Abstract
Context:
Posterior hip pain is a relatively uncommon but increasingly recognized complaint in the orthopaedic community. Patient complaints and presentations are often vague or nonspecific, making diagnosis and subsequent treatment decisions difficult. The purposes of this article are to review the anatomy and pathophysiology related to posterior hip pain in the athletic patient population.
Evidence Acquisition:
Data were collected through a thorough review of the literature via a MEDLINE search of all relevant articles between 1980 and 2010.
Results:
Many patients who complain of posterior hip pain actually have pain referred from another part of the body—notably, the lumbar spine or sacroiliac joint. Treatment options for posterior hip pain are typically nonoperative; however, surgery is warranted in some cases.
Conclusions:
Recent advancements in the understanding of hip anatomy, pathophysiology, and treatment options have enabled physicians to better diagnosis athletic hip injuries and select patients for appropriate treatment.
Keywords: posterior hip pain, piriformis syndrome, sciatica, referred pain, gluteal region
Injury to the hip joint is a relatively uncommon but important clinical problem in the athletic population. Any athlete—especially one participating in golf, soccer, or dancing—is at risk of hip injury; thus, it is important to recognize and treat injuries associated with the hip joint. In the past, patients with athletic hip injuries were typically treated conservatively, regardless of their diagnosis.34 Recently, however, the literature regarding hip pathology has grown, and advances in arthroscopic treatment† techniques and implants have increased the ability of athletes to return to sport following hip injury. Furthermore, improvements in various imaging modalities3,11,18,32,42,54 have increased the ability of physicians to understand the cause of hip disorders and to more accurately diagnosis the various pathologies.1 In actuality, the incidence of posterior hip injury may be climbing yet it is still underreported because of misdiagnosis.6
Hip pain can be classified in a variety of ways,34,50 including overall location (anterior, posterior, lateral, medial/groin), location about joint (intra-articular, extra-articular), and onset (acute/traumatic, insidious). In addition, some patients presenting with hip pain have problems that mimic hip pathology, or they have pain referred from other joints. In particular, posterior hip pain—the least common type of hip pain (compared to lateral and anterior hip pain)—is often due to factors outside the hip joint, as discussed below.
Recent advancements in the understanding of hip anatomy, pathophysiology, and treatment options have enabled physicians to better diagnosis athletic hip injuries and select patients for appropriate treatment. Although much is known about the posterior hip in terms of anatomy and physiology, there are, to our knowledge, no complete reviews in the literature thoroughly describing the pathophysiology, presentation, diagnostic tools, and treatment modalities for the management of posterior hip pain.
Anatomy
The hip joint receives loads up to 6 and 8 times the body weight during normal walking and jogging, respectively.51 When high-impact sports-related activities are factored in, the hip joint bears substantial load and is prone to injury. It is imperative that treating health care providers understand the anatomy of the hip joint and surrounding structures to fully appreciate the sometimes confusing clinical presentations and make accurate diagnosis and appropriate treatment plans.
The hip joint is composed of a complex interaction of bones, muscles, and connective tissue.43 The bony anatomy includes the acetabulum—which contains components of the ischium, ilium, and pubis bones—and the head of the femur. The acetabulum and femoral head articulate to form a spheroidal multiaxial ball-and-socket joint. A fibrous capsulolabral structure composed of the labrum48 and several ligaments17 supports the articulation between the acetabulum and the femoral head. The iliofemoral and pubofemoral ligaments cover the anterior aspect of the joint, whereas the ischiofemoral ligament is posterior; each helps to stabilize the joint by preventing excessive translation of the joint during normal ranges of motion.
The bony geometry and ligamentous support surrounding the hip determine which movements are permitted: flexion, extension, adduction, abduction, external rotation, and internal rotation (Table 1). Muscles are responsible for providing the actual movement, including the iliopsoas,42 which is responsible for hip flexion, and the gluteal muscles,2,44 which are responsible for extension (maximus), abduction (minimus and medius), internal rotation (minimus), and external rotation (maximus). Muscles of the anterior compartment of the thigh include the sartorius, tensor fascia lata, quadriceps femoris, pectineus, and iliopsoas. The medial compartment is composed of the pectineus as well as the adductor muscles (adductor longus, brevis, magnus, and gracilis). Finally, the posterior compartment contains the hamstrings (biceps femoris, semimembranosus, and semitendinosus). Another important muscle assisting in external rotation of the hip is the piriformis,15 which can often cause posterior hip pain when inflamed, owing to its proximity to the sciatic nerve.
Table 1.
Function of the major hip muscles.
| Action | Muscle |
|---|---|
| Flexion | Iliopsoas |
| Rectus femoris | |
| Pectineus | |
| Sartorius | |
| Tensor fascia lata | |
| Extension | Gluteus maximus |
| Biceps femoris | |
| Semimembranosus | |
| Semitendinosus | |
| Adduction | Adductor longus, brevis, magnus |
| Gracilis | |
| Pectineus | |
| Abduction | Gluteus medius |
| Gluteus minimus | |
| Internal rotation | Gluteus minimus |
| Tensor fascia lata | |
| External rotation | Gluteus maximus |
| Piriformis | |
| Superior gemellus | |
| Obturator internus | |
| Inferior gemellus | |
| Obturator externus | |
| Quadratus femoris |
Because the majority of the articular hip is innervated by the femoral or obturator nerves, most intra-articular pathologies radiate to the anterior or medial hip, whereas the majority of posterior hip pain is typically caused by extra-articular conditions. Some conditions may cause a more global distribution or radiate to areas outside their typical clinical presentation. Furthermore, based on Hilton’s law of joint innervation4—which describes how the nerve supplying a joint also innervates the muscles moving the joint and the skin covering the joint—it is possible and even likely that hip joint pain is often referred pain from muscles. Specifically, the hip receives innervation from branches of lumbosacral plexus (L2-S1) and predominantly from the L3 nerve root. Thus, given the distribution of the L3 dermatome, hip joint pathology usually causes anterior or medial thigh pain, whereas posterior thigh pain is rarely a sign of actual hip intra-articular pathology.34
Another important feature of hip anatomy and a common cause of hip pain are the various bursae around the hip joint—namely, the trochanteric bursa,53 the iliopsoas bursa, and the ischial tuberosity bursa. Bursae of the hip, as in any part of the body, prevent excessive friction of soft tissue over bony prominences during normal ranges of motion but can cause severe pain when inflamed. With regard to posterior hip pain, ischial bursitis should always be on the differential diagnosis when a patient complains of severe pain upon direct palpation.
