Abstract
Context:
Whereas the majority of sports concussions are isolated self-limited events, some patients have more complicated presentations and management needs. This review presents a framework for the management of these complicated concussion patients.
Evidence Acquisition:
A MEDLINE search for the years 1990 to 2009 was performed using the search terms concussion and athletic injuries. Secondary search terms included symptom, incidence, treatment, and risk factor. The Strength of Recommendation Taxonomy grading system was used for all clinical recommendations.
Results:
Patterns of complicated sports concussion presentations were identified from literature review, anecdote, and personal experience of the author and colleagues. All clinical recommendations carry a grade of C, unless otherwise noted.
Conclusion:
The sports medicine provider should be aware of certain patterns of complicated sports concussion presentations in order to use a patient-focused approach to management.
Keywords: concussion, management, return-to-play, complicated
Sports concussion is a common injury, with between 1.6 and 3.8 million such injuries occurring each year in the United States alone.13 At the high school level, concussion composes almost 9% of all athletic injuries.8 The majority of these injuries (80% to 90%) are short-lived, with symptoms abating after 7 to 10 days.18 The management of most concussions as individual injuries can be straightforward when one applies the established paradigm of physical and cognitive rest until asymptomatic and a gradual, stepwise return to activity, culminating in a return to participation without restrictions.12 Considered in a larger context, however, each concussive injury is only one piece of the more complicated clinical landscape for each athlete. The frequency of concussions, prolonged symptom courses, and possible long-term cognitive and personality sequelae are just some of the clinical factors that can effect management.
Despite the best efforts of clinicians and researchers the world over, relatively little has been established regarding the pathophysiology, risk factors, and long-term sequelae of concussion. Efforts have focused on attempting to create a clinically relevant classification system for concussion.1,3,5 No one system has garnered long-term acceptance. When applied in the clinical arena, the value of classifying concussion, especially at the time of presentation, has not been realized.14-16 The latest international effort at a consensus concluded that even dividing concussion into “simple” and “complex” entities is not clinically useful.18
Beyond the classification of individual concussive injuries, a more useful framework may exist at the patient level. Although it has proven difficult to classify concussion types, it is clear to sports medicine providers that certain concussed athletes are more complicated than others.
Terminology
Some authors have used the terms concussion and mild-traumatic brain injury interchangeably. Others have attempted to establish differences between the 2, but one definition of the latter has not been agreed on. For the purposes of this review, concussion is used exclusively and is defined per the consensus statement from the Third International Conference on Concussion in Sport.18 In short, concussion represents an injury of physiologic dysfunction resulting from biomechanical forces acting on the brain.
Acute Worsening
In most cases, symptoms of a concussion begin immediately following the offending impact. Symptoms may be maximal at onset and gradually resolve over time, or they may worsen somewhat in the minutes to hours following the injury. Symptoms may even be delayed completely for several hours. This pattern of delayed worsening is thought to be more common when the athlete continues in the contest, either as a manifestation of continued physical activity or as the result of a second impact.9 Overall, once an athlete has been removed from the game and is resting both physically and mentally, his or her course should improve from that point forward.
In some cases, an athlete will have an acute clinical worsening of signs or symptoms minutes to hours after a stable or improving clinical picture. This pattern should alert all present to the possibility of an epidural hematoma, which occurs as the result of damage to a cerebral artery, most often the middle meningeal artery and most often in the setting of a skull fracture. This injury is known to produce a typical lucid interval, during which the athlete improves symptomatically shortly after the injury and may even appear completely normal while complaining of only minimal symptoms. As the hematoma expands, intracranial pressure increases to the point of compromising brain function, and the lucid interval comes to an end, producing a dramatic clinical worsening, most notably in the level of consciousness. Given that the expanding hematoma is the result of an arterial hemorrhage, this process is relatively quick, with worsening expected within minutes to an hour. Without emergent evaluation and treatment, an epidural hematoma can result in death.4
A concussive injury can also produce an interval of stable or improving symptoms followed by acute worsening, making the diagnosis of concussion versus epidural hematoma a difficult one. Given that the majority of the clinical information available at the time of the injury is subjective, even defining “acute worsening” can be difficult. Those caring for the athlete should keep 2 ideas in mind. First, it is imperative to continue close observation, especially of level of consciousness, for 1 to 2 hours postinjury. Second, the presence of an epidural hematoma should be considered more likely when a skull fracture is suspected. Skull fractures can be obvious or subtle, depending on the location, severity, and type of fracture. Some clinical signs should increase suspicion for fracture, such as otorrhea and rhinorrhea, suggesting a leakage of cerebral-spinal fluid. Postauricular and periorbital hematomas are also suggestive. Overall, suspicion for skull fracture should stem from the mechanism of the injury itself. The clinical approach to this dilemma should be conservative, with emergent hospital evaluation and neuroimaging (head computed tomography scan) whenever an epidural hematoma or skull fracture is suspected.
