Abstract
Background:
For persons with unicompartment knee osteoarthritis (OA), off-unloader braces are a mechanical intervention designed to reduce pain, improve physical function, and possibly slow disease progression. Pain relief is thought to be mediated by distracting the involved compartment via external varus or valgus forces applied to the knee. In so doing, tibiofemoral alignment is improved, and load is shifted off the degenerative compartment, where exposure to potentially damaging and provocative mechanical stresses are reduced.
Objectives:
To provide a synopsis of the evidence documented in the scientific literature concerning the efficacy of off-loader knee braces for improving symptomatology associated with painful disabling medial compartment knee OA.
Search Strategy:
Relevant peer-reviewed publications were retrieved from a MEDLINE search using the terms with the reference terms osteoarthritis, knee, and braces (per Medical Subject Headings), plus a manual search of bibliographies from original and review articles and appropriate Internet resources.
Results:
For persons with combined unicompartment knee OA and mild to moderate instability, the strength of recommendation reported by the Osteoarthritis Research Society International in the ability of off-loader knee braces to reduce pain, improve stability, and diminish the risk of falling was 76% (95% confidence interval, 69%-83%). The more evidence the treatment is effective, the higher the percentage.
Conclusions:
Given the encouraging evidence that off-loader braces are effective in mediating pain relief in conjunction with knee OA and malalignment, bracing should be fully used before joint realignment or replacement surgery is considered. With the number of patients with varus deformities and knee pain predicted to increase as the population ages, a reduction of patient morbidity for this widespread chronic condition in combination with this treatment modality could have a positive impact on health care costs and the economic productivity and quality of life of the affected individuals.
Keywords: osteoarthritis, knee, pain, orthotics
Osteoarthritis (OA) is one of the most prevalent rheumatic diseases, afflicting a large and growing portion of the American population. An estimated 27 million American adults live with OA,55 and the number is expected to increase—a number that correlates with increased obesity rates as the population ages.35 OA is a progressive disease that, at present, has no cure; as such, by 2020, the incidence of OA is predicted to reach 40 million and become the fourth-leading cause of disability.38
Of the joints afflicted, the knee is commonly affected—the medial compartment in particular.65 To date, approximately 6% of U.S. adults over the age of 30 and 12% of the population over 65 suffer from the disorder.21,26 Most exhibit frontal plane laxity, broadly defined as the passive displacement or rotation of the tibia with respect to the femur,75 which is a precursor to instability. Pain and instability form the common complaint, limiting functional performance and quality of life.30 New evidence suggests that nearly half the adult population (46%) will develop over their lifetime painful knee OA in at least 1 knee.63 Obesity, which is a major risk factor, increases lifetime risk to 60%, and those with a history of knee injury have a lifetime risk of 57%.63 Not only consequent for the individual, OA is a considerable burden to society because of its chronic course and the high costs associated with treatment interventions,36 which are important public health issues. There is a need for improved understanding of the mechanisms of progression, as well as the methods in treating the disease.
The effectiveness of knee braces as conservative modalities for the prevention and treatment of injury is controversial, despite their wide clinical use. Knee braces currently fall into 4 classifications (Table 1), as outlined in the position statement published by the American Academy of Orthopaedic Surgeons.1 Valgus off-loader braces offer a conservative (nonoperative) method for realigning the knee for persons with moderate to severe medial knee OA. Evidence suggests that external valgus forces applied by the brace improves tibiofemoral alignment; therefore, load is shifted away from the degenerative compartment, where it is thought that exposure to potentially damaging and provocative mechanical stresses will be reduced.35 Off-loader braces are reported to be a safe and an inexpensive treatment that mediates pain relief and ameliorates function for patients with knee OA.23,43,53,65 Yet their efficacy remains in question. The American Academy of Orthopaedic Surgeons reported that off-loader braces, when properly fitted, may provide significant pain relief for a select group of knee OA patients,1 citing generally consistent, well-designed studies. According to the Osteoarthritis Research Society International’s new guidelines for managing hip and knee OA, the strength of recommendations scored 76% (95% confidence interval, 69%-83%) in the ability of off-loader knee braces to reduce pain and improve stability81 (the higher the percentage, the more evidence-based and expert consensus that the braces were effective). In contrast, the 2008 update of the 2005 Cochrane Review concluded that there was limited evidence on the effectiveness of brace treatment for knee OA, mainly because of the lack of well-designed studies.10 Despite the debate, their use is becoming more common. The purpose of this review is to therefore provide a synopsis of the evidence documented in the scientific literature concerning the efficacy of off-loader knee braces for improving symptomatology associated with painful, disabling medial compartment knee OA.
Table 1.
American Academy of Orthopaedic Surgeons brace classification.1
| Type | Function |
|---|---|
| Prophylactic | Prevent or reduce the severity of knee injury |
| Functional | Provide stability for the anterior cruciate ligament or other ligament deficiencyProvide protection for the anterior cruciate ligament or other ligaments after repairs or reconstructions |
| Rehabilitative | Allow protected motion of injured knees or knees that have been treated operatively |
| Unloader/offloader | Provide pain relief in arthritic knees |
The following search parameters were employed using MEDLINE during July 2008, with the reference terms osteoarthritis, knee, and braces (per Medical Subject Headings), plus a manual search of bibliographies of original and review articles and appropriate Internet resources. Criteria for inclusion were as follows: Articles were limited to the English language and to humans, and they had to have been originally published in peer-reviewed scientific journals.
Malalignment and OA Initiation and Progression
The most influential factor affecting the onset of medial knee OA and progression is genu varum (bowleggedness) or malalignment,8,76 confirmed from standing weightbearing anteroposterior radiographs of the entire lower extremity.24 There are several methods of quantifying frontal plane alignment, as described by the orientation of the femoral and tibial mechanical axes.17 The femoral mechanical axis runs distally from the center of the femoral head to a single knee center point (ie, the center of the femoral intercondylar notch or the midpoint between the tibial spines). The tibial mechanical axis originates from this single knee center point to the center of the ankle mortise. The angle between these 2 axes is the hip-knee-ankle angle. Varus knees have angles less than 180° or may be expressed as a negative deviation from neutral (ie, 0° = neutral alignment).39 An alternative is to calculate the weightbearing line ratio by drawing a line from the center of the femoral head to the middle of the tibiotalar joint. A second line is drawn parallel to the tibial articular surface running medial-lateral. The point where both lines bisect, the perpendicular distance from the weightbearing line to the medial edge of the proximal tibia, is divided by the full width of the tibial plateau and expressed as a percentage.24,62 A ratio less than 50% denotes varus alignment.
Varus angular deformity forces the leg into a bowlegged position, predisposing the medial compartment to focal overload, leading to failure of the load-bearing capacity of the affected cartilage and subchondral bone. In the varus knee, the line of action of the ground reaction force vector passes medially and away from the knee’s frontal plane axis of rotation. The perpendicular distance between the ground reaction force vector and the knee’s center of rotation (moment arm) produces an external adduction moment (also called varus moment), which has been identified as the mechanism primarily responsible for much of the compressive load on the medial compartment.47,53,76 The larger adduction (varus) moment shifts the weightbearing line medially within the knee, which increases medial compartment loading and joint compression.23 High loading within the medial compartment may exacerbate joint pain and OA progression, as manifested by continued articular cartilage destruction and joint space narrowing, meniscal disruption, erosion of bone, and frontal plane laxity.4,48,53,65 A 4° to 6° increase in varus alignment can increase medial compartment loading from 70% to 90% during single-limb weightbearing,29 and a 20% increase in the peak adduction moment has been shown to increase the risk of disease progression.52 Varus deformity coupled with increased medial compartment loading has been associated with a fourfold increase in the odds of medial knee OA worsening over 18 months.76 Given that external adduction moments precipitate OA progression, if not development,2,5,37,45,46,61,73 treatment interventions designed to reduce medial compartment loading are of great interest.
