Abstract
Context:
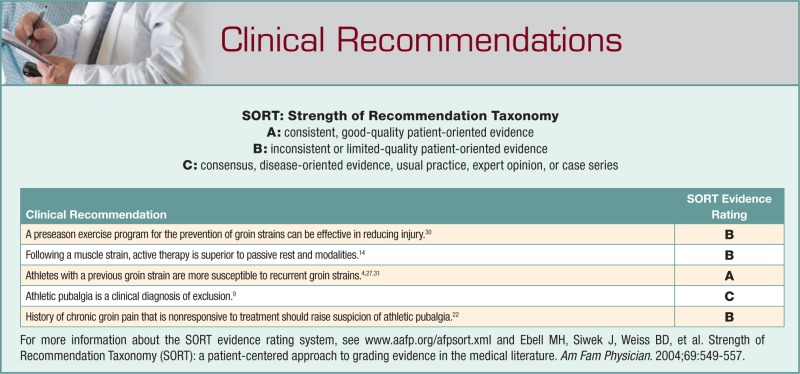
An in-season groin injury may be debilitating for the athlete. Proper diagnosis and identification of the pathology are paramount in providing appropriate intervention. Furthermore, an adductor strain that is treated improperly can become chronic and career threatening. Any one of the 6 muscles of the adductor muscle group can be involved. The degree of injury can range from a minor strain (grade 1), where minimal playing time is lost, to a severe strain (grade 3), in which there is complete loss of muscle function. Persistent groin pain and muscle imbalance may lead to athletic pubalgia.
Evidence Acquisition:
Relevant studies were identified through a literature search of MEDLINE and the Cochrane database from 1990 to 2009, as well as a manual review of reference lists of identified sources.
Results:
Ice hockey and soccer players seem particularly susceptible to adductor muscle strains. In professional ice hockey and soccer players throughout the world, approximately 10% to 11% of all injuries are groin strains. These injuries have been linked to hip muscle weakness, a previous injury to that area, preseason practice sessions, and level of experience. This injury may be prevented if these risk factors are addressed before each season.
Conclusion:
Despite the identification of risk factors and strengthening intervention for athletes, adductor strains continue to occur throughout sport. If groin pain persists, the possibility of athletic pubalgia needs to be explored, because of weakening or tears in the abdominal wall muscles. A diagnosis is confirmed by exclusion of other pathology.
Keywords: adductor strain, athletic pubalgia, groin injury
The evaluation and treatment of groin pain in athletes is challenging, and the anatomy is complex. Multiple pathologies often coexist that may cause similar symptoms, and several organ systems can refer pain to the groin. Many athletes with groin pain have tried prolonged rest and various treatment regimens and received differing opinions regarding the cause of their pain. The rehabilitation specialist is often given a nonspecific referral of “groin pain” or “anterior hip pain,” the cause of which can be as simple as a tight iliopsoas (which may require stretching) or as complex as athletic pubalgia.
Athletic pubalgia is defined as an injury to the rectus abdominis insertion onto the pubic symphysis, often accompanied by injury to the conjoined tendon insertion and the adductor longus attachment to the pelvis.1,3,21 The distinctive feature of this disorder is subtle pelvic instability and accompanying compromise of the transversalis fascia, eventually leading to incompetency of the posterior inguinal wall.10,17 The exact structures involved are not always clear unless surgery is performed, and overlapping conditions may exist.12 A muscle imbalance between the adductor muscles and abdominal muscles may be the underlying cause of athletic pubalgia,3 but this has yet to be proven.
