports-related injuries of the hip and groin are far less frequent than injuries to the more distal aspect of the extremity, accounting for less than 10% of lower extremity injuries.15 Despite the lower incidence, hip and groin injuries can lead to significant clinical and diagnostic challenges related to the complex anatomy and biomechanical considerations of this region. Loads up to 8 times body weight across the joint are common in daily activities, such as jogging, with significantly greater force expected during competitive athletics.13 Treatment for hip and groin injuries may require the participation of medical and surgical specialties; a multidisciplinary approach is frequently required. Delay in diagnosis and triage may cause not only loss of time from competition but potentially early onset of degenerative changes.45
Magnetic resonance imaging (MRI) of the hip is the gold standard for the diagnosis of sports-related hip and groin injuries in the setting of negative radiographs. With its exquisite soft tissue contrast, multiplanar capabilities, and lack of ionizing radiation, MRI is unmatched in the noninvasive diagnosis of intra-articular and extra-articular pathology as well as intraosseous processes.
Labral Pathology
Over the past two decades, labral pathology has been found to play a significant role in patients with hip pain. Recent advances in imaging techniques, including technical advances in MRI and magnetic resonance (MR) arthrography, have increased our understanding of the pivotal role of the acetabular labrum as the cause of hip pain in many patients. Many recent studies have been performed to evaluate the role of MR arthrography in diagnosing labral pathology.69
The labrum is a fibrocartilaginous structure that lines the peripheral aspect of the acetabular rim and serves to deepen the socket joint while acting as a seal to prevent fluid expression from the joint. This seal serves to maintain the hydraulic load-bearing capacity of the joint fluid in the joint. The dual role of the labrum aids in distributing the forces in the hip joint.48,55,56 There is much variability in the literature regarding the morphologic appearance of the labrum, especially with advancing age.1 Predisposing conditions also lead to early labral pathology, such as femoroacetabular impingement syndromes and developmental dysplasia of the hip.48
Patients with labral pathology typically present with pain localizing to the hip, groin, pelvis, or medial knee. They occasionally describe locking, clicking, or catching. Plain radiographs are typically not diagnostic.69 MR arthrography has become the least invasive study of choice to evaluate the labrum at many institutions. The sensitivity of MR arthrography to diagnose labral pathology may be as high as 92% when using a small field of view with adequate distention of the hip with contrast.69 Sensitivities for conventional MRI of the hip have ranged from 8% to 25% using large field of view and small field of view, respectively.1 In a study by Mintz et al, a sensitivity of 97% and an accuracy of 95% were reported in an evaluation of 92 patients, using arthroscopy as the standard.38
Studies have been performed to evaluate the normal imaging appearance of the labrum in asymptomatic patients. In 2000, Abe et al evaluated 71 asymptomatic hips, with radial sectioning perpendicular to the acetabular labrum at 30° intervals.1 Patients were stratified according to age; the shape and signal intensity of the labrum were evaluated for each age group. The shape of the labrum was triangular in 80% of the segments, round in 13%, irregular in 7%, and absent in 1%. Homogeneous low-signal intensity was seen in 56% (Figure 1). The triangular shape predominated in young patients, and an irregular or rounded appearance became more pronounced in the older age groups. Signal characteristics also increased with increasing age. The data suggest significant variability in the imaging appearance of the labrum and a complex direct correlation between imaging appearance and a patient’s clinical presentation.32
Figure 1.
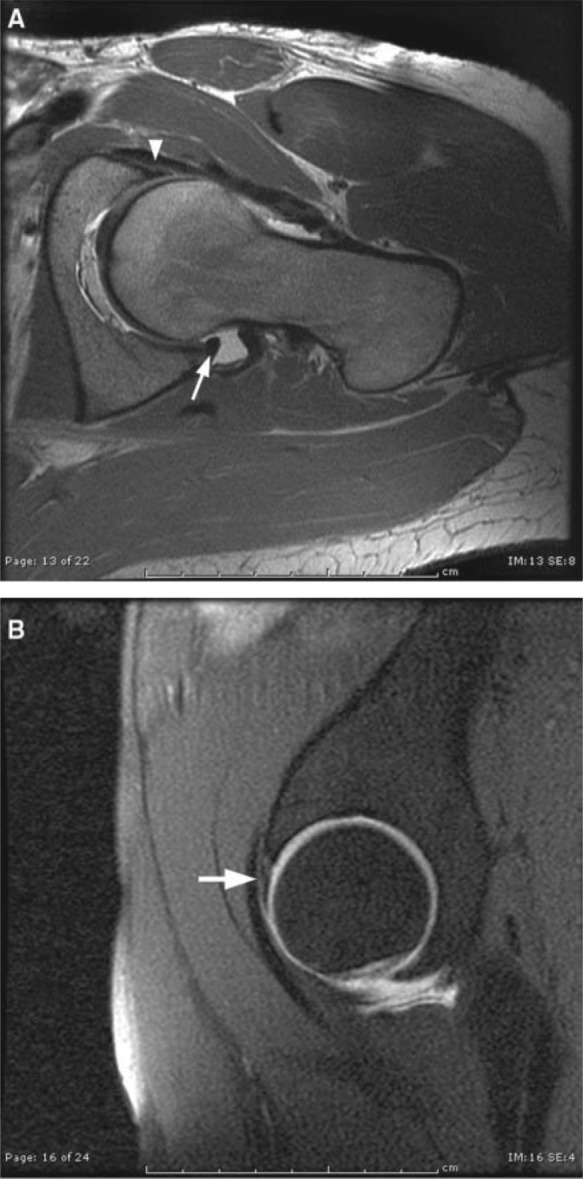
Normal acetabular labrum. Axial oblique proton-density image (A) and sagittal fat-suppressed T1-weighted image (B) from a magnetic resonance arthrogram show a normal acetabular labrum. On the axial oblique image, the anterior (arrowhead) and posterior (arrow) labrum is uniformly low signal with no contrast tracking into the labral substance; the sagittal image illustrates the normal low-signal anterior–superior labrum (arrow).
Several pitfalls have been encountered with imaging the acetabular labrum. A common site of observer misinterpretation involves the presence of a normal sulcus at the anterosuperior aspect of the joint. There is also significant variability at the labral junction with the transverse ligament inferiorly. Considerable variability is also seen at the labral cartilaginous interface.16 Multiple cadaveric studies of the labrum have been performed demonstrating that a significant majority of true labral tears occur at the anterior superior labral margin.49,70
Two types of labral pathology have been described33,48: fraying at the labral articular junction and tearing of the labrum with separation from the articular cartilage. Fraying can occur at any point within the labrum, whereas separation occurs in the anterior aspect of the joint in 86% of patients.33,48 A direct correlation has been found between labral pathology and articular cartilage defects with subsequent development of osteoarthritis.48 In a study by McCarthy and colleagues, 73% of labral lesions were accompanied by a cartilaginous lesion.33,56
Findings at MR arthrography that suggest a tear include contrast intravasation and undermining of the labrum.48 Any extension of contrast into the acetabular labral junction should be considered abnormal (Figure 2). The presence of paralabral cysts further supports the presence of labral pathology24,55 (Figure 3).
