Abstract
Symptomatic muscle herniations are an unusual cause of upper extremity pain in the athlete that is rarely reported in the literature. Out of 18 reported cases of upper extremity herniations, only 3 were caused by strenuous exertion. This article describes a successful repair of a 21-year-old rock climber’s ventral forearm herniation with polypropylene mesh.
Keywords: symptomatic herniation, forearm hernia, muscle hernia, rock climbing, mesh graft
A muscle hernia is defined as a protrusion of the muscle belly through an acquired or congenital fascial defect. Constitutional herniations may occur through congenital fascial defects, or they may be acquired by means of exertional fatigue.1 Repetitive exercise may result in muscle hypertrophy and elevated compartment pressures, which in turn produces herniations through weak points in the fascia where small vessels emerge from the deep muscle compartment.12 Traumatic defects are due to either fascial tears caused by direct penetrating wounds or fascial ruptures produced by blunt trauma of a contracted muscle.12
Symptomatic muscle hernias in the lower extremity are much more common than they are in the upper extremity, with the anterior compartment of the lower leg being the most common site.6 A symptomatic muscle hernia in the forearm is rare, with only 18 cases being reported.3,5,6,10,12-14 Muscle hernias in the upper extremity occur almost exclusively in males, with only 1 previously reported case occurring in a female.10 Of the 18 cases, 12 were caused by sharp or blunt trauma, whereas 3 were constitutional defects caused by strenuous exertion.6
The diagnosis of a muscle hernia can be made clinically by palpating a protruded muscle belly at the fascial defect, which increases in size with contraction of that muscle. Dynamic sonographic evaluation is an effective tool that can be performed before and after a muscle contraction to verify and assess the size of the hernia.1,2,5 The advantage of an ultrasound evaluation is its relative ease of application and low cost. MRI can be used evaluate the size of the hernia, the extent of the fascial defect, the amount of soft tissue edema, and the specific muscles and structures involved.5,8,16 Dynamic MRI before and after muscle contraction can delineate the fascial defect and size of muscle herniation.5
Several treatments have been devised for the treatment of forearm muscle hernias, including rest, physiotherapy, fasciorrhaphy or primary repair, and fasciotomy with fascial lata inlay, onlay, or wraparound.3,5,6,10-14
Case Report
A 21-year-old female rock climber was performing a single-armed body lift on a handhold when she felt a pop and burning sensation in the midaspect of the volar forearm, with immediate onset of pain and deformity. She also described subjective paresthesias in the ulnar distribution of the hand, which later resolved. Owing to persistent pain after several days of rest, she presented for evaluation. Physical examination demonstrated a 1-cm2 herniation of the muscle at the volar forearm fascia between the flexor carpi radialis and palmaris longus muscle bellies (Figure 1). There was pain with muscle contraction as well as a visible increase in the size of the herniation with attempted wrist flexion. A trial of formal and informal physical therapy was carried out over 9 months, with no relief of symptoms, and the patient decided to proceed with surgical repair.
Figure 1.

Preoperative evaluation demonstrating muscle herniation at the volar forearm fascia between the flexor carpi radialis and palmaris longus muscle bellies.
At surgery a 2-cm incision was made over the defect and a circular 1.5-cm defect noted in the volar forearm fascia (Figure 2). A small amount of the palmaris longus was exposed, as well as the flexor carpi radialis muscle belly. Because of its small size, the fascial rent seemed amenable to primary repair, with augmentation to prevent recurrence. A polypropylene mesh (Prolene, Ethicon Inc, Somerville, New Jersey) was cut 1 cm larger than the diameter of the circular defect and deployed subfascially. A 2-0 Monocryl suture (Monocryl, Ethicon Inc) was then used to repair the defect with a longitudinally oriented running suture. Figure-of-8 sutures were then placed to stabilize the mesh (Figure 3). There were no complications, and formal physical therapy was not utilized.
Figure 2.

At surgery, a 2-cm incision was made over the defect and a circular 1.5-cm defect noted in the volar forearm fascia.
Figure 3.
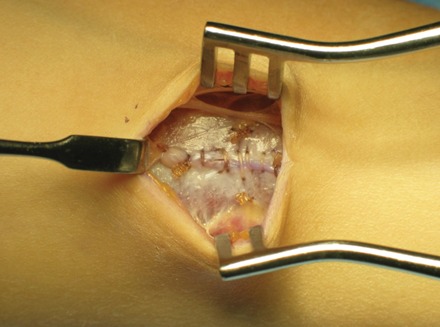
Intraoperative photograph demonstrates the repaired defect, with polypropylene mesh deployed subfascially under the defect.
At 6 weeks, the patient was asymptomatic and had full range of motion of the wrist and fingers. She was already performing yoga and some light rock climbing without symptoms and was pleased with her cosmetic result (Figure 4). She was released to full activities at this stage. At 9 months, she returned to activities, including rock climbing, without symptoms.
Figure 4.

