Abstract
Context:
Double-row rotator cuff repair methods have improved biomechanical performance when compared with single-row repairs.
Objective:
To review clinical outcomes of single-row versus double-row rotator cuff repair with the hypothesis that double-row rotator cuff repair will result in better clinical and radiographic outcomes.
Data Sources:
Published literature from January 1980 to April 2010. Key terms included rotator cuff, prospective studies, outcomes, and suture techniques.
Study Selection:
The literature was systematically searched, and 5 level I and II studies were found comparing clinical outcomes of single-row and double-row rotator cuff repair. Coleman methodology scores were calculated for each article.
Data Extraction:
Meta-analysis was performed, with treatment effect between single row and double row for clinical outcomes and with odds ratios for radiographic results. The sample size necessary to detect a given difference in clinical outcome between the 2 methods was calculated.
Results:
Three level I studies had Coleman scores of 80, 74, and 81, and two level II studies had scores of 78 and 73. There were 156 patients with single-row repairs and 147 patients with double-row repairs, both with an average follow-up of 23 months (range, 12-40 months). Double-row repairs resulted in a greater treatment effect for each validated outcome measure in 4 studies, but the differences were not clinically or statistically significant (range, 0.4-2.2 points; 95% confidence interval, –0.19, 4.68 points). Double-row repairs had better radiographic results, but the differences were also not statistically significant (P = 0.13). Two studies had adequate power to detect a 10-point difference between repair methods using the Constant score, and 1 study had power to detect a 5-point difference using the UCLA (University of California, Los Angeles) score.
Conclusions:
Double-row rotator cuff repair does not show a statistically significant improvement in clinical outcome or radiographic healing with short-term follow-up.
Keywords: rotator cuff repair, outcomes, double row, prospective studies
Rotator cuff tears are one of the most common orthopaedic disorders, and they occur in patients with a wide range of ages. Repair approaches have progressed over time from open techniques to mini-open, arthroscopic-assisted, and arthroscopic techniques. Repair methods have evolved as well, from single-row (SR) transosseous or suture anchor repairs to double-row (DR) suture anchor and suture bridge techniques. Biomechanical studies have demonstrated anatomic footprint restoration, diminished contact pressure, and increased contact area of DR repair methods.1,6,13,14,16,17,24 A recent systematic review found lower retear rates in DR versus SR repairs when structural healing was assessed by clinical imaging.7 Individual clinical studies show a trend toward improved healing of DR over SR repairs but are limited by small numbers and are often retrospective.11,25
The purpose of our study was to determine whether SR or DR rotator cuff repair was significantly better in terms of clinical outcomes (as measured by functional assessment scores) and structural healing (as assessed by postoperative imaging). The hypothesis was that DR rotator cuff repair would result in better clinical and radiographic outcomes.
Methods
Literature Search
A search was performed of Medline, Pubmed, Cochrane Database of Systematic Reviews, American College of Physicians Journal Club, Database of Abstracts of Reviews of Effects, and Cochrane Central Register of Controlled Trials (Figure 1) to find relevant articles on rotator cuff repair published from January 1980 to April 2010.8 Studies were included if they assessed the results of repair according to repair method in a comparative fashion, contained a detailed description of the operative technique, allowed extraction of data on clinical outcomes (strength, range of motion, functional assessment scales) according to repair method, and used validated outcome scores (American Shoulder and Elbow Surgeons [ASES]; Disabilities of the Arm, Shoulder, and Hand [DASH]; University of California Los Angeles [UCLA]; Constant; and/or Western Ontario Rotator Cuff Index [WORC]) as a primary means of patient assessment at a minimum of 1 year following surgery. Because of a paucity of studies on DR rotator cuff repair with 2-year follow-up, studies were selected with 1-year outcomes. Retrospective or level III or IV studies were excluded. The references of included articles were reviewed for articles not identified by the literature search. The authors of the included studies were contacted to acquire primary data and clarify outcome measures. Results were analyzed according to repair method and grouped as SR or DR suture anchor.
Figure 1.