Figure 2.
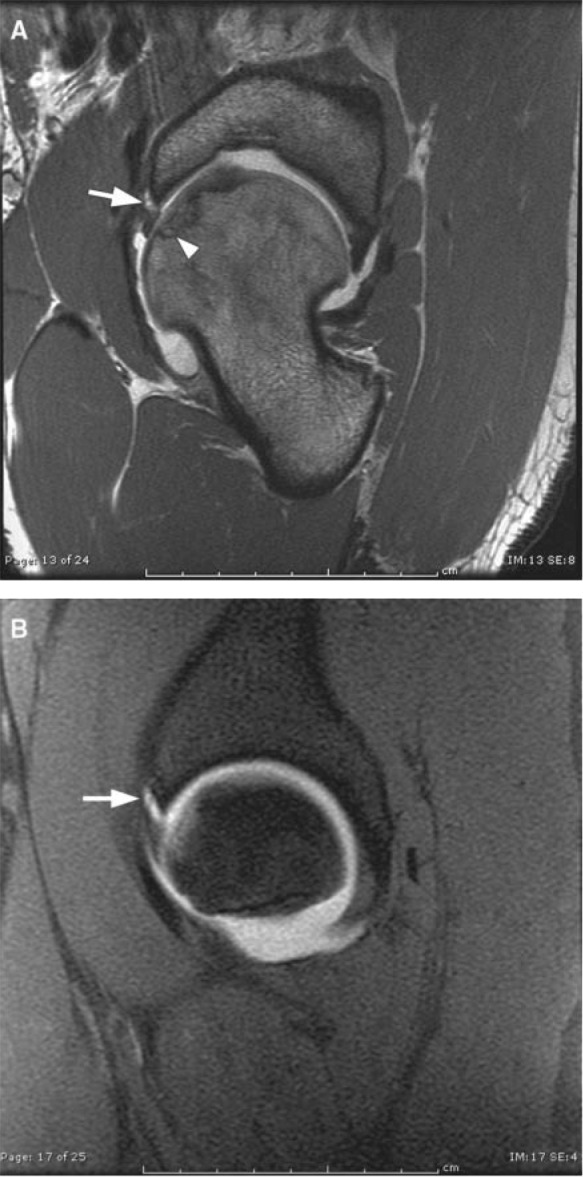
Acetabular labral tear. Axial oblique proton-density image (A) and sagittal fat-suppressed T1 images (B) from a magnetic resonance arthrogram show an acetabular labral tear. On the axial oblique image (A), there is contrast (high signal) tracking between the acetabular labrum and the bony acetabulum (arrow). Note the articular cartilage irregularity and subchondral changes in the femoral head (arrowhead). The sagittal fat-suppressed T1-weighted image (B) again shows contrast tracking between the acetabulum and fibrocartilaginous labrum anterosuperiorly (arrow).
Figure 3.
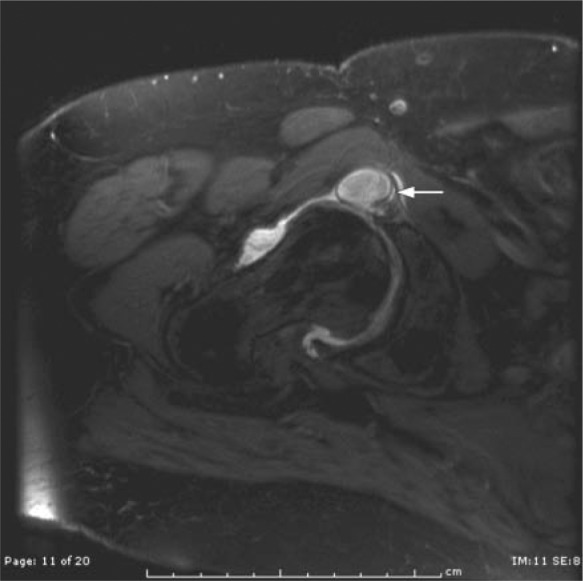
Acetabular labral tear with paralabral cyst. Axial oblique fat-suppressed proton-density image shows a large cyst emanating from the anterior superior labrum (arrow), which confirms the diagnosis of a labral tear.
As the ability to image the acetabular labrum improves, so will our knowledge of labral pathology and its relationship to clinical presentation.
Femoral Acetabular Impingement
Although the causative factors for osteoarthritis of the hip are extensive, femoroacetabular impingement syndrome should not be missed in the early setting.20,66
Femoroacetabular impingement is abnormal contact between the acetabular rim and the proximal femur as a result of morphological abnormalities affecting the acetabulum, proximal femur, or both.
The clinical manifestations of femoroacetabular impingement include hip and groin pain with flexion and internal rotation of the hip.26 Femoroacetabular impingement can be further subdivided into cam impingement and pincer impingement, with the former occurring more commonly in young men (average age of 32 years) and the latter occurring more commonly in middle-aged women (average age, 40 years).65 The majority of patients with femoroacetabular impingement have a combination of the cam and pincer forms (approximately 86%) versus either one alone (approximately 14%).5
Cam Impingement
The principal problem with cam impingement is incomplete sphericity at the anterior-to-anterolateral aspect of the femoral head-neck junction, which results in compression and shear stresses at the anterosuperior labrum and cartilage interface during hip flexion.5,10,11,17,29,33,54 The result is a labrum that is stretched and pushed laterally and cartilage that is compressed and pushed medially, allowing for separation between the labrum and cartilage and for cartilage shearing.5
A lack of sphericity of the femoral head-neck junction is usually caused by a growth abnormality of the capital femoral epiphysis.60 A number of other causes have been described and include slipped capital femoral epiphysis,21,30,31 Legg-Calvé-Perthes disease,40,62 increased femoral anteversion,68 and prior femoral neck fractures.20,63
The abnormal sphericity at the femoral head-neck junction often presents as an osseous bump or a flattened head-neck junction anterosuperiorly (previously described as a pistol-grip deformity)64 (Figure 4).
Figure 4.
