Abstract
Background:
Wrist injuries are common in sports. Those who are involved in the care of athletes should be familiar with hand and wrist anatomy, common wrist injuries, and clinical examination; they should also know how to recognize emergent problems.
Level of Evidence:
Level V, expert opinion.
Keywords: sports injuries, wrist, adult
Sports-related wrist injuries are relatively common. According to the National Collegiate Athletic Association Sports Injury Monitoring System, 349 of the 5900 rostered athletes (5.9%) sustained a primary fracture from 1986 to 2000.13 Of these 349 incidents, hand and carpal bone fractures were the most common injuries overall; wrist fractures were the sixth-most common. The Royal Infirmary of Edinburgh has also performed a retrospective study of sports-related injuries.7 Of the 5953 fractures treated, 761 (12.8%) were sports related; furthermore, 131 injuries involved the distal radius and distal ulna and 39 involved the carpus. Distal radius and carpal bone fractures accounted for 24.1% of fractures in soccer, 11.8% in rugby, 43.5% in snowboarding, 15.0% in basketball, 25.0% in running, 45.5% in ice skating, and 87.0% in in-line skating.7 When this series was examined in detail, analysis revealed that a majority of carpal fractures involved the scaphoid.2
Given the high incidence of sports-related hand and wrist fractures, it is important for those involved in the care of athletes to be knowledgeable about the evaluation and treatment of these injures. Furthermore, it is critical for those caring for athletes to understand the potential morbidity of neglected or mistreated fractures.
Anatomy
The wrist is a complex articulation involving the 8 carpal bones and the distal radius and ulna. The carpal bones are divided into the proximal and distal rows. The proximal row consists of the scaphoid, lunate, triquetrum, and pisiform. The distal row consists of the trapezium, trapezoid, capitate, and hamate. The scaphoid is sometimes considered to be a part of the proximal and distal rows. These carpal bones are connected to one another by various ligaments. In the proximal row, the scapholunate and lunotriquetral ligaments are most important. They link the lunate to the scaphoid and triquetrum, respectively. On the volar side of the wrist, a number of stout intracapsular ligaments connect the distal radius and distal ulna to the carpus (Figure 1A). On the dorsal side of the wrist, an intracapsular ligament attaches to the dorsal side of the triquetrum9 (Figure 1B).
Figure 1.
A, volar wrist ligaments. Ligaments link adjacent carpal bones to one another, link the carpal bones to the radius, and link the carpal bones to the ulna. B, dorsal wrist ligaments. Ligaments link adjacent carpal bones to one another and link the carpal bones to the radius. A long ligament spans the carpal bones dorsally. (From Bednar JM, Osterman AL. Carpal instability: evaluation and treatment. J Am Acad Orthop Surg. 1993;1:10-17. Reprinted with permission.)
The distal radius and ulna articulate at the distal radioulnar joint. The soft tissues around this joint consist of volar and dorsal radioulnar ligaments, which are the primary stabilizers. These ligaments converge toward the ulnar head. An articular disc originates from the ulnar edge of the distal radius and blends into the radioulnar ligaments. In addition, the sheath of the extensor carpi ulnaris (ECU) blends into and augments the dorsal radioulnar ligament. Volar intracapsular ulnocarpal ligaments augment the volar radioulnar ligament. The radioulnar ligaments, articular disc, ECU sheath, and ulnocarpal ligaments are collectively called the triangular fibrocartilage complex1 (Figure 2).
Figure 2.

The triangular fibrocartilage complex consists of the radioulnar ligaments, articular disc, extensor carpi ulnaris subsheath, and ulnocarpal ligaments. (From Chidgey LK. The distal radioulnar joint: problems and solutions. J Am Acad Orthop Surg. 1995;3:95-100. Reprinted with permission.)
