Abstract
Context:
Although disorders of the patellofemoral joint are common in the athlete, their management can be challenging and require a thorough physical examination and radiologic evaluation, including advanced magnetic resonance imaging techniques.
Evidence Acquisition:
Relevant articles were searched under OVID and MEDLINE (1968 to 2010) using the keywords patellofemoral joint, patellofemoral pain or patella and radiography, imaging, or magnetic resonance imaging, and the referenced sources were reviewed for additional articles. The quality and validity of the studies were assessed on the basis of careful analysis of the materials and methods before their inclusion in this article.
Results:
Physical examination and imaging evaluation including standard radiographs are crucial in identifying evidence of malalignment or instability. Magnetic resonance imaging provides valuable information about concomitant soft tissue injuries to the medial stabilizers as well as injuries to the articular cartilage, including chondral shears and osteochondral fractures. Quantitative magnetic resonance imaging assessing the ultrastructure of cartilage has shown high correlation with histology and may be useful for timing surgery.
Conclusions:
Evaluation of patellofemoral disorders is complex and requires a comprehensive assessment. Recent advancements in imaging have made possible a more precise evaluation of the individual anatomy of the patient, addressing issues of malalignment, instability, and underlying cartilage damage.
Keywords: Patellofemoral joint, patellofemoral pain, chondromalacia patella, Magnetic Resonance Imaging
Patellofemoral disorders are some of the most common problems seen in the orthopaedic surgeon’s office, affecting as many as 30% of athletes in some sports.2 Despite their frequency, these problems can be some of the most challenging and often frustrating to both the patients and the clinicians. Over the past decade, we have made significant advances in this field, including improved imaging and newer and more anatomic surgical techniques.1
Many terms have been given to these patellofemoral problems—such as “runner’s knee,” chondromalacia patella, anterior knee pain, and patellofemoral syndrome—none of which accurately describes the underlying pathology. To better define the problem, it is necessary to understand both the anatomy and the biomechanics involved in this enigmatic joint.
The patella engages and tracks within the trochlea, the distal end of the femur. The hyaline cartilage in most joints is 2 to 3 mm thick. However, the patellar cartilage is 4 to 5 mm thick, accommodating the enormous forces it transmits during daily activity. The biomechanics of the patellofemoral joint are complex; stability of this joint is dictated by its unique shape as well as the bony and surrounding soft tissue restraints. The distal femur forms a track for the patella (the trochlea), which is elevated on its lateral side to help maintain stability and resist lateral translation of the patella. Warren and Marshall described the medial soft tissue restraints as 3 layers.43 The medial patellofemoral ligament (MPFL) forms part of layer 2, and layers 1 and 2 converge anteriorly to form the medial retinaculum. The MPFL is the primary static restraint to lateral translation of the patella. It provides up to 60% of the force that resists lateral translation of the patella, with the medial patellomeniscal ligament providing up to 20%.9,12,37
The MPFL has received significant attention in the diagnosis of injury as well as its repair and/or reconstruction. The major dynamic stabilizer of the patellofemoral joint is the vastus medialis obliquus, which acts both dynamically and statically as its fascia merges with the fibers of the MPFL, essentially dynamizing this ligament.37 It is helpful to separate patellar overuse from instability; classic patellofemoral overload is a multifactorial problem.
Overuse Disorders
Overuse injuries of the patellofemoral joint are common with activities that cause repeated knee flexion and extension. As the patella tracks in the trochlea, it tilts and rotates, changing the location and degree of loading.22 The alignment of the lower limb plays an intricate role in the balance of this joint; small alterations can disrupt the fine balance, resulting in pain and dysfunction. Problems at the foot (pes planus), the leg (tibial torsion), and the hip (femoral anteversion) can all cause lateral patellar compression syndrome.18 Pain may be seen with activity but may persist after the activity has been stopped. Pain caused by the increased loads often inhibits the quadriceps, which can aggravate the patient’s symptoms.
Trauma
Traumatic injuries to the patellofemoral joint can be the result of direct impact or instability, and both can cause damage to the articular cartilage (Figure 1). With direct impact, the damage is usually a crush injury, often central. With traumatic dislocation or subluxation, the injury is usually a shear-type injury, most often seen on the medial facet of the patella or along the lateral trochlea (“relocation injury”). During dislocation or subluxation of the patellofemoral joint, the medial stabilizers (MPFL) are often stretched or torn (Figure 2). Although these medial structures can heal, the stretch injury often compromises their integrity, allowing repeated episodes of instability to occur and putting the articular cartilage at increased risk for repeated damage.
Figure 1.
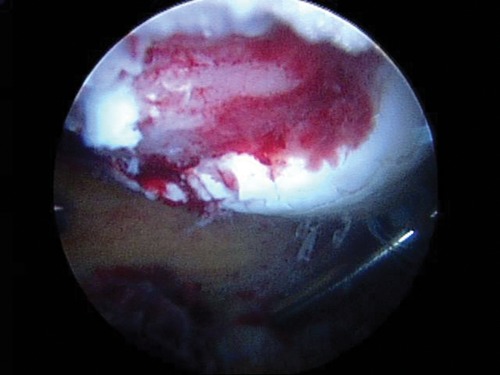
Arthroscopic image of a large cartilage defect in the patella.
Figure 2.
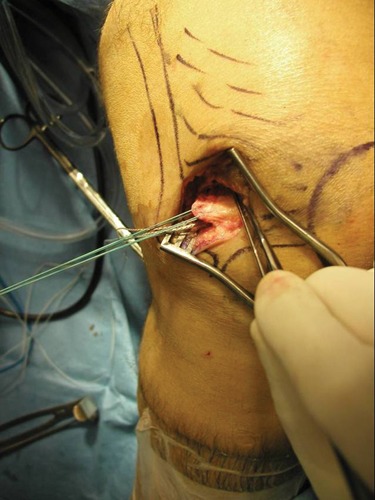
Intraoperative image of torn medial patellofemoral ligament off the femur during its repair.
Patellar Tendinitis
Patellar tendinitis is the result of chronic overload, usually at the inferior pole of the patella, and is most common with repetitive jumping sports, such as basketball and volleyball. Radiographic results are most often normal, but MRI reveals tendon thickening and changes in tendon signal (Figure 3).
Figure 3.
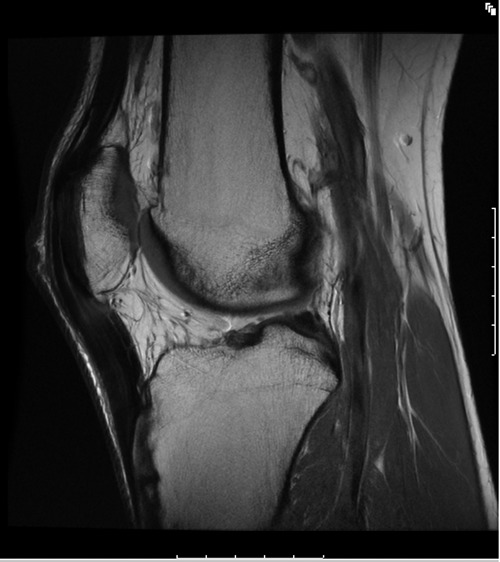
Sagittal proton density MRI of the knee (TR = 5067 milliseconds, TE = 25 milliseconds), 29-year-old male professional basketball player. Image shows thickening of the patellar tendon and intermediate signal intensity within the tendon indicative of patellar tendinitis.