History, Physical Examination, and Imaging Studies
History and Physical Examination
A thorough history and complete physical examination are crucial for accurate diagnosis and treatment of any patient complaining of posterior hip pain. Because the hip joint is close to several important structures, including organs of the reproductive and gastrointestinal tracts, any patient presenting with systemic symptoms in addition to hip pain should be immediately worked up for potential infection or cancer, as well as for inflammatory arthritis.21 Alarming symptoms include fever, malaise, night sweats, weight loss, history of drug abuse, past or present diagnosis of cancer, or being immunocompromised. In addition, if the patient reports a history of trauma, a hip fracture must be ruled out.
After determining that the patient has no systemic symptoms and no history of trauma, the physician must learn as much as possible about the injury—specifically, the location of the pain (anterior, posterior, lateral, or medial/groin) as well as the characteristics of the pain. With the onset of pain, provocative activities, age, activity level, and other medical conditions should always be considered.
After eliciting as much information as possible from the patient, the physician should complete a thorough physical examination of both hips, which should follow a typical stepwise approach, including observation, palpation, and testing for range of motion, stability, and strength in all planes. A gait assessment should be included with each examination. Specifically, the physician should note if the patient has an antalgic or Trendelenburg gait or sign, and he or she should ask the patient to transfer from standing to sitting to lying down and, finally, back to standing. The height symmetry of the iliac crests, as well as leg length, should be assessed, given that differences in leg length can often cause or contribute to lower back pain, hip pain, and sacroiliac (SI) joint pain. When palpating each muscle group, the physician should pay particular attention to the various hip bursae, which are common sources of pain when inflamed—especially the ischial bursa in the patient presenting with posterior hip pain.
Range of motion testing should be performed on both the symptomatic hip and the contralateral hip. It is helpful to begin with the contralateral hip to avoid eliciting painful symptoms at the beginning of the examination, which may lead to guarding throughout the remainder of the exam. Passive and active internal rotation, external rotation, flexion, extension, abduction, and adduction should be measured with a goniometer: Normal values for these movements are 35°, 45°, 120°, 30°, 45°, and 20°, respectively.34 The Thomas test is performed to evaluate for the presence of a hip flexion contracture. In the supine position, the patient grabs one knee with both hands and flexes it to the chest as the hip of the examined leg is allowed to completely extend. The test result is positive for a hip flexion contracture if the examined leg is unable to completely extend. To better stabilize the pelvis, this test may be performed with the hip flexed only to 90° instead of full flexion. Strength in each plane should also be tested: internal and external rotation, adduction seated or prone, abduction lying lateral with the leg abducted against the examiner’s resistance, extension while standing, and flexion in the seated and supine positions. Logrolling and impingement testing are not necessarily specific to posterior hip pathology but may be performed to rule out other potential etiologies of hip pain, including femoreacetabular impingement.
Examination should include Trendelenburg, Ober, FABER (Patrick), and Thomas tests. The Trendelenburg test assesses the gluteus medius and is performed by having the patient stand on one leg. The test is positive for gluteus medius weakness on the standing/supported leg if the pelvis on the opposite, or unsupported, leg drops or tilts. The gluteus medius on the standing leg should contract and elevate the pelvis on the opposite side.
The FABER (flexion, abduction, and external rotation) test can differentiate lumbar spine pathology from primary hip pathology. This test is performed supine with the painful leg flexed and externally rotated and with the ankle resting on the opposite knee, followed by manual pressure on the abducted knee. If the patient experiences posterior hip pain, the SI joint may be responsible. If groin pain occurs without loss of motion, the problem is most likely native to the hip (88% sensitivity in the athletic population for intra-articular pathology).36 Patients with intra-articular hip pain may report that their “hip pain” is located in the distribution known as the C-sign, in which the patient grasps the lateral aspect of the hip with his or her thumb and pointer finger to indicate that the pain is located in between.6 The posterior impingement test of the hip is performed with the buttock at the end of the examination table with both legs suspended. With the hip extended, the examiner externally rotates the hip, and the test is positive if this maneuver reproduces pain.33 A thorough lumbosacral examination—including inspection, palpation, range of motion, neurosensory assessment, and straight leg raises—should also be performed to rule out other causes or contributing factors related patient’s hip pain.