Whereas joint compressive forces associated with high knee adduction moments have received considerable attention, passive frontal plane knee laxity and instability may contribute to disease progression and functional decline.29,57,75 Varus-valgus knee laxity is multifactorial, likely exacerbated by chronic capsuloligamentous stretch owing to malalignment; pseudolaxity owing to meniscal and articular cartilage degeneration that decreases the distance between the tibiofemoral surfaces; or combinations of ligamentous, meniscal, muscular, and capsular pathology.74,75,79 For persons with medial knee OA, laxity appears to be localized to the medial compartment.57 Greater laxity raises the likelihood of episodes of knee instability.31 Many report functional instability,31,56,57 defined as the patient’s perception of the knee “shifting, buckling, and giving way” during activities of daily living.49 A consequence of joint laxity and instability is that of increased muscle activity and coactivation of antagonistic muscles to stabilize the knee.7,13,44,57,75 Persons who are functionally unstable compensate by “stiffening” their knee during weightbearing, which involves increased muscular co-contraction combined with reduced knee flexion excursions.14,15,68,69 Over the long term, the stiffer knee may adversely affect the knee joint. Increased co-contraction, although stabilizing the knee, increases joint contact pressures that could exacerbate joint destruction.13,42,56,57
Contemporary management of unicompartment knee OA is to control pain and to improve function and health-related quality of life while avoiding therapeutic toxicity.27 Knee replacements, a procedure once reserved for persons over the age of 65, accounted for 69% of replacements in 1997, yet their numbers have grown exponentially since 1999.78 By 2004, knee replacements increased 53%, but the proportion of elderly grew only 5%. Persons between the ages of 45 and 64, and 65 and 84, saw increases of 83% and 38% respectively, when compared with 1997 rates. Knee replacements in 2006 totaled 418 000, at an estimated cost of $19 billion.12 If this exponential trend continues, the number of knee replacements and financial costs will exceed 1.3 million and $49 billion by 2015, respectively.78 Alternatively, for young and physically active persons with significant impairment, high tibial osteotomy is a realignment procedure that shifts weight away from the diseased knee compartment and delays the need for joint replacement.10,18,80 The most critical factor affecting outcome is inappropriate correction,9 which has been shown to yield poor results (success rate of 26% to 63% at 5 to 10 years).51 Although many patients ultimately require surgery, this may not be suitable for some because of the high cost, the variable success rates, the time loss from normal activity, and possible surgical morbidity.59
Conservative (Nonoperative) Realignment Strategy
In recent years, knee unloader braces with valgus adjustments have been prescribed for persons with unicompartment knee OA because they offer a reasonable alternative to osteotomy or arthroplasty. Osteoarthritic knee braces are generally prescribed according to the criteria outlined in Table 2. In theory, valgus unloader braces provide pain relief by reducing the load on the medial compartment through the application of an opposing external valgus moment about the knee.65 This is achieved through the application of an external corrective force to the knee via the adjustable straps or condylar pads while opposing counterforces (arising from the upper and lower brace supports) act proximal and distal to the knee joint.16 The small improvement in alignment is thought to shorten the moment arm (the perpendicular distance between the ground reaction force and the knee joint center), which should in turn lower the external adduction or varus moment. At the same time, compressive load is shifted away from the medial compartment, thereby improving the distribution of compressive load over the joint surfaces. Both changes help to alleviate mechanical stress on the medial compartment.
Table 2.
Management guidelines for prescribing unloader braces for the treatment of moderate to severe knee osteoarthritis.1
| Unicompartmental disease requiring load reduction on affected compartment |
| Documented failure of prior medical treatment modalities (eg, nonsteroidal anti-inflammatory medications, steroid injections, viscoelastic supplementation) |
| Radiographic evidence of unicompartment knee osteoarthritis with or without varus/valgus deformity |
| Persistent knee pain limiting activities of daily living |
Unloader braces have been shown to delay the requirement for surgery43,59,65 and to be a highly cost-effective treatment intervention, as based on an examination of the ratio between cost and the quality of adjusted life years.71 Sales of OA knee braces in the United States are projected to number 108 000,32 yet greater access in response to clinical need appears appropriate. Among a group of patients with OA who were questioned about their health status, use of medications, various nonsurgical treatment modalities, and use of health care resources, only 11% were informed of bracing—only 12% of whom tried them.58
Self-Report Questionnaires: Pain, Function, and Instability
Several studies that have investigated the efficacy of valgus unloader braces have found improvements in pain§ and physical function,13,19,23,41,59,60 but others have reported that function remained unchanged.40,43,53 Pain improvement during walking and stair negotiation have been recorded at 1 week,41 6 weeks,33 8 weeks,6 9 weeks,40 12 weeks,41 and 12 months.28,40 Significant improvement in pain and function assessed with validated knee instruments have been reported at 3 months,50 6 months,53 and 12 months,60 and significant reduction of pain during activities of daily living has been reported at 4 weeks,59 6 weeks,43 9 weeks,40 and 12 months.41
Matsuno et al60 found, among 20 medial knee OA patients who underwent gait analysis after having been prescribed their custom off-loader brace, that 19 reported substantial pain relief and that knee pain scores had improved from 18.0 to 21.5 during walking. These findings were later confirmed by Hewett et al,41 who found that 78% of their OA patients experienced significant pain that limited their physical activity. After 9 weeks of bracing (first assessment), self-reported knee pain was significantly reduced, with only 39% and 31% complaining of pain during their first and second assessments, respectively. Persons tolerated, on average, about 51 minutes of walking before onset of pain, whereas after the first evaluation, participants’ walking improved by about 138 minutes without pain. Pollo et al65 found that after only 2 weeks of brace use, patients reported that their pain and activity level improved. Draper et al23 conducted a 3-month study that found all patients reported immediate symptomatic improvement, with less pain during gait analysis. In a randomized cross-over study, Richards et al67 fitted 12 patients with an off-the-shelf brace with bilateral uniaxial hinges and with a valgus corrective brace for periods of 6 months. Knee kinematics and ground reaction forces were compared during walking and stair climbing, combined with measures of pain using self-reported activity questionnaires. Pain, function, loading, and propulsive forces were all statistically improved with the valgus brace only, leading the authors to speculate that confidence had improved during loading.