Patellar Osteochondritis Dissecans
Osteochondritis dissecans (OCD) is a disease in which the underlying bone and its associated cartilage begin to separate from the adjacent articular surface (Figure 4). OCD is most commonly seen in the knee, and the most common location within the knee is the medial femoral condyle, whereas the least common is the patella. The cause of OCD lesions is not fully understood, although trauma and ischemia have both been implicated. OCD most commonly presents in the second and third decades of life and is more common in men than women. It is often asymptomatic and commonly an incidental finding on radiographs.
Figure 4.
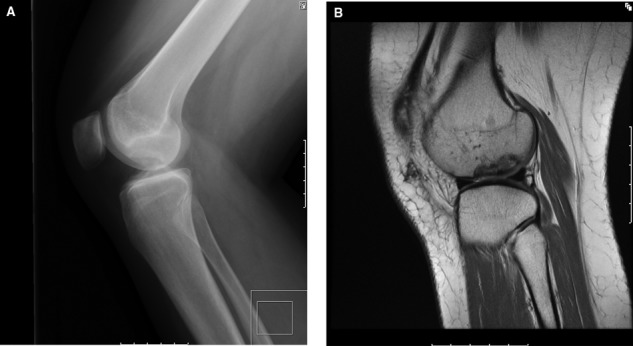
Lateral radiograph (A) and sagittal proton density MRI (TR = 4067 milliseconds, TE = 25 milliseconds) (B) demonstrate an OCD lesion in the lateral femoral condyle in a 17-year-old girl.
Imaging
Radiographs
Imaging of the patellofemoral joint begins with standard radiographs of the knee, including anteroposterior, lateral, and axial views. The anteroposterior view is the least valuable in evaluating the patellofemoral compartment, but it can demonstrate multipartite patellae as well as gross patella alta or baja.
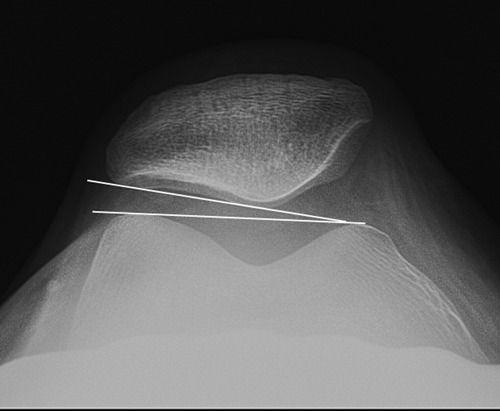
The height of the patella with respect to the tibia can be assessed on the lateral radiograph, with its implications for patella alta or baja. The ratio of the length of the patellar tendon to the longest diagonal length of the patella (Insall-Salvati ratio) is approximately 1.0; discrepancy of more than 20% to 30% is abnormal (Figure 5).23,24 Grelsamer and Meadows proposed a modified Insall-Salvati ratio in which the length of the patellar articular surface is used instead of the longest length of the patella.20 Blackburne and Peel used the distance between the inferior margin of the articular surface of the patella and a line drawn through the tibial plateaus as a reference, instead of the length of the patellar tendon.5
Figure 5.
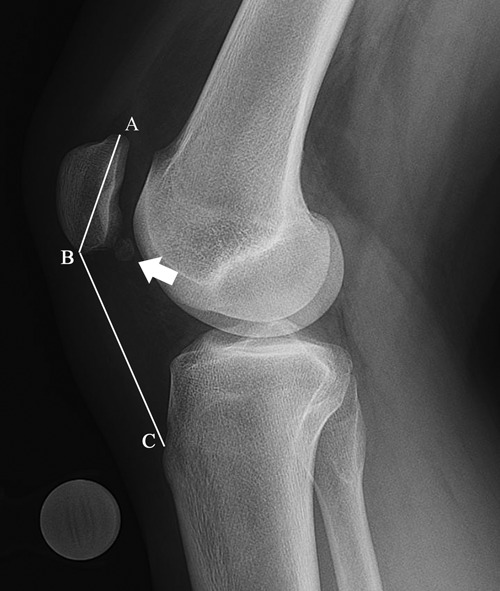
Lateral radiograph demonstrating the Insall-Salvati ratio, the ratio of the length of the patellar tendon (BC) to the longest length of the patella (AB). The ratio is elevated in this 15-year-old girl, indicative of patella alta. The patient also had an ossified body (arrow) adjacent to the patella, related to a prior osteochondral injury.
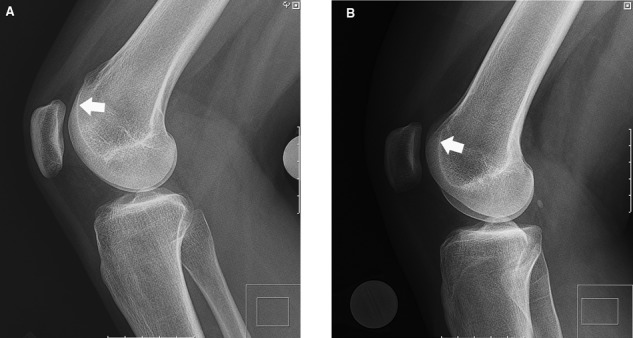
The lateral radiograph can also be used to assess patellar tilt. In a true lateral view such that the posterior medial and lateral femoral condyles precisely overlap, the median ridge of the patella normally projects posterior to the lateral facet of the patella (Figure 6A). With increasing degrees of lateral patellar tilt, the median ridge will superimpose on and eventually project anterior to the lateral facet (Figure 6B and 6C).18,27,32 Murray and colleagues reported a higher sensitivity of detecting patellar malalignment on the lateral radiograph compared with the axial view.32
Figure 6.

Lateral radiographs showing (A) normal relationship of the median ridge (arrow) and lateral facet (arrowhead) of the patella, (B) median ridge (arrow) superimposed on the lateral facet (arrowhead), and (C) median ridge (arrow) projecting anterior to the lateral facet (arrowhead).