Imaging Studies
Imaging studies—including radiographs, computed tomography (CT) scanning, fluoroscopically and ultrasound guided injection, and magnetic resonance imaging (MRI) or magnetic resonance arthrography—can sometimes be helpful in evaluating posterior hip pain. The radiographic series should always include standard anterior-posterior films of the pelvis, with the coccyx 1 to 3 cm above the pubic symphysis with concentric obturator foramen. A number of lateral views of the hip have been used, including the cross-table lateral, frog-leg lateral, Dunn lateral, and false profile.52 It is important to obtain radiographs if the patient is at risk for bony pathology owing to trauma, osteoporosis, cancer, steroid, or alcohol use. Careful assessment of the posterior inferior portion of the hip joint is important because early arthritis can often be seen there, even when the superior joint space is normal. CT scan, especially with 3-dimensional reconstructions, can provide important information on the femoral version and osseous abnormalities. MRI is the study of choice in athletes; namely, it is helpful in providing information about the soft tissue structures surrounding the hip.18 Fluoroscopically guided hip injections of anesthetic medication can be useful in differentiating intra-articular from extra-articular pathology; ultrasound-guided injections to the iliopsoas and trochanteric bursae are also helpful.52 Of note, hip arthroscopy has been shown to be the final and definitive diagnostic procedure for assessing intra-articular pathology.36
Differential Diagnosis and Treatment Options
As mentioned above, posterior hip pain is the least common when compared with anterior, lateral, and medial pain.34 The structures around the hip—especially the lower back as well as the nerves coursing through the pelvis—are important when considering a patient presenting with posterior hip pain. Thus, a thorough understanding of hip anatomy is vital to appropriate diagnosis and potential treatment. In addition, fractures must be considered, especially in high-risk patients such as long-distance runners, those with osteoporosis, and those with a history of trauma or a falling episode. Table 2 describes common causes and classifications of general hip pain.
Table 2.
Differential diagnosis of hip pain.
| Classification | Potential Etiologies |
|---|---|
| Location | |
| Lateral hip pain | Greater trochanteric bursitis |
| Gluteus medius dysfunction | |
| Iliotibial band syndrome | |
| Meralgia paresthetica | |
| Anterior hip pain | Osteoarthritis |
| Hip flexor tendinopathy | |
| Iliopsoas bursitis | |
| Hip fracture | |
| Stress fracture | |
| Acetabular labral tear | |
| Avascular necrosis of humeral head | |
| Posterior hip pain | Referred from lumbar spine |
| Sacroiliac joint dysfunction | |
| Hip extensor or rotator strain | |
| Proximal hamstring rupture | |
| Piriformis syndrome | |
| Medial hip pain | Groin pain |
| Location about joint | |
| Intra-articular | Labral tears |
| Loose bodies | |
| Femoroacetabular impingement | |
| Capsular laxity | |
| Ligamentum teres rupture | |
| Chondral damage | |
| Extra-articular | Iliopsoas tendonitis |
| Iliotibial band | |
| Gluteus medius/minimus | |
| Greater trochanteric bursitis | |
| Stress fracture | |
| Abductor strain | |
| Piriformis syndrome | |
| SI joint pathology | |
| Onset | |
| Acute | Muscle strain |
| Contusion (hip pointer) | |
| Avulsions and apophyseal injuries | |
| Hip dislocation/subluxation | |
| Acetabular labral tears and loose bodies | |
| Proximal femur fractures | |
| Insidious | Sports hernias and athletic pubalgia |
| Osteitis pubis | |
| Bursitis | |
| Snapping hip syndrome | |
| Stress syndrome | |
| Osteoarthritis | |
| Systemic causes | Cancer |
| Infection | |
| Inflammatory arthritis | |
| Mimickers of hip pain | Athletic pubalgia |
| Sports hernia | |
| Osteitis pubis | |
| Referred pain | Lumbar spine |
| Degenerative disc disease | |
The most common causes of posterior hip pain include referred pain from the lumbar spine, SI joint dysfunction, hip extensor or rotator muscle pain, proximal hamstring rupture, early arthritis, and piriformis syndrome (Table 3). Table 4 describes effective therapeutic exercises for these conditions, which can typically be performed at home.
Table 3.
Differential diagnosis of posterior hip pain.
| Diagnosis | Findings |
|---|---|
| Referred pain from lumbar spine | Low back pain |
| Pain elicited with isolated lumbar, flexion/extension | |
| Radicular symptoms | |
| Sacroiliac joint dysfunction | Pelvic asymmetry on examination |
| Posterior hip or buttocks pain (especially runners) | |
| Hip extensor or rotator muscle strain | History of overuse |
| Acute injury | |
| Pain with resisted muscle testing | |
| Tenderness to palpation over gluteal muscles | |
| Proximal hamstring rupture | Posterior hip pain |
| Signs of muscle weakness and sciatica | |
| Piriformis syndrome | Pain in the sciatic nerve distribution (low back, buttock, leg) |
| Pain exacerbated by stooping or lifting | |
| Pain with straight leg raise |
Table 4.
Examples of home exercises.