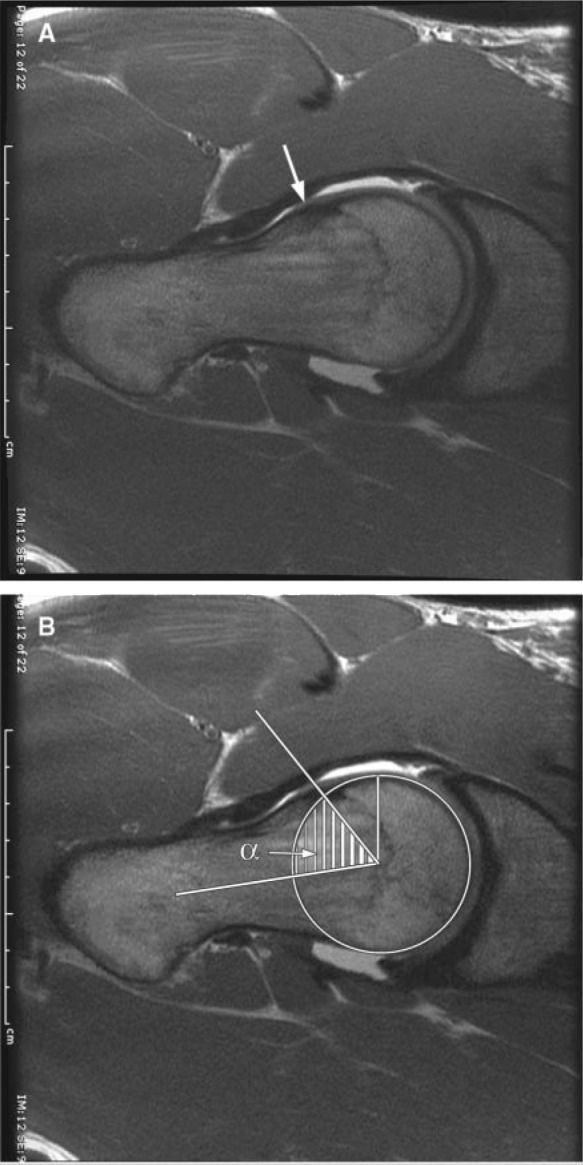
Cam femoral acetabular impingement. Axial oblique proton density images (A) show a bony prominence at the femoral head neck junction (arrow) consistent with a cam-type femoral acetabular impingement. The second image (B) shows how the alpha angle is measured.
The asphericity of the femoral head can be evaluated by the alpha angle and the femoral head-neck offset.42 The alpha angle is measured between the femoral neck axis and a line connecting the center of the femoral head with the starting point of the head-neck junction asphericity. An angle exceeding 50° is indicative of an abnormal femoral head-neck contour65 (Figure 4). The amount of femoral head-neck offset is defined as the difference in radius between the anterior femoral head and the anterior femoral neck, with a femoral head-neck offset less than 10 mm being a strong indicator for cam impingement.65
Pincer Impingement
The principal problem with pincer impingement is a deep socket, which limits range of motion by the overcoverage.5 At the extremes of hip motion, the femoral neck impacts the labrum, which acts like a bumper and is consequently compressed between the femoral neck and the underlying acetabulum. The force is transmitted along a narrow band of cartilage along the acetabular rim.5 Because the majority of hip motion is flexion, most of the articular cartilage injuries are centered along the anterosuperior acetabular rim.5 With continued abutment of the femoral head against the acetabulum, it can sublux posteriorly, creating contrecoup cartilage injuries to the posteroinferior acetabulum by impaction against the posteromedial aspect of the femoral head.5,8 Continued abutment of the femoral head against the acetabulum can also lead to bone growth at the base of the labrum, leading to further deepening of the acetabulum and worsening overcoverage.6,20,59
Unlike the cam effect, the cartilage damage in pincer impingement tends to be focal and confined to a small circumferential strip near the labrum.5 Abnormalities that result in overcoverage and are intimately associated with pincer impingement include coxa profunda, protrusio acetabuli, and acetabular retroversion.6,20,59
The anteroposterior radiograph of a normal hip routinely demonstrates the acetabular fossa line lying lateral to the ilioischial line (Figure 5). In the setting of coxa profunda, the acetabular fossa line touches or overlaps the ilioischial line medially. In the setting of protrusio acetabuli, the femoral head overlaps the ilioischial line medially.65
Figure 5.
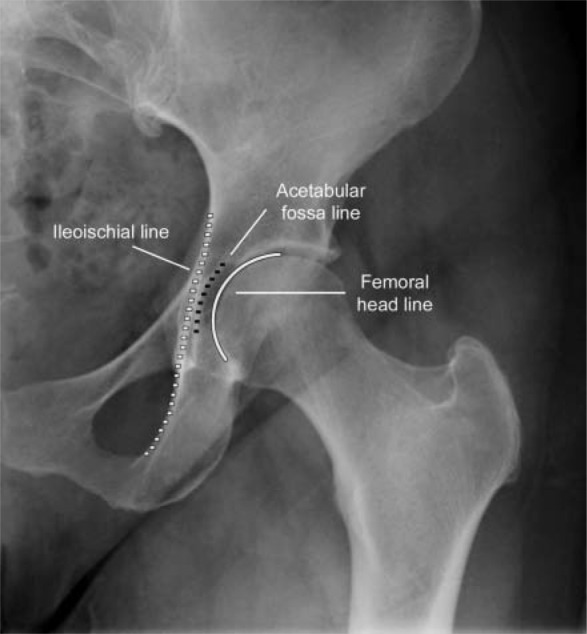
Normal hip. Anteroposterior radiograph of the left hip demonstrates the normal relationship of the acetabular fossa line and the femoral head lines lateral to the ilioischial line.
The acetabular opening is anteverted in relation to the normal hip and is posteriorly oriented when retroverted.52,59 The diagnosis of acetabular retroversion can be made on an anteroposterior radiograph of the pelvis by searching for the crossover, or figure of 8, and posterior wall signs.52,59 The crossover sign is the result of overlapping radiodensities created by the anterior aspect of the acetabular rim being more laterally located than the posterior aspect of the acetabular rim, at the level of the superior acetabulum.8 The posterior wall sign refers to the shadow of the posterior edge of the posterior wall of the acetabulum, which in the retroverted acetabulum lies medial to the center point of the femoral head.52,59
Alternatively, excessive acetabular coverage can be quantified with the lateral center edge angle.39,68 This angle is formed by a vertical line at the femoral head center and a line connecting the femoral head center with the lateral edge of the acetabulum; an angle of 39° or greater is indicative of acetabular overcoverage.39,68
Muscle Injuries
Muscle strains are the most common injuries around the hip and groin related to athletic competition.4 Muscle strains commonly occur at the myotendinous junction, the weakest point in the musculotendinous unit. Muscles that are prone to strains typically cross 2 joints, have a high percentage of fast-twitch muscle fibers, and have a propensity for eccentric contraction.46
Muscle strains are clinically graded as first, second, or third degree.72 First-degree strains, or stretch injuries, are characterized on MRI as edema surrounding the myotendinous junction, without disruption or hematoma. Second-degree strains on MRI show partial-thickness tears of the myotendinous junction manifested by edema, hematoma, and partial disruption of the myotendinous junction (Figure 6). Complete myotendinous rupture, or third-degree strain, is typically diagnosed clinically by retracted muscle fibers and complete loss of function (Figure 7). MRI can document complete disruption of the myotendinous margins and retracted muscle. MRI can also differentiate tendon avulsions and myotendinous rupture, which is essential when considering surgical therapy. This is of considerable importance in the juvenile or adolescent athlete, especially in the region of the pelvis, where apophyseal avulsions are more common for this age group. Additionally, MRI may have prognostic implications if greater than 50% of the cross-sectional area of the muscle is involved or if fluid collections are present. These factors have been associated with longer recovery times.50 MRI may assist in evaluating complications of muscle injuries, such as chronic hamstring injury, where the sciatic nerve may scar to the retracted tendon.
