Abstract
Background:
The impetus for the use of patellar straps in the treatment of patellar tendinopathy has largely been based on empirical evidence and not on any mechanistic rationale. A computational model suggests that patellar tendinopathy may be a result of high localized tendon strains that occur at smaller patella–patellar tendon angles (PPTAs).
Hypothesis:
Infrapatellar straps will decrease the mean localized computational strain in the area of the patellar tendon commonly involved in jumper’s knee by increasing the PPTA.
Study Design:
Controlled laboratory study.
Methods:
Twenty adult males had lateral weightbearing and nonweightbearing radiographs of their knees taken with and without 1 of 2 infrapatellar straps at 60° of knee flexion. Morphologic measurements of PPTA and patellar tendon length with and without the straps were used as input data into a previously described computational model to calculate average and maximum strain at the common location of the jumper’s knee lesion during a simulated jump landing.
Results:
The infrapatellar bands decreased the predicted localized strain (average and maximum) in the majority of participants by increasing PPTA and/or decreasing patellar tendon length. When both PPTA and patellar tendon length were altered by the straps, there was a strong and significant correlation with the change in predicted average localized strain with both straps.
Conclusion:
Infrapatellar straps may limit excessive patella tendon strain at the site of the jumper’s knee lesion by increasing PPTA and decreasing patellar tendon length rather than by correcting some inherent anatomic or functional abnormality in the extensor apparatus.
Clinical Relevance:
The use of infrapatellar straps may help prevent excessive localized tendon strains at the site of the jumper’s knee lesion during a jump landing.
Keywords: infrapatellar straps, patellar tendon strain, patellar tendinopathy, patella–patellar tendon angle, computational model
Patellar tendinopathy (jumper’s knee) is a condition usually associated with activities requiring repetitive forceful quadriceps contraction, and it is characterized by localized pain and tenderness of the patellar tendon at its origin on the inferior pole of the patella.4,11,12,30,33,35 While the precise etiopathogenesis of patellar tendinopathy is unclear, numerous studies have implicated excessive loading of the patellar tendon and increased knee flexion angles as contributing factors.4,11,12,21-23,33-35 Since the pain experienced in patellar tendinopathy has been associated with increased load on the extensor mechanism,18,24,34 it has been suggested that treatment strategies for patellar tendinopathy focus on reducing the loading of the knee extensors.15
Infrapatellar straps have been advocated for more than 30 years as a treatment to reduce anterior knee pain from a variety of sources, including patellar tendinopathy, patellar subluxation, patellar femoral syndrome, Osgood-Schlatter disease, and chondromalacia patella.2,7,8,10,20,29 In spite of the frequent use of these orthotics and the subjective report of decreased anterior knee pain experienced by the athletes wearing them,7,9,14,37 the underlying mechanisms by which patellar straps may exert their effects have not been elucidated. A recent cadaveric study demonstrated that infrapatellar straps decreased the infrapatellar fat pad pressure and reduced patellofemoral contact pressures by an average of 10%.7 However, no studies have assessed the effect of these straps on the strain occurring in the patellar tendon itself. Studies examining similar-type bands used to treat lateral epicondylitis (tennis elbow) have suggested that the bands reduce strain in the extensor carpi radialis brevis musculotendinous unit proximal to the band by limiting the magnitude of muscle contraction.1,26 In addition, the bands have been shown to change the orientation of the origin of this musculotendinous unit, which is thought to further reduce strain.26,28,38 It is possible that infrapatellar straps may also exert a positive effect in jumper’s knee patients by decreasing localized patellar tendon tension (strain) as a result of altering the orientation of the tendon origin on the inferior pole of the patella (patella–patellar tendon angle [PPTA]).