Barnes et al6 reported that the application of a brace yielded significant pain and oral medication reduction, with statistical improvements in performing activities of daily living and quality of life. Lindenfeld and colleagues59 saw pain scores decrease 48%, whereas activities of daily living performed without pain symptoms increased 69%. Functional scores during activities of daily living increased 79%, along with a trend toward increased sports activity (28%, although not statistically significant). No change in pain during walking was observed after brace wear. Horlick and Loomer43 conducted a double crossover design where patients underwent testing with no brace and with braces in neutral and valgus; as such, they reported statistically significant pain relief with the valgus brace. Gaasbeek et al33 reported similar significant improvements in pain and function. Finger and Paulos28 found that after 3 months of brace wear, average resting pain was reduced from 4.2 to 2.1, night pain decreased from 3.9 to 2.6, and pain during activities of daily living decreased from 7.2 to 3.9. No further changes in pain were evident at 6 months. In the crossover study by Draganich et al,22 custom braces provided significantly greater improvements in stiffness and function than those offered by off-the-shelf braces during gait and stair stepping, with statistical improvements in pain also noted. Conversely, Brouwer et al11 found no significant differences in quality of life between patients with and without the use of bracing, although increasingly lower medication use was found in the brace group.
In a prospective, randomized clinical trial of 119 OA patients, Kirkley et al53 compared 3 treatments: standard medical treatment (n = 33), combined medical treatment with neoprene sleeve (n = 36), and combined medical treatment with custom valgus unloader brace (n = 41). At the 6-month follow-up, those with the valgus braces had, on average, significantly improved scores on the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and the McMaster Toronto arthritis patient preference questionnaires (MACTAR) for pain, stiffness, and physical function, as compared with those patients who had neoprene sleeves or medical treatment alone. As a result of bracing, patients gained significant pain relief and improved activity levels and quality of life, with concomitant reductions of pharmacological aids.
Evidence suggests that mediolateral laxity and instability also contribute to disease progression and functional decline.29,57,75 In surveying 105 participants with knee OA, Fitzgerald et al31 found that 63% of respondents reported episodes of knee instability when performing activities of daily living, with 44% claiming that instability reduced their ability to function. New evidence from the study by Ramsey et al66 suggests that the effectiveness of off-loading braces is predicated on the degree to which unloader knee braces control knee instability and influence muscle co-contractions during gait. Sixteen OA volunteers underwent gait analysis on 3 occasions, with their involved knee unsupported, followed by a neutral brace setting (normal knee alignment) and an unloading condition (4° of valgus). Volunteers served as their own controls, with analysis focusing on the differences between brace conditions. Instability was assessed using the question “To what degree does giving way, buckling or shifting of the knee affect your level of daily activity?” as taken from the Knee Outcome Survey–Activities of Daily Living Scale.31,49 When the knee was unsupported, 60% of participants reported episodes of instability, with 30% stating that it negatively affected their activities of daily living. Instability was found to be significantly correlated to self-report ratings of pain, symptoms, activities of daily living, and quality of life. Those who complained of instability had increased pain and symptoms, with lower activities of daily living, knee function, and quality of life. After patients wore the braces in both the neutral and unloaded setting (interspersed with a 2-week washout period, where nothing was worn), the neutral brace resulted in the highest overall improvement in stability, pain, and knee function. Although pain and functional disability were significantly reduced (compared with baseline measures), no significant differences were apparent between bracing conditions, leading the authors to speculate that neutral alignment afforded the same benefit as 4° of valgus correction. The lack of statistical differences between brace conditions may be such that anthropometric measures were taken with the knee unloaded and the brace was manufactured accordingly. Casting the knee in load bearing may result in differences being observed.
Whereas evidence indicates that off-loader braces appear to be clinically successful when used as a conservative treatment for osteoarthritic knees, compliance is a known issue and their long-term efficacy remains questionable, although the results from recent studies are promising. Giori34 found that the majority of patients, when issued unloader braces, wore them for more than 3 years. Brace use was found to have a survival rate of 76% at 1 year, 69% at 2 years, and 61% at 3 years, with younger patients having a higher probability of longer brace use than that of older patients. These findings are similar to those of Barnes et al,6 who reported that 41% continued with brace use after 2 years whereas 35% discontinued for a variety of reasons and 24% ultimately went on to have surgery. Finger and Paulos28 reported that after 6 months, 22% of patients used the brace continually, 65% during strenuous activity only, and 15% ceased brace use, citing discomfort. Similarly, Horlick and Loomer43 observed that after about 20 months, 93% of patients using valgus braces with medial hinges continued to use them as their principal form of therapy. Later, Horlick et al (unpublished data, June 2006) found that after 2 years, 12% of patients wore their brace regularly, 64% utilized the brace during certain activities, and 70% wore the brace during sports or recreation. Notably, 55% responded that the brace enabled them to pursue activities otherwise not possible. However, Hewett et al40 found that 50% of patients no longer wore their brace after 1 year. Table 3 summarizes the data for comparisons across investigations.
Table 3.
Summary of pain, function, and instability.a
| Author | Brace Type | Questionnaire(s) | Results |
|---|---|---|---|
| Barnes et al6 n, 30 | CounterForce brace (Breg) | AAOS Arthritis QuestionnaireSF-36 | From initial to final evaluation, function, pain, stiffness, and swelling significantly improved. |
| Brouwer et al11 n, 117 | OAsys brace | HSS scoreEQ-5D | Pain severity was less in the brace group; no significant difference in quality of life was reported; increasingly lower medication use. |
| Draganich et al22 n, 10 | Off-the-shelf adjustable (OAdjuster)Custom adjustable (OA Defiance) | WOMAC | Both braces significantly reduced pain and stiffness. For the custom brace, improved function was found during gait and stair stepping, compared with baseline and off-the-shelf bracing. |
| Draper et al23 n, 30 | GII ADJ Unloader | HSS score | All patients reported immediate symptomatic improvement with less pain on walking. |
| Finger et al28 n, 28 | OAdjuster unloading brace | VAS | Average resting pain decreased from 4.2 to 2.1 at 3 months; night pain decreased from 3.9 to 2.6; pain with activity decreased from 7.2 to 3.9. |
| Gaasbeek et al33 n, 15 | SofTec OA valgus brace | WOMACVAS | Significant improvement of pain and function were reported after 6 weeks of brace use. |
| Giori et al34 n, 49 | DJ Defiance braceDJ Monarch braceMOS Genu brace | Knee Society pain and function scores | Brace use has a survival of 76% at 1 year, 69% at 2 years, and 61% at 3 years. Of the patients still using a brace, Knee Society pain scores increased an average of 26 points, from 13 to 3; Knee Society function scores progressed from 61 to 72 points. |
| Hewett et al40 n, 18 | Bledsoe | Cincinnati Knee Rating System VAS | Self-reported knee pain was significantly reduced, with only 39% and 31% complaining of pain during their first and second assessments. Patients tolerated about 51 minutes of walking before onset of pain, whereas after the first evaluation, walking improved by about 138 minutes without pain. |
| Horlick and Loomer43 n, 39 | GII Unloader | Daily diary | 82% success rate for pain relief with brace use. |
| Kirkley et al53 n, 119 | GII UnloaderNeoprene sleeve | WOMACMACTAR | Patients gained significant pain relief and improved activity levels and quality of life as result of bracing. |
| Lindenfeld et al59 n, 11 | Custom unloader, Big Sky Medical | Cincinnati Knee Rating SystemVAS | With brace wear, pain symptoms decreased significantly, function scores and sports activity increased, and overall activity level increased 69%. |
| Matsuno et al60 n, 20 | GII Unloader | JOA | 19 of the 20 patients reported significant pain relief. Knee pain scores for gait increased from 18.0 to 21.5 and progressed during stair stepping from 12.8 to 15.8. |
| Pollo et al65 n, 11 | GII ADJ Unloader | VAS | Pain and activity level improved in all patients with valgus bracing. |
| Ramsey et al66 n, 16 | GII Select Unloader | KOOSKOS | The scores for pain, symptoms, and activities of daily living significantly increased for both brace settings, compared with baseline. An improvement from baseline as a result of both brace settings was seen for sports and recreation and for quality of life. |
| Richards et al67 n, 12 | Off-the-shelf bilateral uniaxial hingeGII ADJ Unloader | VASHSS | With GII brace, HSS scores improved to 65.7. |
AAOS, American Academy of Orthopaedic Surgeons; SF-36, 36-item short-form health survey; EQ-5D, health outcome measure by EuroQol Group; HSS, Hospital for Special Surgery; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index; VAS, visual analogue scale; MACTAR, McMaster Toronto arthritis patient preference questionnaires; JOA, Japanese Orthopaedic Association; KOOS, Knee injury and Osteoarthritis Outcome Score; KOS, Knee Outcome Survey.