The ulnar artery supplies the hand predominately through the superficial arch, and the radial artery supplies the hand predominately through the deep arch. The superficial arch is complete in 80% of individuals, and the deep arch is complete in 97%.6
The extrinsic finger flexors, flexor pollicis longus, and the median nerve pass through the carpal tunnel on the volar side of the wrist. A thick transverse carpal ligament extends from the hook of the hamate and triquetrum to the scaphoid and trapezium. Adjacent to the carpal tunnel is Guyon’s canal, which contains the ulnar nerve and artery. The thick retinaculum, the volar carpal ligament, overlies the ulnar artery and nerve as they pass adjacent to the pisiform and beneath the ligament connecting the pisiform to the hamate. On the dorsal surface of the wrist, the extrinsic finger extensors originate proximally on the lateral epicondyle, and the corresponding tendons pass beneath the extensor retinaculum through 1 of 6 compartments.
Evaluation
Evaluation of the acutely injured hand and wrist involves obtaining and performing a detailed history and physical examination. Important elements of the history include prior injury to the wrist, mechanism and time of injury, and associated symptoms. From the history, the examiner can also begin to determine if the problem is serious enough to warrant immediate transport to the emergency department.
A carefully performed physical examination expands on information obtained from the history. A systematic approach to examination is useful, beginning with observation, then palpation, active range of motion, and neurovascular examination. Complex provocative maneuvers will not be discussed, because they often have limited utility in acute evaluation of wrist injuries and variable utility among different examiners.20,28
Observation of the patient’s upper extremity may reveal an obvious open wound, deformity, or swelling. Gloves, tape, and all other equipment should be removed. The skin is inspected for any lacerations, abrasions, or puncture wounds. The examiner should be mindful that even the smallest puncture wound may be indicative of an open fracture.
If the patient can tolerate it, the wrist can be more thoroughly palpated from the radial side to the ulnar side. Begin by palpating the radial styloid. Then, examine the scaphoid by applying an axial load on the thumb metacarpal, palpating the scaphoid tubercle volarly, and then palpating the radial snuffbox to examine the scaphoid. The borders of the snuffbox are the abductor pollicis longus–extensor pollicis brevis tendons, the extensor pollicis longus tendon, and the radial styloid proximally. The distal radius is palpated. The wrist can be supinated and pronated while palpating the distal radioulnar joint to see if there is any gross instability or pain. The pisiform, the hook of hamate, the ulna fovea, and the ECU sheath are palpated. The ulna fovea is located in the recess between the distal ulna and the carpus along the ulnar side of the forearm and wrist. Circumduction of the wrist may cause the ECU to dislocate volarly if the sheath is torn.
When possible, assess the patient’s active flexion and extension of the elbow, supination and pronation of the forearm, flexion and extension of the wrist, and flexion and extension of the fingers. In addition, disproportionate pain with passive range of motion of the digits is a warning sign of acute nerve compression, fracture, or dislocation.
A careful neurovascular examination should be performed. Light touch sensibility is assessed in the following areas: median nerve (radial-volar tip of the index finger); ulnar nerve (ulnar-volar tip of the small finger); and superficial radial nerve (the first dorsal interspace). Motor function should also be tested in the following ways: median nerve, by pushing the thumb palmarly from the coronal plane of the hand (Figure 3A); ulnar nerve, by finger abduction and adduction (Figure 3B); and radial nerve, by thumb retropulsion (Figure 3C). Capillary refill should be noted in the digits, and the radial and ulnar pulses noted.
Figure 3.

A, motor examination of the median nerve. The thumb is palmarly abducted out of the plane of the palm against resistance, and the muscle belly is palpated. B, motor examination of the ulnar nerve. The index finger is abducted against resistance, and the muscle belly of the first dorsal interosseous is palpated. C, motor examination of the radial nerve. The thumb is retropulsed dorsally out of the plane of the palm against resistance. The tendon of extensor pollicis longus is palpated for tension.
Emergent Problems
It is important for the examiner to be aware of those clinical conditions that require immediate treatment. The major emergencies are the dysvascular hand, acute nerve compression, open fracture, dislocation, or, rarely, traumatic amputation. Note that these emergencies are not mutually exclusive. For example, a perilunate dislocation may be accompanied by acute carpal tunnel syndrome.
