Abstract
Background:
Novel interventions that can safely and effectively overload muscle early following anterior cruciate ligament reconstruction are needed to minimize atrophy and weakness that often becomes longstanding.
Evidence Acquisition:
Eccentrically induced forces can be safely applied during the early stages of rehabilitation following surgery and serve as a potent stimulus for increasing muscle size and strength.
Results:
Compared to a standard rehabilitation program, adding an early 12-week eccentric resistance-training program 3 weeks after anterior cruciate ligament reconstruction induces improvement in quadriceps and gluteus maximus volume at 15 weeks and at 1 year after surgery. Likewise, those who performed an eccentrically biased rehabilitation program also achieved greater improvements in quadriceps strength and hopping ability measured at 15 weeks and at 1 year after surgery.
Clinical Relevance:
There is potential to safely and feasibly perform eccentric contractions as part of a formal rehabilitation program following anterior cruciate ligament reconstruction.
Keywords: eccentric, rehabilitation, anterior cruciate ligament reconstruction, outcomes
The gross atrophy of the quadriceps following a knee injury and eventual anterior cruciate ligament reconstruction (ACL-R) is profound and can be a source of angst for the patient and the rehabilitation specialist. Fortunately, most postoperative rehabilitation approaches are safe, accelerated, and generally effective. However, persistent 10% to 20% deficits in quadriceps size and strength can remain for years after surgery, and this can adversely impact performance.§ Because the greatest deficits occur during the early stages (ie, first 3 months postoperatively) of rehabilitation, 3-5,22,24,26 the use of eccentric (ECC) muscle activity has been tested as a countermeasure to these muscle impairments.5-8 This work has capitalized on the basic physiologic principle of muscle overload induced by the early introduction of progressive ECC muscle activity performed in a controlled fashion for a typical 15-week postoperative rehabilitation program; such a program is designed to counter quadriceps atrophy and strength loss in a safe and efficacious manner. The purpose of this manuscript is to review the experience using an eccentrically biased resistance exercise program following ACL-R.
Eccentric Resistance Exercise
An acute exposure to high-force ECC muscle contractions can induce muscle damage. Importantly, however, a chronic, gradually increasing exposure to eccentrically induced forces can be safe and serve as a potent stimulus for increasing muscle size and strength.6,8,11,17,18 These improvements appear to be a function of the muscle’s ability to produce high forces.19,20 Because ECC muscle contractions produce 2 to 3 times greater force than either isometric or concentric muscle contraction,14,15 ECC exercise has the potential to overload the muscle to a greater extent and to enhance improvements in muscle size and strength.
Research Design
The research design of the studies underlying this review has been previously published.5-8 A complete list of testing measures and time periods is included in Table 1. Briefly, 40 subjects who were matched by graft type, gender, and age were randomly assigned into either an eccentrically biased or standard rehabilitation program beginning 3 weeks after ACL-R. The subjects in the ECC group then began a 12-week progressive, eccentrically induced, negative-work exercise program using 1 of 2 available recumbent ECC ergometers (Figure 1). Following the 12-week training program (approximately 15 weeks following ACL-R surgery) supervised rehabilitation was discontinued for both rehabilitation groups. At that time, subjects were encouraged to perform traditional progressive resistance exercises 2 to 3 times per week as a home exercise program and to gradually increase activity as tolerated. Periodic routine physical evaluations were continued until 1 year following ACL-R.
Table 1.
Summary of tests and measures taken during various times following anterior cruciate ligament reconstruction.a
| Pretraining | Training | Post-training | |||||
|---|---|---|---|---|---|---|---|
| Constructs | Variables (Instruments/Measures) | 3 Days Before ACL-R | 3 Weeks After ACL-R | 3-15 Weeks After ACL-R | 15 Weeks After ACL-R | 26 Weeks After ACL-R | 52 Weeks After ACL-R |
| Safety | Knee stability (KT-1000) | √ | √ | √ | √ | ||
| Knee effusion (joint circumference) | √ | √ | √ | √ | √ | √ | |
| Knee pain (VAS) | √ | √ | √ | ||||
| Thigh pain (VAS) | √ | √ | √ | ||||
| Muscle size | Muscle volume (MRI) | √ | √ | √ | |||
| Muscle function | Strength (isokinetic peak torque) | √ | √ | √ | √ | ||
| Performance | Hopping ability (distance hopped) | √ | √ | √ | √ | ||
| Self-report (questionnaires) | Disability (ADLS-KOS) | √ | √ | √ | √ | ||
| General health (SF-36) | √ | √ | √ | √ | √ | ||
| Activity level (Tegner) | √ | √ | √ | √ | |||
| Overall ACL-R outcome | Disease specific measure (Lysholm) | √ | √ | √ | √ | ||
| Disease specific measure (IKDC) | √ | √ | √ | √ | |||
ACL-R, anterior cruciate ligament reconstruction; VAS, visual analogue scale; MRI, magnetic resonance imaging; ADLS-KOS, Activities of Daily Living Scale of the Knee Outcome Survey; SF-36, Medical Outcomes General Health Survey (SF-36); IKDC, International Knee Documentation Committee.
