Abstract
Apophyseal avulsion injuries of the hip and pelvis are frequent athletic injuries in children and adolescents, most commonly associated with explosive movement or sprinting. This article details typically encountered apophyseal injuries and their appearance on magnetic resonance imaging.
Keywords: apophyseal avulsion, hip and pelvis, magnetic resonance imaging, adolescent
A 15-year-old male soccer player presents with left hip pain and weakness for 4 weeks without a known injury. He has severe pain over the left anterior superior iliac spine (ASIS) after activity. A frontal radiograph of the left hip (Figure 1) and a fat-suppressed T2-weighted axial image of the upper pelvis (Figure 2) illustrate relevant findings (marked with arrows). What are the findings? What is the diagnosis?
Figure 1.

A frontal radiograph of the left hip shows subtle cortical irregularity of the anterior superior iliac spine (arrow).
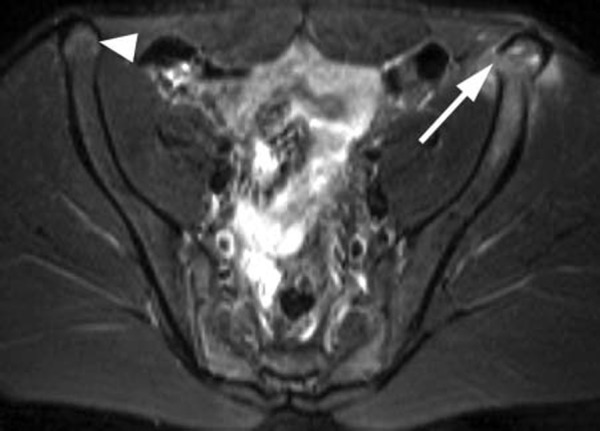
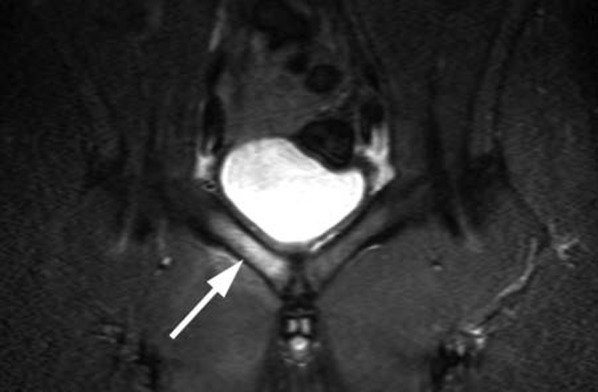
Figure 2.
A mildly displaced fracture (arrow) is seen through the physis of the left anterior superior iliac spine. The edema in the fractured apophysis, iliac wing, and adjacent soft tissues is relatively mild, which is indicative of a subacute injury. Hyperintense signal in the contralateral anterior superior iliac spine (arrowhead) represents growth cartilage in this skeletally immature individual.
Findings
In Figure 1, the frontal radiograph of the left hip demonstrates subtle cortical irregularity in the region of the ASIS. In Figure 2 (the fat-suppressed T2-weighted axial image), an increased signal is present in the left ASIS and the surrounding soft tissues. The apophysis of the ASIS is slightly displaced and laterally angulated with interruption of the physis.
Diagnosis
Apophyseal avulsion injury of the left ASIS.
Discussion
Apophyseal avulsion injuries of the hip and pelvis account for 10% to 24% of athletic injuries in children.2 The most commonly implicated activities are soccer, running, and ballet.2 Similar injuries also occur in football, baseball, track, gymnastics, and cheerleading.4,10,12 When a strain-type injury occurs, it is the patient’s age that tends to determine where the disruption occurs in the chain of bone, tendon, and muscle. In a young adult, the failure usually involves the myotendinous junction. In an older adult, the failure tends to target the tendon, which is often weakened by tendinosis. The weak link in children and adolescents is the physis, especially at times of growth acceleration.3,9
In a study of 203 avulsion fractures seen on radiographs,10 the most commonly affected apophyses were as follows: the ischial tuberosity (the origin of the hamstrings), the anterior inferior iliac spine (AIIS) (the origin of the straight head of the rectus femoris), the ASIS (the origin of the sartorius and some fibers of the tensor fascia lata), and the pubic symphysis (the origin of the adductor brevis, adductor longus, and the gracilis).