On examination, the dysvascular hand will be pale or mottled, and capillary refill will be sluggish. Acute nerve compression—most commonly, acute carpal tunnel syndrome—is characterized by disproportionate pain relative to examination, pain with passive range of motion of the digits, and paraesthesias or numbness in the thumb, index, middle, and ring fingers. An open fracture or dislocation may demonstrate gross deformity, swelling, loss of motion, or pain on motion. Again, the clinician should be aware that any puncture wound or laceration, no matter the size, may be a result of the bone violating the skin during fracture. A traumatic amputation should be examined quickly to assess the extent of the injury. The amputated part should be examined to ensure the entire part has been recovered for transport to the hospital.
Although many of these problems need rapid transport to the emergency department, some basic on-field interventions can be helpful. In the grossly deformed wrist with a dysvascular limb or with symptoms of acute nerve compression, it is reasonable to perform a closed reduction on the field and to splint the wrist at a more natural length. Gross angulation may result in arterial spasm or compression of the vessels, and even incomplete reduction with improved limb positioning can be helpful. It is important to release any tight clothing or equipment proximally; it is also important not to wrap the hand and wrist too tightly during splinting. An amputated part should be wrapped with a moist gauze sponge and placed in a plastic bag. The bag with the limb should be placed in a second bag, filled with ice or ice water. The amputated part should never be placed on dry ice.
Radiographs
In some situations, fluoroscopy or radiography is available on-site. Standard radiographs include anteroposterior, oblique, and lateral views of the wrist. A scaphoid view is recommended if there is radial-sided wrist pain. This is performed with the wrist in ulnar deviation with slight flexion. When evaluating a radiograph, one should evaluate the soft tissues for swelling and foreign bodies that may be radio-opaque. The bones of the hand should be screened before examination of the carpus and distal radius and ulna.
The carpal bones should each demonstrate a smooth outline. Subtle fractures can demonstrate cortical disruption or discontinuity. Basic features of the carpus include smooth continuous arcs representing the proximal and distal carpal rows, called Gilula’s lines (Figure 4). If these arcs are disrupted, a disorder of the wrist is likely present.
Figure 4.
A, Gilula’s arcs. The borders of the proximal and distal carpal rows should form a smooth contour and not be disrupted. B, Gilula’s arcs have been disrupted in this perilunate fracture-dislocation.
Fractures
Distal Radius Fracture
Distal radius fractures are common injuries, especially in hockey, ice-skating, and in-line skating (Figure 5). The typical mechanism for these injuries is a fall on an outstretched hand. Depending of the severity of the mechanism, distal radius injuries may be accompanied by scaphoid fracture, intercarpal ligament injury, distal radioulnar joint injury, or fractures of the elbow region.10,11
Figure 5.

A, distal radius fracture. Posteroanterior radiograph demonstrates extra-articular fracture of the distal radius and ulna styloid fracture. B, distal radius fracture. Lateral radiograph demonstrates dorsally angulated extra-articular fracture of the distal radius.
Physical examination reveals swelling of the wrist, possible gross deformity, limited range of motion, and point tenderness along the distal radius. Radiographs of the wrist are routinely obtained. If the distal radius fracture is displaced, a closed reduction may be performed using a hematoma block or formal sedation. Radiographs are obtained after reduction. If the fracture is stable and in acceptable alignment, cast immobilization is an option. If the distal radius fracture is unstable or cannot be satisfactorily aligned, then operative intervention is warranted.
Return to sport after distal radius fracture depends on adequate healing, which usually takes 6 to 8 weeks. In patients treated operatively or nonoperatively, it is important to emphasize early finger range of motion and swelling control during the subacute period. Upon healing of the fracture, wrist and forearm range of motion should be emphasized and progressive strengthening initiated as motion improves.
Late complications of distal radius fracture include extensor pollicis longus tendon rupture, which manifests as an inability to retropulse the thumb. This is typically seen in the nondisplaced fracture treated in a cast. Stiffness of the fingers and dystrophic changes may be seen as well.