The morphology of the trochlea and the degree of trochlear dysplasia may be more accurately depicted on the lateral radiograph than on the axial view.18,28 The depth of the trochlea can be measured on the lateral radiograph, with a shallow trochlea being indicative of trochlear dysplasia (Figure 7). Malghem and Maldague showed that trochlear depth less than 5 mm was a risk factor for patellar instability.28 Dejour et al described an indication of trochlear dysplasia as the appearance of the floor of the trochlea when it crosses the anterior margin of the medial and lateral femoral condyles (“crossing sign”) (Figure 8).11 “Supratrochlear spur” and “double contour” are other signs of trochlear dysplasia that can be seen on a lateral radiograph (Figure 8).10,42 Patellar subluxation will alter the positions of the articular surfaces on the lateral view, making joint space assessment inaccurate.25
Figure 7.
Lateral radiographs showing (A) decreased depth of the proximal trochlea (arrow) compared to (B) normal depth (arrow).
Figure 8.

Lateral knee radiograph of a 32-year-old woman with prior patellar realignment and retinacular reconstruction demonstrating features of trochlear dysplasia, including the “crossing sign” (curved arrow), “supratrochlear spur” (arrow), and “double contour” (arrowhead). Note that this patient had undergone prior medial patellofemoral ligament reconstruction, with the femoral tunnel placed excessively anteriorly.
Axial radiographs of the patellofemoral joint (“sunrise” views) are useful for demonstrating the general morphology of the patella, including the different Wiberg types based on the lengths of the medial and lateral facets,45 as well as the size of the patella with respect to the trochlea (Figure 9).18 Techniques described by Merchant et al30 and Laurin et al26 are the 2 most widely used.
Figure 9.
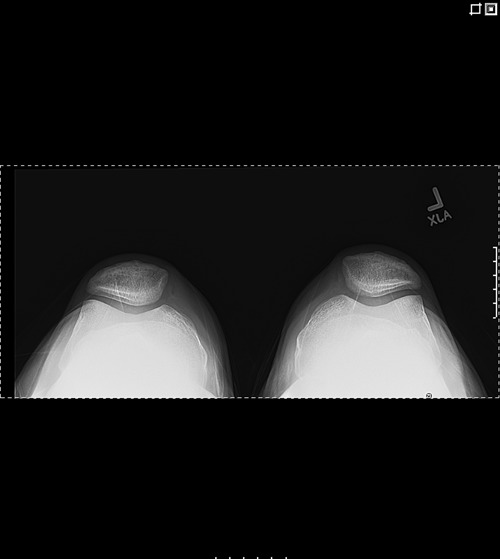
Axial (Merchant) view of the knees demonstrating normal patellofemoral articulations.
The sulcus angle, as measured by lines connecting the anterior tips of the femoral condyles with the deepest point of the intercondylar sulcus, can be used to assess for trochlear dysplasia (Figure 10). The average sulcus angle in normal knees is 138° to 142°,6,30 with a greater angle suggesting dysplasia and risk factor for patellar instability.11 The congruence angle is formed by a line bisecting the sulcus angle and a line drawn from the median ridge of the patella to the deepest point of the intercondylar sulcus (Figure 10).30 The congruence angle measures an average of −6° in normal subjects and is abnormal if it is greater than 16°, indicating patellar subluxation.30
Figure 10.
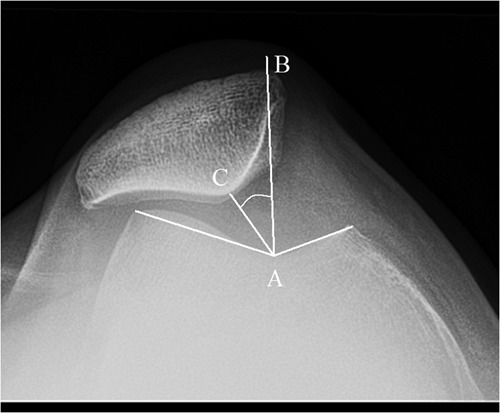
Axial radiograph of the knee in a 49-year-old woman demonstrating the sulcus angle as well as the congruence angle (CAB), composed of the line bisecting the sulcus angle (BA) and the line connecting the patellar median ridge to the trough of the trochlear sulcus (CA). In this patient, the congruence angle measures greater than +16 degrees, thus the patella is subluxated.
The lateral patellofemoral angle is formed by a line drawn along the lateral facet of the patella and a line connecting the anterior margins of the medial and lateral femoral condyles on an axial radiograph (Figure 11).26 This angle opens laterally in 97% of normal knees. With patellar subluxation, the lines lay parallel in 60%, and the angle opened medially in the remaining 40%.26 The lateral patellofemoral angle is a reflection of patellar tilt, and patellar subluxation may be more accurately assessed by Merchant congruence angle.18 The patellofemoral index is the ratio of the medial and lateral patellofemoral joint spaces on an axial radiograph at 20° of flexion (Figure 12).26 Relative widening medially is an indication of lateral patellar tilt, and a patellofemoral index greater than 1.6 is considered abnormal.26
Figure 11.
Axial radiograph demonstrating the lateral patellofemoral angle opening up laterally.
Figure 12.
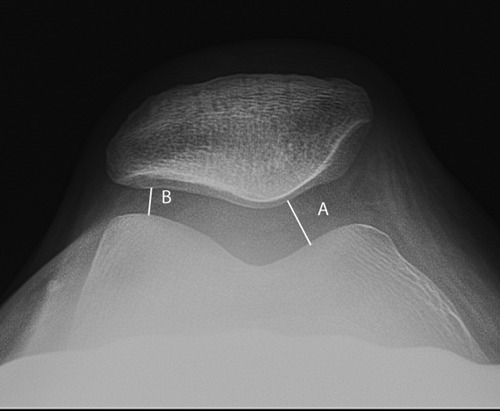
Axial radiograph demonstrating measurement of the medial (A) and lateral (B) interspaces. A patellofemoral index (A:B) greater than 1.6 is abnormal.
Computed Tomography
Computed tomography allows tomographic imaging through the patellofemoral joint without overlap of structures as in plain radiographs. On computed tomography, the patellar tilt angle can be measured between a line parallel to the lateral patellar facet and a line parallel to the posterior intercondylar line (Figure 13).39,40 The tibial tubercle–trochlear groove distance is measured by superimposing images at the level of the tibial tubercle and at the steepest portion of the trochlea (Figure 14). Distance of 15 to 20 mm is considered significant malalignment.8
Figure 13.
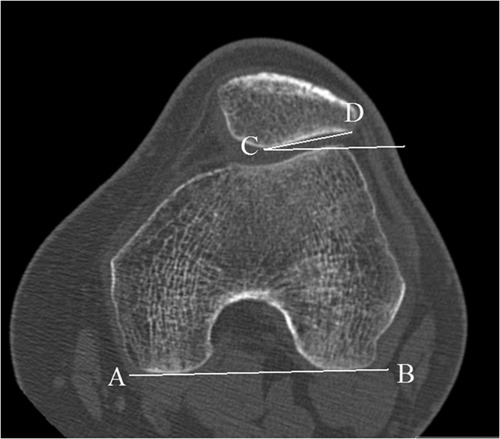
Axial computed tomography of the knee in a 35-year-old man demonstrating the patellar tilt angle measured with a line along the lateral patellar facet (CD) and a line parallel to the posterior intercondylar line (AB).