Figure 1.
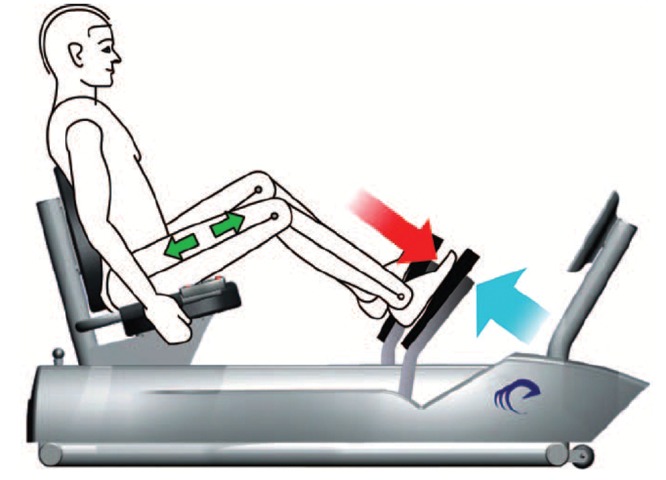
Two eccentric ergometers. As the pedals move toward the participant (to the right in these figures) resistance is applied to the pedals from approximately 20° to 60° of knee flexion in a closed kinetic-chain fashion. Because the magnitude of force produced by the motor exceeds that produced by the participant, the knee and hip extensors act eccentrically, creating negative work. (Reprinted from Marcus RL, Smith S, Morrell G, et al. Comparison of combined aerobic and high-force eccentric resistance exercise with aerobic exercise only for people with type 2 diabetes mellitus. Physical Therapy. 2008;88(11):1345-1354, with permission of the American Physical Therapy Association. This material is copyrighted, and any further reproduction or distribution is prohibited.)
Thirty-two of the 40 enrolled patients completed all aspects of the study.8 However, the most accurate representation for a descriptive analysis over time includes only those matched pairs who completed all testing. After dropouts and their matched pairs were eliminated, 14 pairs (or 28 subjects) remained. For this review, tables and figures demonstrating changes over time represent this subset of the entire sample.
Quadriceps Muscle Size
The major component of this research effort was to determine the magnitude of muscle size changes over time after ACL-R. Obtaining muscle volume measurements through the use of serial magnetic resonance images (MRI) at the pretraining (3 weeks following surgery) and post-training (15- and 52-week) time points following surgery provided valuable and somewhat surprising insights regarding muscle changes following ACL-R. From the time of the initial knee injury to the third postoperative week, when ECC training was initiated, a tremendous amount of quadriceps volume was lost: 25% to 33% of the involved quadriceps. While the greatest amount of atrophy occurred to the involved lower extremity, evidence from our case and clinical trial reports suggest the uninvolved quadriceps also atrophies 5% to 10%.5,7
From this severely atrophied starting point, a standard, accelerated rehabilitation program produced typical and respectable improvements. Quadriceps volume of the involved side increased approximately 8% in 12 weeks. During the subsequent 9 months of unsupervised rehabilitation and return to full activity, the quadriceps volume improved an additional 10%. In contrast, eccentrically biased rehabilitation produced a 25% increase in quadriceps volume after the 12-week training period and an additional 3% improvement during the subsequent 9 months of unsupervised rehabilitation and return to full activity. Therefore, the majority of quadriceps volume improvement occurred during the 3 months of formal rehabilitation in the ECC group, while the majority of the quadriceps volume improvement in the standard group occurred after formal rehabilitation was discontinued. As well, the overall magnitude of the quadriceps volume increase in the ECC group was more than 50% greater than the standard rehabilitation group at 1 year following ACL-R.8 The greater amount of quadriceps hypertrophy observed in the ECC group 1 year after surgery occurred independent of whether the ACL-R included a semitendinosus-gracilis surgical graft or a bone-patellar tendon-bone graft, though the overall magnitude of improvement was approximately 4% less in the bone-patellar tendon-bone cohort (Figure 2, Figure 3, and Table 2).
Figure 2.
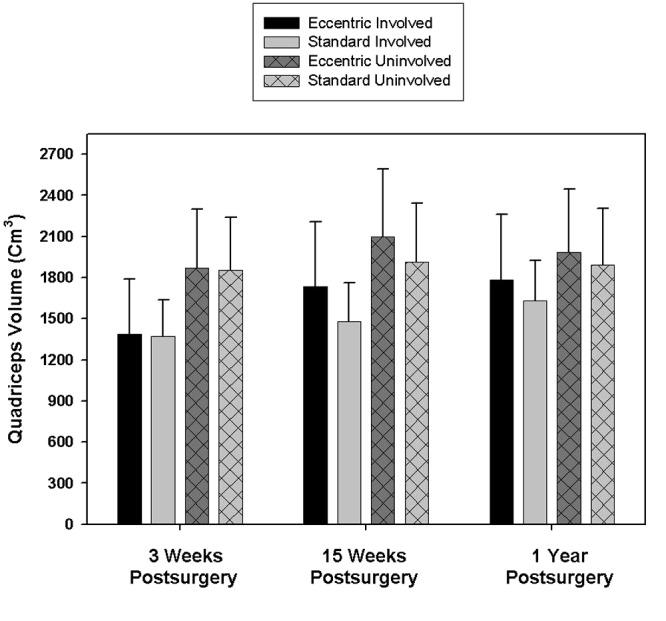
Comparison of quadriceps volume between the eccentric and standard rehabilitation groups of both the involved and uninvolved thighs at 3 weeks (pretraining), at 15 weeks (post-training), and at 1 year (post-training) after ACL reconstruction. Values represent the means (error bars = 1 SD).