| Sacroiliac joint dysfunction | |
| Knee to chest | Lie flat, bring knee to chest with hands, alternate knees. |
| → Repeat 10×, 3 sets | |
| Prone press-up | Lie prone, press up with hands while keeping pelvis on floor/table. |
| → Hold for 30 seconds, repeat 10×, 3 sets | |
| Nonweightbearing lumbar rotation | Lie flat with feet flat on table/floor, rock both knees back and forth in small movements. |
| → Perform for 30 seconds, 3 sets | |
| Extensor/rotator strain | |
| Hip abduction | Lie on side (injured leg on top, bottom knee slightly bent), lift top leg up leading with heel, hold for 5 seconds. |
| → Repeat 10×, 3 sets | |
| Hip abduction alternate | Get on hands and knees, lift knee up and out to the side from the hip, hold for 5 seconds. |
| → Repeat 10×, alternate legs, 3 sets | |
| Hip abduction with tubing | Sit, place resistance tubing around thighs above knees, spread legs against the resistance, hold for 5 seconds. |
| → Repeat 10×, 3 sets | |
| Hamstring strain/rupture | |
| Supine stretch | Lie flat, support back of knee with hand or towel, and attempt to extend knee so that plantar surface of foot faces ceiling. |
| → Hold for 20 to 30 seconds | |
| Hip extension | Lie prone, raise up leg from behind the hip while keeping knee straight, hold for 5 seconds. |
| → Repeat 10×, 3 sets | |
| Isometric strengthening | Lie supine, flex knee, and push heel into floor/table with force, hold for 5 seconds. |
| → Repeat 10×, 3 sets | |
| Hamstring curls | Lie prone, flex knee to 90°, hold for 5 seconds, slowly extend leg until flat. |
| → Repeat 10×, 3 sets | |
| Piriformis syndrome | |
| Prone hip extension | Lie prone with pillow under hips, bend knee, and contract gluteal muscles, then lift leg off surface 6 in. (15 cm) (leg on surface stays straight), hold for 5 seconds. |
| → Repeat 10×, 3 sets | |
| Resisted abduction with resistance band | Stand sideways near doorway with resistance band around ankle away from door (place other end of resistance band into doorway and close), then extend leg out to side with knee straight. |
| → Repeat 10×, 3 sets | |
| Hamstring stretch seated | Sit with heel of injured leg resting on a 15-in. (38-cm) platform with knee extended, then lean forward at hips until stretch is felt (do NOT bend at waist or shoulders). |
| → Hold for 30 seconds, repeat 3× | |
| Gluteal stretch | Lie flat with knees bent and ankle of one leg over knee of other. Then hold thigh of bottom leg and pull toward chest. |
| → Hold for 30 seconds, repeat 3× | |
Referred Pain From Lumbar Spine
The most common cause of posterior hip pain is referred pain from the lumbar spine area, the most common causes of which include herniated disks and sciatic radiculopathy. The pain is attributed to the innervation of the hip by the lumbar plexus, most notably via the L3 nerve root, as described above. Such patients typically complain of a history of low back pain that has worsened, with new onset of posterior hip and/or buttock pain. Symptoms can usually be reproduced during flexion or extension of the lumbar spine, and the patient may describe radicular symptoms traveling down the leg. Treatment for referred pain depends on the cause of the lumbar pathology, and it can range from conservative care, including therapy and activity modification, to steroid injections to surgical intervention.
SI Joint Dysfunction
SI joint dysfunction has a variety of causes—including hypermobility, hypomobility, trauma, degenerative arthritis, inflammatory arthropathy (sacroiliitis), infection, ligament strain, and/or stress fractures.50 Patients with any of these conditions can experience pain near the posterior superior iliac spine and may have buttock pain that radiates down the leg. Pathology of the SI joint can be difficult to diagnosis; thus, a thorough neurological examination is warranted to rule out other pathology, including tumors. Images—including radiographs, CT scans, and MRI scans (Figure 1)—are helpful, but fluoroscopic-guided injection into the SI joint is considered diagnostic if the patient experiences relief of pain.10 Treatment depends on the cause of the SI dysfunction, and it ranges from physical therapy (for patients with strength/flexibility deficits) to antirheumatic agents and nonsteroidal anti-inflammatory drugs for patients with inflammatory arthropathies. Surgical correction, manipulation, and radiofrequency neurotomy are controversial treatments and are considered on a case-by-case basis when more conservative therapies have failed.43
Figure 1.
Sagittal magnetic resonance imaging of the lumbosacral spine demonstrating large herniated nucleus pulposus at L5-S1 (left, T2; right, proton density fat-saturated image).
Extensor or Rotator Muscle Pain
The muscular support of the hip joint is complicated by the presence of several muscle attachments in a small, confined space, many of which have overlapping functions. Thus, when one muscle or muscle group is strained or overworked, it is common for the patient to complain of generalized hip pain, thereby making diagnosis difficult. The extensor muscles of the hip—including the biceps femoris, semimembranosus, and semitendinosus—all insert into various components of the posterior pelvis; strain or tear of any of these tendons can lead to posterior hip pain. The biceps femoris has 2 proximal attachments: the long head attaches to the ischial tuberosity and sacrotuberous ligament; the short head attaches to the lateral lip of the linea aspera and the lateral intermuscular septum. The semimembranous and semitendinosus also arise from the ischial tuberosity, and so injury to any of the hamstring tendons can lead to posterior hip pain. The rotator muscles, including internal and external rotators, have attachments on the posterior aspect of the hip; thus, strain or overuse of these muscles can lead to posterior hip pain as well. It is important to recognize gluteal tendinopathy, given that the gluteal muscles lie near the posterior hip but more often cause lateral hip pain in association with greater trochanteric pain syndrome,23,25,28,31,41 as opposed to posterior hip pain. Treatment for overuse of these muscles is typically conservative and includes activity modification, physical therapy, and nonsteroidal anti-inflammatory drugs.
Piriformis Syndrome
Piriformis syndrome is another cause of posterior hip pain, and it may account for up to 5% of all cases of low back, buttock, and leg pain.40 Patients generally complain of pain in a sciatic nerve distribution; that is, buttock pain referred down the leg. The classic features of piriformis syndrome include pain in the region of the SI joint, greater sciatic notch, and piriformis muscle and exacerbation of pain caused by stooping or lifting and, potentially, gluteal atrophy.40 Patients may complain of pain with straight leg raise. Results of the Pace test are positive if the patient has pain with resisted hip abduction in a seated position.39 The Freiberg test can be performed with forceful internal rotation of the extended hip, the result of which is positive if the pain is produced by stretching the piriformis muscle.14 Some recommend a pelvic or rectal examination, which may reveal a tender, palpable, spindle-shaped mass considered to be the intrapelvic portion of the piriformis muscle.46 Because clinical presentations can be vague and there are few validated and/or standardized diagnostic tests, patients are often diagnosed via exclusion. Electrodiagnostic testing with electromyographic and nerve conduction studies should be performed if piriformis syndrome is suspected, which may provide findings consistent with sciatic nerve compression at the level of the piriformis muscle.19 Traditional treatment includes conservative therapy with a focus on physical therapy, stretching, and steroid or analgesic37 injections. Recently, the use of botulinum toxin22,26 and arthroscopic release8 have been used as a therapy with promising results.