Figure 14.
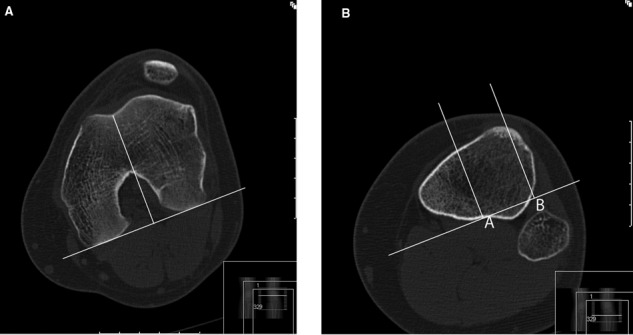
Tibial tubercle–trochlear groove (TT-TG) distance is measured by (A) first drawing a line from the trough of the trochlea perpendicular to the line connecting the posterior condyles. These lines are superimposed onto an image through the tibial tubercle (B), and the TT-TG distance is measured as that between the above-described line and the tibial tubercle (distance AB). In this patient, the TT-TG distance measured 25 cm, indicative of malalignment.
Studies of computed tomography scans with varying degrees of knee flexion concluded that a congruence angle greater than 0° at 10° of knee flexion indicates subluxation.39,40 Significant patellar tilt or subluxation by 20° of flexion should be considered malalignment.18 Scanning with and without contraction of the quadriceps can reveal additional information (Figure 15).21
Figure 15.
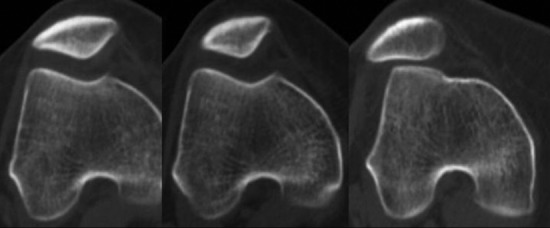
Computed tomography scan of the patellofemoral joint: from left to right, during 30° of knee flexion with quadriceps contraction, 30° of knee flexion without contraction, and full knee extension without contraction. The image demonstrates lateral subluxation of the patella during only full extension. (Image courtesy of Theodore Miller, MD)
By playing the computed tomography images as a cine loop, Stanford et al demonstrated lateral displacement of the patella during the terminal 10° to 20° of knee extension in a subgroup of their patients.41 Cine can demonstrate additional information about patellar tracking compared to individual images.14
Radionuclide Scintigraphy
Radionuclide scintigraphy (bone scans) using technetium-99m-labeled diphosphonates is a sensitive marker of bone turnover.3 In patients with anterior knee pain, increased radiotracer uptake can be seen in the patella or femoral trochlea before an abnormality is seen on radiographs (Figure 16).15
Figure 16.
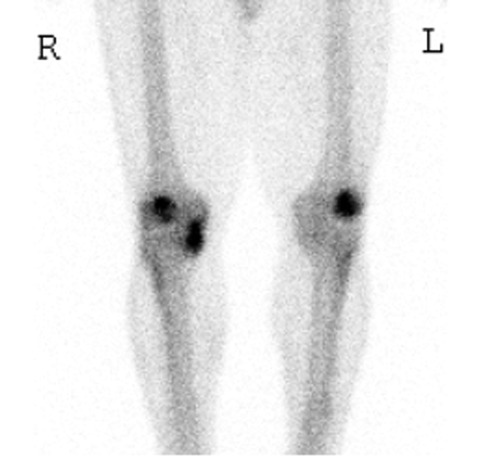
Bone scan of a 61-year-old woman demonstrates increased radiotracer uptake indicative of arthrosis involving the patellofemoral compartment of both knees as well as the medial compartment of the right knee.
Sonography
Sonography can evaluate the tendons and ligaments around the patella.4,17,34 In pediatric patients in whom the patella has not completely ossified, sonography may more accurately evaluate patellar positioning than radiography.29 The trochlear articular cartilage can also be visualized with the knee in flexion (Figure 17).36 However, the cartilage of the patella is difficult to evaluate secondary to the overlying bony patella. Nevertheless, the lack of ionizing radiation and the ability to perform a real-time evaluation make sonography a valuable problem-solving tool.
Figure 17.
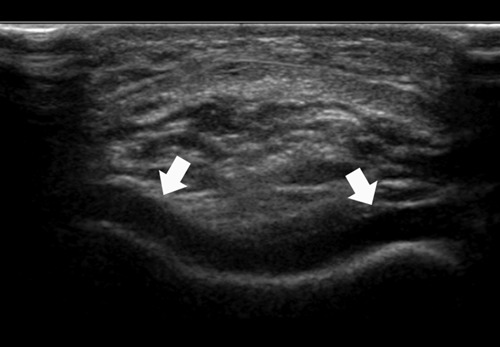
Ultrasound of the knee of an 8-year-old boy in short axis demonstrates uniform thickness of normal trochlear cartilage (arrows).
Magnetic Resonance Imaging
Multiplanar capability, lack of ionizing radiation, and superior soft tissue contrast make MRI an effective means by which to evaluate the painful patellofemoral joint. Standardized pulse sequences should include at least 1 series obtained with fat suppression, which “rescales” the contrast range, making bone marrow edema pattern and fluid collections more conspicuous (Figure 18). This also highlights the presence of an acute subluxation episode in a patient with chronic instability and helps to disclose areas of reactive bone marrow edema in the setting of patellofemoral osteoarthritis (Figure 19). Standardized cartilage-sensitive pulse sequencing is also recommended.35 The most commonly utilized cartilage techniques are proton density–weighted fast spin echo sequences, which are obtained with a longer repetition time and a moderate- or intermediate-weighted echo time, the latter of which is approximately 34 milliseconds at 1.5 T and 28 milliseconds at 3 T. These techniques accentuate the inherent magnetization transfer contrast that occurs in fast spin echo sequencing, producing the essential differential contrast between articular cartilage and fluid (Figure 20). Additional pulse sequences for assessment of cartilage include volumetric or 3-dimensional sequences, using either traditional fat-suppressed T1-weighted gradient echo or the more recently developed 3-dimensional fast spin echo techniques.7,13,35,38
Figure 18.

Sagittal fat-saturated T2-weighted sequence (TR = 3550 milliseconds, TE = 49 milliseconds) demonstrating characteristic bone marrow edema in the lateral femoral condyle and conspicuous posttraumatic joint effusion from acute patellar dislocation. Note the anterior extracapsular soft tissue edema (arrow).
Figure 19.