A recent study based on a computational model to predict patellar tendon strains revealed that during a simulated jump landing, the localized tendon strain at the classic location of the jumper’s knee lesion increased in association with an increase in the magnitude of applied patellar tendon strain and a decrease in the PPTA.19 It is possible that the beneficial effects that have been associated with the use of infrapatellar straps for the treatment of jumper’s knee may be a result of increasing the PPTA and thus decreasing localized patellar tendon strain. Therefore, the purpose of this study was to examine the effect of 2 commonly used infrapatellar straps on the PPTA of male participants and to use these data in a previously described computational model19 to predict relative changes in localized patellar tendon strain. We hypothesized that infrapatellar straps would decrease the mean localized strain in the area of the patellar tendon commonly involved in jumper’s knee by increasing PPTA.
Methods
This study was performed with institutional review board approval and a waiver of informed consent. Twenty men participated in this study (mean age, 34 years; range, 24-62 years). They had a mean weight of 186 lbs (84 kg), ranging from 150 to 240 lbs (68-109 kg), with no past or current history of lower extremity musculoskeletal problems in their dominant leg and no patella or patellar tendon abnormalities on physical exam or radiographic assessment. Participants were provided with the appropriately sized infrapatellar straps (Cho-Pat Knee Strap, Cho-Pat Hainesport, New Jersey; DonJoy Cross Strap, DJO, Vista, California) and instructed by a sports medicine physician (J.D.) on proper application (according to manufacturer’s instruction insert)8,10 (Figure 1). This entailed each participant’s adjusting the strap for a snug fit that did not restrict circulation. The order in which the straps were tested on each volunteer was randomized. The men had lateral radiographs of their dominant knees taken at 60° of knee flexion, during weightbearing and nonweightbearing, with and without each infrapatellar strap in place (Figure 2). Previous studies have shown that during a simulated jump landing, the patellar tendon strain is highest at 60° of knee flexion.19,31 Merchant25 views of the patella were also taken, with and without the infrapatellar straps in place (Figure 3).
Figure 1.
Participant wearing the (A) Cho-Pat Knee Strap and (B) DonJoy Cross Strap.
Figure 2.
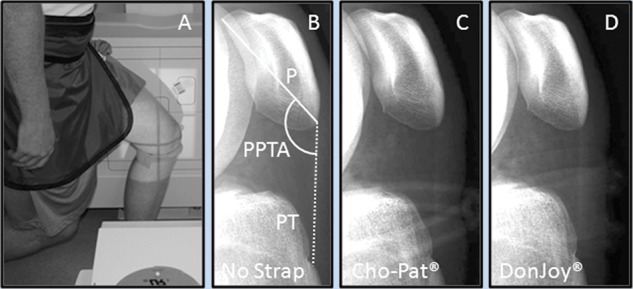
(A) participant at 60° of knee flexion during weightbearing with an infrapatellar strap in place. Representative lateral weightbearing radiographs of a participant with (B) no strap, (C) Cho-Pat Knee Strap, and (D) DonJoy Cross Strap. These images were used to obtain measurements of patella (P) height, patellar tendon (PT) length, and patella–patellar tendon angle α (PPTA).
Figure 3.
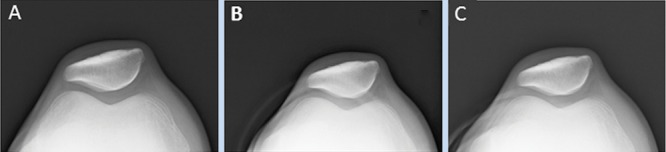
Representative Merchant view radiographs of a participant with and without the infrapatellar straps in place: A, no strap; B, Cho-Pat Knee Strap; C, DonJoy Cross Strap.
Radiographs were viewed with either DICOM Litebox software (Sorna Corporation, Eagan, Minnesota) or ImageJ software (http://rsb.info.nih.gov/ij/) to examine the effects of infrapatellar straps on patellar tilt, PPTA, and patella–tibial tuberosity distance (patellar tendon length [PTL]). The average patellar tendon thickness at 3 locations (proximal, middle, distal) along the length of the tendon was also measured from the radiographic images. In addition, the effect of infrapatellar bands on patellofemoral congruence was evaluated with a previously described radiographic analysis.25 The PPTA was measured as previously decribed.35 To eliminate potential measurement error from different radiograph scaling, PTL was expressed as a ratio of PTL to patella height17 (Figure 2). The radiographs were also used to determine the position of the patellar bands in relation to the patellar tendon. These measurements were used as input data for a previously described computational model19 to determine the effect of each infrapatellar strap on the mean and maximum localized patellar tendon strain at the site of the jumper’s knee lesion.