Return to Play
In the case of an athlete who experiences a concussion with an episode of acute worsening, the return-to-play paradigm should not be affected overall. In the case of an epidural hematoma, other intracranial hemorrhage, or skull fracture, the return-to-play decision becomes much more complicated. Although none of these injuries should be considered absolute indications for retirement from contact sports, they should trigger a significantly more conservative approach. Neurological or neurosurgical consultation should be obtained to help delineate future risk of further participation in sports.
Seizure
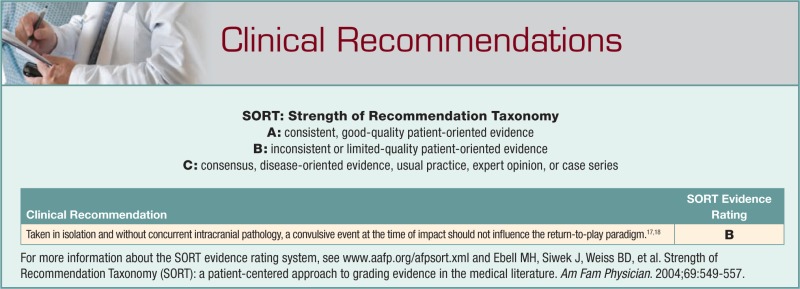
At the time of a concussive event, convulsive phenomena are relatively uncommon, with 1 study of Australian Rules football players demonstrating an incidence of 1 convulsive episode in 70 concussions.17 The clinical value of this finding appears to be minimal, and no significant change in management is required.17 In contrast, a seizure that occurs minutes to hours after the acute injury should be considered a marker for a trauma-induced structural brain lesion or hemorrhage, and the athlete should be managed appropriately, as outlined above.
Epilepsy is defined as a disorder of recurrent unprovoked seizures. Owing to the provocation of the head injury, an athlete who suffers a convulsion or seizure in the setting of concussion does not have epilepsy. Epilepsy could be diagnosed if the athlete were to have more than 1 unprovoked seizure. There does not appear to be a significant risk of developing epilepsy after a single concussion, but no data describe the risk following multiple concussions. In a study of individuals with a single “mild head injury” (defined as the absence of fracture and either a loss of consciousness or posttraumatic amnesia for less than 30 minutes), the 1-year incidence of seizure was 0.2% (incidence ratio = 3.1, 95% confidence interval = 1.0, 7.2), with no statistically significant elevated lifetime risk.2
Return to Play
Taken in isolation and without concurrent intracranial pathology, an isolated convulsive event at the time of impact should not influence the return-to-play paradigm (Strength of Recommendation Taxonomy, B).17,18 In the case of (1) a prolonged, generalized tonic-clonic seizure at the time of impact or (2) spells consistent with seizure after the initial event, neurological consultation should be obtained. In all cases, further evaluation with a routine electroencephalogram and brain magnetic resonance imaging is suggested. Patients with epilepsy, either as a preexisting condition or as a result of the head injury in question, can be cleared to play most sports once they have been evaluated and treated.7 If they participate in a sport that carries undo risk to themselves or others if they were to have a seizure, such as auto racing or swimming, neurological consultation should be an essential aspect of management.
Repetitive Concussions
In 2000, Guskiewicz and colleagues reported that high school football players who suffered a concussion were 3 times more likely to sustain another concussion during the same season, as compared to their nonconcussed teammates.10 In another report, athletes who experienced concussion with a loss of consciousness were found to be 6 times more likely to sustain another concussion than were those who had been concussed but never lost consciousness.6 These observations support the presence of one type of complicated patient, the one who experiences repetitive concussion. Without more detailed epidemiological studies, it is difficult to describe patterns of concussion at the individual level: Some athletes appear to have a propensity for concussive injury, and recognizing that propensity can be clinically useful. It can be of great benefit to the patient if the clinician carefully considers the possible reasons the patient is set apart from his or her peers.