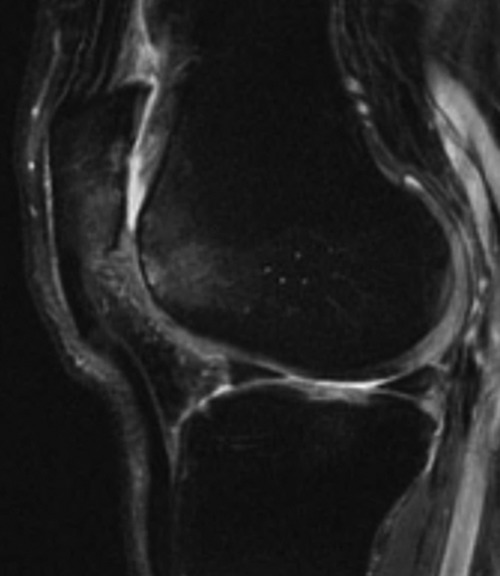
Sagittal fat-saturated T2-weighted sequence demonstrating reactive marrow edema in the patellofemoral compartment secondary to advanced patellofemoral osteoarthritis.
Figure 20.
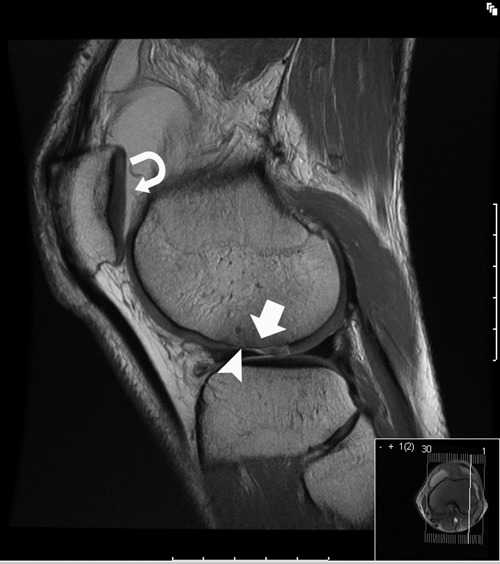
Sagittal proton density sequence (TR = 4400 milliseconds, TE = 24 milliseconds) demonstrating chondral shear injury of the lateral femoral condyle (arrow) related to patellar dislocation. Note the low signal intensity tidemark (arrowhead) indicative of intact subchondral bone. Proton density–weighted fast spin echo allows differential contrast between articular cartilage and fluid, as seen around the patellofemoral compartment (curved arrow).
In acute patellar dislocation, extracapsular soft tissue edema is typically localized at the anterior margin of the knee (Figure 18). A classic lateral patellar subluxation will result in a traumatic bone marrow edema pattern in the anterior portion of the lateral femoral condyle and the inferomedial portion of the patella (Figure 21). Careful scrutiny of the images is important to distinguish a traumatic chondral shear (Figure 22) from a frank osteochondral fracture (Figure 23). The distinction is made by the appearance of the low signal subchondral plate at the bone-cartilage interface (Figure 20). If absent, a bone fragment has been lost with the cartilage, which may be of sufficient size to warrant primary repair. Careful evaluation for loose bodies in the gutter, intercondylar notch, and posterior recess should also be made (Figure 24). Osteochondral fracture or chondral shear may occur either over the anterior portion of the condyle or the patella proper (Figure 24).
Figure 21.
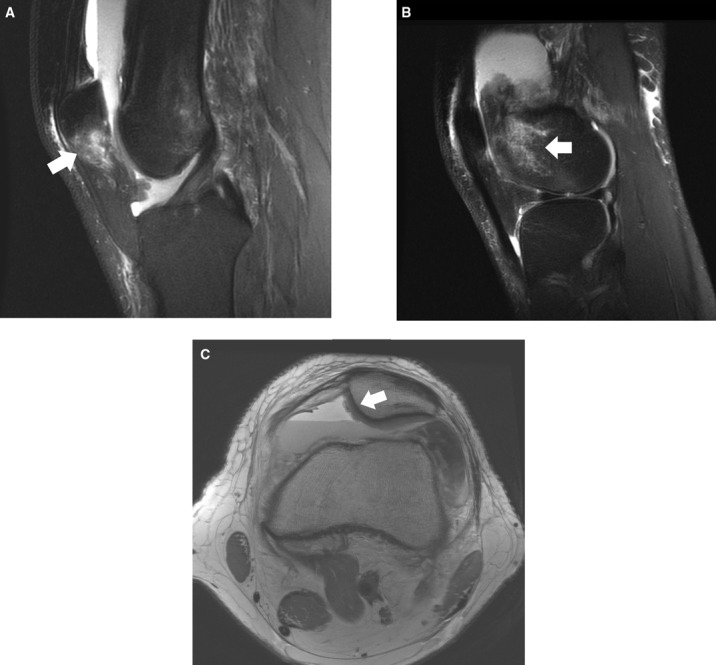
Sagittal fat-saturated T2-weighted sequences (TR = 5867 milliseconds, TE = 41 milliseconds) through the midline of the patella (A) and the lateral femorotibial compartment (B) of a 22-year-old man with patellar dislocation 10 days prior. The sequences demonstrate the characteristic bone marrow edema pattern involving the inferior pole of the patella and anterior lateral femoral condyle (arrows). C, axial proton density sequence (TR = 4033 milliseconds, TE = 25 milliseconds) through the midpatella demonstrates a chondral injury to the medial patellar facet (arrow) with hemarthrosis.
Figure 22.
Axial proton density images (TR = 5858 milliseconds, TE = 25 milliseconds) of the knee in a 13-year-old boy demonstrate (A) traumatic chondral shear of the lateral aspect of the trochlea (arrow) in the setting of a hypoplastic trochlear sulcus, with (B) the loose chondral fragment (arrow) in a popliteal cyst.
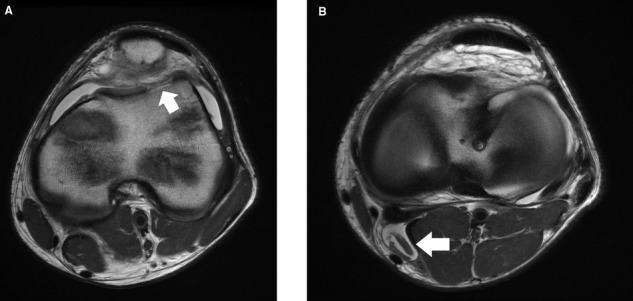
Figure 23.
(A) sagittal proton density sequence (TR = 3750 milliseconds, TE = 25 milliseconds) of the lateral aspect of the knee of a 16-year-old girl demonstrates an osteochondral fracture of the anterior lateral femoral condyle (arrow). (B) axial proton density sequence (TR = 6167 milliseconds, TE = 24 milliseconds) shows the same fracture (arrow), with the osteochondral fragment adjacent to it in the lateral recess of the joint, as well as another osteochondral fracture involving the medial patellar facet (arrowhead). Note the lack of the low signal intensity tidemark, indicative of osteochondral injury.