In the computational model, the patella and the infrapatellar straps were modeled with 2-node plane strain rigid elements (strain only within the 2-dimensional plane), and the patellar tendon was modeled with 8-node plane strain elements with neo-Hookean (nonlinear elastic) material properties of tensile modulus (E = 1000 MPa) and Poisson ratio (ν = 0.49). Tie constraints were used to join the patellar tendon and patella. The anatomic relationships of the patella and patellar tendon were determined from lateral radiographs, as were the boundaries of the insertion of the patellar tendon onto the inferior pole of the patella. The patellar band in the region of contact with the patellar tendon was modeled with a circular profile (9-mm diameter).
To account for the variability of initial nonweightbearing PPTA and PTL, changes in angle and length from nonweightbearing to weightbearing were used as input variables to the computational model. In the model, a uniform displacement was applied to the distal portion of the tendon with a rotation of the patella (ΔPTTA) at the calculated center of rotation, as well as a fixed displacement of the band, to match the band location in the radiograph, in 0.005-second intervals for 0.2 seconds (Figure 4).
Figure 4.
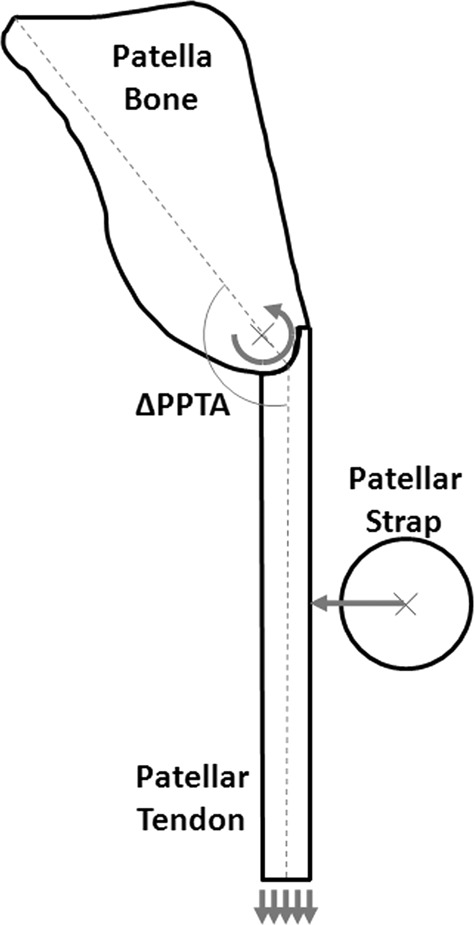
Schematic of the modeled patella–patellar tendon complex showing the uniform displacement applied to the distal portion of the patellar tendon (multiple arrows) with a rotation of the patella (ΔPTTA [patella–patellar tendon angle]) at the calculated center of rotation (curved arrow), as well as a fixed displacement of the band (single arrow), to match the strap location in the radiograph.
The finite element program ABAQUS 6.8.1 (ABAQUS, Inc, Pawtucket, Rhode Island) was used for all analyses. The maximum principal strain value at each node in a predetermined set of nodes, which corresponded to the site of the jumper’s knee lesion on magnetic resonance imaging, was averaged to give the mean localized strain value. In addition, the maximum principal strain was determined at a unique node in the location of the highest maximum principal strain. However, because the degree of material inhomogeneity of the patellar tendon is unknown, both the maximum point strain (at a single node) and the mean localized strain are reported.