Dorsal Cortical Triquetral Fracture
Dorsal cortical triquetral fractures are the second-most-common carpal fracture.4 Many dorsal triquetral fractures are often diagnosed as a wrist sprain. These injuries have been traditionally considered to be avulsion fractures of the dorsal capsular ligaments off the triquetrum, but some authors believe that the injury is the result of the triquetrum striking the distal ulna.15
Physical examination findings are often nonspecific, other than tenderness and swelling; however, careful examination may detect (1) tenderness over the triquetrum as well as (2) the dorsal capsular fragment, as confirmed by the lateral radiograph. The mainstay of treatment is immobilization for approximately 2 to 3 weeks. The dorsal fragments do not often unite but remain asymptomatic. It is important, however, to distinguish these fractures from triquetral body or volar triquetral fractures given that these may represent a more severe injury (Figure 6).
Figure 6.

A, triquetral fracture. This is the most common variant of triquetral fracture. B, triquetral body fracture. This fracture represents a more significant injury than the more common triquetral fracture.
Scaphoid Fracture
The scaphoid is the most commonly fractured carpal bone.14 The mechanism of injury is postulated to be a fall on an extended wrist with a primarily radial load.30 Scaphoid fracture has been described as occurring simultaneously with wrist fractures; they may also be part of a greater-arc perilunate fracture-dislocation.24
The patient typically presents with radial-sided wrist pain. Tenderness in the anatomic snuffbox, pain with axial loading of the thumb, and/or tenderness on the scaphoid tubercle are helpful findings. Radiographs should include a dedicated scaphoid view; however, many nondisplaced scaphoid fractures are difficult to detect. If plain radiographs are normal and clinical suspicion is high, magnetic resonance imaging (MRI) is warranted (Figure 7).
Figure 7.

A, scaphoid fracture. The scaphoid-view radiograph does not show any significant abnormality; however, clinical suspicion was high and magnetic resonance imaging was obtained. B, scaphoid fracture. Magnetic resonance imaging demonstrated nondisplaced scaphoid fracture.
It is important to recognize that complications of scaphoid fractures are difficult to manage. The blood supply enters the scaphoid from the distal half of the bone, and the supply to the proximal pole is relatively tenuous.12 As a result, proximal pole fractures are at high risk for the development of avascular necrosis and nonunion. Therefore, a high index of suspicion and thorough examination at the time of initial injury can help preclude such complications.
Treatment options for the nondisplaced middle-third fracture include thumb-spica cast immobilization or placement of a compression screw fixation. Screw fixation provides immediate stability and allows gentle active motion and progressive strengthening to begin 2 weeks postoperatively in cases where there is a simple nondisplaced scaphoid fracture. In cases where there is a more complex, unstable fracture pattern, it is wise to immobilize the scaphoid for several weeks and avoid early return to sport. There is some evidence that screw fixation leads to early scaphotrapezial arthritis.29
Immediate return to play in a cast has been successfully documented in certain sports and positions.21-23 Rettig et al reported full return to sports at an average of 5.8 weeks, although radiographic healing was noted at an average of 9.8 weeks after screw fixation.21 Proximal third fractures may be at higher risk of nonunion in patients who return to play in a cast or splint.23 Displaced fractures require operative treatment, and return to play should be approached cautiously given that such fractures have a higher risk of malunion and nonunion.3
Hook of Hamate Fracture
The hamulus, or hook of hamate, is a bony process that is speculated to function as a pulley for the flexor tendons during power grip. Hook of hamate fractures are often seen in baseball, golf, and tennis.25,26 Most believe that this injury occurs owing to transmission of the force from the bat, club, or racquet to the palm, thus leading to fracture.
Hook of hamate fractures can be difficult to diagnose. A general guideline to remember during examination is that the hook sits approximately 1 thumbnail’s breadth radial and distal to the pisiform. A carpal tunnel–view radiograph has traditionally been used to evaluate the injury; however, if the injury is suspected despite unremarkable radiographs, MRI, or computed tomography is recommended (Figure 8). Hemorrhage from the fracture can result in ulnar or median nerve symptoms.4 Chronic hook of hamate fractures may result in a nonunion. These nonunions have been associated with flexor digitorum profundus tendon rupture of the small finger.
Figure 8.