Adductor Muscle Strains
The adductors of the hip joint include 6 muscles: the adductor longus, magnus, and brevis and the gracilis, obturator externus, and pectineus. All these are innervated by the obturator nerve, with the exception of the pectineus, which receives innervation from the femoral nerve. The primary function of this muscle group is adduction of the thigh in open chain motions and stabilization of the lower extremity and pelvis in closed chain motion. The adductor longus is most commonly injured during sporting activity.26 Its lack of mechanical advantage may make it more susceptible to strain. An important anatomic consideration in groin pain is the local distribution of cutaneous nerves in the inguinal region. Akita et al1 examined the cutaneous branches of the inguinal region in 27 male adult cadavers. The ilioinguinal nerve and cutaneous branches were present in 49 of 54 half specimens, and genitofemoral cutaneous branches were present in 19 of 54.1 The cutaneous branches of the ilioinguinal nerve traverse around the spermatic cord and are distributed to the skin of the dorsal surface of the scrotum. The ilioinguinal nerve and the genital branch of the genitofemoral nerve are considered the most critical sensory nerves, and they likely play a key role in the chronic pain produced by groin injuries.
Adductor muscle strains can result in missed playing time for athletes in many sports. Adductor muscle strains are frequently encountered in ice hockey and soccer.6,8,20 These sports require a strong eccentric contraction of the adductor musculature during competition.29 Adductor muscle strength has recently been linked to the incidence of adductor muscle strains. Specifically, the strength ratio of the adduction:abduction muscle groups has been identified as a risk factor in professional ice hockey players.31 Intervention programs can lower the incidence of adductor muscle strains but not prevent them altogether.12,30 Proper injury treatment and rehabilitation should be implemented to limit the amount of missed playing time and avoid surgical intervention.14
An adductor strain is defined as an injury to the muscle-tendon unit that produces pain on palpation of the adductor tendons or its insertion on the pubic bone with or without pain during resisted adduction.20 Adductor strains are graded as a first-degree strain if there is pain but minimal loss of strength and minimal restriction of motion. A second-degree strain is defined as tissue damage that compromises the strength of the muscle but does not include complete loss of strength and function. A third-degree strain denotes complete disruption of the muscle tendon unit and loss of muscle function.20 A thorough history, clinical examination, magnetic resonance imaging (MRI), bone scan, and radiograph can be useful in differentiating groin strains from athletic pubalgia, osteitis pubis, hernia, hip flexor strain, intra-articular hip abnormalities, rectal or testicular referred pain, piriformis syndrome, lumbar disc pathology, or a fracture of the pelvis or the lower extremities. More obscure etiologies may include genitourinary infections, avascular necrosis of the hip, or soft tissue tumors.5
Epidemiology
The exact incidence of adductor muscle strains in most sports is unknown because athletes often play through minor groin pain and the injury goes unreported. In addition, overlapping diagnoses can skew the incidence. Groin strains accounted for 10% of all injuries in elite Swedish ice hockey players.17 Molsa et al23 reported that groin strains accounted for 43% of all muscle strains in elite Finnish ice hockey players. The incidence of groin strains in a single National Hockey League (NHL) team was 3.2 strains per 1000 player-game exposures.31 In a larger study of 26 NHL teams, Emery et al8 reported that the incidence of adductor strains in the NHL increased from 2003 to 2009. The rate of injury was greatest during the preseason compared with regular and postseason play. Prospective soccer studies in Scandinavia showed a groin strain incidence rate of 10 to 18 injuries per 100 soccer players.24 Giza et al12 reported that 9.5% of all professional US male soccer players incurred a groin strain in the 2002 season. Ekstrand and Gillquist6 documented 32 groin strains in 180 male soccer players, representing 13% of all injuries over the course of 1 year. Despite their prevalence, adductor muscle strains are not isolated to these 2 sports.