Patellar tilt (patellofemoral congruence), PPTA, PTL, the computational localized patellar tendon strain average, and the maximum point strain were compared with a repeated measures analysis of variance (significance at P < 0.05). As a measure of reproducibility, the repeated measures analysis of variance was also used to determine the mean variances for the PPTA and PTL measurements. In addition, linear regression analyses were performed to determine if correlations exist between the predicted average localized strain and the change in PTL and/or PPTA.
Results
Neither infrapatellar band significantly altered patellar tilt (patellofemoral congruence).
The highest predicted localized strain (average and maximum) in all participants during weightbearing without infrapatellar straps was found at the classic location of the jumper’s knee lesion (Figure 5A). The DonJoy Cross Strap reduced the average and maximum computational localized weightbearing patellar strain in this location in 15 of 20 participants, whereas the Cho-Pat Knee Strap reduced the average and maximal computational localized weightbearing patellar strain in this location in 16 of 20 participants (Figure 5B, 5C). Three volunteers had no predicted decrease in their average or maximum localized tendon strain with either infrapatellar strap. There was no significant difference in the predicted initial (no strap) localized weightbearing patellar strain between participants who demonstrated a decrease in strain with either infrapatellar strap and those who did not. In addition, there was no significant difference in initial PTL or average patellar tendon thickness between participants who demonstrated a decrease in strain with either infrapatellar strap and those who did not.
Figure 5.
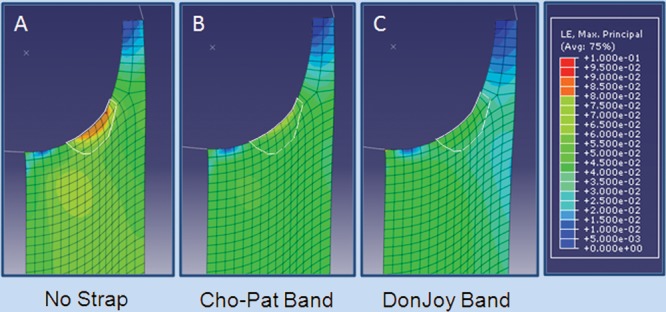
Representative finite element analysis demonstrating a decrease in the average localized tendon strain at the location of the jumper’s knee lesion with the infrapatellar straps in place: A, no strap; B, Cho-Pat Knee Strap; C, DonJoy Cross Strap.
For the 15 participants in which the DonJoy Cross Strap reduced the average localized weightbearing patellar tendon strain, this strain was reduced an average of 34.0% (range, 2.5%-87.6%), and the maximal local strain was reduced an average of 32.3% (range, 2.8%-84.0%) (Table 1). The DonJoy Cross Strap increased PPTA in 13 of these 15 volunteers and reduced PTL in 14 of them. The DonJoy Cross Strap increased both the PPTA and the PTL in 12 of these participants. Among the 5 volunteers in whom the DonJoy Cross Strap produced no reduction in computational localized weightbearing patellar tendon strain, 3 had increased PPTA and 3 had reduced PTL. Only 1 of these 5 had both increased PPTA and reduced PTL; however, neither of these changes were significant.
Table 1.
Values for participants in which the infrapatellar straps decreased localized tendon strain.
| Cho-Pata | DonJoyb | |||
|---|---|---|---|---|
| No Strap | Cho-Pat | No Strap | DonJoy | |
| Local strain, % | ||||
| Average | 6.72 ± 2.50 | 5.70 ± 2.66c | 6.97 ± 2.79 | 5.02 ± 3.10c |
| Maximum | 9.03 ± 3.24 | 7.68 ± 3.49c | 9.35 ± 3.61 | 6.79 ± 4.01c |
| Patella–patellar tendon angle | ||||
| Weightbearing | 142.7 ± 6.1 | 143.8 ± 6.0c,d | 143.3 ± 6.4d | 144.7 ± 5.7c,d |
| Nonweightbearing | 144.2 ± 5.9 | 146.2 ± 6.5c | 145.3 ± 5.8 | 147.0 ± 6.5c |
| Patellar tendon length/patella length | ||||
| Weightbearing | 1.23 ± 0.17d | 1.22 ± 0.17c,d | 1.25 ± 0.19d | 1.23 ± 0.19c,d |
| Nonweightbearing | 1.17 ± 0.16 | 1.17 ± 0.16 | 1.18 ± 0.17 | 1.17 ± 0.18 |
n = 16 of 20.
n = 15 of 20.