Figure 24.
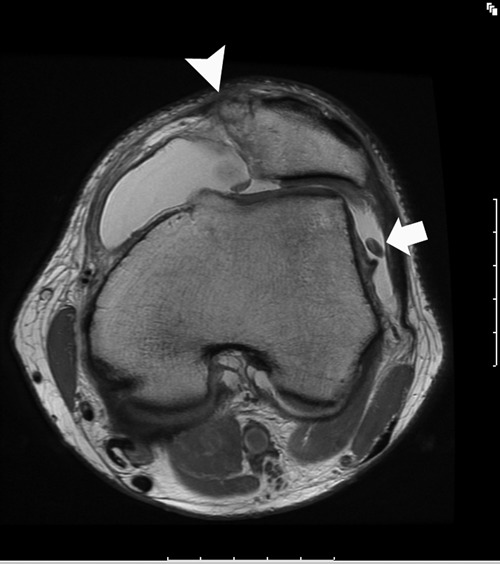
Axial proton density sequence (TR = 3800 milliseconds, TE = 23 milliseconds) demonstrating chondral loose body in the lateral gutter of the joint (arrow) in a patient who has sustained an avulsion fracture of the medial patella and a tear of the medial retinaculum (arrowhead).
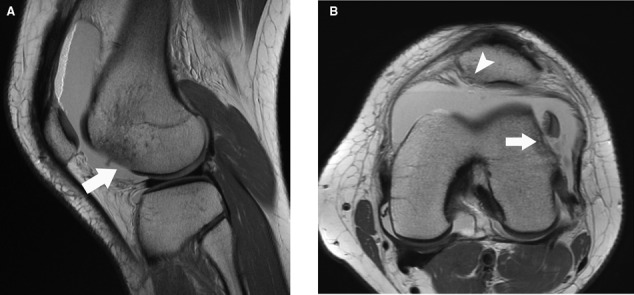
A study of 23 patients with patellar dislocation noted that 87% of patients had tears of the femoral insertion of the MPFL, with edema extending to the vastus medialis muscle and associated bone impaction injury (Figure 25).37 A correlative study between MRI and open surgical evaluation of patellar dislocations in 27 knees with acute injury demonstrated that 13 of 16 knees (82%) had tears at the femoral margin.33 Conversely, a larger study involving 81 patients noted that 67% of the 82 MRI examinations showed retinacular disruption at the patella (Figure 24) and 30% in the midsubstance.16 Forty-eight percent of examinations showed more than 1 injury site in the medial stabilizers.16 Acute patellar dislocation in 44 children demonstrated MPFL injury, with isolated patellar detachment in 62% and at the femoral origin in only 12% (Kepler, et al, unpublished data presented at the 2010 annual meeting of the Pediatric Orthopaedic Society of North America). There is considerable variability in the location of MPFL and retinacular injury, and careful inspection of images in all 3 planes is warranted (Figure 26).
Figure 25.
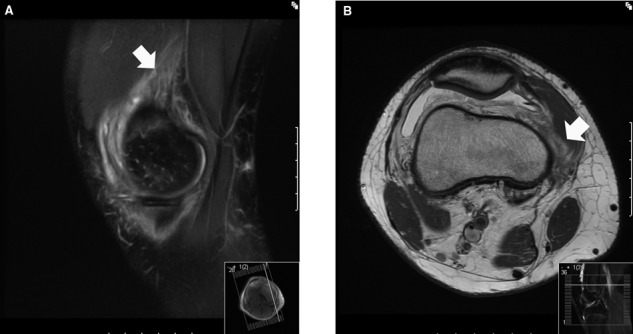
(A) Sagittal fat-saturated T2-weighted sequence (TR = 3683 milliseconds, TE = 42 milliseconds) and (B) axial proton density sequence (TR = 5017 milliseconds, TE = 25 milliseconds) in a patient with recent patellar dislocation demonstrate edema extending into the vastus medialis muscle (arrows).
Figure 26.
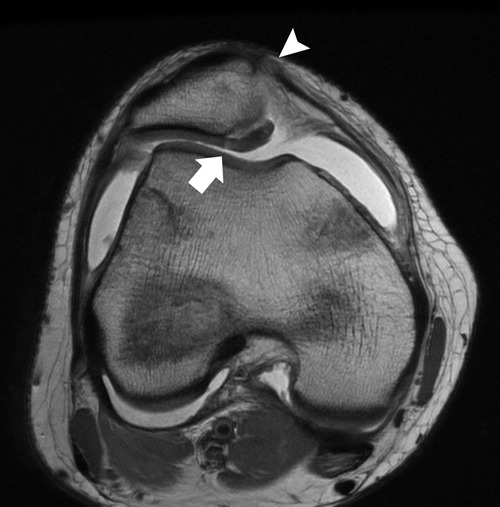
Axial proton density sequence (TR = 4383 milliseconds, TE = 26 milliseconds) through the patella in a 15-year-old girl who sustained a patellar dislocation demonstrates an osteochondral fracture of the medial patellar facet (arrow) and a tear of the medial retinaculum and medial patellofemoral ligament at the patellar attachment (arrowhead).
Chronic Patellar Pain
Early osteoarthritis manifests as increased signal intensity in the cartilage, sometimes associated with a superficial blister (Figure 27). Progressive degeneration leads to loss of cartilage thickness, with subtle changes in the superficial layer of cartilage known as the lamina splendens (Figure 28). Progressive cartilage loss may then be seen, eventually extending down to subchondral bone. Evaluation of the tidemark or cartilage-bone interface is important to discern areas of proud bone formation and sclerosis, which may have implications for subsequent repair (Figure 29).
Figure 27.

Axial proton density sequence (TR = 5700 milliseconds, TE = 26 milliseconds) through the patella in a 25-year-old man demonstrates blisters of cartilage over the median ridge of the patella (arrow) as well as the medial patellar facet (arrowhead). Note the well-delineated low signal line along the superficial margin of the lateral patellar facet, representing the lamina splendens.
Figure 28.

Axial proton density sequence (TR = 5900 milliseconds, TE = 25 milliseconds) showing intact lamina splendens over the lateral margin of the medial patellar facet (arrow), as well as early degeneration over the medial margin (arrowhead).
Figure 29.

Axial proton density sequence (TR = 4133 milliseconds, TE = 24 milliseconds) showing proud subchondral bony remodeling (arrow) and adjacent subchondral sclerosis (arrowhead) along the lateral trochlear sulcus.