Figure 3.
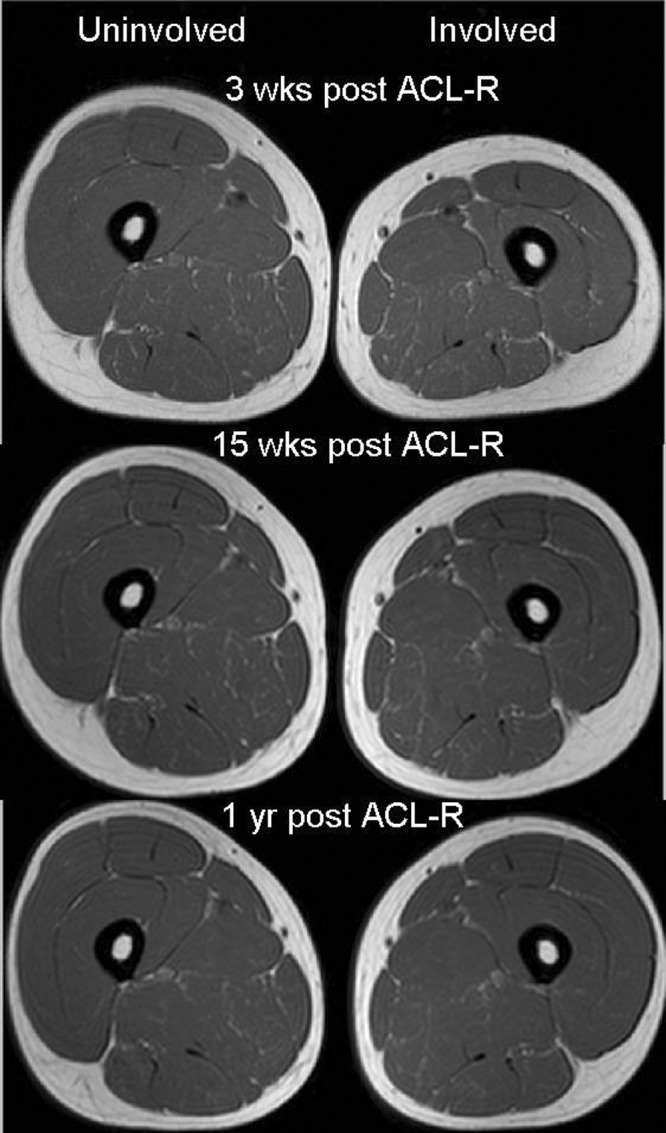
Mid-thigh, axial, T1-weighted magnetic resonance images of a subject assigned to the eccentric-exercise group. Quadriceps volume of the involved thigh was 30% less than the uninvolved thigh at 3 weeks post–ACL-R (pretraining). Quadriceps volume improved 28% at 15 weeks post–ACL-R (post-training) and 32% overall at 1 year post–ACL-R.
Table 2.