At 6 weeks postoperatively, the herniation has resolved with acceptable cosmetic appearance.
Discussion
Muscle herniations can be found at various sites of the body, with the lower leg being the most common. Though rare, these may be underdiagnosed or misdiagnosed as hematomas and varicosities.13 The forearm is a rare site for a symptomatic hernia, although it has been reported.3,5,6,10-14 Pain is generated from the protrusion and compression of the muscle at the proximal edge of the fascial defect in the volar forearm.6 If the fascial split is large enough, the area may be asymptomatic, whereas strangulation or incarceration can cause significant pain and disability. Almost all symptomatic volar forearm hernias occur in the midforearm, with only 1 reported in the distal forearm.10
The most common cause of a forearm muscle herniation is trauma, with blunt trauma causing 7 of the 18 cases and with sharp trauma causing 5. Only 3 previous herniations occurred from exertional activity. Khalid et al6 reported a case in the flexor forearm in an assembly line worker from repeated strenuous activity, which was repaired by a fascia lata graft. Kendi et al5 described a case in the flexor forearm from chopping wood, which was not repaired, and Roberts et al12 described a case in the extensor forearm from lifting a bale of hay, which was primarily closed with a palmaris longus interweave.
Reports of surgical treatment of muscle hernias date back to the early 20th century, where separate examples were published on an anterior tibialis and adductor longus hernia repair.4,7 Since then, various treatments have surfaced, and the best option has become somewhat controversial.3,5,6,10-14 There are several reports of compartment syndrome of the lower leg after fascial repair.9,15 Compartment syndrome occurred after primary repair of the anterior compartment of the lower leg, performed solely for cosmetic appearance,9 which resulted in multiple debridements, skin grafts, and a persistent footdrop.9 Asymptomatic muscle hernias should usually be treated without surgery, and symptomatic hernias should be given a trial of conservative management before surgical options are discussed.9
Because of the risk of compartment syndrome, open fasciotomies may be the best option for treatment of hernias. Some have been performed in the upper extremity,9,10 although a fasciotomy in the upper extremity may lead to a more noticeable and often unacceptable cosmetic appearance. Fascia lata grafts are an option in the forearm.3,6,11,12 A major drawback is the morbidity at the donor site.12
Polypropylene mesh is an option to augment a primary repair of a small volar forearm muscle herniation. The present repair restored normal anatomy without undue tension and obviated the morbidity of a fascial lata or other autogenous graft harvest. Using mesh to augment the repair allowed early return to activities without undue concern for herniation.
Footnotes
No potential conflict of interest declared.
References
- 1. Bates DG. Dynamic ultrasound findings of bilateral anterior tibialis muscle herniation in a pediatric patient. Pediatr Radiol. 2001;31:753-755 [DOI] [PubMed] [Google Scholar]
- 2. Bianchi S, Abdelwahab IF, Mazzola CG, Ricci G, Damiani S. Sonographic examination of muscle herniation. J Ultrasound Med. 1995;14:357-360 [DOI] [PubMed] [Google Scholar]
- 3. Golshani SD, Lee C, Sydorak R. Symptomatic forearm muscle hernia: repair by autologous fascia lata inlay. Ann Plast Surg. 1999;43:204-206 [PubMed] [Google Scholar]
- 4. Hartzell JB. The use of living fascia transplant to repair a hernia of the tibialis anticus muscle. JAMA. 1936;107:492-493 [Google Scholar]
- 5. Kendi TK, Altinok D, Erdal HH, et al. Imaging in the diagnosis of symptomatic forearm muscle herniation. Skeletal Radiol. 2003;32:364-366 [DOI] [PubMed] [Google Scholar]
- 6. Khalid KA, Mah ET. Treatment of a symptomatic forearm muscle herniation with a wrap-around fascia lata graft. J Hand Microsurg. 2009;1(1):54-59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McWilliams CA. Hernia of the adductor longus muscle with operation. Med Rec. 1901;59:468 [Google Scholar]
- 8. Mellado JM, Perez del Palomar L. Muscle hernias of the lower leg: MRI findings. Skeletal Radiol. 1999;28:465-469 [DOI] [PubMed] [Google Scholar]
- 9. Miniaci A, Rorabeck CH. Compartment syndrome as a complication of repair of a hernia of the tibialis anterior: a case report. J Bone Joint Surg Am. 1986;68:1444-1445 [PubMed] [Google Scholar]
- 10. Olch CL, Watson HK. Symptomatic forearm fascial hernia. J Hand Surg Am. 1996;21:693-695 [DOI] [PubMed] [Google Scholar]
- 11. Riordan C, Hussain M, McCann J. Forearm muscle hernia: a case report. Eur J Plast Surg. 2002;25:231-232 [Google Scholar]
- 12. Roberts JO, Regan PJ, Dickinson JC, Bailey BN. Forearm muscle herniae and their treatment. J Hand Surg Br. 1989;14:319-321 [DOI] [PubMed] [Google Scholar]
- 13. Schecter DC, Waddell WR, Coppinger WR. Muscle hernia: twenty personal observations. Am Surg. 1963;29:483-490 [PubMed] [Google Scholar]
- 14. Simon HE. Muscle hernia: with report of six additional cases in the arm and leg. Mil Surg. 1945;97:369-374 [Google Scholar]
- 15. Wolfort FG, Molvang LC, Piltzer HS. Anterior tibial compartment syndrome following muscle hernia repair. Arch Surg. 1973;106:97-99 [DOI] [PubMed] [Google Scholar]
- 16. Zeiss J, Nabil AE, Woldenberg LS. Magnetic resonance imaging in the diagnosis of anterior tibialis muscle herniation. Clin Orthop. 1989;244:249-253 [PubMed] [Google Scholar]