The structural integrity of articular cartilage depends on the components of the extracellular matrix. Compressive strength is afforded by the negatively charged hydrophilic glycosaminoglycans of the proteoglycan macromolecules, and tensile strength is afforded by the long length:thickness ratio of the collagen fibrils.31 Proteoglycan content of articular cartilage may be targeted using several magnetic resonance (MR) techniques, including sodium imaging, which is typically performed at 3 T or 7 T and which requires special surface coils suitable for evaluating the resonant frequency of sodium.19 Owing to the special coil requirements as well as the specialized MR hardware and software requirements, sodium imaging is limited to a few research centers. Additional evaluation using delayed gadolinium-enhanced imaging of cartilage (dGEMRIC) requires a double dose of intravenous gadolinium tagged to a negatively charged salt, followed by a short period of exercise and delayed T1-weighted techniques, where T1 maps are obtained. In areas depleted of negatively charged glycosaminoglycan, there is an increased distribution of the negatively charged gadolinium salt.
Proteoglycan may also be assessed using T1 rho imaging.44 T1 rho is a pulse sequence that assesses interactions between macromolecules and free water; T1 rho has been highly correlated to histologic depletion of proteoglycan, as well as assessment of fixed charge density using sodium imaging as a standard.44 In addition, quantitative T2 mapping has been highly correlated to the orientation of the collagen.46 These quantitative magnetic resonance techniques permit identification of focal alterations in cartilage ultrastructure that precede morphologic loss of cartilage thickness (Figure 30). Longitudinal evaluation of such patients may help to time surgical operations aimed at delaying the progression of osteoarthritis, such as patellofemoral realignment.
Figure 30.
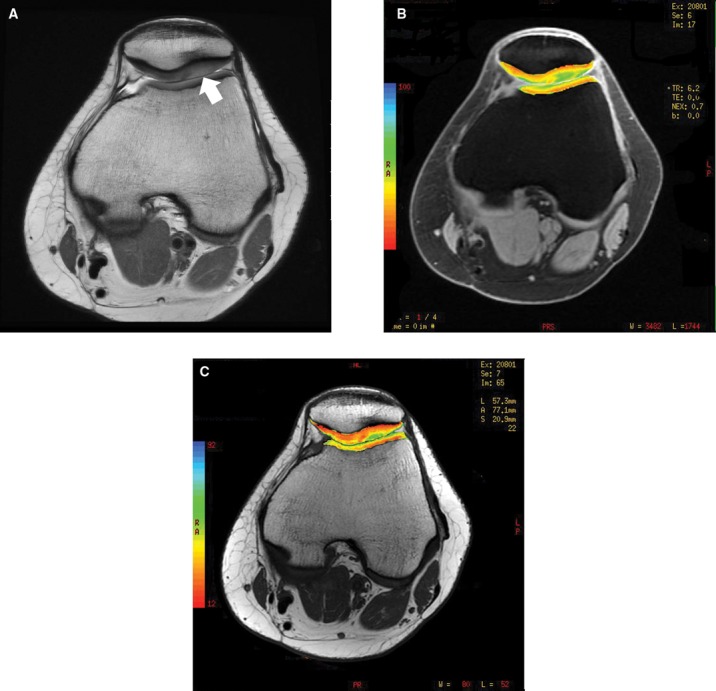
(A) Axial proton density sequence (TR = 4850 milliseconds, TE = 26 milliseconds) of the knee in a 21-year-old woman who has undergone distal realignment 3 years prior demonstrates loss of the normal gray scale stratification of cartilage along the lateral patellar facet (arrow) with subchondral sclerosis, suggestive of lateral facet overload. T1 rho imaging (B) and T2 mapping (C) demonstrate prolonged relaxation times in the same area, indicating depletion of proteoglycan and abnormal collagen orientation, respectively.
Conclusion
Evaluation and management of the painful patellofemoral joint in the athlete requires a thoughtful clinical evaluation including a comprehensive physical examination, standardized radiographs, and, often, advanced imaging such as MRI to evaluate the static and dynamic stabilizers as well as the articular surfaces of the joint. Newer imaging techniques provide noninvasive insight into cartilage ultrastructure, detecting early degenerative change before loss of cartilage thickness.
Footnotes
No potential conflict of interest declared.
References
- 1. Ahmad CS, Brown GD, Stein BS. The docking technique for medial patellofemoral ligament reconstruction: surgical technique and clinical outcome. Am J Sports Med. 2009;37:2021-2027 [DOI] [PubMed] [Google Scholar]
- 2. Ahmad CS, Shubin Stein B, Matuz D, Henry JH. Immediate surgical repair of the medial patellar stabilizers for acute patellar dislocation: a review of eight cases. Am J Sports Med. 2000;28:804-810 [DOI] [PubMed] [Google Scholar]
- 3. Barrett JJ, Smith PHS. Bone imaging with 99Tcm polyphosphate: a comparison with 18F and skeletal radiography. Br J Radiol. 1974;47:387-392 [DOI] [PubMed] [Google Scholar]
- 4. Bianchi S, Zwass A, Abdelwahab IF, Banderali A. Diagnosis of tears of the quadriceps tendon of the knee: value of sonography. AJR Am J Roentgenol. 1994;162:1137-1140 [DOI] [PubMed] [Google Scholar]
- 5. Blackburne JS, Peel TE. A new method of measuring patellar height. J Bone Joint Surg Br. 1977;59:241-242 [DOI] [PubMed] [Google Scholar]
- 6. Brattstroem H. Shape of the intercondylar groove normally and in recurrent dislocation of patella: a clinical and x-ray-anatomical investigation. Acta Orthop Scand Suppl. 1964;68:1-148 [PubMed] [Google Scholar]
- 7. Bredella MA, Tirman PF, Peterfy CG, et al. Accuracy of T2-weighted fast spin echo MR imaging with fat saturation in detecting cartilage defects in the knee: comparison with arthroscopy in 130 patients. AJR Am J Roentgenol. 1999;172:1073-1080 [DOI] [PubMed] [Google Scholar]
- 8. Caton JH, Dejour D. Tibial tubercle osteotomy in patello-femoral instability and in patellar height abnormality. Int Orthop. 2010;34:305-309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Conlan T, Garth WP, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75:682-693 [DOI] [PubMed] [Google Scholar]
- 10. Dejour D, Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc. 2007;15:39-46 [DOI] [PubMed] [Google Scholar]
- 11. Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19-26 [DOI] [PubMed] [Google Scholar]
- 12. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26:59-65 [DOI] [PubMed] [Google Scholar]
- 13. Disler DG, McCauley TR, Kelman CG, et al. Fat-suppressed three-dimensional spoiled gradient-echo MR imaging of hyaline cartilage defects in the knee: comparison with standard MR imaging and arthroscopy. AJR Am J Roentgenol. 1996;167:127-132 [DOI] [PubMed] [Google Scholar]
- 14. Dupuy DE, Hangen DH, Zachazewski JE, Boland AL, Palmer W. Kinematic CT of the patellofemoral joint. AJR Am J Roentgenol. 1997;169:211-215 [DOI] [PubMed] [Google Scholar]
- 15. Dye SF, Boll DA. Radionuclide imaging of the patellofemoral joint in young adults with anterior knee pain. Orthop Clin North Am. 1986;17:249-262 [PubMed] [Google Scholar]