Pretraining, post-training, and 1-year muscle volume (cm3) for both rehabilitation groups and graft types.a
| Involved Limb | Uninvolved Limb | ||||||
|---|---|---|---|---|---|---|---|
| Muscle Graft Type | Rehabilitation Group | Pretraining | Post-training | 1 year | Pretraining | Post-training | 1 year |
| Quadriceps | |||||||
| Hamstring graft | Eccentric (n = 7) | 1444 ± 431 | 1876 ± 519 | 1887 ± 549 | 1924 ± 455 | 2098 ± 524 | 2015 ± 516 |
| Standard (n = 7) | 1287 ± 224 | 1386 ± 238 | 1534 ± 284 | 1711 ± 338 | 1719 ± 347 | 1716 ± 346 | |
| Patellar tendon graft | Eccentric (n = 7) | 1333 ± 400 | 1590 ± 416 | 1681 ± 409 | 1817 ± 427 | 2101 ± 501 | 1949 ± 450 |
| Standard (n = 7) | 1459 ± 288 | 1572 ± 311 | 1726 ± 294 | 2001 ± 399 | 2106 ± 440 | 2069 ± 418 | |
| Both grafts combined | Eccentric (n = 14) | 1388 ± 403 | 1733 ± 476 | 1784 ± 477 | 1870 ± 428 | 2099 ± 492 | 1982 ± 466 |
| Standard (n = 14) | 1374 ± 264 | 1479 ± 283 | 1630 ± 295 | 1856 ± 385 | 1913 ± 430 | 1893 ± 412 | |
| Gluteus Maximus | |||||||
| Hamstring graft | Eccentric (n = 7) | 574 ± 166 | 701 ± 178 | 707 ± 168 | 676 ± 206 | 739 ± 214 | 718 ± 211 |
| Standard (n = 7) | 574 ± 132 | 627 ± 131 | 666 ± 169 | 640 ± 135 | 633 ± 140 | 659 ± 180 | |
| Patellar tendon graft | Eccentric (n = 7) | 555 ± 209 | 714 ± 279 | 680 ± 223 | 610 ± 211 | 681 ± 221 | 657 ± 219 |
| Standard (n = 7) | 684 + 155 | 748 ± 129 | 774 ± 167 | 745 ± 154 | 769 ± 146 | 786 ± 168 | |
| Both grafts combined | Eccentric (n = 14) | 565 ± 182 | 707 ± 225 | 694 ± 190 | 643 ± 203 | 710 ± 211 | 688 ± 209 |
| Standard (n = 14) | 629 ± 150 | 688 ± 140 | 720 ± 171 | 693 ± 159 | 702 ± 154 | 722 ± 180 | |
| Hamstrings | |||||||
| Hamstring graft | Eccentric (n = 7) | 651 ± 170 | 676 ± 174 | 692 ± 169 | 731 ± 193 | 745 ± 186 | 752 ± 184 |
| Standard (n = 7) | 590 ± 137 | 604 ± 123 | 634 ± 134 | 662 ± 138 | 675 ± 145 | 687 ± 148 | |
| Patellar tendon graft | Eccentric (n = 7) | 650 ± 173 | 685 ± 182 | 694 ± 157 | 684 ± 150 | 699 ± 168 | 696 ± 150 |
| Standard (n = 7) | 708 ± 131 | 757 ± 154 | 775 ± 174 | 786 ± 154 | 792 ± 171 | 794 ± 176 | |
| Both grafts combined | Eccentric (n = 14) | 649 ± 143 | 680 ± 171 | 693 ± 157 | 707 ± 168 | 722 ± 172 | 724 ± 164 |
| Standard (n = 14) | 651 ± 165 | 680 ± 156 | 705 ± 166 | 724 ± 154 | 734 ± 164 | 740 ± 166 | |
| Gracilis | |||||||
| Hamstring graft | Eccentric (n = 7) | 83 ± 27 | 67 ± 22 | 62 ± 25 | 109 ± 32 | 110 ± 30 | 112 ± 30 |
| Standard (n = 7) | 74 ± 16 | 62 ± 14 | 54 ± 12 | 92 ± 17 | 93 ± 18 | 92 ± 17 | |
| Patellar tendon graft | Eccentric (n = 7) | 82 ± 22 | 89 ± 22 | 86 ± 19 | 87 ± 21 | 88 ± 22 | 88 ± 22 |
| Standard (n = 7) | 107 ± 22 | 111 ± 26 | 107± 26 | 111 ± 24 | 111 ± 22 | 110 ± 24 | |
| Both grafts combined | Eccentric (n = 14) | 82 ± 23 | 78 ± 24 | 74 ± 25 | 98 ± 28 | 100 ± 22 | 100 ± 28 |
| Standard (n = 14) | 91 ± 25 | 86 ± 32 | 80 ± 34 | 102 ± 22 | 102 ± 22 | 101 ± 22 | |
Values are given as mean and standard deviation. Pretraining magnetic resonance images were obtained 3 weeks (mean, 22.9 ± 3.9 days) after surgery. Post-training images were obtained 15 weeks (mean, 107.6 ± 7.7 days) after surgery. The images taken for the 1-year measurements were obtained a mean of 368.1 ± 18.2 days after surgery.
Gluteus Maximus Muscle Size
Because the synergistic relationship between the quadriceps and gluteus maximus for lower extremity extension support is evident in many activities, such as landing from a jump or performing a cutting maneuver, we also described muscle size changes in the gluteus maximus. While the intent was to focus on an ECC intervention designed to overload the quadriceps, it became obvious that the closed-chain intervention produced overload to both knee and hip extensors, as subjects frequently reported muscle soreness in the gluteal region as a result of postoperative rehabilitation. Therefore, a muscle volume evaluation of the distal portion of the gluteus maximus beginning from the superior border of the femoral head was included.5
It was interesting that improvements of gluteus maximus size basically mirrored improvements of quadriceps size for both the ECC and standard rehabilitation groups. Large gains were observed during the 3-month formal rehabilitation training period in the ECC group, while most gains in the standard group were observed after the formal 3-month period was completed. Overall gluteus maximus volume improvement from 3 weeks after surgery (pretraining) to 1 year after surgery was significantly greater—more than 50%—in the ECC group (Table 2).8
The possibility that the ACL-R graft type might also have an impact on muscle size also was explored. In the ECC group the quadriceps and gluteus maximus improved approximately 27% and 22%, respectively, in the semitendinosus-gracilis cohort compared to 20% and 29%, respectively, in the bone-patellar tendon-bone cohort.5 It is possible that patients may have adopted different strategies to complete the ECC exercise training (ie, a greater hip extensor movement control strategy with the bone-patellar tendon-bone graft procedure in attempts of alleviating potential stress and discomfort in the patellar tendon). Further research would be needed to investigate that hypothesis.