Risk Factors
Previous studies have shown an association between strength or flexibility and musculoskeletal strains in various athletic populations.6,18,25 Ekstrand and Gillquist6 found decreased preseason hip abduction range of motion in soccer players who subsequently sustained groin strains, compared with uninjured players. This finding is in contrast to the data on professional ice hockey players that found no relationship between passive or active abduction range of motion (adductor flexibility) and adductor muscle strains.7,8,29 Adductor muscle strength has been associated with a subsequent muscle strain. Tyler et al31 found that preseason hip adduction strength was 18% lower in NHL players who subsequently sustained groin strains, compared with the uninjured players. The hip adduction:abduction strength ratio was also significantly different between the 2 groups. Injured players had less adduction strength. In the players who sustained a groin strain, preseason adduction:abduction strength ratio was lower on the side that subsequently sustained a groin strain (as compared with the uninjured side). Adduction strength was 86% of abduction strength on the uninjured side but only 70% of abduction strength on the injured side. Conversely, a study on adductor strains in ice hockey players found no relationship between peak isometric adductor torque and the incidence of adductor strains.7 Unlike the Tyler study, this study had multiple testers using a handheld dynamometer, which could increase the variability in strength testing and decrease the likelihood of finding strength differences.
Emery and colleagues’ results7 demonstrated that players who practiced during the off-season were less likely to sustain a groin injury, as were rookies in the NHL. In this study, the final risk factor was the presence of a previous adductor strain. Tyler et al31 also linked preexisting injury as a risk factor to recurrent injury for 4 of the 9 groin strains (44%). This is consistent with Seward et al,27 who reported a 32% recurrence rate for groin strains in Australian Rules football.
Arnason et al4 conducted a multivariate prospective analysis in 306 professional male soccer players in Iceland and determined that the predictor risk factors were previous groin strains (odds ratio = 7.3, P = .001) and decreased range of motion in hip abduction (odds ratio = 0.9 [1°], P = .05). It has become increasingly apparent that groin strains and athletic pubalgia have continued to rise in hockey, soccer, and American football.§
Intervention
Tyler et al30 were able to demonstrate that strengthening the adductor muscle group could be an effective method for preventing adductor strains in professional ice hockey players. Before the 2000 and 2001 seasons, professional players were strength tested, and 33 of 58 players were classified as at risk—that is, an adduction:abduction strength ratio of less than 80%. These players were placed on an intervention program consisting of strengthening and functional exercises aimed at increasing adductor strength (see Tables 1 and 2). The injuries were tracked over the course of the 2 seasons: 3 adductor strains occurred in games. The incidence was 0.71 adductor strains per 1000 player-game exposures and accounted for approximately 2% of all injuries. In the previous 2 seasons before the intervention, there were 11 adductor strains (incidence of 3.2 per 1000 player-game exposures), accounting for approximately 8% of all injuries. This was significantly lower than the incidence reported by Lorentzon et al,19 who found adductor strains to account for 10% of all injuries in ice hockey players. Of the 3 players injured in the Tyler study, none had sustained a previous adductor strain on the same side. One player had bilateral adductor strains at different times during the first season. The Tyler et al study suggests that adductor strengthening can be an effective method for preventing adductor strains in professional ice hockey players.
Table 1.
Adductor strain postinjury program.
| Phase 1: Acute | First 48 hours after injury: RICE (rest, ice, compression, elevation) |
| Nonsteroidal anti-inflammatory drugs | |
| Massage | |
| Transcutaneous electrical nerve stimulation | |
| Ultrasound | |
| Submaximal isometric adduction with knees bent → with knees straight progressing to maximal isometric adduction, pain free | |
| Hip passive range of motion in pain-free range | |
| Nonweightbearing hip progressive resistance exercises without weight in antigravity position (all except abduction): pain free, low load, high repetition | |
| Upper body and trunk strengthening | |
| Contralateral lower extremity strengthening | |
| Flexibility program for noninvolved muscles | |
| Bilateral balance board | |
| Clinical milestone | Concentric adduction against gravity without pain |
| Phase 2: Subacute | Bicycling/swimming |
| Sumo squats | |
| Single-limb stance | |
| Concentric adduction with weight against gravity | |
| Standing with involved foot on sliding board moving in frontal plane | |
| Adduction in standing on cable column or resistance band | |
| Seated adduction machine | |
| Bilateral adduction on sliding board moving in frontal plane (ie, simultaneous bilateral adduction) | |
| Unilateral lunges (sagittal) with reciprocal arm movements | |
| Multiplane trunk tilting | |
| Balance board squats with throwbacks | |
| General flexibility program | |
| Clinical milestone | Lower extremity passive range of motion equal to that of the uninvolved side and involved adductor strength at least 75% that of the ipsilateral abductors |
| Phase 3: Sports-specific training | Phase II exercises with increase in load, intensity, speed and volume |
| Standing resisted stride lengths on cable column to simulate skating | |
| Slide board | |
| On ice kneeling adductor pull togethers | |
| Lunges (in all planes) | |
| Correct or modify ice skating technique | |
| Clinical milestone | Adduction strength at least 90-100% of the abduction strength and involved muscle strength equal to that of the contralateral side |
Table 2.