Significantly different from no-strap condition (P ≤ 0.05).
Significantly different from nonweightbearing (P ≤ 0.05).
The Cho-Pat Knee Strap reduced the average localized weightbearing patellar tendon strain in 16 volunteers an average of 19.6% (range, 0.9%-62.5%) and the maximal local strain, an average of 19.2% (range, 1%-59%) (Table 1). The Cho-Pat Knee Strap increased PPTA in 13 of these 16 and reduced PTL in 13 of these 16 volunteers. The Cho-Pat Knee Strap increased both the PPTA and the PTL in 10 volunteers. Among the 4 participants in whom the Cho-Pat Knee Strap produced no reduction in computational localized weightbearing patellar tendon strain, 2 had increased PPTA and 2 had reduced PTL.
An increase in the PPTA was not significantly correlated with a decrease in the predicted average localized strain in either the DonJoy Cross Strap (r2 = 0.14, P = 0.18) or the Cho-Pat Knee Strap (r2 = 0.14, P = 0.151). However, a decrease in PTL demonstrated a moderate but significant correlation with a decrease in the predicted average localized strain with both the DonJoy Cross Strap (r2 = 0.70, P < 0.0001) and the Cho-Pat Knee Strap (r2 = 0.44, P = 0.0002). When PPTA and PTL were examined together, there was a strong and significant correlation with the predicted average localized strain with the both the DonJoy Cross Strap (r2 = 0.88, P < 0.001) and the Cho-Pat Knee Strap (r2 = 0.85, P = 0.001).
During nonweightbearing, the PPTA was significantly increased in 15 of 20 participants by the DonJoy Cross Strap and 16 of 20 by the Cho-Pat Knee Strap. Two had no increase in PPTA with either infrapatellar strap. During nonweightbearing, the PTL was significantly decreased in 17 of 20 volunteers by the DonJoy Cross Strap and 15 of 20 by the Cho-Pat Knee Strap. Two had no decrease in PTL with either infrapatellar strap.
The mean variance of the PPTA and PTL measurements were 0.186° and 0.196, respectively. These values represent a high degree of reproducibility in these measurements.
Discussion
The use of patellar orthotics (patellofemoral braces, infrapatellar bands, and taping) has long been advocated as an adjunct to conservative treatment of anterior knee pain resulting from a variety of conditions related to the patellofemoral joint.§ Many of these orthotics have been developed to treat the most commonly accepted etiology of anterior knee pain: malalignment of the patellar femoral joint.16 Thus, most patellofemoral braces are designed to reduce compression of the patella as well as prevent excessive lateral shifting of the patella.27 Although athletes report a subjective benefit in wearing a variety of patellofemoral orthotics, especially in running and jumping sports,7,14,37 the underlying mechanism (or mechanisms) by which this improvement occurs is unclear.7 While infrapatellar straps have been successfully used to treat generalized anterior knee pain7,14,20 and have been advocated by manufacturers for treating patellar tendinitis and overuse injuries of the patellar tendon,8,10 a literature PubMed search (November 8, 2010) did not reveal a single peer-reviewed publication that has critically examined the use of infrapatellar straps in the treatment of patellar tendinopathy.
The results of the current study suggest that infrapatellar straps reduced the predicted average and maximum localized tendon strain at the site of the jumper’s knee in the majority of volunteers tested. A previous study using the same computational model identified the PPTA and the level of applied tendon strain as significant covariables in determining the predicted localized strain at the site of the jumper’s knee lesion.19 In the current study, there was a strong and significant correlation between the ability of the infrapatellar straps to increase the PPTA and decrease the PTL (which indirectly decreased patellar tendon strain) and their ability to lessen the predicted average and maximum localized patellar tendon strain.