The first, and widely discussed, explanation is that an athlete’s first concussion produces a long-lasting change in brain physiology that makes it easier to be concussed a second time.20 In this paradigm, the risk of concussion continues to increase with each subsequent concussion, as the athlete’s threshold for concussion is lowered. In these cases, it may be increasingly noticeable that less force is being required to produce each concussion. A second group of athletes may suffer from repeat concussions, not because their threshold is being lowered with the previous injury, but because their threshold was low to begin with. In these cases, there may be a sense from the onset that the athlete is more easily concussed than her or his peers. A third group may be presenting with repetitive concussions because of extrinsic (ie, not intrinsic) factors. The style of play, the adherence to rules of play, and the equipment used can all greatly increase the risk of concussion. Care should be taken to ensure that the helmets used at all levels are fitted properly and so adhere to the current standards put forth by the National Operating Committee on Standards for Athletic Equipment (see http://www.nocsae.org/).
When one evaluates an athlete who is presenting with repetitive concussions, the first step is to flesh out the nature of each individual concussion. What types of forces were experienced? Was the concussion an unexpected consequence of the impact? Had the athlete returned to baseline in between concussions? By exploring the answers to these questions, one may gain a better understanding of that athlete’s risk profile for the future.
Return to Play
Whenever possible, the clinician should first explore the possibility that the recurrent concussions are secondary to extrinsic factors, such as style of play and risk-taking behavior. Education and coaching can be powerful preventive tools. In these cases, return-to-play decisions do not hinge as much on medical issues as they do on the athletes’ understanding and willingness to adapt to safer techniques.
If one suspects that concussions are occurring with less force, serious consideration should be given to retiring the athlete from contact sports. If the athlete appears to have a low concussion threshold at the onset, retirement should also be considered, although the rationale may not be as clear, given that the long-term sequelae of multiple concussions are unknown. In such cases, neurological consultation should be strongly considered.
Prolonged Concussive Symptoms
The majority of concussions will be symptomatic for 7 to 10 days. Within this time frame, the clinician can be reasonably certain that the symptoms and findings in question are secondary to the concussive mechanism itself. As the duration of the symptomatic effect grows, one must become increasingly aware of other possible mechanisms of symptom generation, such as mood and sleep disturbances. In this setting, the return-to-play decision becomes much more difficult.
If we accept that 80% to 90% of sports-related concussions will abate symptomatically in 7 to 10 days, we can infer from estimated incidence rates that in the United States alone, between 240,000 and 570,000 concussions will last longer than 10 days. The epidemiologic characteristics of this group are largely unknown, however. Some percentage of these cases will last slightly longer than 10 days but will be otherwise similar to a typical concussion course. These cases require no significant change in the typical concussion management strategy. Other symptom courses may last for weeks to months, whereas others may seemingly take on lives of their own, lasting up to a year or beyond. Managing the patients in these 2 latter groups can be extremely difficult.
If we look closely at the possible underlying mechanisms of prolonged concussion symptoms, we find a useful theoretical clinical construct. Prolonged symptoms can be the result of a prolonged version of the initial concussion pathophysiology, or they can be manifestations of a secondary process. If present, the secondary process can be a dysfunction of neuronal physiology related to the concussive mechanism or a psychological effect of normal neuronal function. Delineating these 2 causes of a secondary effect at the physiological level is, and will likely remain, extremely difficult. Nonetheless, considering the likelihood of a primary versus secondary mechanism for the prolonged symptoms in a patient can be clinically useful.
When one evaluates a patient with prolonged symptoms, one needs to understand the natural history of the current concussion, the evolution of the symptoms, and the activity level (physical and mental) of the athlete during the period in question. Furthermore, taking a detailed history and determining the presence of any preexisting symptoms can help determine if any comorbid conditions (eg, depression, migraine headache) may be adding to the overall clinical picture. This approach may help determine if the prolonged symptoms are being driven by a primary or secondary process.
If a prolonged primary concussive mechanism is responsible, the patient is likely still improving, albeit slowly and perhaps imperceptibly. A picture of improvement can be especially hard to establish if symptoms of worsening are reported with day-to-day activity. The classic example of this is the student athlete who continues to work hard academically and has a setback after a difficult examination or assignment, experiencing an increase in headache, light sensitivity, or nausea. If the patient has a migraine headache history as well, the postconcussive period can act to increase headache frequency, producing symptoms that appear postconcussive.7 If the history is prolonged, even up to 6 to 8 weeks, but is punctuated with events of worsening with exertion and improvement with rest, the clinician should suspect that a prolonged primary mechanism is at play. These cases of prolonged concussion are best treated with the same rest-until-asymptomatic approach. The return-to-activity paradigm should be more conservative in these cases, and the clinician may even look to establish a detailed schedule of observed physical exertion. The use of medications in these patients should be minimal and restricted to short-acting, symptomatic therapies, to not cloud the pattern of resolution.