Adductor strain injury prevention program.
| Warm-up | Bike |
| Adductor stretching | |
| Sumo squats | |
| Side lunges | |
| Kneeling pelvic tilts | |
| Strengthening program | Ball squeezes (legs bent to legs straight) |
| Different ball sizes | |
| Concentric adduction with weight against gravity | |
| Adduction in standing on cable column or elastic resistance | |
| Seated adduction machine | |
| Standing with involved foot on sliding board moving in sagittal plane | |
| Bilateral adduction on sliding board moving in frontal plane (ie, simultaneous bilateral adduction) | |
| Unilateral lunges with reciprocal arm movements | |
| Sports-specific training | On ice kneeling adductor pull togethers |
| Standing resisted stride lengths on cable column to simulate skating | |
| Slide skating | |
| Cable column crossover pulls | |
| Clinical goal | Adduction strength at least 80% of the abduction strength |
Despite the identification of risk factors and strengthening intervention for ice hockey players, adductor strains continue to occur in most sports.3,13,16,19 The high incidence of recurrent strains could be due to incomplete rehabilitation or inadequate time for complete tissue repair.30 Hagglund et al13 studied 12 elite Swedish male soccer teams to determine if prior injury served as a risk factor for a recurrence in a subsequent consecutive season. They determined that those players who sustained a previous hamstring, groin, or knee injury were 2 to 3 times more likely to incur a recurrence in the following season. Interestingly, no such relationship was found with ankle sprains.13 Homlich et al14 found that an 8- to 12-week active strengthening program consisting of progressive resistive adduction and abduction exercises, balance training, abdominal strengthening, and skating movements on a slide board proved more effective in treating chronic groin strains, whereas a passive physical therapy program of massage, stretching, and modalities was ineffective in treating chronic groin strains.
An increased emphasis on strengthening exercises may reduce the recurrence rate of groin strain. Tyler et al30 developed an adductor muscle strain injury program progressing the athlete through the phases of healing, which, anecdotally, seems to be effective (Table 2). This type of treatment regime combines modalities: passive treatment immediately followed by an active training program emphasizing eccentric resistive exercise. This method of rehabilitation has been supported.3,22
A comprehensive 20-minute alternative warm-up program was recently developed to address the rise in groin-related injuries in adult male professional soccer players in US Major League Soccer. This 20-minute program was used 2 to 3 times per week during the 2004 season. Active players (N, 315) were prospectively and randomly enrolled into 1 of 2 groups: Group 1 participants (n, 106) served as the groin injury prevention group; Group 2 participants (n, 209) served as the matched control group (age, sex, skill) and continued with their usual preseason and warm-up training. The groin injury prevention program was a combination of dynamic stretching, core strengthening, and pelvic proprioceptive exercises to encourage a neutral pelvis during dynamic activities using the lumbar paraspinals, multifidus, rectus abdominus, transversus, internal and external obliques, abductors, adductors, and hip external and internal rotators. During the season, certified athletic trainers recorded all groin injuries into a central database. The overall incidence of groin injuries occurring in the 2004 season was 10.9%; in Group 1 (intervention), 0.44 injuries per 1000 hours; and in Group 2 (control), 0.61 injuries per 1000 hours. The incidence of athletes requiring groin surgery in the intervention group was 0.13 per 1000 hours, compared with the control group incidence of 0.18 per 1000 hours (P > .05). The groin injury prevention program was successful in reducing injury by 28%, when compared with the control group (P < .05).