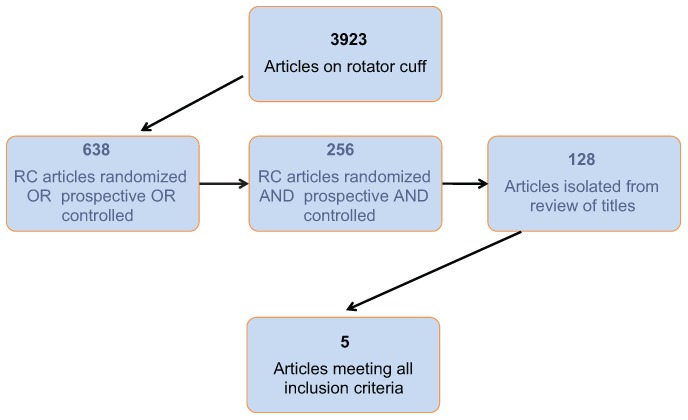
Literature search.
Methodology Scoring
A Coleman methodology score was independently calculated for each eligible study by 2 researchers, who resolved conflicting assessments (Table 1).4
Table 1.
Coleman methodology scores for each study.
| Min-Max | Franceschi9 | Grasso10 | Burks2 | Park20 | Charousset3 | |
|---|---|---|---|---|---|---|
| Study size | 0-10 | 7 | 10 | 10 | 10 | 10 |
| Mean follow-up | 0-5 | 2 | 5 | 2 | 5 | 5 |
| No. procedures | 0-15 | 0 | 0 | 0 | 0 | 0 |
| Type of study | 0-1 | 15 | 15 | 15 | 10 | 10 |
| Diagnostic certainty | 0-5 | 5 | 5 | 5 | 5 | 5 |
| Surgical description | 0-5 | 5 | 5 | 5 | 5 | 5 |
| Rehab description | 0-10 | 10 | 10 | 10 | 10 | 10 |
| Outcome criteria | 0-10 | 10 | 8 | 10 | 10 | 10 |
| Outcome assessment | 0-15 | 5 | 8 | 8 | 5 | 8 |
| Patient selection | 0-15 | 15 | 15 | 15 | 10 | 15 |
| Total | 74 | 81 | 80 | 73 | 78 |
Meta-analysis
The treatment effect between the SR and DR rotator cuff repair methods for each clinical variable was the postoperative mean difference. For imaging results, the odds ratio was used to compare the probability of anatomic and watertight healing. The overall treatment effect for each variable was estimated with the minimum-variance estimator, commonly used in the context of meta-analyses and defined as the linear combination of the study-specific treatment effects inversely weighted by their corresponding estimated sampling variances. Estimates of the sampling variance for each study-specific treatment effect were obtained directly from the individual study reports or extracted using the available statistical quantities.15 For each overall treatment effect, a corresponding 95% confidence interval was computed on the basis of asymptotic normality of the sampling distributions. The log odds ratio was used instead of the odds ratio when results were combined, because the sampling distribution is better approximated in this case. All analyses were performed using SAS 9.2.
Sample Size Calculation
A clinically significant difference between repair methods was defined as a postoperative improvement of 2 and 5 points (UCLA score) or 5 and 10 points (all other scoring scales). Published standard deviations of these scores were used to calculate the sample size necessary to detect these differences for each clinical outcome score. The clinically significant difference for the postoperative improvement was based on previously published studies.5,14,24 There is no validated clinical difference for the Constant score.22 Five points was chosen for a clinically important difference in the Constant score on the basis of noninjured individuals according to age.5,12 An effect size (or clinical difference) of 2 and 5 points for the UCLA score was used; a difference of 2 at the upper end of the scale separates good and excellent, whereas > 5-point differences are found between poor and fair, fair and good.8 Sample sizes were calculated for a 5-point effect because the minimal clinically important difference for the ASES score is close to 5, at 6.4.18,21 Ten points was also used for a sample size calculation; the minimal clinically important difference for the DASH score was 10.2 (DASH correlates well with ASES and Constant).18,21,23
Results
Literature Search
Of the 128 abstracts reviewed, 5 articles met the inclusion criteria and were the foundation of this study (Figure 1)—specifically, 3 level I randomized controlled trials2,9,10 and 2 prospective cohort studies,3,20 yielding 156 patients with SR repairs and 147 with DR repairs. These studies were arthroscopic repairs with suture anchors. Transosseous suture bridge or combined techniques were not included. The studies did not include individual patient data, only averages for the patients with SR versus DR repair. The average Coleman score for all studies was 77.2; for level I studies, 78.3; for level II, 75.5 (Table 1).