In contrast, prolonged symptoms that are the result of a secondary process tend to develop their own natural history. Close examination of the overall symptom course may uncover the usual period of initial improvement that ends before complete resolution and is followed by a period of relative stability and then clinical worsening.19 In general, these symptoms worsen with even minimal activity and no longer respond to periods of rest. These patients may be experiencing continued or worsening symptoms as the result of psychological factors related to being held out of participation; that is, a strategy of continued rest may actually be an exacerbating factor. Some authors have suggested that physical activity in these patients may be helpful.21 Because the initial concussive pathophysiology has presumably given way to a secondary process, the clinician may more confidently consider using medications with a goal of promoting a normal state of brain physiology by addressing mood and sleep symptoms. This aspect of management should be directed by a clinician who has experience managing long-term concussive symptoms.18
The clinical picture of these patients may fit into some definitions of postconcussive syndrome. The definition of postconcussive syndrome varies widely, and its diagnosis and management have been controversial.11 For purposes of this review, patients are defined as having postconcussive syndrome when they experience symptoms that the clinician believes are not directly caused by the acute concussive process.
Return to Play
At the onset, the hallmark of concussion management is physical and cognitive rest. As symptoms continue along a prolonged course, there will come a time when rest alone does not provide the desired benefit. It is at this point that the focus of management should expand to include the careful reintroduction of physical activity, the possible introduction of pharmacological therapies, and the consideration of psychological evaluation and treatment. The difficult role of the sports medicine care provider in these cases is to determine which of these management strategies are appropriate. Input from a neurologist with experience in concussion management can be useful. Ultimately, the return-to-play decision still hinges on being as certain as possible that the concussive event is over.
Retirement From Contact Sports
It is important that any return-to-play or retirement decision not be made based only on the circumstances of the most recent concussion. In every case, the most recent event should be placed in the context of the athlete’s lifetime concussion experience. The sports medicine field is currently unable to predict the absolute number of concussions that any individual can experience without producing long-term effects. The sports medicine provider should carefully examine all available subjective and objective clinical evidence for the presence of any troublesome pattern or trend. The identification of any of the following 3 scenarios should warrant the strong consideration of recommending retirement from contact sports.
Substantial Symptom Burden
If an athlete’s symptomatic course following concussion is serious enough to interfere with school, work, or family productivity to a significant degree, retirement should be considered. The term significant is relative, of course, and its meaning to the patient should be explored. The important concept is that the athlete fully understand what consequences future concussions could have on his or her productivity.
Decreasing Force Needed to Cause Injury
Determining the nature and severity of each impact that leads to concussion can help establish a trend. Often times, this requires seeking out and asking teammates and witnesses who may not be with the athlete at the time of the clinical evaluation. Although the risks of repetitive concussions are not yet well established, an individual who appears to be sustaining injuries with diminishing force should be counseled to avoid contact sports.
Changes From Baseline in Cognition or Personality
The complexity and plasticity of the brain make it difficult to determine if it is functioning “normally,” which is relative to the individual. For these reasons, establishing a change in the baseline function of the brain of a previously concussed athlete becomes paramount in making retirement decisions. The determination of a new baseline level of brain function implies that there are no longer any ongoing direct effects from a previous concussion. Measures of cognitive function over time are extremely helpful. In addition to the use of computerized neuropsychological testing, the work or school performance of the athlete should be considered. Formal neuropsychological evaluation is often required to help establish and define cognitive dysfunction. Other aspects of the athlete’s mental status should be explored—especially, personality and affect. Questioning family members and friends can help elucidate subtle changes.
It is also important to investigate other possible causes of changes in cognition or personality. Psychiatric disorders, neurodegenerative disorders, and substance abuse can all produce similar presentations. Any objective change in baseline cognitive ability that is thought to be attributable to concussive injury warrants retirement from contact sports. Subjective changes in cognitive abilities or personality are more difficult to assess. In these cases, neurological or neuropsychological consultation may be helpful.
Several additional considerations can affect the retirement decision. In the case of a skull fracture, the increased risk of a subsequent head injury should be discussed with a neurosurgical consultant. As well, any evidence of trauma-induced brain pathology (as described on neuroimaging) or the presence of incidental findings (eg, arachnoid cysts, arteriovenous malformations) can significantly change an athlete’s risk profile and so warrant further specialist consultation.
Finally, note that the decision to retire an athlete from contact sports should be made while considering the benefits of continued participation. Depending on the level of play and the age of the athlete, the positive outcomes from playing contact sports can range from simple, beneficial effects of exercise to a professional livelihood. Each situation requires careful consideration of all the possible outcomes, positive and negative, that can result from the decision.