Athletic Pubalgia
Athletic pubalgia occurs with weakening of the rectus abdominis, pyramidalis, internal and external obliques, transversus abdominis muscles, and/or the tendons.10 This is where inguinal hernias occur: the inguinal canal. When an inguinal hernia occurs because of weakening of the abdominal wall, a hernia may be felt. In the case of an athletic pubalgia, there is weakening or tears in the abdominal wall muscles but no palpable hernia. Fon et al9 described athletic pubalgia as an incipient hernia, based on the findings of a posterior bulge found in 80% to 85% of surgeries. This is analogous to a classic inguinal hernia where the absence of striated muscle at the posterior inguinal wall and the passage of the spermatic cord predispose the abdominal wall to weakness. In athletic pubalgia, the anatomically thin transversalis fascia that forms part of the posterior wall is injured. Joesting15 defines the athletic pubalgia as an actual tear in the transversalis fascia in the posterior inguinal wall between the internal inguinal ring and the pubic tubercle, typically 3 to 5 cm long.15 Lynch and Renstrom also localized the pathology to the posterior inguinal wall.20
Athletic pubalgia is a common cause of chronic groin pain in athletes. Most often seen in soccer and ice hockey players, athletic pubalgia can be encountered in a variety of sports and in a variety of age groups. Despite several reports of athletic pubalgia in women, it is almost exclusively found in men.4,6 It is largely a clinical diagnosis of exclusion, with a history of chronic groin pain that is nonresponsive to treatment. Physical examination findings are subtle, and most tests do not definitively confirm the diagnosis.20 Nonoperative treatment of athletic pubalgia does not often result in resolution of symptoms.21 Surgical intervention results in a pain-free return of full activities in a majority of cases.7,12,14
The symptoms of athletic pubalgia are characterized by pain during sports movements—particularly, twisting and turning during single-limb stance. This pain usually radiates to the adductor muscle region and origin and to the testicles, often difficult for the patient to pinpoint. There may be excessive anterior pelvic tilting and/or an internal rotation of the ilium on the symptomatic side concomitant with the adductor pathology. Following sports activity, the athlete may be stiff and sore, and after competition, mobility and practice can be difficult. Physical exertion that increases intra-abdominal pressure, such as coughing or sneezing, can cause pain. Pain resolution after a sports herniorrhaphy may be due to the nerve decompression during the surgical procedure itself.1
Imaging
Groin pain has been investigated through plain radiograph, dynamic ultrasound, bone scan, computed tomography scanning, and MRI.2,5 Although MRI findings such as bone marrow edema, adductor muscle strain, and hernias have been described in athletes with chronic groin pain, there has been a paucity of attention to a direct association between clinical findings and the on-field functional performance.2,5,11 Slavotinek et al published a report analyzing the association of preseason clinical findings and functional outcomes throughout the season with 52 Australian football players28: Preseason MRI showed pubic bone marrow edema in 19 (37%) and linear parasymphysial T2 hyperintensity in 16 (31%). Groin pain restricted training during the season in 22 (42%), and 9 (17%) missed at least 1 game. Preseason pain (P = .0004), pubic bone tenderness (P = .02), and linear parasymphysial T2 hyperintensity (P = .01) were directly associated with restricted training capacity during the subsequent season. Of 39 athletes with groin tenderness, 16 (41%) had linear parasymphyseal T2 hyperintensity on MRI (largely paracortical in location), of whom 11 (69%) experienced training restriction. The 16 athletes with groin tenderness and a T2 hyperintense line were more likely to experience training restriction (P = .01) than were other athletes in the study.28 Continued advancement in imaging techniques may allow the clinician to identify high-risk individuals and institute preventative intervention before the development of symptoms.