There was also a significant increase in PTL between nonweightbearing and weightbearing with both straps. The effect of this difference in PTL on localized patellar tendon strain in the nonweightbearing tendon just before impact during a jump landing is unknown. It is possible that this decrease in nonweightbearing PTL could further affect the influence of the infrapatellar straps on localized tendon strain.
As previously noted, the infrapatellar straps did not reduce the predicted localized tendon strain in all participants. The reason (or reasons) for this is unclear because there was no significant difference in the thickness or length of the patellar tendon and no obvious differences in patella anatomy between those who demonstrated a predicted decrease in local tendon strain with the straps and those who did not. Note that although the participants received instructions on the proper application of these straps, no additional attempt was made to standardize the strap tightness among them. A study examining the use of tennis elbow straps (lateral epicondylitis bands) noted that the level of strap tightness played a role in forces at the lateral epicondyle.26 Therefore, the lack of apparent efficacy in some participants in the current study may be due to variations in band tightness, as well as potential differences in tissue compliance.
The inability of infrapatellar straps to produce a demonstrable effect in all participants was observed in a previous study that examined the effect of an infrapatellar strap in relieving patellofemoral pain.20 In that study, 77% of patients (41 of 53) who wore the strap experienced enough subjective pain relief to resume normal activities.20 The study also demonstrated that by wearing the strap, 75% of the patients with symptoms < 2 months improved and 88% of patients with symptoms > 1 year benefited as well.20 The infrapatellar strap also resulted in a higher percentage of subjective pain relief in males (88%) compared to females (71%).20 However, the potential reasons for these differences were not examined.
Similar to a previous investigation, the current study found that infrapatellar straps did not alter patellofemoral congruity.7 Studies have suggested that changes in patellar alignment by themselves may not be responsible for pain alleviation after patellar bracing.6,32 Thus, it is possible that the predicted decrease in localized tendon strain could be a factor in the perceived decrease in pain reported with the use of these straps.9,20
The current study was done in a single-sex population with no evidence of patella or patellar tendon abnormalities (by history, physical examination, or radiographs). While it is possible that the infrapatellar straps could have had a different effect in tendinopathy patients, an elegant clinical study reported no significant differences in the PPTAs or inferior pole anatomy between patients with and without symptomatic patellar tendinopathy.35 Thus, infrapatellar straps may simply serve to limit excessive patella tendon strain at the site of the jumper’s knee lesion by increasing PPTA and decreasing PTL rather than by correcting some inherent anatomic or functional abnormality in the extensor apparatus.
Although the infrapatellar straps were found to decrease the predicted patellar tendon strain at the site of the jumper’s knee lesion in these noninjured volunteers by the aforementioned mechanisms, it is unclear how or if reducing tendon strain would contribute to the resolution of symptoms or alter the pathology of a patient suffering from patellar tendinopathy. Likewise, the ability of an infrapatellar strap to prevent patellar tendinopathy cannot be predicted from this study. Prospective randomized clinical trials are needed to ultimately determine the efficacy of infrapatellar straps in the treatment and/or prevention of patellar tendinopathy.