Gracilis and Hamstring Muscle Size
No apparent differences were observed between the ECC and standard rehabilitation groups at any time period for hamstring and gracilis volume changes.5,8 Realize that the tested cohort was small (n = 28), and that a sample size estimate was based on improvement of quadriceps muscle volume (not for gracilis or hamstring volume). Therefore, a difference might have been found in the gracilis and hamstring muscles had the tested cohort been larger. Additionally, differential volume changes were observed depending on graft type. Hamstring volume on the involved side was approximately 2% to 3% less (patellar tendon graft) and 7% to 8% less (semitendinosus-gracilis graft) 1 year after surgery (Table 2). Gracilis volume in the semitendinosus-gracilis graft group (ECC and standard group combined) deteriorated over time. Reductions in gracilis volume of 22% were already evident 3 weeks after ACL-R. This deficit was approximately 37% at 15 weeks and 44% at 1 year after surgery. Although deficits in hip adductor strength have been reported after this surgical procedure,10 it is unknown whether this results in functional deficits or whether a resistance training intervention could alter this downward spiral in gracilis volume following ACL-R with the semitendinosus-gracilis graft.
Strength, Performance, and Self-Report/Disease-Specific Measures
Strength and hop testing performance abilities are common outcome measures after ACL-R. It is common to see precipitous declines in both strength and performance after 3 months of formal rehabilitation following ACL-R. By 1 year after surgery, however, these values typically reach or even exceed preoperative values.1,3,24 This same pattern was observed for those in the standard rehabilitation group. In contrast, values for strength and hopping reached or exceeded preoperative levels in the ECC group after 3 months of formal postoperative rehabilitation and greatly exceeded preoperative levels 1 year following ACL-R. Both groups improved in a similar fashion after the 12-week intervention period (Figures 4 and 5).
Figure 4.
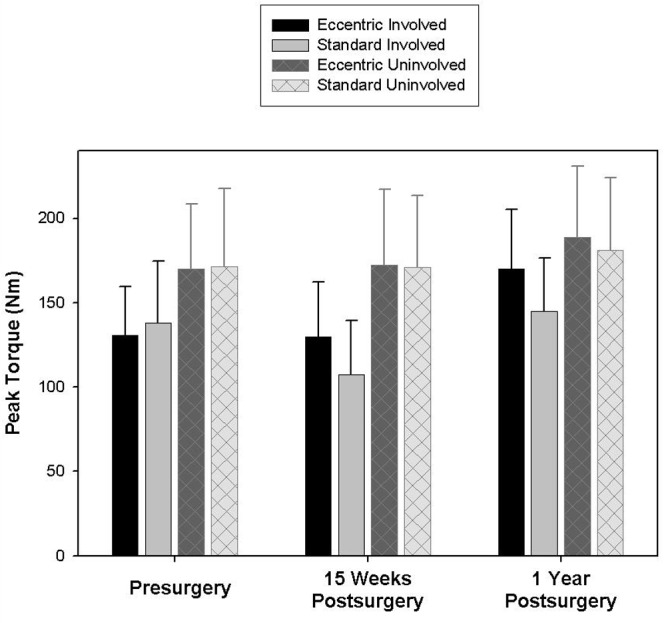
Comparison of quadriceps strength (isokinetic peak torque) between the eccentric and standard rehabilitation groups of both the involved and uninvolved thighs before ACL reconstruction, and at 15 weeks (post-training) and at 1 year (post-training) after surgery. Values represent the means (error bars = 1 SD
Figure 5.
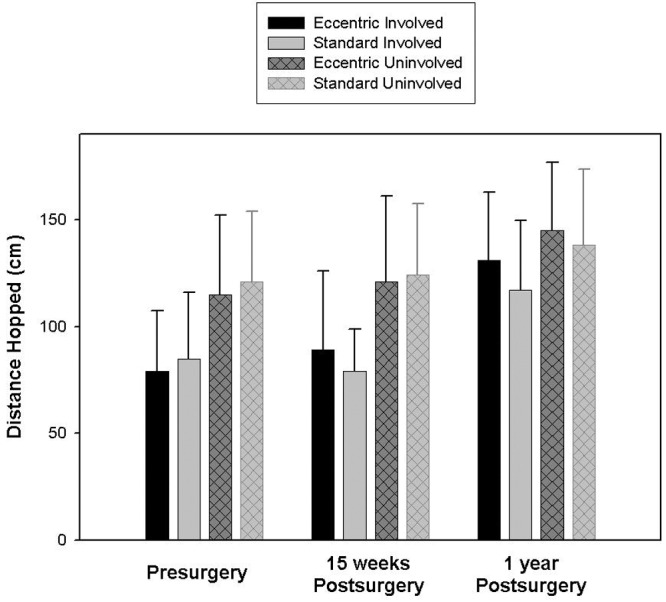
Comparison of one leg hopping distance between the eccentric and standard rehabilitation groups of both the involved and uninvolved lower extremities before anterior cruciate ligament reconstruction, and at 15 weeks (post-training) and at 1 year (post-training) after surgery. Values represent the means (error bars = 1 SD).