Kinematics and Kinetics
Only recently has it been possible to measure load distributions experimentally in vivo. Anderson et al3 inserted pressure transducers onto the medial compartment of osteoarthritic knees to test the assertion that valgus unloader knee braces unload the medial compartment. Contact forces were measured when patients walked with and without an unloader brace during unassisted double-leg stance and single-leg stance. No significant effects of bracing were observed because of the large variations in force as the transducer shifted position, which consequently influenced load measures. The area over which the sensor was placed was approximately one third of the total contact area of the medial compartment. Therefore, small changes in knee flexion angle between measurements introduced large changes in contact conditions on the sensor.
Because of the inherent problems in quantifying load distributions in vivo, imaging techniques and computer modeling have been used as an alternative to conventional gait analysis and inverse dynamics. Using a static 2-dimensional mathematical leg model, Shelburne et al77 analyzed both the forces and the moments acting on the knee to examine interactions among ground reaction force, knee abduction moment, and medial compartment loading. The external adduction moment was calculated by multiplying the magnitude of the resultant ground reaction force by the perpendicular distance between the line of action of this force and the center of the knee joint in the coronal plane. The simulation depicted that load distribution was derived mainly from knee adduction moments. However, the model neglected muscular and ligamentous actions; ground force was assumed to pass through the center of the ankle joint; and analysis was confined to the frontal plane. Decreased knee adduction moments and medial compartment loading were found to be directly proportional to increased valgus moments applied by the brace. Dynamic simulations were also derived whereby joint angles, ground reaction forces, and muscle forces obtained from simulated gait trials were applied to a comprehensive 3-dimensional musculoskeletal model. Valgus loading was simulated by applying incremental 1 N·m abduction moments up to 12 N·m, reflecting magnitudes reported in the literature.65,72 Dynamic simulation revealed that valgus moments reduced medial compartment loading throughout stance. For every 1 N·m valgus moment increment, the model predicted a 3% reduction in peak knee adduction moment and a 1% reduction of the maximum force (19 N, or 0.03 body weight) acting in the medial compartment. Even at 12 N·m, the model predicted reductions will be no more than 228 N, or 0.3 body weight. Whether these small reductions mediated pain relief cannot be determined from modeling.
Two-dimensional fluoroscopy has been used to analyze frontal plane knee motion during treadmill gait.20,54,64 Komistek et al54 reported that off-loading knee braces mediate condylar separation, as evidenced by average changes in condylar separation (1.2 mm) and angle (2.2°) at heel strike. However, among obese patients, a lack of subjective pain relief was noted and found to correlate with the absence of condylar separation. Nadaud et al64 measured changes in condylar separation, comparing 5 brace designs. Based on 3-dimensional knee models derived from computed tomographic scans that were overlaid onto fluoroscopic images, comparative analysis revealed that 4 of 5 patients achieved some degree of unloading, whereas 1 experienced no benefit from any of the braces. Average condylar separation varied across braces and volunteers. The largest separation was measured at greater than 2.0 mm, occurring at heel strike. Four of 5 braces achieved a 1.0 mm maximum separation at midstance and 2, a maximum separation of > 1.0 mm at toe-off. The authors suggested that unloader braces are most effective at heel strike, yet the results should be interpreted with caution because of the small sample size. Dennis et al,20 who recruited a larger sample size and restricted analysis to a single brace, reported that 78% of participants demonstrated significant (P = .015) medial condylar separation and condylar separation angle with corresponding pain relief after brace application. Magnitudes of separation and angles averaged 1.7 mm and 2°, respectively, at heel strike and midstance, suggesting that braces may realign the knee and lessen the adduction moment during weight acceptance.
Static radiographic evaluations (during involved unilateral stance) have shown a 1.4° lateral shift of the femoral-tibial angle with bracing.60 From weightbearing radiographs, Draganich et al22 depicted that custom braces were more effective in reducing varus angulation, an average of 1.5°, compared with no brace (baseline) and 1.3° with an off-the-shelf brace. No reductions were observed with the off-the-shelf brace. Conversely, Horlick and Loomer43 observed no significant changes in femoral-tibial angle or joint space in standing posterior-anterior radiographs during weightbearing and nonweightbearing, with and without valgus brace.
Others have tried instrumenting unloader braces to measure the valgus moment exerted by the brace. Pollo et al65 determined the valgus moment exerted by brace using strain gauges and buckle transducers affixed onto custom braces. Four brace settings were tested. Net knee moments were calculated by subtracting the brace valgus moment from the external knee varus moment as a result of the ground reaction force vector. In 3 of the 4 settings, net knee moments were significantly reduced when compared with the unbraced knee. No reductions were observed with only the standard clinical brace setting (4° of valgus relative to the patient’s alignment). In the calibrated 4° and 8° valgus settings (relative to the instrumented zero baseline), decreases were as much as 20% at 8°, which were significant. On average, net varus moments were reduced 11% (7.1 N·m). Increasing strap tension reduced neither net knee moment nor medial compartment load. Self et al72 measured valgus brace moments using an instrumented bladder, and valgus brace moments were estimated using a simple 2- dimensional model. External knee varus moments were compared between braced and nonbraced conditions and found to be significantly reduced at 20% and 25% of stance. Since the force exerted by the brace remained fairly constant throughout stance, the small countermoment was insufficient in mediating the differences in varus moments between brace conditions. The authors speculated that the brace likely altered knee kinematics and temporal-spatial parameters, which could have altered knee moments, although this was not substantiated. Although Self and colleagues72 state that the reduced varus moment may contribute to pain reduction, the lack of clinical outcome measures for pain and functional status makes their claim conjecture.