Conclusions
Sports-related concussion is a common injury with a varied and complex presentation. Classifying concussive injuries into a clinically useful schema has proven difficult, but the sports medicine provider can recognize complicated concussion patients when considering the larger clinical picture. Concussion management should include consideration of the athlete’s lifetime concussion experience, unusual aspects of the concussion history, and a careful estimation of the overall risk of continued participation.
Footnotes
No potential conflict of interest declared.
References
- 1. American Academy of Neurology Practice parameter: the management of concussion in sports (summary statement). Report of the Quality Standards Subcommittee. Neurology. 1997;48:581-585 [DOI] [PubMed] [Google Scholar]
- 2. Annegers J, Hauser W, Coan S, Rocca W. A population-based study of seizures after traumatic brain injuries. N Engl J Med. 1998;338(1):20-24 [DOI] [PubMed] [Google Scholar]
- 3. Aubry M, Cantu R, Dvorak J, et al. Summary and agreement statement of the First International Conference on Concussion in Sport, Vienna, 2001. Recommendations for the improvement of safety and health of athletes who may suffer concussive injuries. Br J Sports Med. 2002;36:6-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cantu R. Head injuries in sport. Br J Sports Med. 1996;30:289-296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cantu R. Posttraumatic retrograde and anterograde amnesia: pathophysiology and implications in grading and safe return to play. J Athl Train. 2001;36(3):244-248 [PMC free article] [PubMed] [Google Scholar]
- 6. Delaney J, Lacroix V, Leclerc S, et al. Concussions during the 1997 Canadian Football League season. Clin J Sport Med. 2000;10(1):9-14 [DOI] [PubMed] [Google Scholar]
- 7. Dimberg E, Burns T. Management of common neurologic conditions in sports. Clin Sports Med. 2005;24(3):637-662 [DOI] [PubMed] [Google Scholar]
- 8. Gessel B, Fields S, Collins C, et al. Concussions among United States high school and collegiate athletes. J Athl Train. 2007;42(4):495-503 [PMC free article] [PubMed] [Google Scholar]
- 9. Guskiewicz K, McCrea M, Marshall S, et al. Cumulative effects of recurrent concussion in collegiate football players: The NCAA Concussion Study. JAMA. 2003;290:2549-2555 [DOI] [PubMed] [Google Scholar]
- 10. Guskiewicz K, Weaver N, Padua D, Garett W. Epidemiology of concussion in collegiate and high school football players. Am J Sports Med. 2000;28(5);643-650 [DOI] [PubMed] [Google Scholar]
- 11. Iverson GL. Outcome from mild traumatic brain injury. Curr Opin Psychiatry. 2005;18(3):301-317 [DOI] [PubMed] [Google Scholar]
- 12. Johnston K, Bloom G, Ramsay J, et al. Current concepts in concussion rehabilitation. Curr Sports Med Rep. 2004;3:316-323 [DOI] [PubMed] [Google Scholar]
- 13. Langlois J, Rutland-Brown W, Marlena M. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21:375-378 [DOI] [PubMed] [Google Scholar]
- 14. Lovell M, Iverson G, Collins M, et al. Does loss of consciousness predict neuropsychological decrements after concussion? Clin J Sport Med. 1999;9:193-199 [DOI] [PubMed] [Google Scholar]
- 15. McClincy M, Lovell M, Pardini J, et al. Recovery from sports concussion in high school and collegiate athletes. Brain Inj. 2006;20(1):33-39 [DOI] [PubMed] [Google Scholar]
- 16. McCrea M, Guskiewicz K, Marshall S, et al. Acute effects and recovery time following concussion in collegiate football players: the NCAA concussion study. JAMA. 2003;290(19):2556-2563 [DOI] [PubMed] [Google Scholar]
- 17. McCrory P, Berkovic S. Concussive convulsions: incidence in sport and treatment recommendations. Sports Med. 1998;23(2):131-136 [DOI] [PubMed] [Google Scholar]
- 18. McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on concussion in sport: the 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Clin J Sport Med. 2009;19:185-195 [DOI] [PubMed] [Google Scholar]
- 19. McHugh T, Laforce R, Gallagher P, et al. Natural history of the long-term cognitive, affective, and physical sequelae of mild traumatic brain injury. Brain Cogn. 2006;60(2):209-211 [PubMed] [Google Scholar]
- 20. Schultz M, Marshall S, Mueller F, et al. Incidence and risk factors for concussion in high school athletes, North Carolina, 1996-1999. Am J Epidemiol. 2004;160(10):937-944 [DOI] [PubMed] [Google Scholar]
- 21. Willer B, Leddy J. Management of concussion and post-concussive syndrome. Curr Treat Options Neurol. 2006;8:415-426 [DOI] [PubMed] [Google Scholar]