Proximal Hamstring Rupture
Rupture of the proximal hamstring tendons is another common cause of posterior hip pain.7,20,38 Injury can occur following a one-time traumatic rupture, or it can occur over time after several episodes of hamstring strain and tendonitis. Patients with rupture present with posterior hip pain and often have signs of muscle weakness and sciatica.23,25,28,31,41 In the past, treatment consisted of conservative therapies; however, recent research has shown that early operative intervention,5,30 compared with conservative therapy or late surgical intervention,47 yields substantially better results. In addition, some studies have shown that surgical repair with allograft tendons can be successful in acute and chronic cases (Figures 2-4).13,27
Figure 2.

Physical examination demonstrating ecchymosis after a torn hamstring.
Figure 4.
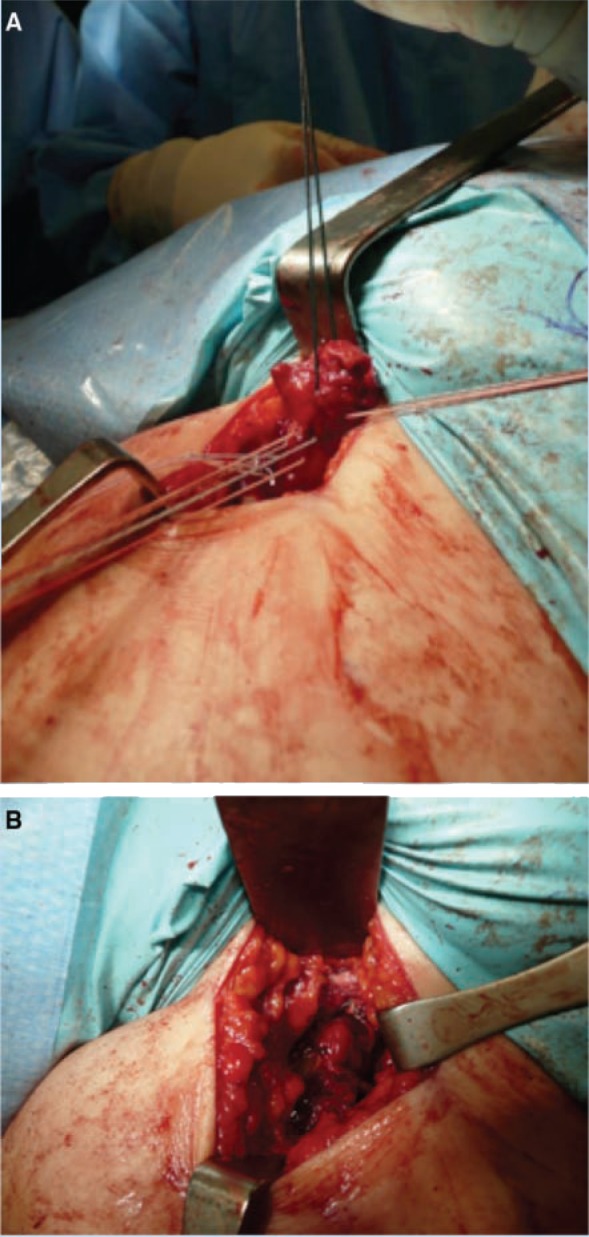
Intraoperative images of proximal hamstring repair. A, proximal end of the hamstring tendon tagged with numerous sutures. B, repair of proximal hamstring with suture anchors to the ischium.
Figure 3.
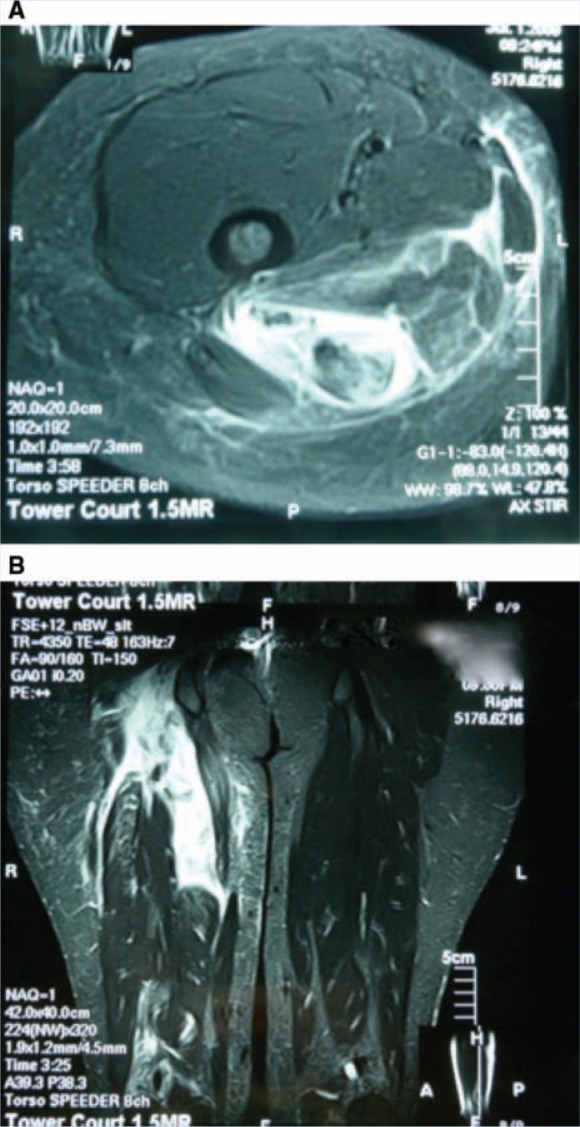
T2 magnetic resonance images of acutely torn hamstring tendons: A, axial cuts demonstrating torn hamstring tendon with fluid around the proximal end; B, coronal image with 3 hamstring tendons torn with retraction and hematoma formation.