Using conventional kinematic gait analysis, Ramsey et al66 found that knee adduction excursions were significantly reduced with the use of bracing, with excursions reported to be lowest at 4° of valgus correction. The magnitude of knee flexion excursion and medial joint space narrowing were strongly correlated; those with substantial narrowing exhibited greater knee stiffening, demonstrated by lower knee flexion excursions during weight acceptance. Indirect measures of the knee adduction moment using inverse dynamics have demonstrated that valgus-producing braces reduce the external adduction moments about the knee during gait. Gaasbeek et al33 found that before brace treatment, peak knee varus moments were statistically higher in patients’ affected limbs, compared with their unaffected limbs. Bracing tended to lower peak varus moments, although differences were not statistically significant. This lack of significance may likely be explained by the small sample size and high variability. However, for those with greater varus knee deformity, the effect of bracing was more profound, with greater reductions in the peak varus moments achieved during walking. Draganich et al22 observed that reductions in the peak adduction (varus) moments were 3 to 4 times greater for the custom brace than for the off-the-shelf brace. Lindenfeld and colleagues59 found an average of 10% reduction in the mean adduction moment at the knee. With the brace, 9 of the 11 patients had a decrease in the adduction moment, and 5 of 11 patients had a decrease greater than 10%. The authors suggested that the advantages of valgus bracing occurred as a result of an altered gait pattern, which involved a decrease of the external varus moment. In contrast, Hewett et al41 saw no change in the adduction moment with the application of bracing, yet significant pain relief was reported, along with extended walking time after 9 weeks of wearing the brace. Similarly, Pollo et al65 found that external varus moments were only marginally reduced.
Because direct measurement of medial compartment load is impracticable, load reduction has been indirectly estimated using instrumented braces with combined gait analysis. Using a generic knee model, Pollo and colleagues65 estimated the change in medial compartment load as a result of valgus bracing. Load reductions were reportedly as much as 17% on the medial side during the stance phase of gait. Normal 4° valgus alignment via the adjustable hinge had a greater effect on reducing medial compartment load than did increasing strap tension. Adjusting valgus angulation from 4° to 8° had a significant effect on reducing the medial compartment load as well.
Loads, however, were derived assuming constant ligament forces, joint contact points, intercondylar distance, muscle moment arms, and directions of muscle pull between brace conditions and patients. Moreover, quadriceps force and hamstring force were considered to contribute entirely to the joint compression force, but no adjustments were made for flexion angle. Individuals with knee OA, however, utilize different movement and muscle activation patterns, compared with the healthy population.13 Patients with knee OA walk with less knee flexion excursion during weight acceptance and reduced peak vertical ground reaction forces relative to body weight.13 They also demonstrate significantly increased muscle coactivation and duration of muscle activity during gait. The combination of limitations invalidates the assertion of uniformity in Pollo’s generic knee model. Table 4 is a summary of the data for comparisons across investigations.
Table 4.
Summary of kinematic and kinetic data.
| Author | Brace Type | Results |
|---|---|---|
| Davidson et al19 n, 12 | GII Unloader | The brace had no effect on thigh coronal angle but reduced shank coronal angle at toe-off. The brace prevented full extension during midstance. |
| Dennis et al20 n, 45 single brace n, 5 multiple brace | Single-Brace Bledsoe ThrusterMultiple-Brace Bledsoe ThrusterDJ OrthoIsportsBreg TraditionGII UnloaderACL brace | Single-brace study: 31 of 40 patients (78%) demonstrated an increase in medial compartment separation at heel strike. During the midstance phase of gait, 70% of patients exhibited an increase in medial condylar separation. 85% judged brace to be effective in reducing pain relief.Multiple-brace study: Bledsoe and DJ Ortho braces achieved greatest amount of condylar separation at heel strike. At midstance, the Bledsoe brace was the only one to produce a significant condylar separation value. |
| Draganich et al22 n, 10 | Off-the-shelf adjustable (OAdjuster)Custom (OA Defiance) | The custom-brace significantly decreased varus angulation of the knee by 1.5°, compared with baseline, and by 1.3°, compared with the off-the-shelf brace, and reduced peak adduction moments were reported during gait and stair stepping, compared with baseline and off-the-shelf bracing. |
| Gaasbeek et al33 n, 15 | SofTec OA valgus brace | Gait analysis showed that the brace had a tendency of lowering peak varus moment about the knee. This effect was more profound in the presence of higher initial varus deformity angle of the knee. Bracing led to a small decrease in knee extension at the end of the swing phase and increase of walking velocity. |
| Hewett et al40 n, 18 | Bledsoe | Results while wearing a brace showed no significant change in the adduction moment. |
| Horlick and Loomer43 n, 39 | GII Unloader | Found no substantial changes in the femoral-tibial angle or joint space. |
| Komistek et al54 n, 15 | Bledsoe Thruster | 12 of 15 patients reported relief of pain and demonstrated condylar separation of the medial compartment with the use of bracing. |
| Lindenfeld et al59 n, 11 | Custom unloaderBig Sky Medical | 9 of 11 patients had a decrease in the adduction moment when wearing the brace, with the moment decreasing by as much as 32%. No apparent gait adaptations were observed. |
| Matsuno et al60 n, 20 | GII Unloader Brace | The femorotibial angle decreased in 12 of the 20 patients. The average angle decreased from 185.1° to 183.7° with the application of the brace. |
| Nadaud et al64 n, 5 | Bledsoe Thruster 2Breg Tradition X2KDJ AdjusterGII Unloader SpiritOAsysACL | On average, the largest magnitude of medial condylar separation occurred at heel strike. 4 of 5 braces achieved a maximum separation value ≥ 1 mm at midstance. The Bledsoe braces and DJ braces attained the largest amount of separation at heel strike. |
| Pollo et al65 n, 11 | GII Unloader ADJ | Reduced net varus moment by an average of 13% and medial compartment load at the knee by an average of 11%. Increasing valgus alignment had greater effect than increasing strap tension. |
| Ramsey et al66 n, 16 | GII Select Unloader | Knee adduction excursions were significantly reduced with the use of bracing, with excursions reported to be lowest at 4° of valgus correction. |
| Richards et al67 n, 12 | Off-the-shelf bilateral uniaxial hingeGII ADJ Unloader | Significant improvements in loading and propulsive forces were seen with the valgus brace. Treatment with a simple brace showed only significant improvements in loading forces. |
| Self et al72 n, 5 | DJ Monarch brace | Varus moment was significantly higher during unbraced condition than braced condition. |
Muscle Activity
Little research has examined the effects of bracing on muscle activity, although new evidence suggests that off-loading braces may influence antagonist muscle co-contractions.66 Previous studies have reported greater vastus medialis-medial hamstring co-contraction in varus aligned knees. The greater co-contraction, coupled with the larger medial load (adduction moment), may be a response to stabilize the medial compartment by increasing compression.57 Increased joint contact pressures could, however, exacerbate joint destruction and pain.13,42,56,57 In the study by Ramsey et al,66 vastus lateralus-lateral hamstring co-contractions were greater in magnitude than those of vastus medialis-medial hamstring, confirming earlier studies that this may represent an attempt to redistribute the load laterally.4,70 During neutral and valgus brace settings, a significant lowering of antagonist vastus medialis-medial hamstring and vastus lateralis-lateral hamstrings pairings was reported.66 Persons with greater knee varus alignment demonstrated greater declines in vastus medialis-medial hamstring and vastus lateralis-lateral hamstring co-contraction. The data led the authors to speculate that pain relief from off-loader bracing may be the result of reduced muscle co-contractions, as mediated by the brace, mechanically stabilizing the knee. Table 5 summarizes the data for comparisons across investigations.
Table 5.