Clinical Outcomes
The average age for SR repairs was 58.5 years and for DR repairs, 56.9 years. The average follow-up was 23.4 months for SR repairs and 23.5 months for DR. Only 1 study required a minimum of 24 months’ follow-up3; 3 studies2,9,20 included patients with less than 24 months’ follow-up (Table 2). Patient-oriented outcome measures varied among studies (Table 3).
Table 2.
Population data and clinical assessments used in the included studies.a
| Constant2,3,20 | DASH10 | ASES2,20 | UCLA2,9 | WORC2 | |
|---|---|---|---|---|---|
| Studies, n | 3 | 1 | 2 | 2 | 1 |
| Repairs, n | |||||
| SR | 93 | 37 | 60 | 46 | 20 |
| DR | 86 | 35 | 58 | 46 | 20 |
| SR | |||||
| Age, y | 57.1 | 58.3 | 56.7 | 60.2 | 56 |
| Follow-up, mon | 23.2 | 24.8 | 20.7 | 17.9 | 12 |
| Tear size | N/A | 244.7 mm2 | < 3 cm, n = 43 | 1-3 cm, n = 18 | 1-3 cm, n = 18 |
| > 3 cm, n = 17 | > 3 cm, n = 28 | > 3 cm, n = 2 | |||
| DR | |||||
| Age, y | 56.8 | 55.2 | 55.3 | 58.5 | 57 |
| Follow-up, mon | 23.2 | 24.8 | 20.6 | 17.9 | 12 |
| Tear size | N/A | 261.9 mm2 | < 3 cm, n = 36 | 1-3 cm, n = 15 | 1-3 cm, n = 15 |
| > 3 cm, n = 22 | > 3 cm, n = 31 | > 3 cm, n = 5 |
SR, single row; DR, double row; Constant, Constant-Murley; DASH, Disabilities of the Arm, Shoulder, and Hand; ASES, American Shoulder and Elbow Surgeons; UCLA, University of California, Los Angeles; WORC, Western Ontario Rotator Cuff Index.
Table 3.
Meta-analysis of clinical outcomes: double-row versus single-row rotator cuff repair.a
| Single Row | Double Row | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Endpoint | nb | Mean | SD | nb | Mean | SD | Point Estimate | SE of Estimate | 95% CI |
| Constant | |||||||||
| Burks2 | 20 | 77.8 | 9 | 20 | 74.4 | 18.4 | −3.40 | 4.58 | −12.79, 5.99 |
| Charousset3 | 35 | 80.7 | 9.6 | 31 | 82.7 | 9.6 | 2.00 | 2.37 | −2.73, 6.73 |
| Park20 | 40 | 76.68 | 8.56 | 38 | 79.66 | 4.52 | 2.98 | 1.54 | −0.1, 6.06 |
| Overall | 2.24 | 1.24 | −0.19, 4.68 | ||||||
| ASES | |||||||||
| Burks2 | 20 | 85.9 | 14 | 20 | 85.5 | 20 | −0.40 | 5.46 | −11.49, 10.69 |
| Park20 | 40 | 91.6 | 4.48 | 38 | 92.97 | 2.27 | 1.37 | 0.80 | 0.23, 2.97 |
| Overall | 1.33 | 0.79 | −0.22, 2.88 | ||||||
| UCLA | |||||||||
| Burks2 | 20 | 28.6 | 3.6 | 20 | 29.5 | 5.6 | 0.90 | 1.49 | −2.13, 3.93 |
| Franceschi9 | 26 | 32.9 | 1.17 | 26 | 33.3 | 0.97 | 0.40 | 0.30 | −0.2, 1.0 |
| Overall | 0.42 | 0.29 | −0.15, 0.99 | ||||||
Meta-analysis of mean diff (double row minus single row). ASES, American Shoulder and Elbow Surgeons; UCLA, University of California, Los Angeles; CI, confidence interval.
Sample size.
We were unable to analyze repair results according to tear size or number of anchors, owing to lack of detail in the studies. Strength was recorded as an individual variable in 3 studies2,3,20 but was measured differently among them, thus not allowing direct comparison. Range of motion was recorded independently in 1 study9; pain, activity, and subjective satisfaction were also recorded independently in only 1 study.3
Radiographic Outcomes
Radiographic assessment of structural healing (odds ratios of anatomic and watertight healing) was performed for 81 SR and 77 DR rotator cuff repair in 3 studies (Table 4).
Table 4.