Femoroacetabular Impingement
Although the typical presentation of femoroacetabular impingement (FAI) occurs in the groin area, there are cases that present globally or focally (ie, on the posterior aspect of the hip). FAI occurs as a result of structural abnormalities that cause chondral and labral injury with repetitive hip motion. A number of osseous abnormalities of the acetabulum and/or femoral head may lead to hip impingement, including CAM impingement, Pincer impingement from focal acetabular overcoverage (acetabular retroversion) or global acetabular overcoverage (coxa profunda or protrusion acetabuli) (Figure 5). If an athlete has repetitive groin strains with loss of range of motion that is refractory to physical therapy and so results in loss of participation, the next step is referral to a hip specialist and radiographic evaluation. As previously mentioned, such patients typically have groin pain, worse with prolonged sitting or rotational maneuvers. The physical examination demonstrates limitations, with hip flexion, internal rotation, and external rotation being involved in some cases. Less than 20° of internal rotation is abnormal, and the clinician should be suspicious of FAI. An impingement sign is positive if the patient has groin pain with flexion, adduction, and internal rotation. The posterior impingement test is performed with the hip in extension and external rotation, and the result is considered positive if the test produces pain in the posterior aspect of the hip. Patients with global acetabular overcoverage may have a positive posterior impingement sign. Fluoroscopic injection of the hip joint with lidocaine is the next step. A positive response to the injection, with hip motion or activity that elicits the pain, is considered to be diagnostic for an intra-articular cause of hip pain. Advanced imaging studies with MRI or CT scans are appropriate to further delineate the hip morphology and injury to the articular cartilage and labrum. If the patients have symptoms that are refractory to nonsurgical management, hip surgery to correct bony deformities can be performed through an open approach or hip arthroscopy.
Figure 5.

Bilateral global acetabular overcoverage secondary to acetabular protrusio. Radiographs demonstrate that the acetabular line (arrow) is medial to the ilioischial line. A crossover sign is also evident, with the anterior wall (dashed line) being more lateral than the posterior wall (solid line).
Clinical Workup
A systematic approach34 to address posterior hip pain should be used in an attempt to diagnosis the cause of pain and select the appropriate treatment strategy. If the patient describes an acute onset of pain and has a history of low back pain or radiating symptoms, the physician should perform imaging studies of the lumbar spine. In these cases, the most likely cause of pain is herniated nucleus pulposus, lumbar degenerative disc disease, arthropathy, or spinal stenosis, and the appropriate treatment typically begins with conservative measures. If the patient describes a more gradual onset of injury, as in the case of overuse or sports-related pain, the physical exam can be helpful in narrowing the possible causes. Specifically, if the patient has a positive result for the FABER test or has pelvic asymmetry, SI joint dysfunction can be considered, with appropriate therapy including physical therapy, modification of activity, and selective injections. For patients who do not experience relief of symptoms, the physician should perform an MRI or bone scan of the pelvis to rule out a stress reaction within the pelvis. If the patient instead has pain with resisted extensor or rotator muscle testing and/or gluteal muscle tenderness to palpation, the likely diagnosis is muscle strain. The appropriate treatment in this case is activity modification, physical therapy, and nonsteroidal anti-inflammatory drugs. Athletes with persistent groin strain with limitations in range of motion may have FAI and so require evaluation by a hip specialist for possible radiographic evaluation and injections. Those who do not improve with activity modification and therapy may be indicated for either open or arthroscopic hip surgery. In addition, patients with proximal hamstring avulsion should immediately be referred to an orthopaedic surgeon for possible repair of hamstring tendon.
Conclusions
Posterior hip pain is the least common complaint among patients with hip pain. To make proper treatment decisions, physicians must use a logical and systemic approach to assess patients presenting with posterior hip pain. Common causes of posterior hip pain include referred pain from the lumbar spine, SI joint dysfunction, hip extensor or rotator muscle strain, proximal hamstring rupture, and piriformis syndrome.
One or more authors has indicated a potential conflict of interest: Shane J. Nho and Charles A Bush-Joseph have received research and institutional support from Arthrex, Smith & Nephew, Livatec, Miomed, Athletico, and DJ Ortho.