Figure 6.
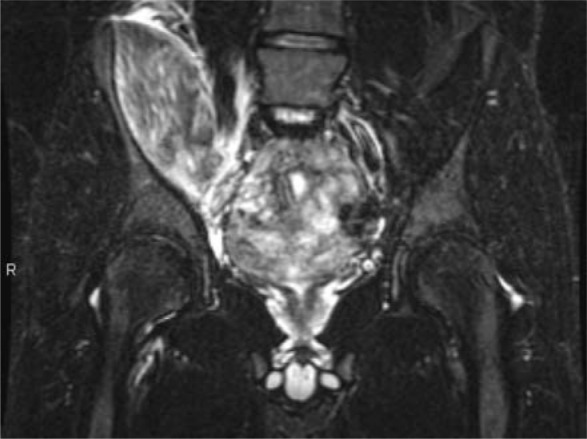
Second-degree muscle strain. Coronal fat-suppressed T2-weighted image demonstrates moderate muscle edema in the right iliopsoas muscle consistent with a grade II strain.
Figure 7.
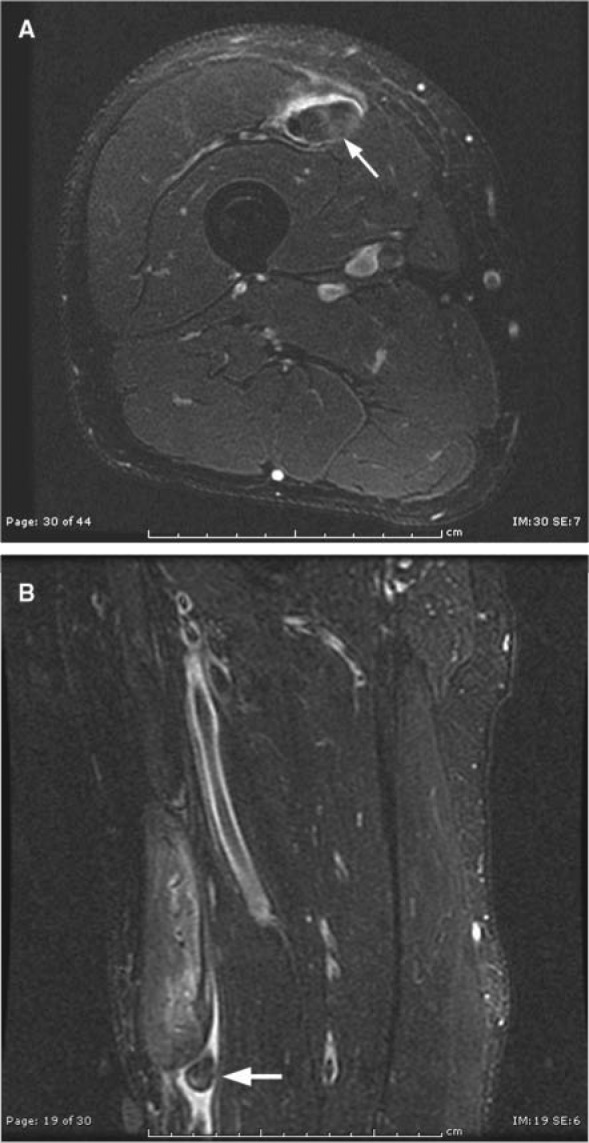
Third-degree muscle strain. Axial (A) and sagittal (B) fat-suppressed T2-weighted images demonstrate complete discontinuity of the deep tendon of the rectus femoris in the midthigh. The tendon (arrow) is seen with surrounding edema.
Muscle contusions are often seen in contact sports such as football. Direct trauma causes blood vessel disruption, hemorrhage, and edema. These are seen on MRI as increased signal on T2 or inversion recovery sequences with a feathery pattern not centered on the myotendinous junction (Figure 8). Contusions may be associated with hematomas, which can limit range of motion and cause prolonged disability. The hematomas can also ossify (myositis ossificans), which can be confused with a soft tissue sarcoma on MRI and pathology. Plain radiography may discern the peripheral ossification seen with myositis ossificans from the central ossification seen with osteogenic sarcoma.
Figure 8.
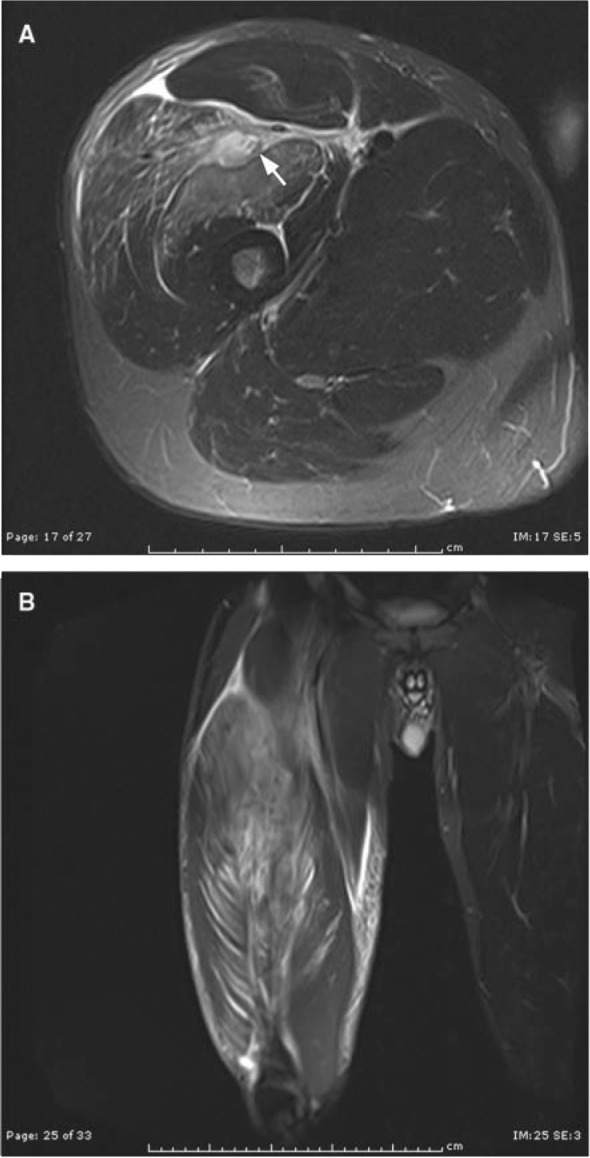
Muscle contusion. Axial (A) and coronal (B) STIR images (short TI inversion recovery; edema sensitive) demonstrate a feathery pattern of muscle edema involving the vastus lateralis and vastus medialis with an interfascial hematoma between these 2 muscles (arrow).