Footnotes
References
- 1. Altan L, Kanat E. Conservative treatment of lateral epicondylitis: comparison of two different orthotic devices. Clin Rheumatol. 2008;27:1015-1019 [DOI] [PubMed] [Google Scholar]
- 2. American Academy of Orthopaedic Surgeons Athletic Training and Sports Medicine. 2nd ed. Park Ridge, IL: American Academy of Orthopaedic Surgeons; 1991:716 [Google Scholar]
- 3. Aminaka N, Gribble P. A systematic review of the effects of therapeutic taping on patellofemoral pain syndrome. J Athl Train. 2005;40(4):341-351 [PMC free article] [PubMed] [Google Scholar]
- 4. Andres BM, Murrell GAC. Treatment of tendinopathy. Clin Orthop Relat Res. 2008;466:1539-1554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bizzini M, Childs JD, Piva SR, Delitto A. Systematic review of the quality of randomized control trials for patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2003;33:4-20 [DOI] [PubMed] [Google Scholar]
- 6. Bockrath K, Wooden C, Worrell T, Ingersoll CD, Farr J. Effects of patellar taping on patellar position and perceived pain. Med Sci Sports Exerc. 1993;25:989-992 [PubMed] [Google Scholar]
- 7. Bohnsack M, Halcour A, Klages P, et al. The influence of patellar bracing on patellar and knee load-distribution and kinematics: an experimental cadaver study. Knee Surg Sports Traumatol Arthrosc. 2008;16:135-141 [DOI] [PubMed] [Google Scholar]
- 8. Cho-Pat Knee Strap [product] Hainesport, NJ: Cho-Pat [Google Scholar]
- 9. D’hondt NE, Struijs PA, Kerkhoffs GM, et al. Orthotic devices for treating patellofemoral pain syndrome. Cochrane Database Syst Rev. 2002;2:CD002267 [DOI] [PubMed] [Google Scholar]
- 10. DonJoy Cross Strap [product] Vista, CA: DJO [Google Scholar]
- 11. Ferretti A. Epidemiology of jumper’s knee. Sports Med. 1986;3:289-295 [DOI] [PubMed] [Google Scholar]
- 12. Ferretti A, Ippolito E, Mariani P, Puddu G. Jumper’s knee. Am J Sports Med. 1983;11:58-62 [DOI] [PubMed] [Google Scholar]
- 13. Fulkerson JP. Diagnosis and treatment of patients with patellar-femoral pain. Am J Sports Med. 2002;30:447-456 [DOI] [PubMed] [Google Scholar]
- 14. Gerrard DF. External knee support in rugby union: effectiveness of bracing and taping. Sports Med. 1998;25:313-317 [DOI] [PubMed] [Google Scholar]
- 15. Grau S, Maiwald C, Krauss I, Axmann D, Janssen P, Horstmann T. What are the causes and treatment strategies for patellar-tendinopathy in female runners? J Biomech. 2008;41:2042-2046 [DOI] [PubMed] [Google Scholar]
- 16. Gravlee JR, van Durme DJ. Braces and splints for musculoskeletal conditions. Am Fam Physician. 2007;75:342-348 [PubMed] [Google Scholar]
- 17. Insall J, Salvati E. Patella position in the normal knee. Radiology. 1971;101:101-104 [DOI] [PubMed] [Google Scholar]
- 18. Kujala UM, Aalto T, Osterman K, Dahlstrom S. The effect of volleyball playing on the knee extensor mechanism. Am J Sports Med. 1989;17:766-769 [DOI] [PubMed] [Google Scholar]
- 19. Lavagnino M, Arnoczky S, Elvin N, Dodds J. Patellar tendon strain is increased at the site of the jumper’s knee lesion during knee flexion and tendon loading. Am J Sports Med. 2008;36:2110-2118 [DOI] [PubMed] [Google Scholar]
- 20. Levine J, Splain S. Use of the infrapatellar strap in the treatment of patellofemoral pain. Clin Orthop Relat Res. 1979;139:179-181 [PubMed] [Google Scholar]
- 21. Lian Ø, Engebretsen L, Ovrebø RV, Bahr R. Characteristics of the leg extensors in male volleyball players with jumper’s knee. Am J Sports Med. 1996;24(3):380-385 [DOI] [PubMed] [Google Scholar]