References
- 1. Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med. 2001;29(4):521-533 [DOI] [PubMed] [Google Scholar]
- 2. Beck M, Sledge JB, Gautier E, Dora CF, Ganz R. The anatomy and function of the gluteus minimus muscle. J Bone Joint Surg Br. 2000;82(3):358-363 [DOI] [PubMed] [Google Scholar]
- 3. Blankenbaker DG, Ullrick SR, Davis KW, De Smet AA, Haaland B, Fine JP. Correlation of MRI findings with clinical findings of trochanteric pain syndrome. Skeletal Radiol. 2008;37(10):903-909 [DOI] [PubMed] [Google Scholar]
- 4. Brand R. John Hilton, 1805-1878. Clin Orthop Relat Res. 2009;467:2208-2209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brucker PU, Imhoff AB. Functional assessment after acute and chronic complete ruptures of the proximal hamstring tendons. Knee Surg Sports Traumatol Arthrosc. 2005;13(5):411-418 [DOI] [PubMed] [Google Scholar]
- 6. Byrd JW, Jones KS. Diagnostic accuracy of clinical assessment, magnetic resonance imaging, magnetic resonance arthrography, and intra-articular injection in hip arthroscopy patients. Am J Sports Med. 2004;32(7):1668-1674 [DOI] [PubMed] [Google Scholar]
- 7. Cohen S, Bradley J. Acute proximal hamstring rupture. J Am Acad Orthop Surg. 2007;15(6):350-355 [DOI] [PubMed] [Google Scholar]
- 8. Dezawa A, Kusano S, Miki H. Arthroscopic release of the piriformis muscle under local anesthesia for piriformis syndrome. Arthroscopy. 2003;19(5):554-557 [DOI] [PubMed] [Google Scholar]
- 9. Dines JS, Strauss EJ, Fealy S, Craig EV. Arthroscopic-assisted core decompression of the humeral head. Arthroscopy. 2007;23(1):103, e101-e104 [DOI] [PubMed] [Google Scholar]
- 10. Dreyfuss P, Dreyer SJ, Cole A, Mayo K. Sacroiliac joint pain. J Am Acad Orthop Surg. 2004;12(4):255-265 [DOI] [PubMed] [Google Scholar]
- 11. Dwek J, Pfirrmann C, Stanley A, Pathria M, Chung CB. MR imaging of the hip abductors: normal anatomy and commonly encountered pathology at the greater trochanter. Magn Reson Imaging Clin N Am. 2005;13(4):691-704 [DOI] [PubMed] [Google Scholar]
- 12. Farr D, Selesnick H, Janecki C, Cordas D. Arthroscopic bursectomy with concomitant iliotibial band release for the treatment of recalcitrant trochanteric bursitis. Arthroscopy. 2007;23(8):901-905 [DOI] [PubMed] [Google Scholar]
- 13. Folsom GJ, Larson CM. Surgical treatment of acute versus chronic complete proximal hamstring ruptures: results of a new allograft technique for chronic reconstructions. Am J Sports Med. 2008;36(1):104-109 [DOI] [PubMed] [Google Scholar]
- 14. Freiberg A, Vinke T. Sciatica and the sacroiliac joint. J Bone Joint Surg Am. 1934;16:126-136 [Google Scholar]
- 15. Guvencer M, Akyer P, Iyem C, Tetik S, Naderi S. Anatomic considerations and the relationship between the piriformis muscle and the sciatic nerve. Surg Radiol Anat. 2008;30(6):467-474 [DOI] [PubMed] [Google Scholar]
- 16. Hase T, Ueo T. Acetabular labral tear: arthroscopic diagnosis and treatment. Arthroscopy. 1999;15(2):138-141 [DOI] [PubMed] [Google Scholar]
- 17. Hewitt JD, Glisson RR, Guilak F, Vail TP. The mechanical properties of the human hip capsule ligaments. J Arthroplasty. 2002;17(1):82-89 [DOI] [PubMed] [Google Scholar]
- 18. Hong RJ, Hughes TH, Gentili A, Chung CB. Magnetic resonance imaging of the hip. J Magn Reson Imaging. 2008;27(3):435-445 [DOI] [PubMed] [Google Scholar]
- 19. Hughes SS, Goldstein MN, Hicks DG, Pellegrini VD., Jr Extrapelvic compression of the sciatic nerve: an unusual cause of pain about the hip: report of five cases. J Bone Joint Surg Am. 1992;74(10):1553-1559 [PubMed] [Google Scholar]
- 20. Ishikawa K, Kai K, Mizuta H. Avulsion of the hamstring muscles from the ischial tuberosity: a report of two cases. Clin Orthop Relat Res. 1988;232:153-155 [PubMed] [Google Scholar]
- 21. Jennings F, Lambert E, Fredericson M. Rheumatic diseases presenting as sports-related injuries. Sports Med. 2008;38(11):917-930 [DOI] [PubMed] [Google Scholar]
- 22. Jeynes LC, Gauci CA. Evidence for the use of botulinum toxin in the chronic pain setting: a review of the literature. Pain Pract. 2008;8(4):269-276 [DOI] [PubMed] [Google Scholar]
- 23. Kandemir U, Bharam S, Philippon MJ, Fu FH. Endoscopic treatment of calcific tendinitis of gluteus medius and minimus. Arthroscopy. 2003;19(1):E4. [DOI] [PubMed] [Google Scholar]
- 24. Kelly BT, Williams RJ, III, Philippon MJ. Hip arthroscopy: current indications, treatment options, and management issues. Am J Sports Med. 2003;31(6):1020-1037 [DOI] [PubMed] [Google Scholar]
- 25. Kingzett-Taylor A, Tirman PF, Feller J, et al. Tendinosis and tears of gluteus medius and minimus muscles as a cause of hip pain: MR imaging findings. AJR Am J Roentgenol. 1999;173(4):1123-1126 [DOI] [PubMed] [Google Scholar]
- 26. Kirschner JS, Foye PM, Cole JL. Piriformis syndrome, diagnosis and treatment. Muscle Nerve. 2009;40(1):10-18 [DOI] [PubMed] [Google Scholar]
- 27. Klingele KE, Sallay PI. Surgical repair of complete proximal hamstring tendon rupture. Am J Sports Med. 2002;30(5):742-747 [DOI] [PubMed] [Google Scholar]
- 28. LaBan MM, Weir SK, Taylor RS. “Bald trochanter” spontaneous rupture of the conjoined tendons of the gluteus medius and minimus presenting as a trochanteric bursitis. Am J Phys Med Rehabil. 2004;83(10):806-809 [DOI] [PubMed] [Google Scholar]