Athletic Pubalgia
Groin pain in the athlete is a relatively common occurrence, with a long differential diagnosis. Pain in or around the pubic symphysis may be a sports hernia, or athletic pubalgia.43 Imaging has traditionally been an ineffective tool in the evaluation of this entity. More recently, the pathophysiology of athletic pubalgia has become more clear, and MRI has increasingly become important in diagnosis and directing treatment.3,41
The pubic symphysis is a diarthrodial joint composed of paired pubic bones separated by a fibrocartilaginous disc. The pubic bone is divided into the pubic body (which is adjacent to the symphysis) and the inferior and superior rami (which project like osseous struts off the body).19,71 The pubic symphysis is the centerpiece of numerous musculotendinous attachments that act to dynamically stabilize the position of the anterior pelvis. Muscles that attach to the symphysis include the anterolateral abdominal (rectus abdominis [RA], transversus abdominis, external and internal obliques) and thigh adductors (AD; pectineus, AD longus, AD brevis, and AD magnus). The most important of these for maintaining stability of the anterior pelvis are the RA and AD longus (Figure 9). The RA insertion–AD origin is an important structure, rather than 2 separate attachments, and is more aptly described as an aponeurosis because they blend. The lateral edge of the RA attachment is only millimeters from the superficial inguinal ring, undoubtedly a contributing factor in the overlap of RA insertional pathology and inguinal hernia symptoms.43,58
Figure 9.
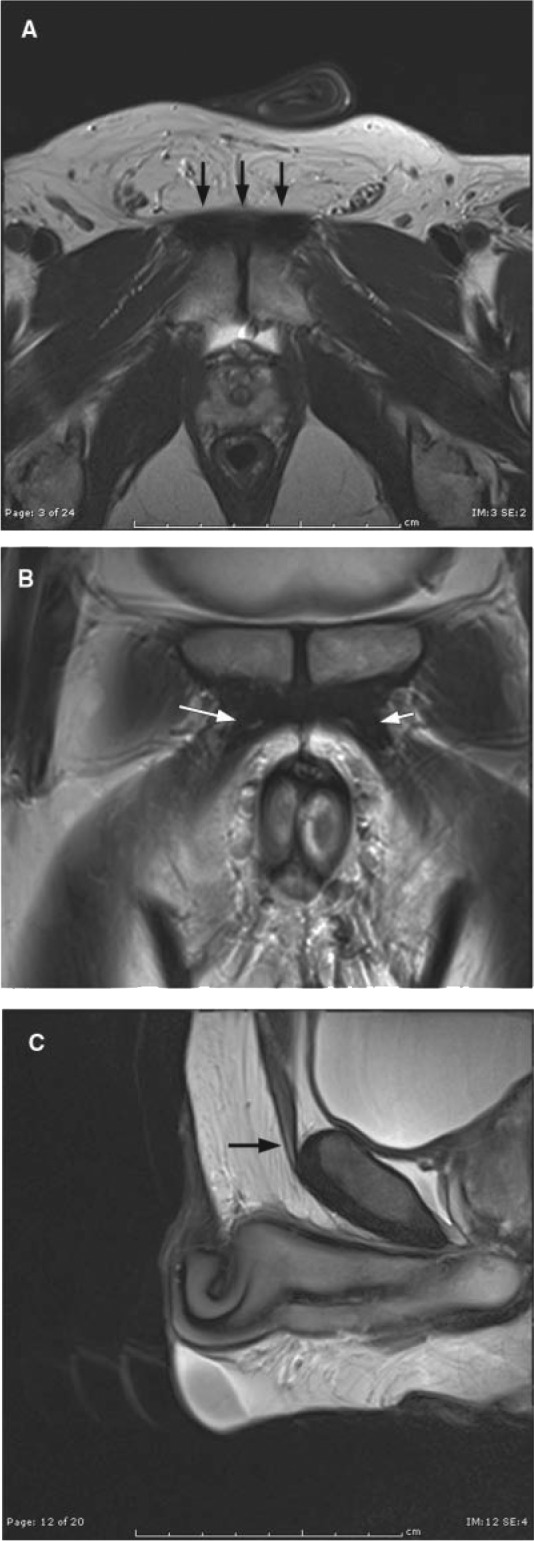
Normal appearance of the rectus abdominis, adductor longus, and their aponeurosis. Axial (A), coronal (B), and sagittal (C) T2-weighted images demonstrate the normal appearance of the rectus abdominis and adductor longus aponeurosis (A; arrows), adductor longus tendons (B; arrows), and rectus abdominis tendon (arrow).
Clinically, athletic pubalgia is classically described as groin pain in high-performance athletes that localizes to the region of the pubic symphysis, with point tenderness on examination over the superficial inguinal ring and without findings of an inguinal hernia.23,34,61 The term sports hernia is an unfortunate and confusing moniker that refers to the initial and erroneous belief that this clinical syndrome was caused by a subclinical inguinal hernia.18,44 It has become clear that few of these patients have hernias. Athletic pubalgia is an injury to the myotendinous structures adjacent to the symphysis pubis that stabilize the anterior pelvis.2,35,36,45,67 Meyer et al reported at least 17 separate clinical syndromes that fall under the umbrella of athletic pubalgia.37 The most common injuries involve the RA and/or AD longus attachments and the associated aponeurosis, where imaging efforts have been directed.35
Imaging patients with athletic pubalgia was thought to be of little value; that has recently changed. Omar et al advocated a survey approach with use of large-field-of-view images to confirm pubic injury and exclude pathology in more remote areas, followed by dedicated imaging of the anterior pubic musculoskeletal structures to further characterize the abnormalities.43 Tears of the RA–AD aponeurosis can often be directly visualized on water-sensitive images as irregular areas of fluid intensity (Figure 10). Other secondary findings of an RA–AD aponeurosis injury include marrow edema isolated to the anterior inferior aspect of the pubic body. The secondary cleft sign may also be seen (an abnormal inferior extension of the central symphyseal fibrocartilaginous cleft along the anteroinferior margin of the pubic body), as may an edematous or atrophic appearance or frank disruption of the RA near its pubic attachment. Thigh AD injuries can also be readily identified—most commonly, the AD longus—including tendon tears or edema at the myotendinous junction compatible with strain. Injury to the myotendinous structures in and around the symphysis pubis creates instability.43 Over time, these injuries can evolve, and initially intact structures may become compromised.43 For instance, an isolated RA attachment injury may extend to involve the contralateral side if untreated.9,14,53,58
Figure 10.
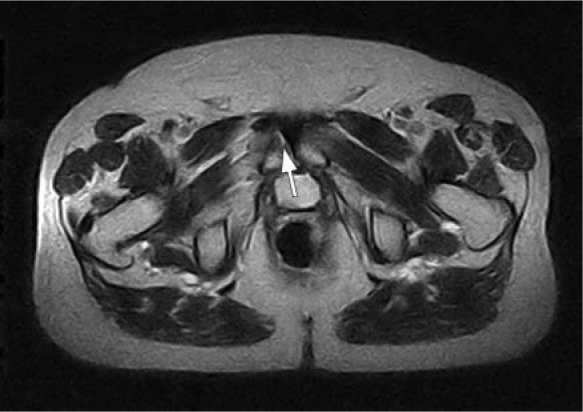
Disruption of the rectus abdominis–adductor longus aponeurosis. Axial T2-weighted image of the pelvis demonstrates fluid signal at the right aponeurosis (arrow) consistent with a tear.