- 22. Lian Ø, Refsnes PE, Engebretsen L, Bahr R. Performance characteristics of volleyball players with patellar tendinopathy. Am J Sports Med. 2003;31(3):408-413 [DOI] [PubMed] [Google Scholar]
- 23. Lian Ø, Scott A, Engebretsen L, Bahr R, Duronio V, Khan K. Excessive apoptosis in patellar tendinopathy in athletes. Am J Sports Med. 2007;5(4):605-611 [DOI] [PubMed] [Google Scholar]
- 24. Lorbach O, Diamantopoulos A, Kammerer K-P, Paesler HH. The influence of the lower patellar pole in the pathogenesis of chronic patellar tendinopathy. Knee Surg Sports Traumatol Arthrosc. 2008;16:348-352 [DOI] [PubMed] [Google Scholar]
- 25. Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391-1396 [PubMed] [Google Scholar]
- 26. Meyer NJ, Pennington W, Haines B, Daley R. The effect of the forearm support band on forces at the origin of the extensor carpi radialis brevis: a cadaveric study and review of literature. J Hand Ther. 2002;15(2):179-184 [DOI] [PubMed] [Google Scholar]
- 27. Nadler R, Nadler S. Assistive devices and lower extremity orthotics in the treatment of osteoarthritis. Phys Med Rehabil. 2001;15:57-64 [Google Scholar]
- 28. Nirschl RP. Tennis elbow. Orthop Clin North Am. 1973;4:787-800 [PubMed] [Google Scholar]
- 29. Nyland J. Clinical Decisions in Therapeutic Exercise: Planning and Implementation. Upper Saddle River, NJ: Pearson Pretice Hall; 2006:263-264 [Google Scholar]
- 30. Peers KH, Lysens RJ. Patellar tendinopathy in athletes: current diagnostic and therapeutic recommendations. Sports Med. 2005;35:71-87 [DOI] [PubMed] [Google Scholar]
- 31. Pflum MA, Shelbourne KB, Torry MR, Decker MJ, Pandy MG. Model prediction of anterior ligament force during drop landings. Med Sci Sports Exerc. 2004;36:1949-1958 [DOI] [PubMed] [Google Scholar]
- 32. Powers CM, Ward SR, Chan LD, Chen YJ, Terk MR. The effect of bracing on patella alignment and patellofemoral joint contact area. Med Sci Sports Exerc. 2004;36(7):1226-1232 [DOI] [PubMed] [Google Scholar]
- 33. Rees JD, Maffuli N, Cook J. Management of tendinopathy. Am J Sports Med. 2009;37:1855-1867 [DOI] [PubMed] [Google Scholar]
- 34. Richards DP, Ajemian SV, Wiley P, Zernicke RF. Knee joint dynamics predict patellar tendonitis in elite volleyball players. Am J Sports Med. 1996;24:676-683 [DOI] [PubMed] [Google Scholar]
- 35. Schmid MR, Hodler J, Cathrein P, Duewell S, Jacob HA, Romero J. Is impingement the cause of jumper’s knee? Dynamic and static magnetic resonance imaging of patellar tendinitis in an open-configuration system. Am J Sports Med. 2001;30:388-395 [DOI] [PubMed] [Google Scholar]
- 36. Selfe J, Richards J, Thewlis D, Kilmurray S. The biomechanics of step decent under different treatment modalities used in patellofemoral pain. Gait Posture. 2008;27:258-263 [DOI] [PubMed] [Google Scholar]
- 37. Van Tiggelen D, Witrouw E, Roget P, Cambier D, Danneels L, Verdonk R. Effect of bracing on the prevention of anterior knee pain-a prospective randomized study. Knee Surg Sports Traumatol Arthrosc. 2004;12:434-439 [DOI] [PubMed] [Google Scholar]
- 38. Wadsworth CT, Nielsen DH, Burns LT, Krull JD, Thompson CG. Effect of the counterforce armband on wrist extension and grip strength and pain in subjects with tennis elbow. J Orthop Sports Phys Ther. 1989;11:192-197 [DOI] [PubMed] [Google Scholar]
- 39. Warden SJ, Hinman RS, Watson MA, Jr, et al. Patellar taping and bracing for the treatment of chronic knee pain: a systematic review and meta-analysis. Arthritis Rheum. 2008;59:73-83 [DOI] [PubMed] [Google Scholar]