- 29. Larson CM, Guanche CA, Kelly BT, Clohisy JC, Ranawat AS. Advanced techniques in hip arthroscopy. Instr Course Lect. 2009;58:423-436 [PubMed] [Google Scholar]
- 30. Lempainen L, Sarimo J, Orava S. Recurrent and chronic complete ruptures of the proximal origin of the hamstring muscles repaired with fascia lata autograft augmentation. Arthroscopy. 2007;23(4):441-445 [DOI] [PubMed] [Google Scholar]
- 31. Lequesne M. From “periarthritis” to hip “rotator cuff” tears: trochanteric tendinobursitis. Joint Bone Spine. 2006;73(4):344-348 [DOI] [PubMed] [Google Scholar]
- 32. Lequesne M, Djian P, Vuillemin V, Mathieu P. Prospective study of refractory greater trochanter pain syndrome: MRI findings of gluteal tendon tears seen at surgery. Clinical and MRI results of tendon repair. Joint Bone Spine. 2008;75(4):458-464 [DOI] [PubMed] [Google Scholar]
- 33. Leunig M, Beaule PE, Ganz R. The concept of femoroacetabular impingement: current status and future perspectives. Clin Orthop Relat Res. 2009;467(3):616-622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Margo K, Drezner J, Motzkin D. Evaluation and management of hip pain: an algorithmic approach. J Fam Pract. 2003;52(8):607-617 [PubMed] [Google Scholar]
- 35. McCarthy JC, Lee J. Hip arthroscopy: indications and technical pearls. Clin Orthop Relat Res. 2005;441:180-187 [DOI] [PubMed] [Google Scholar]
- 36. Mitchell B, McCrory P, Brukner P, O’Donnell J, Colson E, Howells R. Hip joint pathology: clinical presentation and correlation between magnetic resonance arthrography, ultrasound, and arthroscopic findings in 25 consecutive cases. Clin J Sport Med. 2003;13(3):152-156 [DOI] [PubMed] [Google Scholar]
- 37. Naja Z, Al-Tannir M, El-Rajab M, et al. The effectiveness of clonidine-bupivacaine repeated nerve stimulator-guided injection in piriformis syndrome. Clin J Pain. 2009;25(3):199-205 [DOI] [PubMed] [Google Scholar]
- 38. Orava S, Kujala UM. Rupture of the ischial origin of the hamstring muscles. Am J Sports Med. 1995;23(6):702-705 [DOI] [PubMed] [Google Scholar]
- 39. Pace JB, Nagle D. Piriform syndrome. West J Med. 1976;124(6):435-439 [PMC free article] [PubMed] [Google Scholar]
- 40. Papadopoulos EC, Khan SN. Piriformis syndrome and low back pain: a new classification and review of the literature. Orthop Clin North Am. 2004;35(1):65-71 [DOI] [PubMed] [Google Scholar]
- 41. Pfirrmann CW, Chung CB, Theumann NH, Trudell DJ, Resnick D. Greater trochanter of the hip: attachment of the abductor mechanism and a complex of three bursae—MR imaging and MR bursography in cadavers and MR imaging in asymptomatic volunteers. Radiology. 2001;221(2):469-477 [DOI] [PubMed] [Google Scholar]
- 42. Polster JM, Elgabaly M, Lee H, Klika A, Drake R, Barsoum W. MRI and gross anatomy of the iliopsoas tendon complex. Skeletal Radiol. 2008;37(1):55-58 [DOI] [PubMed] [Google Scholar]
- 43. Ripani M, Continenza MA, Cacchio A, Barile A, Parisi A, De Paulis F. The ischiatic region: normal and MRI anatomy. J Sports Med Phys Fitness. 2006;46(3):468-475 [PubMed] [Google Scholar]
- 44. Robertson WJ, Gardner MJ, Barker JU, Boraiah S, Lorich DG, Kelly BT. Anatomy and dimensions of the gluteus medius tendon insertion. Arthroscopy. 2008;24(2):130-136 [DOI] [PubMed] [Google Scholar]
- 45. Robertson WJ, Kelly BT. The safe zone for hip arthroscopy: a cadaveric assessment of central, peripheral, and lateral compartment portal placement. Arthroscopy. 2008;24(9):1019-1026 [DOI] [PubMed] [Google Scholar]
- 46. Robinson D. Piriformis syndrome in relation to sciatic pain. Am J Surg. 1947;73:335-338 [DOI] [PubMed] [Google Scholar]
- 47. Sarimo J, Lempainen L, Mattila K, Orava S. Complete proximal hamstring avulsions: a series of 41 patients with operative treatment. Am J Sports Med. 2008;36(6):1110-1115 [DOI] [PubMed] [Google Scholar]
- 48. Seldes RM, Tan V, Hunt J, Katz M, Winiarsky R, Fitzgerald RH., Jr Anatomy, histologic features, and vascularity of the adult acetabular labrum. Clin Orthop Relat Res. 2001;382:232-240 [DOI] [PubMed] [Google Scholar]
- 49. Shindle MK, Voos JE, Nho SJ, Heyworth BE, Kelly BT. Arthroscopic management of labral tears in the hip. J Bone Joint Surg Am. 2008; 90(suppl 4):2-19 [DOI] [PubMed] [Google Scholar]
- 50. Tibor LM, Sekiya JK. Differential diagnosis of pain around the hip joint. Arthroscopy. 2008;24(12):1407-1421 [DOI] [PubMed] [Google Scholar]
- 51. van Mechelen W. Running injuries: a review of the epidemiological literature. Sports Med. 1992;14(5):320-335 [DOI] [PubMed] [Google Scholar]
- 52. Voos JE, Rudzki JR, Shindle MK, Martin H, Kelly BT. Arthroscopic anatomy and surgical techniques for peritrochanteric space disorders in the hip. Arthroscopy. 2007;23(11):1246, e1241-e1245 [DOI] [PubMed] [Google Scholar]
- 53. Woodley SJ, Mercer SR, Nicholson HD. Morphology of the bursae associated with the greater trochanter of the femur. J Bone Joint Surg Am. 2008;90(2):284-294 [DOI] [PubMed] [Google Scholar]
- 54. Woodley SJ, Nicholson HD, Livingstone V, et al. Lateral hip pain: findings from magnetic resonance imaging and clinical examination. J Orthop Sports Phys Ther. 2008;38(6):313-328 [DOI] [PubMed] [Google Scholar]
- 55. Yamamoto Y, Usui I. Arthroscopic surgery for degenerative rupture of the ligamentum teres femoris. Arthroscopy. 2006;22(6):689, e681-e683 [DOI] [PubMed] [Google Scholar]