Despite the positive effect of ECC training on strength and hopping at 1 year after ACL-R, all patients in both groups scored equally well on a variety of disease-specific, outcome, activity, and general health surveys.5,6,8 Scores between the ECC and standard-rehabilitation groups were within 1 point of each other on each of the following scales: Lysholm: mean 93 ± 4.5; Activities of Daily Living Scale of the Knee Outcome Survey: mean 93.6 ± 5.4; International Knee Documentation Committee (IKDC): mean 88.9 ± 7.1; and Medical Outcomes General Health Survey (SF-36): mean 87.4 ± 5.0, Tegner: mean 6.2 ± 1.1.
Safety
Establishing the safety and feasibility is of utmost importance to any intervention applied after ACL-R. Pain, knee effusion, injury recurrence, and instability rates are measures of knee joint safety in research following ACL-R. There were no differences between rehabilitation groups in any of these safety measures during our 1-year study period. The injury recurrence rate (2 subjects in each group [4/40]; 10% overall) was, however, somewhat high in our sample. While conclusive statements cannot be made, it does not appear that either rehabilitation program contributed to this recurrence rate. One subject in the standard-rehabilitation group reinjured his knee 4 months after ACL-R while playing soccer. The other 3 traumatic reinjury episodes occurred 7 to 11 months after reconstruction. Knee stability outcomes were within acceptable standards for both groups 1 year after ACL-R (mean/range: 1.7 mm/0-5.0 mm [ECC group] 1.9 mm/0-4.5 mm [standard group] side-to-side difference using KT-1000 manual maximum measurements).
It is worth emphasizing that extreme care was exerted by the rehabilitation specialists in implementing this ECC resistance program; safety was always the top priority. Eccentric resistance training, due to the potential for high force generation, may be unsafe for certain patients. This concern excluded some subjects from participation (ie, those with vertical longitudinal meniscal tears requiring repair or those with significant (≥1cm) articular cartilage lesions observed during arthroscopy). Eccentric training on the ergometers was performed from approximately 20° to 60° of knee flexion, effectively minimizing the possibility of a knee hyperextension injury. Increases in the intensity of the ECC loading were carefully titrated during the course of training. Subjects began at a “very, very light” intensity of exercise based on the Borg rating of perceived exertion scale.23 Subjects could gradually progress in exercise duration and intensity only if a favorable individual response to exercise occurred (ie, absence of increased knee pain, effusion, excessive fatigue, etc). Eccentric exercise sessions were initially scheduled 3 times per week during the training period. The average number of sessions completed was 31 out of 36 potential sessions (range: 29-36). As the intensity of resistance training increased, several subjects reported increased muscle fatigue (typically after 8 to 9 weeks of training). In such cases, the frequency of ECC training was lowered to 2 times per week. Given these stringent criteria, it appears an ECC intervention can be applied with reasonable assurance that joint and graft safety is maintained, similar to standard rehabilitation.
Clinical Application of Eccentric Resistance Exercise
The quadriceps is the most important muscle group for lower extremity function following ACL-R. While a larger quadriceps does not guarantee a stronger muscle, a larger quadriceps does provide potential for greater force production. Likewise, greater force production from the quadriceps does not guarantee greater hopping distance, but it does provide a foundation through which performance can be optimized. Anecdotally, many rehabilitation programs are filled with a variety of “functional” exercises that are certainly beneficial but are not designed specifically for muscle overload. The emphasis should be placed on interventions that can safely and effectively overload muscle early during the rehabilitation process. Due to its inherent high loads, which induce high muscle forces, ECC resistance training may be ideally suited if applied in a gradual, progressive, and individualized manner. This does not imply that traditional resistance exercise should not be performed. In fact, a retrospective look at resistance training after the early 12-week intervention confirmed its importance. Quadriceps size in those who reported lower extremity weight lifting an average of 2 or more times per week after the formal 15-week rehabilitation period improved 23% and 34% overall in the standard and ECC groups, respectively, compared to 15% (standard) and 22% (ECC) in those who lifted weights fewer than 2 times per week. Whether an exercise is predominately ECC or concentric in nature, the intensity, frequency, and duration of progressive resistance training programs are all important factors in facilitating muscle recovery after ACL-R.