The mechanism of injury in apophyseal avulsions is sudden forceful concentric or eccentric muscle contraction during running, jumping, or kicking, which results in traction on the unfused apophysis. Extreme passive stretching and chronic repetitive microtrauma have also been implicated in the development of apophyseal avulsions. With an acute apophyseal avulsion injury, the patient often experiences a “pop” and immediate pain following concentric or eccentric muscle contraction. Echymosis, swelling, weakness, and an altered gait ensue. In the subacute or chronic setting, especially when no clear history of trauma is provided, the initial working diagnosis is often neoplasm or infection.
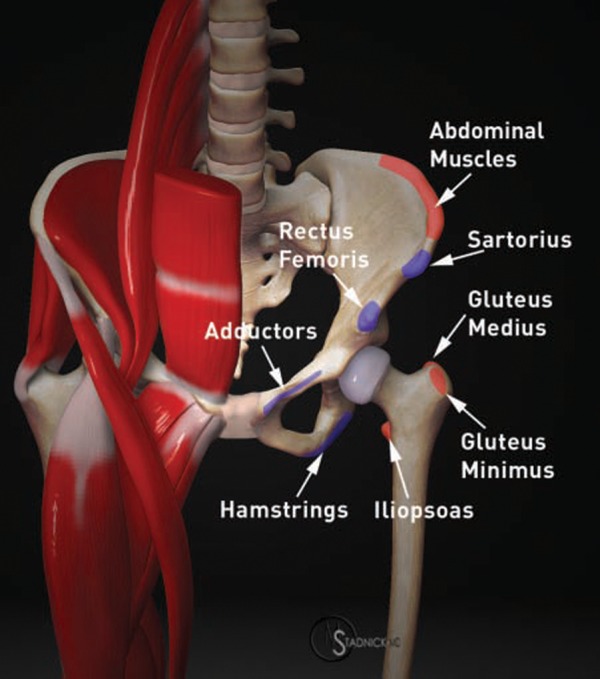
When an apophyseal avulsion is nondisplaced or when the apophysis is not yet ossified, radiographic findings may be interpreted as negative. In cases of excessive callus, the radiographic appearance may mimic an osteosarcoma, an osteochondroma, or an infectious process.11 Knowledge of the tendon attachments to the pelvis is essential in arriving at the correct diagnosis (Figure 3). Magnetic resonance imaging (MRI) of apophyseal avulsions allows direct visualization of the tendon attached to the avulsed apophysis. The involved tendon may have a lax configuration owing to retraction. Variable degrees of edema in the bone and surrounding fat and muscle are present on water-sensitive images. Avulsed cortical bone is hypointense and may be indistinguishable from adjacent tendons or ligaments. Compared to MRI, computed tomography provides better delineation of bone detail from an avulsed apophysis and should be considered when the diagnosis is in doubt and when surgery is contemplated.
Figure 3.
A 3-dimensional model of the pelvis illustrates the most common sites of apophyseal avulsion injury in adolescents, depicted in blue. Less common sites of apophyseal avulsion are indicated in red.
Anterior Superior Iliac Spine
The ASIS apophysis begins to ossify between the ages of 13 and 15 years and fuses with the ilium between the ages of 21 and 25 years. The ASIS is the attachment site for the sartorius and some fibers of the tensor fascia lata. Avulsion of the ASIS occurs from a strong sudden pull of the sartorius with the hip in extension and the knee in flexion, most commonly in kicking athletes and sprinters (Figures 1 and 2). These injuries typically heal quickly with simple restriction of activity.