Shortt et al reported several reproducible patterns of MRI, characterizing injuries in patients presenting with clinical evidence of a “sports hernia.”58 The first was confluent edema extending from anterior to posterior on either side of the symphysis, consistent with osteitis pubis. Other patterns related to RA insertional pathology or RA–AD aponeurosis injuries include pubic marrow edema 1 cm to 2 cm lateral to the symphysis and MR secondary cleft sign (likely indicating disruption of the pubic symphysis capsule as it blends with the RA–AD aponeurosis). Marrow edema at the anteroinferior pubis, a secondary cleft sign, and edema along the lateral edge of the RA attachment and AD longus origin indicate injury at the lateral aspect of the aponeurosis (incidentally near the superficial inguinal ring). Edema may also be seen at the anteroinferior aspect of the pubis bilaterally, with bilateral secondary cleft signs and direct visualization of a discrete breech of the medial rectus abdominis attachment extending across midline to involve the contralateral attachment. Distinguishing between these types of injuries is thought to be important in directing treatment.58 In a study undertaken by Zoga et al, the sensitivity and specificity of MR for detecting RA tendon injuries and AD tendon injuries was reported as 68% and 100% (RA) and 86% and 89% (AD), indicating the promise and limitations of MR evaluation. A challenge is to decrease the number of false-negative evaluations.73
Osseous Injuries
Stress fractures are common injuries and may account for up to 10% of injuries seen in a sports medicine clinic.7 Under normal physiologic conditions, bone is continually remodeling. In the setting of fatigue damage, bone remodeling occurs in response to small cracks. This process is normal for the physiologic development and maintenance of bone, but with increased loading there is increased damage to the microstructure of bone. If this damage to bone exceeds the capacity for bone to repair or if there are deficient repair mechanisms, a stress fracture will ensue.12 There are 2 groups of stress fractures: fatigue and insufficiency. Fatigue fractures result from abnormal forces applied to underlying normal bone; conversely, insufficiency fractures are due to normal forces applied to underlying abnormal bone. Fatigue fractures are most commonly seen in runners, but they also occur with an intense increase in physical activity or a recent uptick in training regimen.25,27,47 Female athletes and the military population are at increased risk.28 Common sites of injury around the hip and pelvis include the femoral neck, inferior pubic ramus, and sacrum. Although the symptoms of these injuries are mostly activity related, they are frequently nonspecific, which necessitates the need for accurate imaging because treatments are site specific.
Fatigue fractures of the femoral neck are classified into compression and distraction types.57 The compression types occur at the inferior medial aspect of the femoral neck along compression trabeculae or calcar (Figure 11). These fractures are usually treated conservatively because they do not have the tendency to displace.57 Conversely, distraction-type fatigue fractures occur through the tensile trabeculae along the superior surface of the femoral neck and propagate across the neck. These fractures can displace; they are associated with a higher morbidity; and they are treated aggressively.45,57
Figure 11.
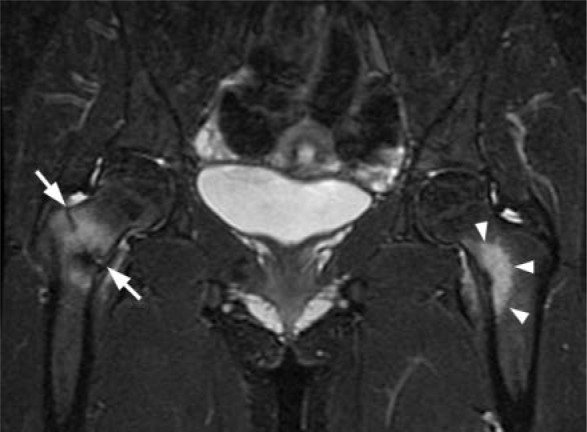
Stress fracture. Coronal fat-suppressed T2-weighted image of the hips demonstrates marrow edema in the left hip (arrowheads) with no appreciable fracture line. In the right hip, there is an incomplete fracture line at the base of the femoral neck (arrows) involving the superior and inferior cortices with surrounding marrow edema.
Initial imaging of hip and pelvic stress fractures should include an anteroposterior view of the pelvis, with the femurs internally rotated, and a cross-table lateral view of the affected hip. In the setting of femoral neck stress fractures, fewer than 10% of radiographs are positive within the first week of pain onset.57 Additional studies have shown that fewer than 55% of patients ever demonstrate radiographic evidence of osseous change.22,51 MRI is the gold standard for classification of stress-related osseous injuries of the hip and pelvis.12 The MR findings include marrow edema on the water-sensitive images (fat-suppressed T2 or inversion recovery) typically in a bandlike distribution in the region of the fracture. Occasionally, a fracture line is seen on either the water-sensitive or T1-weighted sequences (Figure 11). Although nuclear scintigraphy is sensitive for stress fractures, the lack of soft tissue sensitivity and delineation, as well as the radiation dose related to the scans, makes them less appealing than MRI.
Conclusion
Sports-related injuries around the hip and groin are a diverse group of injuries that can be difficult to diagnose and manage and often require a multidisciplinary team of caregivers. MRI can be extremely helpful in the diagnosis and triage of these patients and may expedite their return to athletics.
Footnotes
No potential conflicts of interest declared.