Conclusions
Rehabilitation of the groin should normalize lower extremity muscle balance and protect the groin during energy transfer during sports participation. With the use of an evidence-based rehabilitation program,14,30 the athlete may return to sports and prevent further episodes. Although complex at times, the highly skilled clinician can determine if overlapping conditions exist and can localize the primary source of the pain and dysfunction
Footnotes
NATA Members: Receive 3 free CEUs each year when you subscribe to Sports Health and take and pass the related online quizzes! Not a subscriber? Not a member? The Sports Health–related CEU quizzes are also available for purchase. For more information and to take the quiz for this article, visit www.nata.org/sportshealthquizzes.
No potential conflicts of interest declared.
References
- 1. Akita K, Niga S, Yamato Y, Muneta T, Sato T. Anatomic basis of chronic groin pain with special reference to athletic pubalgia. Surg Radiol Anat. 1999;21(1):1-5 [DOI] [PubMed] [Google Scholar]
- 2. Albers SL, Spritzer CE, Garrett WE, Jr, Meyers WC. MR findings in athletes with pubalgia. Skeletal Radiol. 2001;30(5):270-277 [DOI] [PubMed] [Google Scholar]
- 3. Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med. 2001;29(4):521-533 [DOI] [PubMed] [Google Scholar]
- 4. Arnason A, Sigurdsson SB, Gudmundsson A, Holme I, Engebretsen L, Bahr R. Risk factors for injuries in football. Am J Sports Med. 2004;32(1)(suppl):5-16 [DOI] [PubMed] [Google Scholar]
- 5. Ekberg O, Sjoberg S, Westlin N. Sports-related groin pain: evaluation with MR imaging. Eur Radiol. 1996;6(1):52-55 [DOI] [PubMed] [Google Scholar]
- 6. Ekstrand J, Gillquist J. The avoidability of soccer injuries. Int J Sports Med. 1983;4(2):124-128 [DOI] [PubMed] [Google Scholar]
- 7. Emery CA, Meeuwisse WH. Risk factors for groin injuries in hockey. Med Sci Sports Exerc. 2001;33(9):1423-1433 [DOI] [PubMed] [Google Scholar]
- 8. Emery CA, Meeuwisse WH, Powell JW. Groin and abdominal strain injuries in the National Hockey League. Clin J Sport Med. 1999;9(3):151-156 [DOI] [PubMed] [Google Scholar]
- 9. Fon L, Spence R. Sportsman’s hernia. Br J Sports Med. 2000;87(5):545-552 [DOI] [PubMed] [Google Scholar]
- 10. Genitsaris M, Goulimaris I, Sikas N. Laparoscopic repair of groin pain in athletes. Am J Sports Med. 2004;32(5):1238-1242 [DOI] [PubMed] [Google Scholar]
- 11. Gibbon WW, Hession PR. Diseases of the pubis and pubic symphysis: MR imaging appearances. Am J Roentgenol. 1997;169(3):849-853 [DOI] [PubMed] [Google Scholar]
- 12. Giza E, Mithöfer K, Farrell L, Zarins B, Gill T. Injuries in women’s professional soccer. Br J Sports Med. 2005;39(4):212-216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hagglund M, Waldén M, Ekstrand J. Previous injury as a risk factor for injury in elite football: a prospective study over two consecutive seasons. Br J Sports Med. 2006;40(9):767-772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Holmich P, Uhrskou P, Ulnits L, et al. Effectiveness of active physical training as treatment for long-standing adductor-related groin pain in athletes: randomized trial. Lancet. 1999;353(9151):339-443 [DOI] [PubMed] [Google Scholar]