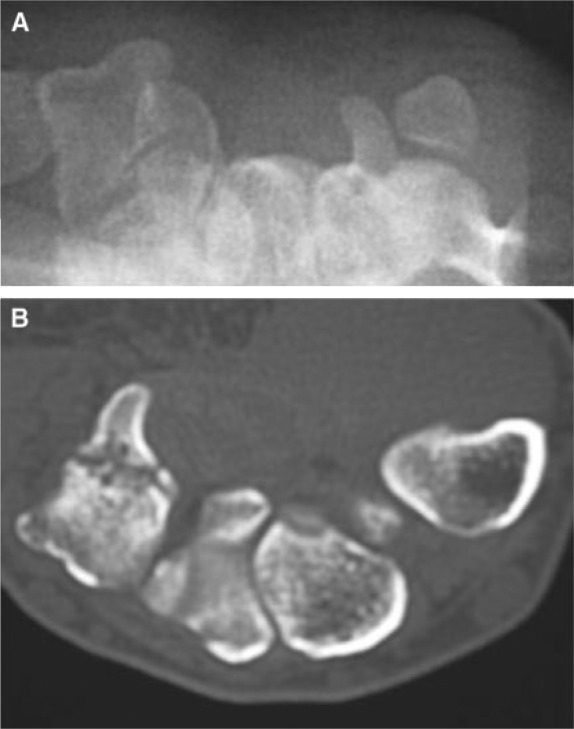
A, hook of hamate fracture. Carpal tunnel view radiograph is unremarkable. Clinical suspicion was high, and a computed tomography scan was obtained. B, hook of hamate fracture. Computed tomography scan demonstrates hook of hamate fracture. Base fractures are difficult to detect on carpal tunnel views.
Some surgeons advocate cast treatment for acute fractures. In general, excision of the fracture fragment yields good results.25,26 The wrist is immobilized for 10 to 14 days to allow wound healing. Return to sport after surgery usually is permitted at 6 to 8 weeks postoperatively.
Soft Tissue Injuries
Scapholunate Ligament Tear
The scapholunate ligament links the scaphoid and the lunate. When the scapholunate ligament is injured, the scaphoid is unlinked from the lunate and the 2 carpal bones move asynchronously. The mechanism of injury is suspected to be a fall on an extended and ulnarly deviated wrist.17
During physical examination, tenderness may be elicited 1 cm distal to Lister’s tubercle. A Watson test may be performed by placing the wrist in ulnar deviation and then applying a dorsally directed load on the scaphoid tubercle. As the wrist is brought into radial deviation, a painful catch or click is considered a positive test result. Radiographs of the wrist demonstrate widening of the scapholunate interval and a cortical ring sign of the scaphoid, which is caused by flexion of the scaphoid relative to the coronal plane. The lateral radiograph may demonstrate that the scaphoid is excessively flexed.
One complicated aspect in the evaluation of scapholunate ligament injuries is that of determining the time of initial injury. When a patient presents with a painful wrist and scapholunate diastasis on radiograph, it can be unclear whether the scapholunate ligament injury is an exacerbation of a chronic injury or the initial presentation of an acute injury.
Wrist arthroscopy is useful in the evaluation and treatment of scapholunate ligament injury.11 If the ligament is injured but not severely disrupted, pins may be placed across the scaphoid and the lunate to provide stability and promote ligament healing. If the ligament is grossly disrupted on arthroscopic evaluation, repair or reconstruction may be performed.
Treatment of a chronic scapholunate ligament injury may consist of splinting or operative intervention. There are numerous techniques for operative reconstruction of the scapholunate ligament; however, the results are modest. In general, because ligament repair or reconstruction is usually tenuous, early return to sports using a playing cast is not recommended.
Perilunate Dislocation
A perilunate dislocation results from the disruption of the scapholunate ligament, then extension of the injury through the capito-lunate articulation and the lunotriquetral ligament.17 One variation of a perilunate dislocation is a fracture dislocation through the scaphoid, rather than an injury through the scapholunate ligament.
Physical examination is often limited, revealing swelling and deformity. The injury may be confused for a distal radius fracture. As the dislocated carpus leads to deformation of the carpal tunnel, paraesthesias or numbness in the median nerve distribution may be present. Radiographs are obtained to confirm the diagnosis (Figure 9). Early, immediate treatment involves reduction of the dislocation. If this is not successful, open reduction should be pursued.