Despite the dearth of studies comparing the traditional resistance exercise component of a formal ACL-R postoperative rehabilitation program to an exclusively ECC resistance exercise, the beneficial effect of the eccentrically biased component is alluring. The eccentrically biased exercise induced high muscle forces in excess of the maximum isometric force, which is only possible during ECC (not isometric or concentric) contractions. If an exercise is designed to simply recover eccentrically the forces generated concentrically, then that exercise does not take advantage of the unique high force–producing properties of ECC contractions. The ECC exercise machine is a convenient and useful way to induce ECC contractions, but it is not the machine that produces these effects. One person in the standard rehabilitation group achieved results comparable to the ECC rehabilitation group.5 The quadriceps volume improvement in this female after the 12-week training period (39.3%) was more than twice that of any other individual in the standard group, and hamstring volume improvement (22.5%) was more than 10 times the average of the entire semitendinosus-gracilis graft cohort. Review of her exercise program showed that she was doing the concentric portion of the leg press and hamstring curl machine bilaterally and the ECC portion unilaterally. Furthermore, the resistance applied during the concentric portion was more than she could do with one leg alone. While other factors certainly could have contributed to her success, this subject used traditional weight training equipment in a nontraditional manner to take advantage of the unique high force-producing characteristics that ECC resistance training has to offer. While methods of performing ECC resistance exercise may differ, this type of training should be considered if the knee joint condition allows and when the goal of rehabilitation is muscle mass and strength improvement.
Limitations
Studies summarized in this review included a relatively small sample size and several subjects were lost to injuries and other miscellaneous issues by the 1-year follow-up, which limits generalizability. Because the primary outcome measures were improvements in muscle size, strength, and functional ability, a detailed description of specific weight lifting activities performed during the 12-week training period and during the subsequent 9 months of unsupervised rehabilitation would have been helpful. The rehabilitation program was also not rigidly controlled. Therapists followed the same postoperative guidelines; however, tailoring the rehabilitation program to best meet the individual needs of the patient was allowed. The weakness in this methodology is that it induces many confounding variables in exercise prescription and progression. The intent was to test the safety, feasibility, and efficacy of an ECC rehabilitation approach in a very typical ACL-R population setting. Maximizing quadriceps activation is also very important following ACL-R when the goal is improving quadriceps strength. The use of ice, neuromuscular electrical stimulation, or compressive wraps during the course of rehabilitation was not controlled. Knee circumference was not used to compare results in those with and without knee effusions. Quadriceps activation deficits via burst superimposition or interpolated twitch were not directly measured. It may be that employing a combination of quadriceps activation approaches in addition to progressive ECC resistance training might produce an additive effect on reducing quadriceps atrophy and weakness following ACL-R.
Conclusion
Following ACL injury and ACL-R, quadriceps and gluteus maximus atrophy of the involved lower extremity is severe. Quadriceps and gluteus maximus atrophy of the uninvolved side also occurs, but to a lesser extent. Compared to standard rehabilitation, adding an early 12-week ECC resistance training program 3 weeks (as part of formal rehabilitation) after ACL-R safely and dramatically improves quadriceps and gluteus maximus volume, strength, and hopping ability measured at 15 weeks and at 1 year following surgery.
Footnotes
References
- 1. Anderson JL, Lamb SE, Barker KL, Davies S, Dodd CA, Beard DJ. Changes in muscle torque following anterior cruciate ligament reconstruction: a comparison between hamstrings and patella tendon graft procedures on 45 patients. Acta Orthop Scand. 2002;73(5):546-552 [DOI] [PubMed] [Google Scholar]
- 2. Arangio GA, Chen C, Kalady M, Reed JF., 3rd Thigh muscle size and strength after anterior cruciate ligament reconstruction and rehabilitation. J Orthop Sports Phys Ther. 1997;26(5):238-243 [DOI] [PubMed] [Google Scholar]
- 3. Elmqvist LG, Lorentzon R, Johansson C, Langstrom M, Fagerlund M, Fugl-Meyer AR. Knee extensor muscle function before and after reconstruction of anterior cruciate ligament tear. Scand J Rehabil Med. 1989;21(3):131-139 [PubMed] [Google Scholar]
- 4. Feller JA, Webster KE. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31(4):564-573 [DOI] [PubMed] [Google Scholar]