Imaging results for single-row and double-row rotator cuff repairs.
| Burks2 | Charousset3 | Franceschi9 | Combined | |
|---|---|---|---|---|
| Method | Nonarthrographic MRI | Arthrographic CT | Arthrographic MRI | |
| Timing | 6 wk, 3 mo, 12 moa | 6 mo | 22.5 mo | 13 mo (average) |
| Single rowb | ||||
| n | 20 | 35 | 26 | 81 |
| Full-thickness tears | 2 (10) | 14 (40) | 2 (7.7) | 18 (22.2) |
| Partial-thickness tears | 0 | 7 (20) | 10 (38.5) | 17 (21) |
| Intact tendons | 18 (90) | 14 (40) | 14 (53.8) | 46 (56.8) |
| Double rowb | ||||
| n | 20 | 31 | 26 | 77 |
| Full-thickness tears | 2 (10) | 7 (22.6) | 1 (3.9) | 10 (13) |
| Partial-thickness tears | 2 (10) | 5 (16.1) | 7 (26.9) | 14 (18.2) |
| Intact tendons | 16 (80) | 19 (61.3) | 18 (69.2) | 53 (68.8) |
| Log of odds ratio | ||||
| Anatomic healingc | −0.81 (−2.64, 1.02) | 0.86 (−0.12, 1.85) | 0.66 (−0.48, 1.79) | 0.55 (−0.14, 1.24) |
| Watertight healingd | 0.00 (−2.07, 2.07) | 0.83 (−0.25, 1.91) | 0.73 (−1.73, 3.20) | 0.66 (−0.23, 1.55) |
Burks performed MRI at multiple points; the published data were from the final follow-up, at 12 months. CT, computed tomography.
n (%).
Intact tendon on postoperative imaging study.
Intact tendon or partial thickness tear on postoperative imaging study.
Sample Size Calculations
Ten patients were needed per repair method for detection of a 5-point difference in UCLA score with a standard deviation of 4 points (Table 5). Furthermore, 250 patients per repair method were needed for detection of a 5-point difference in Constant, ASES, or Western Ontario Rotator Cuff Index scores with a standard deviation of 20 points. Based on these calculations, the Grasso study10 was adequately powered to detect a 10-point difference on the Constant and DASH scores. The Park20 study was adequately powered to detect a 10-point difference on the Constant score. The Franceschi9 study was adequately powered to detect a 5-point difference on the UCLA scale. Burks2 and Charousset3 were both underpowered to detect a 10-point difference on the Constant scale. No study was adequately powered to detect a 5-point difference on the Constant, ASES, or Western Ontario Rotator Cuff Index scores or a 2-point difference on the UCLA scale.
Table 5.
Number of patients needed per group for varying effect size and standard deviation.a
| Effect Size | ||||
|---|---|---|---|---|
| Scoring System | Standard Deviationsb | 2 Points | 5 Points | 10 Points |
| ASES2,20 | 15-20 | 148-250 | 35-64 | |
| Constant2,3,20 | 10-20 | 40-250 | 17-64 | |
| DASH10 | 10-18 | 40-200 | 17-52 | |
| UCLA9,10 | 4-6 | 60-128 | 10-22 | |
| WORC2 | 15-20 | 148-250 | 35-64 | |
Calculated for α = 0.05 and power = 0.80. The range shows the number of patients needed, as calculated from the lower standard deviation to the higher standard deviation.
The standard deviations are taken from the published results of the studies composing the foundation of our study: Constant, Constant-Murley; DASH, Disabilities of the Arm, Shoulder, and Hand; ASES, American Shoulder and Elbow Surgeons; UCLA, University of California, Los Angeles; WORC, Western Ontario Rotator Cuff Index.
Discussion
We were unable to support our hypothesis that DR rotator cuff repair would lead to better clinical and radiographic results compared with SR. For the 3 clinical scoring systems with adequate data, the 95% confidence intervals of the postoperative mean difference for each analyzed score contained zero. Although the majority of treatment effect favored DR repair, no study or score absolutely favored it.
We did not find a statistically significant difference among radiographic outcomes. This may be due to the inclusion of various sized tears (< 1 cm to > 3 cm), which have different rates of healing.8,12,13 Despite randomization, all 3 studies that reported tear size had larger tears in the DR group (Table 2).