Ischial Apophysis
The ischial apophysis starts to ossify between the ages of 14 and 16 years and usually fuses with the ischium between the ages of 18 and 21 years. The hamstring muscle group (semimembranosus, semitendinosus, and biceps femoris) originates from the ischial tuberosity. Injury mechanisms include a sudden contraction of the hamstrings muscles with the knee extended and the hip flexed, and they are commonly seen in sports that require rapid acceleration while running, such as football, track, and soccer (Figures 4 and 5). Avulsions of bone or tendon can also be the result of severe stretching of the hamstrings, which occurs when the hip undergoes a forceful flexion with the knee in extension. Waterskiing and ice skating are examples of the types of sports that can lead to this injury.1 Because of the proximity of the sciatic nerve, acute injuries may present with temporary sciatica or even a sciatic neuropathy. Sciatic neuropathy may also occur in chronic cases owing to excessive callus or displaced bone (Figure 6).
Figure 4.

A coronal T1-weighted image through the posterior pelvis demonstrates a zone of intermediate signal (arrows) along the inferolateral aspect of the left ischial tuberosity in this 15-year-old football player complaining of left buttock pain.
Figure 5.
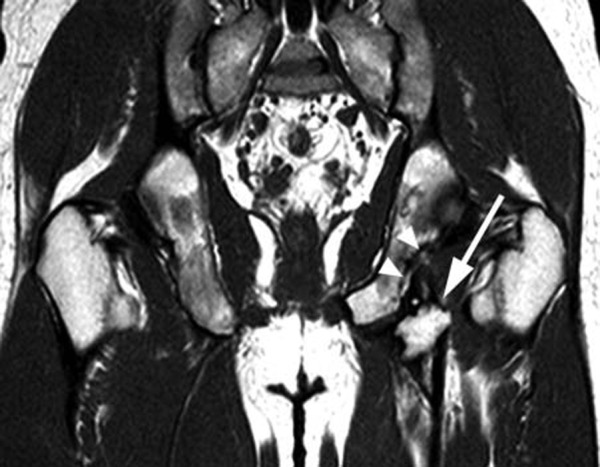
The corresponding coronal T2-weighted fat-suppressed image clearly depicts a fracture line (arrows) through the ischial tuberosity apophysis. An adjacent fluid collection most likely represents a distended bursa (arrowhead).
Figure 6.
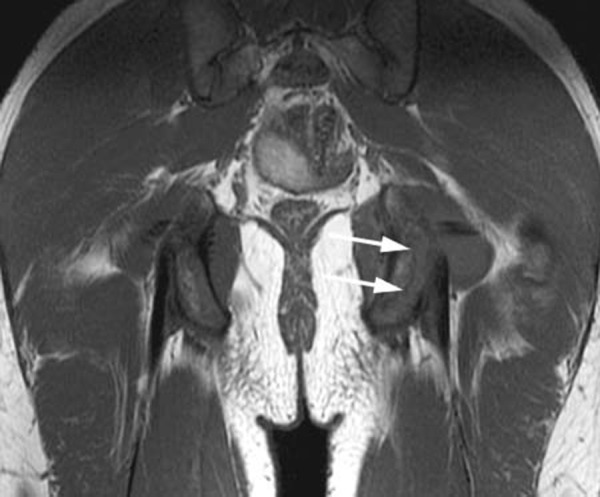
A coronal T1-weighted image of the pelvis demonstrates a displaced bony fragment (arrow) just distal to the left ischial tuberosity and a chronic-appearing defect of the ischium (arrowheads).
Anterior Inferior Iliac Spine
The apophysis of the AIIS starts to ossify between the ages of 13 to 14 years, and it fuses with the ilium between the ages of 16 and 18 years. The direct head of the rectus femoris tendon originates at the AIIS. Slightly more distal, the indirect head arises from the acetabular rim, closely approximated to the hip capsule. The rectus femoris muscle assists in extending the knee and generating hip flexion. Injury of the direct head is more common and typically occurs in early hip flexion, when tension at the direct head is maximal. With greater degrees of flexion, the indirect head becomes taut and is more susceptible to injury. AIIS avulsions are common in runners and are known as sprinter’s fractures (Figures 7 and 8).