- 5. Gerber JP, Marcus RL, Dibble LE, Greis PE, Burks RT, LaStayo PC. Effects of early progressive eccentric exercise on muscle structure after anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2007;89(3):559-570 [DOI] [PubMed] [Google Scholar]
- 6. Gerber JP, Marcus RL, Dibble LE, Greis PE, Burks RT, Lastayo PC. Safety, feasibility, and efficacy of negative work exercise via eccentric muscle activity following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2007;37(1):10-18 [DOI] [PubMed] [Google Scholar]
- 7. Gerber JP, Marcus RL, Dibble LE, Greis PE, LaStayo PC. Early application of negative work via eccentric ergometry following anterior cruciate ligament reconstruction: a case report. J Orthop Sports Phys Ther. 2006;36(5):298-307 [DOI] [PubMed] [Google Scholar]
- 8. Gerber JP, Marcus RL, Dibble LE, LaStayo PC. Effects of early progressive eccentric exercise on muscle size and function 1 year after anterior cruciate ligament reconstruction: a follow-up study. Physical Therapy Journal. In press [DOI] [PubMed] [Google Scholar]
- 9. Hamada M, Shino K, Horibe S, et al. Single- versus bisocket anterior cruciate ligament reconstruction using autogenous multiple-stranded hamstring tendons with EndoButton femoral fixation: a prospective study. Arthroscopy. 2001;17(8):801-807 [DOI] [PubMed] [Google Scholar]
- 10. Hiemstra LA, Gofton WT, Kriellaars DJ. Hip strength following hamstring tendon anterior cruciate ligament reconstruction. Clin J Sport Med. 2005;15(3):180-182 [DOI] [PubMed] [Google Scholar]
- 11. Hortobagyi T, Dempsey L, Fraser D, et al. Changes in muscle strength, muscle fiber size, and myofibrillar gene expression after immobilization and retraining in humans. J Physiol. 2000;524:293-304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jansson KA, Linko E, Sandelin J, Harilainen A. A prospective randomized study of patellar versus hamstring tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31(1):12-18 [DOI] [PubMed] [Google Scholar]
- 13. Jarvela T, Kannus P, Latvala K, Jarvinen M. Simple measurements in assessing muscle performance after an ACL reconstruction. Int J Sports Med. 2002;23(3):196-201 [DOI] [PubMed] [Google Scholar]
- 14. Johnson BL. Eccentric and concentric muscle training for strength development. Med Sci Sports Exerc. 1972;April:111-115 [Google Scholar]
- 15. Jones DA, Rutherford OM. Human muscle strength training: the effects of 3 different regimens and the nature of the resultant changes. J Physiol. 1987;391:1-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Keays SL, Bullock-Saxton JE, Newcombe P, Keays AC. The relationship between knee strength and functional stability before and after anterior cruciate ligament reconstruction. J Orthop Res. 2003;21(2):231-237 [DOI] [PubMed] [Google Scholar]
- 17. LaStayo PC, Ewy GA, Pierotti DD, Johns RK, Lindstedt S. The positive effects of negative work: increased muscle strength and decreased fall risk in a frail elderly population. J Gerontol A Biol Sci Med Sci. 2003;58(5):M419-M424 [DOI] [PubMed] [Google Scholar]
- 18. LaStayo PC, Pierotti DJ, Pifer J, Hoppeler H, Lindstedt SL. Eccentric ergometry: increases in locomotor muscle size and strength at low training intensities. Am J Physiol Regul Integr Comp Physiol. 2000;278(5):R1282-R1288 [DOI] [PubMed] [Google Scholar]
- 19. Lindstedt SL, LaStayo PC, Reich TE. When active muscles lengthen: properties and consequences of eccentric contractions. News Physiol Sci. 2001;16:256-261 [DOI] [PubMed] [Google Scholar]
- 20. Lindstedt SL, Reich TE, Keim P, LaStayo PC. Do muscles function as adaptable locomotor springs? J Exp Biol. 2002;205(Pt 15):2211-2216 [DOI] [PubMed] [Google Scholar]
- 21. Mattacola CG, Perrin DH, Gansneder BM, Gieck JH, Saliba EN, McCue FC., 3rd Strength, functional outcome, and postural stability after anterior cruciate ligament reconstruction. J Athl Train. 2002;37(3):262-268 [PMC free article] [PubMed] [Google Scholar]
- 22. Meighan AA, Keating JF, Will E. Outcome after reconstruction of the anterior cruciate ligament in athletic patients. A comparison of early versus delayed surgery. J Bone Joint Surg Br. 2003;85(4):521-524 [DOI] [PubMed] [Google Scholar]
- 23. Noble BJ, Borg GA, Jacobs I, Ceci R, Kaiser P. A category-ratio perceived exertion scale: relationship to blood and muscle lactates and heart rate. Med Sci Sports Exerc. 1983;15:523-528 [PubMed] [Google Scholar]
- 24. Risberg MA, Holm I, Steen H, Eriksson J, Ekeland A. The effect of knee bracing after anterior cruciate ligament reconstruction. A prospective, randomized study with 2 years’ follow-up. Am J Sports Med. 1999;27(1):76-83 [DOI] [PubMed] [Google Scholar]
- 25. Rosenberg TD, Franklin JL, Baldwin GN, Nelson KA. Extensor mechanism function after patellar tendon graft harvest for anterior cruciate ligament reconstruction. Am J Sports Med. 1992;20(5):519-525; discussion 525-516 [DOI] [PubMed] [Google Scholar]
- 26. Snyder-Mackler L, Ladin Z, Schepsis AA, Young JC. Electrical stimulation of the thigh muscles after reconstruction of the anterior cruciate ligament. Effects of electrically elicited contraction of the quadriceps femoris and hamstring muscles on gait and on strength of the thigh muscles. J Bone Joint Surg Am. 1991;73(7):1025-1036 [PubMed] [Google Scholar]