In an effort to objectively analyze the quality of the studies reviewed, Coleman methodology scores were independently assigned to each study (Table 1).4 All studies specifically included other procedures or did not clearly specify their exclusion—particularly, biceps tenotomy/tenodesis or distal clavicle excision. Thus, it is hard to ascribe the results solely to rotator cuff repair. Studies also lost points in assessing outcomes: Investigators were not independent of the surgeon; written assessments were not completed; or assessments were not completed by the patients themselves.
The meta-analysis was limited by the clinical assessment used in each study. Grasso et al10 used the “total Constant score normalized for age and gender” and compared outcomes “with adjustment for baseline values.” Whereas normalization or adjustment of the Constant score allows comparison of a specific patient population to a matched standard, without the primary individual patient data, it is difficult to understand how a patient could have a score greater than the maximum of 100.10 Comparison of normalized Constant scores may be erroneous if adjustment is not performed using the same calculation reference table.12 The Grasso Constant score data were not included in the meta-analysis.
Use of different scoring scales, even within the same patient samples, may yield varying results because functional assessment assigns different weights to the various domains. The magnitude of a clinically important difference varies among scores and is necessary to appropriately power a study (Table 5).
There have been 2 recent systematic reviews published comparing clinical outcomes of DR versus SR rotator cuff repair.19,26 This study differs in that the results from each level I and II study were combined and analyzed to detect differences in clinical outcomes between SR and DR rotator cuff repairs with larger numbers. In addition, rather than highlight biases, the methodology was analyzed using Coleman scores.
Strengths of this study are the predefined inclusion and exclusion criteria for level I and II studies. In addition, the studies were ranked according to Coleman criteria to assess the quality of the studies. Weaknesses include the small number of extractable cases and the inability to obtain primary data on tear size from the majority of authors.
Conclusions
Compared with SR, DR rotator cuff repair methods are more time-consuming, use more implants, and are more expensive.9 Their use should be justified by well-designed level I studies. The 5 studies analyzed present the highest level evidence available. Even these studies were limited by low Coleman scores (n = 5), short-term follow-up (n = 5), lack of radiographic assessment of healing (n = 2), inconsistent use of scoring systems (n = 2), and small sample size (n = 4).
References
- 1. Brady PC, Arrigoni P, Burkhart SS. Evaluation of residual rotator cuff defects after in vivo single- versus double-row rotator cuff repairs. Arthroscopy. 2006;22(10):1070-1075 [DOI] [PubMed] [Google Scholar]
- 2. Burks RT, Crim J, Brown N, Fink B, Greis PE. A prospective randomized clinical trial comparing arthroscopic single- and double-row rotator cuff repair: magnetic resonance imaging and early clinical evaluation. Am J Sports Med. 2009;37(4):674-682 [DOI] [PubMed] [Google Scholar]
- 3. Charousset C, Grimberg J, Duranthon LD, Bellaiche L, Petrover D. Can a double-row anchorage technique improve tendon healing in arthroscopic rotator cuff repair? A prospective, nonrandomized, comparative study of double-row and single-row anchorage techniques with computed tomographic arthrography tendon healing assessment. Am J Sports Med. 2007;35(8):1247-1253 [DOI] [PubMed] [Google Scholar]
- 4. Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10(1):2-11 [DOI] [PubMed] [Google Scholar]
- 5. Constant CR, Gerber C, Emery RJ, Sojbjerg JO, Gohlke F, Boileau P. A review of the Constant score: modifications and guidelines for its use. J Shoulder Elbow Surg. 2008;17(2):355-361 [DOI] [PubMed] [Google Scholar]
- 6. Domb BG, Glousman RE, Brooks A, Hansen M, Lee TQ, ElAttrache NS. High-tension double-row footprint repair compared with reduced-tension single-row repair for massive rotator cuff tears. J Bone Joint Surg Am. 2008;90(suppl 4):35-39 [DOI] [PubMed] [Google Scholar]