Figure 7.

A 14-year-old male with avulsion of the left anterior inferior iliac spine. A T2-weighted coronal image reveals the avulsion of the apophysis at the direct head of the rectus femoris (arrow) with associated marrow and soft tissue edema (arrowheads). Note the normal anterior inferior iliac spine and rectus femoris tendon on the right (short arrow).
Figure 8.

A sagittal fat-suppressed proton density–weighted image of the left hip (the same patient as Figure 7) depicts the avulsion injury involving both the direct (arrow) and the indirect (arrowhead) heads of the rectus femoris.
Iliac Crest Apophysis
Iliac crest apophyseal avulsion injuries are relatively rare and occur with pulling of 1 or more of the muscles that have their attachment to the iliac crest (the external and internal abdominal oblique muscles, transverse abdominis muscle, gluteus medius muscle, and tensor fascia latae) (Figures 9 and 10). Ossification of the iliac crest apophysis starts along the anterolateral aspect of the iliac crest between the ages of 13 and 15 years and continues posteromedially. The fusion of the ossified apophysis usually starts at the age of 15 years and continues to the age of 25 years.
Figure 9.

A 15-year-old girl with bilateral iliac crest avulsion on a coronal STIR image. Marrow edema and cortical irregularity (arrows) are evident at both iliac crests.
Figure 10.

Iliac crest apophyseal avulsion on the left (arrow), as shown on a plain radiograph (not the patient in Figure 9). Bone resorption is present in the adjacent anterior superior iliac spine (arrowhead), consistent with an additional anterior superior iliac spine avulsion. In a minority of cases, avulsion injuries are multiple at the time of presentation.
Adductor Avulsion
Adductor avulsion injuries are part of a complex of injuries involving the symphysis pubis, the surrounding musculature, and ligamentous structures. These injuries are insidious upon onset and result from repetitive microtrauma, but they may also occur from a single acute event. The adductor longus tendon arises just lateral to the symphysis pubis. Superficial fibers from the adductor longus blend with the superficial fibers of the rectus abdominis, which attach at the superior aspect of the pubic symphysis. Additionally, medial fibers of the adductor longus and brevis blend with the capsule of the symphysis pubis. Athletic injuries to this complex are varied and include traumatic injury to the adductor and rectus abdominis muscles, osteitis pubis, insufficiency fractures of the pelvis, posterior inguinal wall deficiency, and hernias.6 Injuries of the adductor longus muscle and tendon are most common.4 On MRI, subjacent stress-related marrow changes within the pubis and superior pubic ramus are typical (Figure 11). Fluid may be seen at the bone-tendon interface indicating the site of avulsion, and retraction of the tendon may occur resulting in a fluid-filled gap (Figure 12).
Figure 11.
A STIR coronal image of the symphysis pubis in a 16-year-old male soccer player who was initially thought to have osteomyelitis. Diffuse signal abnormality in the right superior pubic ramus (arrow) is present.
Figure 12.

Inferior contour irregularity and marrow signal abnormality are demonstrated (in the same patient as Figure 11) in the right parasymphyseal region (arrow) at the origin of the adductor longus, consistent with an avulsion injury.
Imaging
Plain films can demonstrate avulsion injuries to ossified apophyses. When the apophysis is incompletely ossified or nonossified, findings from plain films are often inconclusive, and advanced imaging strategies are necessary to confirm the presence of an avulsion. MRI is the modality of choice in such situations. Fluid-sensitive sequences, such as fat-suppressed T2-weighted and STIR (short-tau inversion recovery) sequences, are ideal for imaging acute to subacute injuries by demonstrating displaced apophyses surrounded by hemorrhage and edema. Associated osseous or musculotendinous injuries are also well seen. T1-weighted sequences provide anatomical detail and often prove more useful in chronic injuries by demonstrating displaced tendon or osseous fragments. A typical MRI protocol consists of axial fat-suppressed T2-weighted or STIR series, coronal T1-weighted and fat-suppressed T2-weighted or STIR series, and a sagittal T2-weighted series.