References
- 1. Abe I, Harada Y, Oinuma K, et al. Acetabular labrum: abnormal finding at MR imaging in asymptomatic hips. Radiology. 2000;216:576-581 [DOI] [PubMed] [Google Scholar]
- 2. Ahumada LA, Ashruf S, Espinosa-de-los-Monteros A, et al. Athletic pubalgia: definition and surgical treatment. Ann Plast Surg. 2005;55:393-396 [DOI] [PubMed] [Google Scholar]
- 3. Albers SL, Spritzer CE, Garrett WE, Jr, Meyers WC. MR findings in athletes with pubalgia. Skeletal Radiol. 2001;30:270-277 [DOI] [PubMed] [Google Scholar]
- 4. Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med. 2001;29:521-533 [DOI] [PubMed] [Google Scholar]
- 5. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012-1018 [DOI] [PubMed] [Google Scholar]
- 6. Beck M, Leunig M, Parvizi J, et al. Anterior femoroacetabular impingement, part II: midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67-73 [PubMed] [Google Scholar]
- 7. Boyd KT, Peirce NS, Batt ME. Common hip injuries in sport. Sports Med. 1997;24:273-288 [DOI] [PubMed] [Google Scholar]
- 8. Bredella MA, Stoller DW. MR imaging of the femoroacetabular impingement. Magn Reson Imaging Clin N Am. 2005;13:653-664 [DOI] [PubMed] [Google Scholar]
- 9. Brennan D, O’Connell MJ, Ryan M, et al. Secondary cleft sign as a marker of injury in athletes with groin pain: MR image appearance and interpretation. Radiology. 2005;235(1):162-167 [DOI] [PubMed] [Google Scholar]
- 10. Byers PD, Contepomi CA, Farkas TA. A post mortem study of the hip joint: including the prevalence of the features of the right side. Ann Rheum Dis. 1970;29:15-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Byrd JW. Labral lesions: an elusive source of hip pain. Arthroscopy. 1996;12:603-612 [DOI] [PubMed] [Google Scholar]
- 12. Campbell SE, Fajardo RS. Imaging of stress injuries of the pelvis. Semin Musculoskelet Radiol. 2008;12:62-71 [DOI] [PubMed] [Google Scholar]
- 13. Crowninshield RD, Johnston RC, Andrews JG, et al. A biomechanical investigation of the human hip. J Biomech. 1978;11:75-85 [DOI] [PubMed] [Google Scholar]
- 14. Cunningham PM, Brennan D, O’Connell M, MacMahon P, O’Neill P, Eustace S. Patterns of bone and soft–tissue injury at the symphysis pubis in soccer players: observations at MRI. AJR Am J Roentgenol. 2007;188:W291-W296 [DOI] [PubMed] [Google Scholar]
- 15. DeLee JC, Farney WC. Incidence of injury in Texas high school football. Am J Sports Med. 1992;20:575-580 [DOI] [PubMed] [Google Scholar]
- 16. Dinauer PA, Murphy KP, Carroll JF. Sublabral sulcus at the posteroinferior acetabulum: a potential pitfall in MR Arthrography diagnosis of acetabular labral tears. AJR. 2004;183:1745-1753 [DOI] [PubMed] [Google Scholar]
- 17. Fitzgerald RH., Jr Acetabular labrum tears: diagnosis and treatment. Clin Orthop Relat Res. 1995;311:60-68 [PubMed] [Google Scholar]
- 18. Fon LJ, Spence RA. Sportsman’s hernia. Br J Surg. 2000;87:545-552 [DOI] [PubMed] [Google Scholar]
- 19. Gamble JG, Simmons SC, Freedman M. The symphysis pubis: anatomic and pathologic considerations. Clin Orthop Relat Res. 1986;203:361-272 [PubMed] [Google Scholar]
- 20. Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112-120 [DOI] [PubMed] [Google Scholar]
- 21. Goodman DA, Feighan JE, Smith AD, Latimer B, Buly RL, Cooperman DR. Subclinical slipped capital femoral epiphysis: relationship to osteoarthrosis of the hip. J Bone Joint Surg Am. 1997;79:1489-1497 [DOI] [PubMed] [Google Scholar]
- 22. Greaney RB, Gerber FH, Laughlin RL, et al. Distribution and natural history of stress fractures in US Marine recruits. Radiology. 1983;146(2):339-346 [DOI] [PubMed] [Google Scholar]
- 23. Hackney RG. The sports hernia: a cause of chronic groin pain. Br J Sports Med. 1993;27:58-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hase T, Ueo T. Acetabular labral tear: arthroscopic diagnosis and treatment. Arthroscopy. 1999;15:138-141 [DOI] [PubMed] [Google Scholar]
- 25. Hulkko A, Orava S. Stress fractures in athletes. Int J Sports Med. 1987;8:221-226 [DOI] [PubMed] [Google Scholar]
- 26. Ito K, Minka MA, II, Leunig M, Werlen S, Ganz R. Femoracetabular impingement and the cam-effect: an MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171-176 [DOI] [PubMed] [Google Scholar]
- 27. Jones BH, Harris JM, Vinh TN, Rubin C. Exercise-induced stress fractures and stress reactions of bone: epidemiology, etiology, and classification. Exerc Sport Sci Rev. 1989;17:379-422 [PubMed] [Google Scholar]
- 28. Kiuru MJ, Pihlajamaki HK, Ahovuo JA. Fatigue stress injuries of the pelvic bones and proximal femur: evaluation with MR imaging. Eur Radiol. 2003;13:605-611 [DOI] [PubMed] [Google Scholar]
- 29. Lage LA, Patel JV, Villar RN. The acetabular labral tear: an arthroscopic classification. Arthroscopy. 1996;12:269-272 [DOI] [PubMed] [Google Scholar]
- 30. Leunig M, Casillas MM, Hamlet M, et al. Slipped capital femoral epiphysis: early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Orthop Scand. 2000;71:370-375 [DOI] [PubMed] [Google Scholar]
- 31. Leunig M, Fraitzl CR, Ganz R. Early damage to the acetabular cartilage in slipped capital femoral epiphysis: therapeutic consequences. Orthopade. 2002;31:894-899 [DOI] [PubMed] [Google Scholar]
- 32. McCarthy JC. The diagnosis and treatment of labral and chondral lesions. AAOS Instr Course Lect. 2004;53:573-577 [PubMed] [Google Scholar]
- 33. McCarthy JC, Noble PC, Schuck MR, et al. The role labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res. 2001;393:25-37 [DOI] [PubMed] [Google Scholar]
- 34. Malychia P, Lovell G. Inguinal surgery in athletes with chronic groin pain: the “sportsman’s” hernia. Aust N Z J Surg. 1992;62:123-125 [DOI] [PubMed] [Google Scholar]
- 35. Meyers WC, Foley DP, Garrett WE, Lohnes JH, Mandlebaum BR. Management of severe lower abdominal or inguinal pain in high-performance athletes: PAIN (Performing Athletes With Abdominal or Inguinal Neuromuscular Pain Study Group). Am J Sports Med. 2000;28:2-8 [DOI] [PubMed] [Google Scholar]
- 36. Meyers WC, Lanfranco A, Castellanos AE. Surgical management of chronic lower abdominal and groin pain in high-performance athletes. Curr Sports Med Rep. 2001;1:301-305 [DOI] [PubMed] [Google Scholar]
- 37. Meyers WC, McKechnie A, Philippon MJ, Horner MA, Zoga AC, Devon ON. Experience with “sports hernia” spanning two decades. Ann Surg. 2008;248:656-665 [DOI] [PubMed] [Google Scholar]