Summary of neuromuscular activity.
| Author | Brace Type | Results |
|---|---|---|
| Ramsey et al66 n, 16 | GII Select Unloader | During neutral and valgus brace settings, a significant lowering of antagonist vastus medialis-medial hamstring and vastus lateralis-lateral hamstrings pairings was reported. Persons with greater knee varus alignment demonstrated greater declines in vastus medialis-medial hamstring and vastus lateralis-lateral hamstring co-contraction. |
Summary
Valgus off-loader braces are designed to redistribute provocative mechanical forces off the degenerative compartment of the knee. Given the encouraging evidence indicating that they are effective in mediating pain relief in conjunction with knee OA and malalignment, off-loader braces should be fully utilized before joint realignment or replacement surgery is considered. More work, however, is needed to substantiate their long-term benefits, given that patient compliance is an issue. They are reportedly difficult to wear for extended periods because of the degree of force they impart to the limb to alter alignment. Also, bracing in combination with other conservative modalities may provide additional benefit. Whereas intra-articular injections may temporarily elicit pain relief, knee mechanics remain unaffected. Greater peak knee adduction moments and increased muscle activation during gait have been reported among persons who respond to viscosupplementation, which may increase load and thus exacerbates OA progression and joint deterioration (K. Briem, unpublished data, 2008). With the number of patients with varus deformities and knee pain predicted to increase as the population ages, a reduction of patient morbidity for this widespread chronic condition in combination with this treatment modality could have a positive impact on health care costs and the economic productivity and quality of life of the affected individuals.
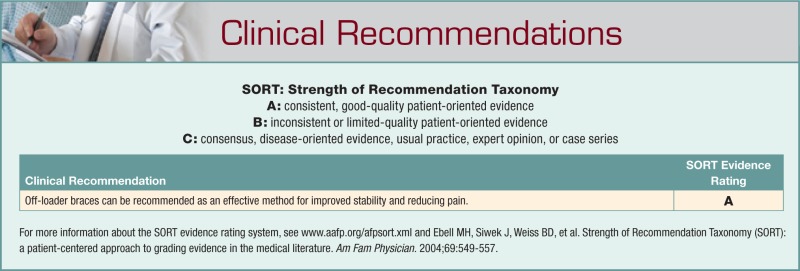
Level of Evidence
The preponderance of evidence suggests that off-loader knee braces are effective in reducing knee pain, improving stability, and diminishing the risk of falling for persons with knee OA and mild to moderate varus or valgus instability. The strength of recommendation was 76% for off-loader braces’ ability to support unstable osteoatrthitic knees, as outlined in the new Osteoarthritis Research Society International’s guidelines81 for managing hip and knee OA. Expressed as a percentage, the strength of recommendation reflects the level of scientific evidence for their efficacy, safety, and cost-effectiveness. The more evidence-based research indicating that the treatment is effective, the higher the strength of recommendation. The level of evidence was based on a meta-analysis of randomized controlled trials10 and randomized clinical trials,53 although it is evident from our review that studies vary in methodological quality.
Footnotes
References
- 1. American Academy of Orthopaedic Surgeons The Use of Knee Braces [position statement]. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2003 [Google Scholar]
- 2. Amin S, Luepongsak N, McGibbon CA, LaValley MP, Krebs DE, Felson DT. Knee adduction moment and development of chronic knee pain in elders. Arthritis Rheum. 2004;51(3):371-376 [DOI] [PubMed] [Google Scholar]
- 3. Anderson IA, MacDiarmid AA, Harris ML, Gillies RM, Phelps R, Walsh WR. A novel method for measuring medial compartment pressures within the knee joint in-vivo. J Biomech. 2003;36(9):1391-1395 [DOI] [PubMed] [Google Scholar]
- 4. Andriacchi TP. Dynamics of knee malalignment [review]. Orthop Clin North Am. 1994;25(3):395-403 [PubMed] [Google Scholar]
- 5. Baliunas AJ, Hurwitz DE, Ryals AB, et al. Increased knee joint loads during walking are present in subjects with knee osteoarthritis. Osteoarthritis Cartilage. 2002;10(7):573-579 [DOI] [PubMed] [Google Scholar]
- 6. Barnes CL, Cawley PW, Hederman B. Effect of CounterForce brace on symptomatic relief in a group of patients with symptomatic unicompartmental osteoarthritis: a prospective 2-year investigation. Am J Sports Med. 2002;31(7):396-401 [PubMed] [Google Scholar]
- 7. Benedetti MG, Bonato P, Catani F, et al. Myoelectric activation pattern during gait in total knee replacement: relationship with kinematics, kinetics, and clinical outcome. IEEE Trans Rehabil Eng. 1999;7(2):140-149 [DOI] [PubMed] [Google Scholar]
- 8. Birmingham TB, Kramer JF, Kirkley A, Inglis JT, Spaulding SJ, Vandervoort AA. Association among neuromuscular and anatomic measures for patients with knee osteoarthritis. Arch Phys Med Rehabil. 2001;82(8):1115-1118 [DOI] [PubMed] [Google Scholar]
- 9. Briem K, Ramsey DK, Newcomb W, Rudolph KS, Snyder-Mackler L. Effects of the amount of valgus correction for medial compartment knee osteoarthritis on clinical outcome, knee kinetics and muscle co-contraction after opening wedge high tibial osteotomy. J Orthop Res. 2007;25(3):311-318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brouwer RW, Jakma TS, Bierma-Zeinstra SM, Verhagen AP, Verhaar J. Osteotomy for treating knee osteoarthritis. Cochrane Database Syst Rev. 2005;1:CD004019. [DOI] [PubMed] [Google Scholar]
- 11. Brouwer RW, van Raaij TM, Verhaar JA, Coene LN, Bierma-Zeinstra SM. Brace treatment for osteoarthritis of the knee: a prospective randomized multi-centre trial. Osteoarthritis Cartilage. 2006;14(8):777-783 [DOI] [PubMed] [Google Scholar]
- 12. Centers for Disease Control and Prevention Lifetime Risk of Symptomatic Knee Osteoarthritis. http://www.cdc.gov/arthritis/misc/osteoarthritis.htm. Accessed July 15, 2009
- 13. Childs JD, Sparto PJ, Fitzgerald GK, Bizzini M, Irrgang JJ. Alterations in lower extremity movement and muscle activation patterns in individuals with knee osteoarthritis. Clin Biomech (Bristol, Avon). 2004;19(1):44-49 [DOI] [PubMed] [Google Scholar]
- 14. Chmielewski TL, Hurd WJ, Snyder-Mackler L. Elucidation of a potentially destabilizing control strategy in ACL deficient non-copers. J Electromyogr Kinesiol. 2005;15(1):83-92 [DOI] [PubMed] [Google Scholar]
- 15. Chmielewski TL, Rudolph KS, Fitzgerald GK, Axe MJ, Snyder-Mackler L. Biomechanical evidence supporting a differential response to acute ACL injury. Clin Biomech (Bristol, Avon). 2001;16(7):586-591 [DOI] [PubMed] [Google Scholar]
- 16. Cole BJ, Harner CD. Degenerative arthritis of the knee in active patients: evaluation and management. J Am Acad Orthop Surg. 1999;7(6):389-402 [DOI] [PubMed] [Google Scholar]