Treatment and Prognosis
Nondisplaced apophyseal avulsions of the pelvis are usually treated with nonsteroidal anti-inflammatory agents, activity modification, and rehabilitation.5 After resolution of clinical symptoms, which usually takes 4 to 6 weeks, the patient can gradually return to athletic activity. Surgery is considered for recent apophyseal avulsion fractures displaced more than 2 cm. In cases of malunited or hypertrophied fragments, surgery may also be beneficial.7 Permanent disability and limitation of sporting activity have been reported.8
Conclusion
Apophyseal avulsion injuries of the pelvis have occurred with increasing frequency over the past several decades because of the increased participation of children and adolescents in competitive athletic activities. The most commonly avulsed apophysis is the ischial tuberosity, followed by the AIIS and the ASIS. Radiographic findings may be interpreted as negative when an apophyseal avulsion is nondisplaced or when the apophysis is unossified. Alternatively, exuberant callus formation may mimic neoplasm or osteomyelitis, confusing the clinical picture. Knowledge of anatomy allows the experienced interpreter of MRI to correctly identify the characteristic appearance and location of apophyseal avulsion injuries. MRI allows evaluation of the extent of injury and osseous displacement (important factors in treatment decisions), and associated muscle and tendon strain injuries are well demonstrated.
Footnotes
No potential conflict of interest declared.
References
- 1. Bencardino JT, Mellado JM. Hamstring injuries of the hip. Magn Reson Imaging Clin N Am. 2005;13:677-690 [DOI] [PubMed] [Google Scholar]
- 2. Boyd KT, Peirce NS, Batt ME. Common hip injuries in sports. Sports Med. 1997;24(4):273-288 [DOI] [PubMed] [Google Scholar]
- 3. Combs J. Hip and pelvis avulsion injuries in adolescents. Phys Sportsmed. 1994;22:41-49 [DOI] [PubMed] [Google Scholar]
- 4. Cunningham PM, Brennan D, O’Connell M, MacMahon P, O’Neill P, Eustace S. Patterns of bone and soft-tissue injury at the symphysis pubis in soccer players: observations at MRI. AJR Am J Roentgenol. 2007;188:W291-W296 [DOI] [PubMed] [Google Scholar]
- 5. Diehl JJ, Best TM, Kaeding CC. Classification and return-to-play considerations for stress fractures. Clin Sports Med. 2006;25:17-28 [DOI] [PubMed] [Google Scholar]
- 6. Koulouris G. Imaging review of groin pain in elite athletes: an anatomic approach to imaging findings. AJR Am J Roentgenol. 2008;191:962-972 [DOI] [PubMed] [Google Scholar]
- 7. Kujala UM, Orava S. Ischial apophysis injuries in athletes. Sports Med. 1993;16(4):290-294 [DOI] [PubMed] [Google Scholar]
- 8. Manthravadi S, Carty H. Avulsion fracture of the pelvis in children: a report of 32 fractures and their outcome. Skeletal Radiol. 1994;23(2):85-90 [DOI] [PubMed] [Google Scholar]
- 9. Micheli LJ, Fehlandt AF., Jr Overuse injuries to tendons and apophyses in children and adolescents. Clin Sports Med. 1992;11:713-726 [PubMed] [Google Scholar]
- 10. Rossi F, Dragoni S. Acute avulsion fractures of the pelvis in adolescent competitive athletes: prevalence, location and sports distribution of 203 cases collected. Skeletal Radiol. 2001;30(3):127-131 [DOI] [PubMed] [Google Scholar]
- 11. Stevens MA, El-Khoury GY, Kathol MH, et al. Imaging features of avulsion injuries. Radiographics. 1999;19(3):655-672 [DOI] [PubMed] [Google Scholar]
- 12. Tehranzadeh J. The spectrum of avulsion and avulsion-like injuries of the musculoskeletal system. Radiographics. 1987;7(5):945-974 [DOI] [PubMed] [Google Scholar]