- 38. Mintz DN, Hooper T, Connell D, Buly R, Padgett DE, Potter HG. Magnetic resonance imaging of the hip: detection of labral and chondral abnormalities using noncontrast imaging. Arthroscopy. 2005;21:385-393 [DOI] [PubMed] [Google Scholar]
- 39. Murphy SB, Kijewski PK, Millis MB, Harless A. Acetabular dysplasia in the adolescent and young adult. Clin Orthop Relat Res. 1990;261:214-223 [PubMed] [Google Scholar]
- 40. Murphy SB, Tannast M, Kim YJ, Buly R, Millis MB. Débridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res. 2004;429:178-181 [DOI] [PubMed] [Google Scholar]
- 41. Nelson EN, Kassarjian A, Palmer WE. MR imaging of sports-related groin pain. Magn Reson Imaging Clin N Am. 2005;13:727-742 [DOI] [PubMed] [Google Scholar]
- 42. Nötzli HP, Wyss TF, Stöcklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556-560 [DOI] [PubMed] [Google Scholar]
- 43. Omar IM, Zoga AC, Kavanagh EC, et al. Athletic pubalgia and “sports hernia”: optimal MR imaging technique and findings. Radiographics. 2008;28:1415-1438 [DOI] [PubMed] [Google Scholar]
- 44. Orchard JW, Read JW, Neophyton J, Garlick D. Groin pain associated with ultrasound findings of inguinal canal posterior wall deficiency in Australian Rules footballers. Br J Sports Med. 1998;32:134-139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Overdeck KH, Palmer WE. Imaging of hip and groin injuries in athletes. Semin Musculoskelet Radiol. 2004;8:41-55 [DOI] [PubMed] [Google Scholar]
- 46. Palmer WE, Kuong SJ, Elmadbouh HM. MR imaging of myotendinous strain. AJR Am J Roentgenol. 1999;173:703-709 [DOI] [PubMed] [Google Scholar]
- 47. Pentecost RL, Murray RA, Brindley HH. Fatigue, insufficiency, and pathologic fractures. JAMA. 1964;187:1001-1004 [DOI] [PubMed] [Google Scholar]
- 48. Petersilge Cheryl MD. Imaging of the acetabular labrum. Magn Reson Imaging Clin N Am. 2005;13:641-652 [DOI] [PubMed] [Google Scholar]
- 49. Peterson W, Peterson F, Tillman B. Structure and vascularization of the acetabular labrum with regard to the pathogenesis and healing of labral lesions. Arch Orthop Trauma Surg. 2003;123:283-288 [DOI] [PubMed] [Google Scholar]
- 50. Pomeranz SJ, Heidt RS., Jr MR imaging in the prognostication of hamstring injury. Radiology. 1993;189:897-900 [DOI] [PubMed] [Google Scholar]
- 51. Prather JL, Nusynowitz ML, Snowdy HA, Hughes AD, McCartney WH, Bagg RJ. Scintigraphic findings in stress fractures. J Bone Joint Surg Am. 1977;59:869-874 [PubMed] [Google Scholar]
- 52. Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum: a cause of hip pain. J Bone Joint Surg Br. 1999;81:281-288 [DOI] [PubMed] [Google Scholar]
- 53. Robinson P, Barron DA, Parsons W, Grainger AJ, Schilders EM, O’Connor PJ. Adductor-related groin pain in athletes: correlation of MR imaging with clinical findings. Skeletal Radiol. 2004;33:451-457 [DOI] [PubMed] [Google Scholar]
- 54. Santori N, Villar R. Arthroscopic findings in the initial stages of hip osteoarthritis. Orthopedics. 1999;22:405-409 [DOI] [PubMed] [Google Scholar]
- 55. Schnarkowski P, Steinbach LS, Tirman PF, et al. Magnetic resonance imaging of labral cysts of the hip. Skeletal Radiol. 1996;25:733-737 [DOI] [PubMed] [Google Scholar]
- 56. Seldes RM, Tan V, Hunt J, et al. Anatomy, histologic features and vascularity of the adult acetabular labra. Clin Orthop Relat Res. 2001;382:232-240 [DOI] [PubMed] [Google Scholar]
- 57. Shin AY, Gillingham BL. Fatigue fractures of the femoral neck in athletes. J Am Acad Orthop Surg. 1997;5:293-302 [DOI] [PubMed] [Google Scholar]
- 58. Shortt CP, Zoga AC, Kavanaghh EC, Meyers WC. Anatomy, pathology, and MRI findings in the sports hernia. Semin Musculoskelet Radiol. 2008;12:54-61 [DOI] [PubMed] [Google Scholar]
- 59. Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion: treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85:278-286 [DOI] [PubMed] [Google Scholar]
- 60. Siebenrock KA, Wahab KH, Kalhor M, Leunig M, Ganz R. Abnormal extension of the femoral head epiphysis as a cause of cam impingement. Clin Orthop Relat Res. 2004;418:54-60 [DOI] [PubMed] [Google Scholar]
- 61. Smodlaka VN. Groin pain in soccer players. Phys Sportsmed. 1980;8:57-61 [DOI] [PubMed] [Google Scholar]
- 62. Snow S, Keret D, Scarangella S, Bowen J. Anterior impingement of the femoral head: a late phenomenon of Legg-Calvé-Perthes’ disease. J Pediatr Orthop. 1993;13:286-289 [DOI] [PubMed] [Google Scholar]
- 63. Strehl A, Ganz R. Anterior femoroacetabular impingement after healed femoral neck fractures. Unfallchirurg. 2005;108:263-273 [DOI] [PubMed] [Google Scholar]
- 64. Stulberg SD, Cordell LD, Harris WH, Ramsey PL, MacEwen GD. Unrecognized childhood hip disease: a major cause of idiopathic osteoarthritis of the hip. In: The Hip: Proceedings of the Third Open Scientific Meeting of the Hip Society. St Louis, MO: CV Mosby Co; 1975:212-228 [Google Scholar]
- 65. Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis; what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540-1552 [DOI] [PubMed] [Google Scholar]
- 66. Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res. 2004;429:170-177 [PubMed] [Google Scholar]
- 67. Taylor DC, Meyers WC, Moylan JA, Lohnes J, Bassett FH, Garrett WE., Jr Abdominal musculature abnormalities as a cause of groin pain in athletes: inguinal hernia and pubalgia. Am J Sports Med. 1991;19:239-242 [DOI] [PubMed] [Google Scholar]
- 68. Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747-1770 [DOI] [PubMed] [Google Scholar]
- 69. Toomayan G, Holman WR, Major N, et al. Sensitivity of MR arthrography in the evaluation of acetabular labral tears. AMJ Am J Roentgenol. 2006;186:449-453 [DOI] [PubMed] [Google Scholar]
- 70. Walker JM. Histological study of the fetal development of the human acetabulum and labrum: significance in congenital hip disease. Yale J Biol Med. 1981;54:255-263 [PMC free article] [PubMed] [Google Scholar]
- 71. Williams A, ed. Thigh. In: Stranding S, ed. Gray’s Anatomy: The Anatomical Basis of Clinical Practice. 39th ed. Edinburgh, Scotland: Elsevier Churchill Livingstone; 2005:1465-1467 [Google Scholar]
- 72. Zarins B, Cuillo JV. Acute muscle and tendon injuries in athletes. Clin Sports Med. 1983;2:167-182 [PubMed] [Google Scholar]
- 73. Zoga AC, Kavanagh EC, Omar IM, et al. Athletic pubalgia and the “sports hernia”: MR imaging findings. Radiology. 2008;247:797-807 [DOI] [PubMed] [Google Scholar]