- 17. Cooke TD, Sled EA, Scudamore RA. Frontal plane knee alignment: a call for standardized measurement. J Rheumatol. 2007;34(9):1796-1801 [PubMed] [Google Scholar]
- 18. Dahl A, Toksvig-Larsen S, Roos EM. A 2-year prospective study of patient-relevant outcomes in patients operated on for knee osteoarthritis with tibial osteotomy. BMC Musculoskelet Disord. 2005;6(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Davidson PL, Sanderson DJ, Loomer RL. Kinematics of valgus bracing for medial gonarthrosis: technical report. Clin Biomech (Bristol, Avon). 1998;13(6):414-419 [DOI] [PubMed] [Google Scholar]
- 20. Dennis DA, Komistek RD, Nadaud MC, Mahfouz M. Evaluation of off-loading braces for treatment of unicompartmental knee arthrosis. J Arthroplasty. 2006;21(4)(suppl 1):2-8 [DOI] [PubMed] [Google Scholar]
- 21. Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey. 1991-94. J Rheumatol. 2006;33(11):2271-2279 [PubMed] [Google Scholar]
- 22. Draganich L, Reider B, Rimington T, Piotrowski G, Mallik K, Nasson S. The effectiveness of self-adjustable custom and off-the-shelf bracing in the treatment of varus gonarthrosis. J Bone Joint Surg Am. 2006;88(12):2645-2652 [DOI] [PubMed] [Google Scholar]
- 23. Draper ER, Cable JM, Sanchez-Ballester J, Hunt N, Robinson JR, Strachan RK. Improvement in function after valgus bracing of the knee: an analysis of gait symmetry. J Bone Joint Surg Br. 2000;82(7):1001-1005 [DOI] [PubMed] [Google Scholar]
- 24. Dugdale TW, Noyes FR, Styer D. Preoperative planning for high tibial osteotomy: the effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop Rel Res. 1992;(274):248-264 [PubMed] [Google Scholar]
- 25. Ebell MH, Siwek J, Weiss BD, et al. Strength of Recommendation Taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. J Am Board Fam Pract. 2004;17(1):59-67 [DOI] [PubMed] [Google Scholar]
- 26. Felson DT, Lawrence RC, Dieppe PA, et al. Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med. 2000;133(8):635-646 [DOI] [PubMed] [Google Scholar]
- 27. Felson DT, Lawrence RC, Hochberg MC, et al. Osteoarthritis: new insights. Part 2: treatment approaches. Ann Intern Med. 2000;133(9):726-737 [DOI] [PubMed] [Google Scholar]
- 28. Finger S, Paulos LE. Clinical and biomechanical evaluation of the unloading brace. J Knee Surg. 2002;15(3):155-158 [PubMed] [Google Scholar]
- 29. Fitzgerald GK. Therapeutic exercise for knee osteoarthritis: considering factors that may influence outcome. Eura Medicophys. 2005;41(2):163-171 [PubMed] [Google Scholar]
- 30. Fitzgerald GK, Childs JD, Ridge TM, Irrgang JJ. Agility and perturbation training for a physically active individual with knee osteoarthritis. Phys Ther. 2002;82(4):372-382 [PubMed] [Google Scholar]
- 31. Fitzgerald GK, Piva SR, Irrgang JJ. Reports of joint instability in knee osteoarthritis: its prevalence and relationship to physical function. Arthritis Rheum. 2004;51(6):941-946 [DOI] [PubMed] [Google Scholar]
- 32. Frost, Sullivan Knee Braces and Support Market: Osteoarthritis Brace Market, 2006. San Antonio, TX: Frost & Sullivan [Google Scholar]
- 33. Gaasbeek RD, Groen BE, Hampsink B, van Heerwaarden RJ, Duysens J. Valgus bracing in patients with medial compartment osteoarthritis of the knee: a gait analysis study of a new brace. Gait Posture. 2007;26(1):3-10 [DOI] [PubMed] [Google Scholar]
- 34. Giori NJ. Load-shifting brace treatment for osteoarthritis of the knee: a minimum 2 1/2-year follow-up study. J Rehabil Res Dev. 2004;41(2):187-194 [DOI] [PubMed] [Google Scholar]
- 35. Gross KD, Hillstrom HJ. Noninvasive devices targeting the mechanics of osteoarthritis. Rheum Dis Clin North Am. 2008;34(3):755-776 [DOI] [PubMed] [Google Scholar]
- 36. Healy WL, Iorio R, Ko J, Appleby D, Lemos DW. Impact of cost reduction programs on short-term patient outcome and hospital cost of total knee arthroplasty. J Bone Joint Surg Am. 2002;84(3):348-353 [DOI] [PubMed] [Google Scholar]
- 37. Heller MO, Taylor WR, Perka C, Duda GN. The influence of alignment on the musculo-skeletal loading conditions at the knee. Langenbecks Arch Surg. 2003;388(5):291-297 [DOI] [PubMed] [Google Scholar]
- 38. Helmick CG, Felson DT, Lawrence RC, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States, part I. Arthritis Rheum. 2008;58(1):15-25 [DOI] [PubMed] [Google Scholar]
- 39. Hernigou P, Medevielle D, Debeyre J, Goutallier D. Proximal tibial osteotomy for osteoarthritis with varus deformity: a ten to thirteen-year follow-up study. J Bone Joint Surg Am. 1987;69(3):332-354 [PubMed] [Google Scholar]
- 40. Hewett TE, Noyes FR, Barber-Westin SD, Heckmann TP. Decrease in knee joint pain and increase in function in patients with medial compartment arthrosis: a prospective analysis of valgus bracing. Orthopedics. 1998;21:131-138 [DOI] [PubMed] [Google Scholar]
- 41. Hillstrom HJ, Brower DJ, Bhimji S, et al. Assessment of conservative realignment therapies for the treatment of varus knee osteoarthritis: biomechanics and joint pathology. Gait Posture. 2000;11(2):170-171 [Google Scholar]
- 42. Hodge WA, Fijan RS, Carlson KL, Burgess RG, Harris WH, Mann RW. Contact pressures in the human hip-joint measured in vivo. Proceedings of the National Academy of Sciences of the United States of America. 1986;83(9):2879-2883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Horlick SG, Loomer RL. Valgus knee bracing for medial gonarthrosis. Clin J Sport Med. 1993;3:251-255 [Google Scholar]
- 44. Hortobagyi T, Westerkamp L, Beam S, et al. Altered hamstring-quadriceps muscle balance in patients with knee osteoarthritis. Clin Biomech (Bristol, Avon). 2005;20(1):97-104 [DOI] [PubMed] [Google Scholar]
- 45. Hunt MA, Birmingham TB, Giffin JR, Jenkyn TR. Associations among knee adduction moment, frontal plane ground reaction force, and lever arm during walking in patients with knee osteoarthritis. J Biomech. 2006;39(12):2213-2220 [DOI] [PubMed] [Google Scholar]
- 46. Hurwitz DE, Ryals AB, Case JP, Block JA, Andriacchi TP. The knee adduction moment during gait in subjects with knee osteoarthritis is more closely correlated with static alignment than radiographic disease severity, toe out angle and pain. J Orthop Res. 2002;20(1):101-107 [DOI] [PubMed] [Google Scholar]
- 47. Hurwitz DE, Ryals AR, Block JA, Sharma L, Schnitzer TJ, Andriacchi TP. Knee pain and joint loading in subjects with osteoarthritis of the knee. J Orthop Res. 2000;18(4):572-579 [DOI] [PubMed] [Google Scholar]
- 48. Iorio R, Healy WL. Unicompartmental arthritis of the knee. J Bone Joint Surg Am. 2003;85(7):1351-1364 [DOI] [PubMed] [Google Scholar]