- 16. Elias DA, White LM, Fithian DC. Acute lateral patellar dislocation at MR imaging: injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology. 2002;225:736-743 [DOI] [PubMed] [Google Scholar]
- 17. Fornage BD, Rifkin MD, Touche DH, Segal PM. Sonography of the patellar tendon: preliminary observations. AJR Am J Roentgenol. 1984;143:179-182 [DOI] [PubMed] [Google Scholar]
- 18. Fulkerson JP. Disorders of the Patellofemoral Joint. 4th ed. Philadelphia, PA: Lippincott Willliams & Wilkins; 2004 [Google Scholar]
- 19. Gold GE, Burstein D, Dardzinski B, Lang P, Boada F, Mosher T. MRI of articular cartilage in OA: novel pulse sequences and compositional/functional markers. Osteoarthritis Cartilage. 2006;14(suppl A):A76-A86 [DOI] [PubMed] [Google Scholar]
- 20. Grelsamer RP, Meadows S. The modified Insall-Salvati ratio for assessment of patellar height. Clin Orthop. 1992;282:170-176 [PubMed] [Google Scholar]
- 21. Guzzanti V, Gigante A, Di Lazzaro A, Fabbriciani C. Patellofemoral malalignment in adolescents: computerized tomographic assessment with or without quadriceps contraction. Am J Sports Med. 1994;22:55-60 [DOI] [PubMed] [Google Scholar]
- 22. Hehne HJ. Biomechanics of the patellofemoral joint and its clinical relevance. Clin Orthop. 1990;258:73-85 [PubMed] [Google Scholar]
- 23. Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101:101-104 [DOI] [PubMed] [Google Scholar]
- 24. Jacobsen K, Bertheussen K. The vertical location of the patella: fundamental views on the concept patella alta, using a normal sample. Acta Orthop Scand. 1974;45:436-445 [DOI] [PubMed] [Google Scholar]
- 25. Lanyon P, Jones A, Doherty M. Assessing progression of patellofemoral osteoarthritis: a comparison between two radiographic methods. Ann Rheum Dis. 1996;55:875-879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Laurin CA, Dussault R, Levesque HP. The tangential x-ray investigation of the patellofemoral joint: x-ray technique, diagnostic criteria and their interpretation. Clin Orthop. 1979;144:16-26 [PubMed] [Google Scholar]
- 27. Maldague B, Malghem J. Interet du profil du genou dans le depistage des instabilites rotuliennes. Radiol J CEPUR. 1989;9:3-14 [PubMed] [Google Scholar]
- 28. Malghem J, Maldague B. Depth insufficiency of the proximal trochlear groove on lateral radiographs of the knee: relation to patellar dislocation. Radiology. 1989;170:507-510 [DOI] [PubMed] [Google Scholar]
- 29. Marek J, Pietrzak S. Evaluation of patella position based on radiologic and ultrasonographic examination: comparison of the diagnostic value. J Pediatr Orthop. 1998;18:679-682 [DOI] [PubMed] [Google Scholar]
- 30. Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391-1396 [PubMed] [Google Scholar]
- 31. Mow VC, Huiskes R. Basic Orthopaedic Biomechanics and Mechano-biology. 3rd ed. New York, NY: Lippincott Williams & Wilkins; 2004 [Google Scholar]
- 32. Murray TF, Dupont JY, Fulkerson JP. Axial and lateral radiographs in evaluating patellofemoral malalignment. Am J Sports Med. 1999;27:580-584 [DOI] [PubMed] [Google Scholar]
- 33. Nomura E, Horiuchi Y, Inoue M. Correlation of MR imaging findings and open exploration of medial patellofemoral ligament injuries in acute patellar dislocations. Knee. 2002;9:139-143 [DOI] [PubMed] [Google Scholar]
- 34. Phornphutkul C, Sekiya JK, Wojtys EM, Jacobson JA. Sonographic imaging of the patellofemoral medial joint stabilizing structures: findings in human cadavers. Orthopedics. 2007;30:472-478 [DOI] [PubMed] [Google Scholar]
- 35. Potter HG, Linklater JA, Allen AA, Hannafin JA, Haas SB. Magnetic resonance imaging of articular cartilage in the knee: an evaluation with use of fast spin-echo imaging. J Bone Joint Surg Am. 1998;80:1276-1284 [DOI] [PubMed] [Google Scholar]
- 36. Richardson ML, Selby B, Montana MA, Mack LA. Ultrasonography of the knee. Radiol Clin North Am. 1988;26:63-75 [PubMed] [Google Scholar]
- 37. Sallay PI, Poggi J, Speer KP, Garrett WE. Acute dislocation of the patella: a correlative pathoanatomic study. Am J Sports Med. 1996;24:52-60 [DOI] [PubMed] [Google Scholar]
- 38. Schmid M, Pfirrmann C, Koch P, Zanetti M, Kuehn B, Hodler J. Imaging of patellar cartilage with a 2D multiple-echo data image combination sequence. AJR Am J Roentgenol. 2005;184:1744-1748 [DOI] [PubMed] [Google Scholar]
- 39. Schutzer SF, Ramsby GR, Fulkerson JP. Computed tomographic classification of patellofemoral pain patients. Orthop Clin North Am. 1986;17:235-248 [PubMed] [Google Scholar]
- 40. Schutzer SF, Ramsby GR, Fulkerson JP. The evaluation of patellofemoral pain using computerized tomography: a preliminary study. Clin Orthop. 1986;204:286-293 [PubMed] [Google Scholar]
- 41. Stanford W, Phelan J, Kathol MH, et al. Patellofemoral joint motion: evaluation by ultrafast computed tomography. Skeletal Radiol. 1988;17:487-492 [DOI] [PubMed] [Google Scholar]
- 42. Tavernier T, Dejour D. Knee imaging: what is the best modality. J Radiol. 2001;82(3, pt 2):387-405 [PubMed] [Google Scholar]
- 43. Warren LF, Marshall JL. The supporting structures and layers on the medial side of the knee: an anatomical analysis. J Bone Joint Surg Am. 1979;61:56-62 [PubMed] [Google Scholar]
- 44. Wheaton AJ, Casey FL, Gougoutas AJ, et al. Correlation of T1ρ with fixed charge density in cartilage. J Magn Reson Imaging. 2004;20:519-525 [DOI] [PubMed] [Google Scholar]
- 45. Wiberg G. Roentgenographic and anatomic studies on the femoro-patellar joint. Acta Orthop Scand. 1941;12:319-410 [Google Scholar]
- 46. Xia Y, Moody JB, Burton-Wurster N, Lust G. Quantitative in situ correlation between microscopic MRI and polarized light microscopy studies of articular cartilage. Osteoarthritis Cartilage. 2001;9:393-406 [DOI] [PubMed] [Google Scholar]