Figure 9.

Perilunate dislocation. The lunate remains in its proper location on the radius, but the remainder of the carpus has separated and is translated radially. This injury has a similar clinical presentation to a distal radius fracture and may be overlooked on radiographs.
Radiographs will demonstrate disruption of Gilula’s lines. The lateral radiograph will demonstrate that the capitate will not be aligned with the lunate, a “spilled teacup sign.”
Operative treatment involves reducing the carpal malalignment with pins, repairing torn ligamentous structures, and internal fixation of fractures. In these cases, early return to play is not generally recommended. Rehabilitation is often prolonged and range of motion limited after this extensive injury.
Triangular Fibrocartilage Complex Tears
The true incidence of triangular fibrocartilage complex (TFCC) tears is unclear. Despite this, some general principles can guide clinical assessment: First, tears are more likely to be a cause of symptoms in younger patients; second, TFCC tears may be associated with injuries to associated structures, such as the ECU, distal radioulnar joint, and lunotriquetral ligament; third, patients with a prominent ulnar head (positive ulna variance) may be predisposed to attritional TFCC tears; and, fourth, attritional TFCC tears may be more common in activities that require ulnar deviation or power gripping.
Physical examination of TFCC tears may be associated with tenderness in the ulna fovea. Since the floor of the ECU sheath is contiguous with the TFCC, there may be tenderness along the ECU. Radiographs may demonstrate positive ulna variance, and MRI or magnetic resonance arthrogram may demonstrate a gross tear of the TFCC or the associated structures.
Nonoperative treatment includes splinting, nonsteroidal anti-inflammatory drugs, and intra-articular corticosteroid injections. In isolated TFCC tears (ie, without distal radioulnar joint instability or ECU instability), definitive management may be deferred until the athlete is out of season.
Wrist arthroscopy is generally the mainstay of treatment if conservative therapy is not successful. Tears in the central, avascular portion of the TFCC are often debrided with an arthroscopic shaver.18 Peripheral tears may be amenable to open or arthroscopic repair.8 After debridement, an athlete can usually return to play in a few weeks. However, TFCC repair requires a longer recovery period of several weeks, until the healing tissue has matured.
Extensor Carpi Ulnaris Subluxation
The ECU is the most ulnar of the extensor tendons. It passes through a sheath in the distal forearm and attaches to the base of the fifth metacarpal. The ECU subsheath also contributes to distal radioulnar joint stability. Acute rupture of this sheath or attenuation of the sheath with gross subluxation of the tendon can occur in tennis players, golfers, and baseball players.
Physical examination may demonstrate subluxation of the ECU with circumduction of the wrist. Subluxation may not be easily elicited at the time of examination. Because the ECU sheath contributes to the TFCC, the ulnar fovea may be tender. Stability of the distal radioulnar joint should be assessed. Although the diagnosis has traditionally been made clinically, dynamic ultrasound is becoming a useful tool in identifying ECU subluxation.
Treatment of these injuries varies from splinting of the wrist in a neutral position to surgical reconstruction of the tendon sheath. An initial trial of nonoperative treatment is recommended. Various surgical approaches have been used for tendon subluxation, including direct repair, groove deepening and sheath plication, and sheath reconstruction.5,16 Return to play depends on healing of the sheath. This often involves immobilization for several weeks.
Return to Play
Details of return to play after specific injuries are discussed above. From a medical standpoint, the optimal time for return to play is after satisfactory bone and soft tissue healing and rehabilitation. In some cases, the athlete may desire early return to play or deferral of definitive management after the season ends. There are several factors to consider in early return to play, including the ability to protect the extremity from further injury, the relative stability of fracture or ligament repair, the player’s position and sport, and social factors. These factors can be in conflict and should be weighed judiciously.19,27
The overriding factor is risk of irrecoverable injury. It is important to consider long-term sequelae and what salvage options are available if the injury is aggravated. Injuries that are difficult to salvage, such as unstable scaphoid fractures or comminuted distal radius fractures, should undergo definitive management, and the athlete should avoid return to play until adequate healing has been demonstrated.