- 49. Irrgang JJ, Snyder-Mackler L, Wainner RS, Fu FH, Harner CD. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998;80(8):1132-1145 [DOI] [PubMed] [Google Scholar]
- 50. Katsuragawa Y, Fukui N, Nakamura K. Change of bone mineral density with valgus knee bracing. Int Orthop. 1999;23(3):164-167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kawakami H, Sugano N, Yonenobu K, et al. Effects of rotation on measurement of lower limb alignment for knee osteotomy. J Orthop Res. 2004;22(6):1248-1253 [DOI] [PubMed] [Google Scholar]
- 52. Kemp G, Crossley KM, Wrigley TV, Metcalf BR, Hinman RS. Reducing joint loading in medial knee osteoarthritis: shoes and canes. Arthritis Rheum. 2008;59(5):609-614 [DOI] [PubMed] [Google Scholar]
- 53. Kirkley A, Webster-Bogaert S, Litchfield R, et al. The effect of bracing on varus gonarthrosis. J Bone Joint Surg Am. 1999;81(4):539-548 [DOI] [PubMed] [Google Scholar]
- 54. Komistek RD, Dennis DA, Northcut EJ, Wood A, Parker AW, Traina SM. An in vivo analysis of the effectiveness of the osteoarthritic knee brace during heel-strike of gait. J Arthroplasty. 1999;14(6):738-742 [DOI] [PubMed] [Google Scholar]
- 55. Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States, part II. Arthritis Rheum. 2008;58(1):26-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lewek MD, Ramsey DK, Snyder-Mackler L, Rudolph KS. Knee stabilization in patients with medial compartment knee osteoarthritis. Arthritis Rheum. 2005;52(9):2845-2853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Lewek MD, Rudolph KS, Snyder-Mackler L. Control of frontal plane knee laxity during gait in patients with medial compartment knee osteoarthritis. Osteoarthritis Cartilage. 2004;12(9):745-751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Li LC, Maetzel A, Pencharz JN, Maguire L, Bombardier C. Use of mainstream nonpharmacologic treatment by patients with arthritis. Arthritis Rheum. 2004;51(2):203-209 [DOI] [PubMed] [Google Scholar]
- 59. Lindenfeld TN, Hewett TE, Andriacchi TP. Joint loading with valgus bracing in patients with varus gonarthrosis. Clin Orthop Rel Res. 1997;344:290-297 [PubMed] [Google Scholar]
- 60. Matsuno H, Kadowaki KM, Tsuji H. Generation II knee bracing for severe medial compartment osteoarthritis of the knee. Arch Phys Med Rehabil. 1997;78(7):745-749 [DOI] [PubMed] [Google Scholar]
- 61. Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002;61(7):617-622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Moore TM, Meyers MH, Harvey JP., Jr Collateral ligament laxity of the knee: long-term comparison between plateau fractures and normal. J Bone Joint Surg Am. 1976;58(5):594-598 [PubMed] [Google Scholar]
- 63. Murphy L, Schwartz TA, Helmick CG, et al. Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum. 2008;59(9):1207-1213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Nadaud MC, Komistek RD, Mahfouz MR, Dennis DA, Anderle MR. In vivo three- dimensional determination of the effectiveness of the osteoarthritic knee brace: a multiple brace analysis. J Bone Joint Surg Am. 2005;87(suppl 2):114-119 [DOI] [PubMed] [Google Scholar]
- 65. Pollo FE, Otis JC, Backus SI, Warren RF, Wickiewicz TL. Reduction of medial compartment loads with valgus bracing of the osteoarthritic knee. Am J Sports Med. 2002;30(3):414-421 [DOI] [PubMed] [Google Scholar]
- 66. Ramsey DK, Briem K, Axe MJ, Snyder-Mackler L. A mechanical theory for the effectiveness of bracing for medial compartment osteoarthritis of the knee. J Bone Joint Surg Am. 2007;89(11):2398-2407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Richards JD, Sanchez-Ballester J, Jones RK, Darke N, Livingstone BN. A comparison of knee braces during walking for the treatment of osteoarthritis of the medial compartment of the knee. J Bone Joint Surg Br. 2005;87(7):937-939 [DOI] [PubMed] [Google Scholar]
- 68. Rudolph KS, Axe MJ, Buchanan TS, Scholz JP, Snyder-Mackler L. Dynamic stability in the anterior cruciate ligament deficient knee. Knee Surg Sports Traumatol Arthrosc. 2001;9(2):62-71 [DOI] [PubMed] [Google Scholar]
- 69. Rudolph KS, Eastlack ME, Axe MJ, Snyder-Mackler L. Movement patterns after anterior cruciate ligament injury: a comparison of patients who compensate well for the injury and those who require operative stabilization. J Electromyogr Kinesiol. 1998;8(6):349-362 [DOI] [PubMed] [Google Scholar]
- 70. Schipplein OD, Andriacchi TP. Interaction between active and passive knee stabilizers during level walking. J Orthop Res. 1991;9(1):113-119 [DOI] [PubMed] [Google Scholar]
- 71. Segal L, Day SE, Chapman AB, Osborne RH. Can we reduce disease burden from osteoarthritis? Med J Aust. 2004;180(5)(suppl):S11-S17 [DOI] [PubMed] [Google Scholar]
- 72. Self BP, Greenwald RM, Pflaster DS. A biomechanical analysis of a medial unloading brace for osteoarthritis in the knee. Arthritis Care Res. 2000;13(4):191-197 [DOI] [PubMed] [Google Scholar]
- 73. Shakoor N, Block JA. Walking barefoot decreases loading on the lower extremity joints in knee osteoarthritis. Arthritis Rheum. 2006;54(9):2923-2927 [DOI] [PubMed] [Google Scholar]
- 74. Sharma L. Proprioceptive impairment in knee osteoarthritis. Rheum Dis Clin North Am. 1999;25(2):299-314 [DOI] [PubMed] [Google Scholar]
- 75. Sharma L, Lou C, Felson DT, et al. Laxity in healthy and osteoarthritic knees. Arthritis Rheum. 1999;42(5):861-870 [DOI] [PubMed] [Google Scholar]
- 76. Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286(2):188-195 [DOI] [PubMed] [Google Scholar]
- 77. Shelburne KB, Torry MR, Steadman JR, Pandy MG. Effects of foot orthoses and valgus bracing on the knee adduction moment and medial joint load during gait. Clin Biomech (Bristol, Avon). 2008;23(6):814-821 [DOI] [PubMed] [Google Scholar]
- 78. Sunny K. Changes in surgical loads and economic burden of hip and knee replacements in the US: 1997-2004. Arthritis Care Res. 2008;59(4):481-488 [DOI] [PubMed] [Google Scholar]
- 79. van der EM, Steultjens M, Wieringa H, Dinant H, Dekker J. Structural joint changes, malalignment, and laxity in osteoarthritis of the knee. Scand J Rheumatol. 2005;34(4):298-301 [DOI] [PubMed] [Google Scholar]
- 80. Warden SJ, Morris HG, Crossley KM, Brukner PD, Bennell KL. Delayed- and non-union following opening wedge high tibial osteotomy: surgeons’ results from 182 completed cases. Knee Surg Sports Traumatol Arthrosc. 2005;13(1):34-37 [DOI] [PubMed] [Google Scholar]
- 81. Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part II: OARSI evidence- based, expert consensus guidelines. Osteoarthritis Cartilage. 2008;16(2):137-162 [DOI] [PubMed] [Google Scholar]