- 7. Duquin T, Buyea C, Bisson L. Which method of rotator cuff repairs leads to the highest rates of structural healing? A systematic review. Am J Sports Med. 2010;38:835-841 [DOI] [PubMed] [Google Scholar]
- 8. Ellman H, Hanker G, Bayer M. Repair of the rotator cuff: end-result study of factors influencing reconstruction. J Bone Joint Surg Am. 1986;68(8):1136-1144 [PubMed] [Google Scholar]
- 9. Franceschi F, Ruzzini L, Longo UG, et al. Equivalent clinical results of arthroscopic single-row and double-row suture anchor repair for rotator cuff tears: a randomized controlled trial. Am J Sports Med. 2007;35(8):1254-1260 [DOI] [PubMed] [Google Scholar]
- 10. Grasso A, Milano G, Salvatore M, Falcone G, Deriu L, Fabbriciani C. Single-row versus double-row arthroscopic rotator cuff repair: a prospective randomized clinical study. Arthroscopy. 2009;25(1):4-12 [DOI] [PubMed] [Google Scholar]
- 11. Ji JH, Shafi M, Kim WY, Kim YY. Clinical outcomes of arthroscopic single and double row repair in full thickness rotator cuff tears. Indian J Orthop. 2010;44(3):308-313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Katolik LI, Romeo AA, Cole BJ, Verma NN, Hayden JK, Bach BR. Normalization of the Constant score. J Shoulder Elbow Surg. 2005;14(3):279-285 [DOI] [PubMed] [Google Scholar]
- 13. Kim DH, Elattrache NS, Tibone JE, et al. Biomechanical comparison of a single-row versus double-row suture anchor technique for rotator cuff repair. Am J Sports Med. 2006;34(3):407-414 [DOI] [PubMed] [Google Scholar]
- 14. Ma CB, Comerford L, Wilson J, Puttlitz CM. Biomechanical evaluation of arthroscopic rotator cuff repairs: double-row compared with single-row fixation. J Bone Joint Surg Am. 2006;88(2):403-410 [DOI] [PubMed] [Google Scholar]
- 15. Masuyama M. The use of sample range in estimating the standard deviation or the variance of any population. Sankhya. 1957;18:159-162 [Google Scholar]
- 16. Meier SW, Meier JD. The effect of double-row fixation on initial repair strength in rotator cuff repair: a biomechanical study. Arthroscopy. 2006;22(11):1168-1173 [DOI] [PubMed] [Google Scholar]
- 17. Meier SW, Meier JD. Rotator cuff repair: the effect of double-row fixation on three-dimensional repair site. J Shoulder Elbow Surg. 2006;15(6):691-696 [DOI] [PubMed] [Google Scholar]
- 18. Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587-594 [DOI] [PubMed] [Google Scholar]
- 19. Nho SJ, Slabaugh MA, Seroyer ST, et al. Does the literature support double-row suture anchor fixation for arthroscopic rotator cuff repair? A systematic review comparing double-row and single-row suture anchor configuration. Arthroscopy. 2009;25(11):1319-1328 [DOI] [PubMed] [Google Scholar]
- 20. Park JY, Lhee SH, Choi JH, Park HK, Yu JW, Seo JB. Comparison of the clinical outcomes of single- and double-row repairs in rotator cuff tears. Am J Sports Med. 2008;36(7):1310-1316 [DOI] [PubMed] [Google Scholar]
- 21. Roy JS, MacDermid JC, Woodhouse LJ. Measuring shoulder function: a systematic review of four questionnaires. Arthritis Rheum. 2009;61(5):623-632 [DOI] [PubMed] [Google Scholar]
- 22. Roy JS, Macdermid JC, Woodhouse LJ. A systematic review of the psychometric properties of the Constant-Murley score. J Shoulder Elbow Surg. 2010;19(1):157-164 [DOI] [PubMed] [Google Scholar]
- 23. Skutek M, Fremerey RW, Zeichen J, Bosch U. Outcome analysis following open rotator cuff repair: early effectiveness validated using four different shoulder assessment scales. Arch Orthop Trauma Surg. 2000;120(7-8):432-436 [DOI] [PubMed] [Google Scholar]
- 24. Smith CD, Alexander S, Hill AM, et al. A biomechanical comparison of single and double-row fixation in arthroscopic rotator cuff repair. J Bone Joint Surg Am. 2006;88(11):2425-2431 [DOI] [PubMed] [Google Scholar]
- 25. Sugaya H, Maeda K, Matsuki K, Moriishi J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy. 2005;21(11):1307-1316 [DOI] [PubMed] [Google Scholar]
- 26. Wall LB, Keener JD, Brophy RH. Clinical outcomes of double-row versus single-row rotator cuff repairs. Arthroscopy. 2009;25(11):1312-1318 [DOI] [PubMed] [Google Scholar]