In cases where the injury can be adequately protected, early return to play may be possible depending on the player’s position and sport. For example, a lineman with a stable, nondisplaced distal radius fracture may return to playing football early in a cast; however, a tennis player with the same injury on the dominant wrist should not return so quickly. In some cases, if an injury is amenable to late reconstruction, then an athlete may be able to defer definitive management until the end of the playing season.
The risks of early return to play and deferral of surgical management are often balanced against pressures related to competition and economic factors. Professional and collegiate athletes may have large financial stakes and career opportunities at risk; high school athletes may have opportunities at collegiate scholarships. These factors are not trivial and should be considered in the overall treatment strategy; the athlete and the physician must seriously and carefully approach the risk to be undertaken. The overall long-term health of the athlete should never be ignored despite the magnitude of outside pressures.
Summary
Wrist injuries are common problems in high-speed contact and racquet sports. The recognition of urgent clinical conditions is crucial—especially, acute carpal tunnel syndrome, an open fracture, and joint dislocation. Careful physical examination and plain radiographs will identify the majority of common injuries. In general, optimal timing for return to play follows adequate bone and soft tissue healing and rehabilitation; however, in the elite athlete, early return to play or deferral of treatment may be possible depending on the type and stability of injury, position and sport played, and desire of the athlete.
Footnotes
No potential conflict of interest declared.
NATA Members: Receive 3 free CEUs each year when you subscribe to Sports Health and take and pass the related online quizzes! Not a subscriber? Not a member? The Sports Health–related CEU quizzes are also available for purchase. For more information and to take the quiz for this article, visit www.nata.org/sportshealthquizzes.
References
- 1. Adams BD. Distal radioulnar joint instability. In: Green DP, ed. Green’s Operative Hand Surgery. Philadelphia, PA: Elsevier; 2005: chapter 15 [Google Scholar]
- 2. Aitken S, Court-Brown CM. The epidemiology of sports-related fractures of the hand. Injury. 2008;39:1377-1383 [DOI] [PubMed] [Google Scholar]
- 3. Amadio PC, Berquist TH, Smith DK, et al. Scaphoid malunion. J Hand Surg [Am]. 1989;14:679-687 [DOI] [PubMed] [Google Scholar]
- 4. Amadio PM, Moran SL. Fractures of the carpal bones. In: Green DP, ed. Green’s Operative Hand Surgery. Philadelphia, PA: Elsevier; 2005: chapter 17 [Google Scholar]
- 5. Burkhart SS, Wood MB, Linscheid RL. Posttraumatic recurrent subluxation of the extensor carpi ulnaris tendon. J Hand Surg [Am]. 1982;7:1-3 [DOI] [PubMed] [Google Scholar]
- 6. Coleman SS, Anson BJ. Arterial patterns in the hand based upon a study of 650 specimens. Surg Gynecol Obstet. 1961;113:409-424 [PubMed] [Google Scholar]
- 7. Court-Brown CM, Wood AM, Aitken S. The epidemiology of acute sports-related fractures in adults. Injury. 2008;39(12):1365-1372 [DOI] [PubMed] [Google Scholar]
- 8. Estrella EP, Hung LK, Ho PC, et al. Arthroscopic repair of triangular fibrocartilage complex tears. Arthroscopy. 2007;23:729-737e1 [DOI] [PubMed] [Google Scholar]
- 9. Garcia-Elias M, Geissler WB. Carpal instability. In: Green DP, ed. Green’s Operative Hand Surgery. Philadelphia, PA: Elsevier; 2005: chapter 14 [Google Scholar]