- 15. Joesting DR. Diagnosis and treatment of sportsman’s hernia. Curr Sports Med Rep. 2002;1(2):121-124 [DOI] [PubMed] [Google Scholar]
- 16. Jorgenson U, Schmidt-Olsen S. The epidemiology of ice hockey injuries. Br J Sports Med. 1986;20(1):7-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kluin J, den Hoed PT, van Linschoten R, Ijzerman JC, van Steensel CJ. Endoscopic evaluation and treatment of groin pain in the athlete. Am J Sports Med. 2004;32(4):944-949 [DOI] [PubMed] [Google Scholar]
- 18. Knapik JJ, Bauman CL, Jones BH, Harris JM, Vaughan L. Preseason strength and flexibility imbalances associated with athletic injuries in female athletes collegiate athletes. Am J Sports Med. 1991;19(1):76-81 [DOI] [PubMed] [Google Scholar]
- 19. Lorentzon R, Wedren H, Pietila T. Incidences, nature, and causes of ice hockey injuries: a three year prospective study of a Swedish elite ice hockey team. Am J Sports Med. 1988;16(4):392-396 [DOI] [PubMed] [Google Scholar]
- 20. Lynch SA, Renstrom PA. Groin injuries in sport: treatment strategies. Sports Med. 1999;28(2):137-144 [DOI] [PubMed] [Google Scholar]
- 21. Meyers WC, Foley DP, Garrett WE, Lohnes JH, Mandlebaum BR. Management of severe lower abdominal or inguinal pain in high-performance athletes: PAIN (Performing Athletes With Abdominal or Inguinal Neuromuscular Pain Study Group). Am J Sports Med. 2000;28(1):2-8 [DOI] [PubMed] [Google Scholar]
- 22. Meyers WC, Lanfranco A, Castellanos A. Groin pain in athletes. Curr Sports Med Rep. 2002;1(5):301-305 [DOI] [PubMed] [Google Scholar]
- 23. Molsa J, Airaksinen O, Näsman O, Torstila I. Ice hockey injuries in Finland: a prospective epidemiologic study. Am J Sports Med. 1997;25(4):495-499 [DOI] [PubMed] [Google Scholar]
- 24. Nielsen AB, Yde J. Epidemiology and traumatology of injuries in soccer. Am J Sports Med. 1989;17(6):803-807 [DOI] [PubMed] [Google Scholar]
- 25. Orchard J, Marsden J, Lord S, Garlick D. Preseason hamstring muscle weakness associated with hamstring muscle injury in Australian footballers. Am J Sports Med. 1997;25(1):81-85 [DOI] [PubMed] [Google Scholar]
- 26. Renström P, Peterson L. Groin injuries in athletes. Br J Sports Med. 1980;14(1):30-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Seward H, Orchard J, Hazard H, Collinson D. Football injuries in Australia at the elite level. Med J Aust. 1993;159(5):298-301 [DOI] [PubMed] [Google Scholar]
- 28. Slavotinek JP, Verrall GM, Fon GT, Sage MR. Groin pain in footballers: the association between preseason clinical and pubic bone magnetic resonance imaging findings and athlete outcome. Am J Sports Med. 2005;33(6):894-899 [DOI] [PubMed] [Google Scholar]
- 29. Tegner Y, Lorentzon R. Ice hockey injuries: incidence, nature and causes. Br J Sports Med. 1991;25(2):87-89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tyler TF, Campbell R, Nicholas SJ, Donellan S, McHugh MP. The effectiveness of a preseason exercise program on the prevention of groin strains in professional ice hockey players. Am J Sports Med. 2002;30(5):680-683 [DOI] [PubMed] [Google Scholar]
- 31. Tyler TF, Nicholas SJ, Campbell RJ, McHugh MP. The association of hip strength and flexibility on the incidence of groin strains in professional ice hockey players. Am J Sports Med. 2001;29(2):124-128 [DOI] [PubMed] [Google Scholar]