- 10. Geissler WB, Fernandez DL, Lamey DM. Distal radioulnar joint injuries associated with fractures of the distal radius. Clin Orthop Relat Res. 1996;327:135-146 [DOI] [PubMed] [Google Scholar]
- 11. Geissler WB, Freeland AE, Savoie FH, et al. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78:357-365 [DOI] [PubMed] [Google Scholar]
- 12. Gelberman RH, Menon J. The vascularity of the scaphoid bone. J Hand Surg [Am]. 1980;5:508-513 [DOI] [PubMed] [Google Scholar]
- 13. Hame SL, LaFemina JM, McAllister DR, et al. Fractures in the collegiate athlete. Am J Sports Med. 2004;32:446-451 [DOI] [PubMed] [Google Scholar]
- 14. Hove LM. Epidemiology of scaphoid fractures in Bergen, Norway. Scand J Plast Reconstr Surg Hand Surg. 1999;33:423-426 [DOI] [PubMed] [Google Scholar]
- 15. Levy M, Fischel RE, Stern GM, et al. Chip fractures of the os triquetrum: the mechanism of injury. J Bone Joint Surg Br. 1979;61:355-357 [DOI] [PubMed] [Google Scholar]
- 16. MacLennan AJ, Nemechek NM, Waitayawinyu T, et al. Diagnosis and anatomic reconstruction of extensor carpi ulnaris subluxation. J Hand Surg [Am]. 2008;33:59-64 [DOI] [PubMed] [Google Scholar]
- 17. Mayfield JK, Johnson RP, Kilcoyne RK. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg [Am]. 1980;5:226-241 [DOI] [PubMed] [Google Scholar]
- 18. Minami A, Ishikawa J, Suenaga N, et al. Clinical results of treatment of triangular fibrocartilage complex tears by arthroscopic debridement. J Hand Surg [Am]. 1996;21:406-411 [DOI] [PubMed] [Google Scholar]
- 19. Morgan WJ, Slowman LS. Acute hand and wrist injuries in athletes: evaluation and management. J Am Acad Orthop Surg. 2001;9:389-400 [DOI] [PubMed] [Google Scholar]
- 20. Parvizi J, Wayman J, Kelly P, et al. Combining the clinical signs improves diagnosis of scaphoid fractures: a prospective study with follow-up. J Hand Surg [Br]. 1998;23:324-327 [DOI] [PubMed] [Google Scholar]
- 21. Rettig AC, Kollias SC. Internal fixation of acute stable scaphoid fractures in the athlete. Am J Sports Med. 1996;24:182-186 [DOI] [PubMed] [Google Scholar]
- 22. Rettig AC, Weidenbener EJ, Gloyeske R. Alternative management of midthird scaphoid fractures in the athlete. Am J Sports Med. 1994;22:711-714 [DOI] [PubMed] [Google Scholar]
- 23. Riester JN, Baker BE, Mosher JF, et al. A review of scaphoid fracture healing in competitive athletes. Am J Sports Med. 1985;13:159-161 [DOI] [PubMed] [Google Scholar]
- 24. Rutgers M, Mudgal CS, Shin R. Combined fractures of the distal radius and scaphoid. J Hand Surg Eur Vol. 2008;33:478-483 [DOI] [PubMed] [Google Scholar]
- 25. Stark HH, Chao EK, Zemel NP, et al. Fracture of the hook of the hamate. J Bone Joint Surg Am. 1989;71:1202-1207 [PubMed] [Google Scholar]
- 26. Stark HH, Jobe FW, Boyes JH, et al. Fracture of the hook of the hamate in athletes. J Bone Joint Surg Am. 1977;59:575-582 [PubMed] [Google Scholar]
- 27. Strickland JW. Considerations for the treatment of the injured athlete. Clin Sports Med. 1998;17:397-400 [DOI] [PubMed] [Google Scholar]
- 28. Tay SC, Tomita K, Berger RA. The “ulnar fovea sign” for defining ulnar wrist pain: an analysis of sensitivity and specificity. J Hand Surg [Am]. 2007;32:438-444 [DOI] [PubMed] [Google Scholar]
- 29. Vinnars B, Pietreanu M, Bodestedt A, Ekenstam F, Gerdin B. Nonoperative compared with operative treatment of acute scaphoid fractures: a randomized clinical trial. J Bone Joint Surg Am. 2008;90(6):1176-1185 [DOI] [PubMed] [Google Scholar]
- 30. Weber ER, Chao EY. An experimental approach to the mechanism of scaphoid waist fractures. J Hand Surg [Am]. 1978;3:142-148 [DOI] [PubMed] [Google Scholar]




